Differential Responders to a Mixed Meal Tolerance Test Associated with Type 2 Diabetes Risk Factors and Gut Microbiota—Data from the MEDGI-Carb Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Trial and Dietary Intervention
2.2. Mixed Meal Tolerance Tests
2.3. Oral Glucose Tolerance Test
2.4. Fecal Microbiota
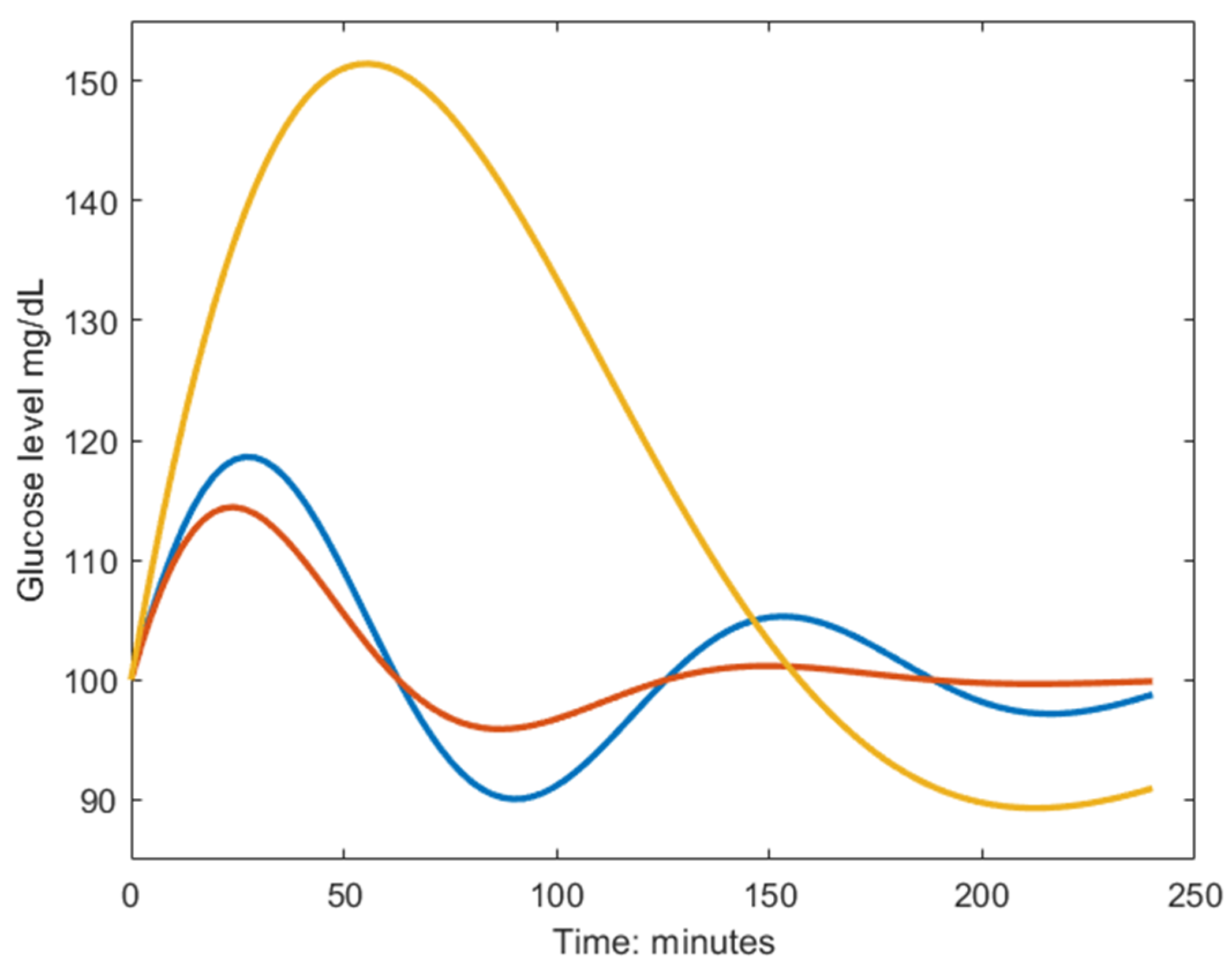
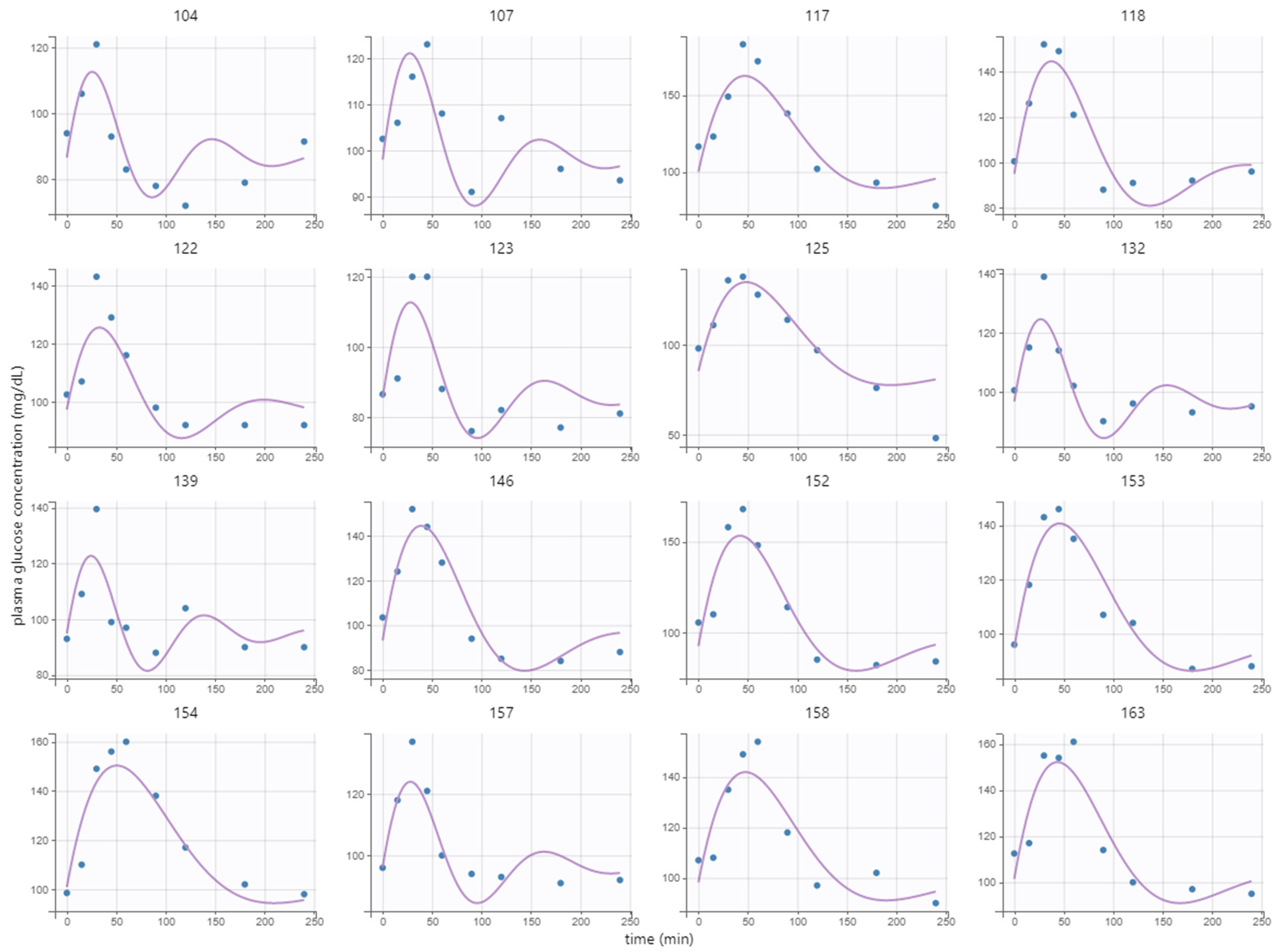
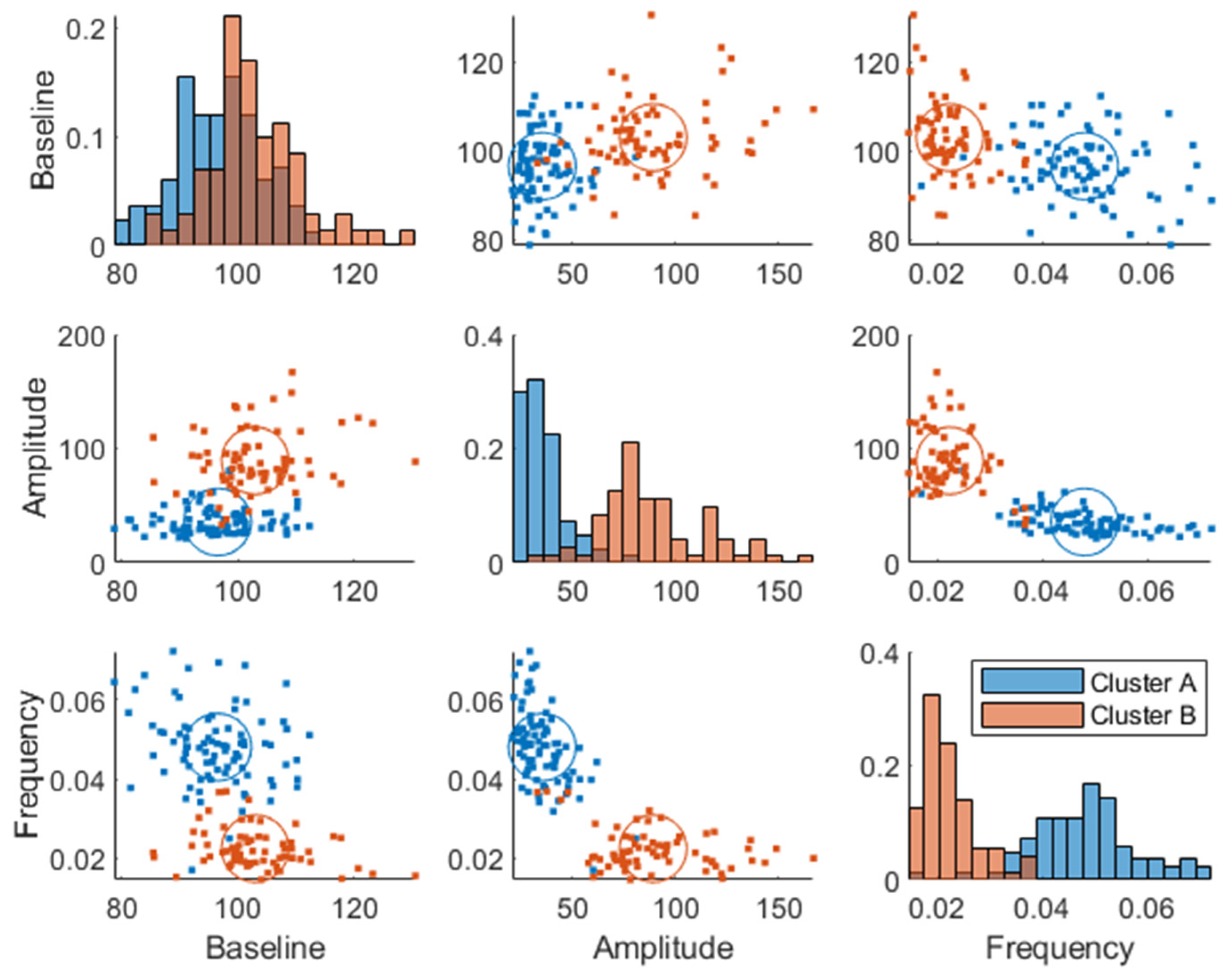
2.5. Mechanistic Model of Glucose Regulation
2.6. Statistical Analyses
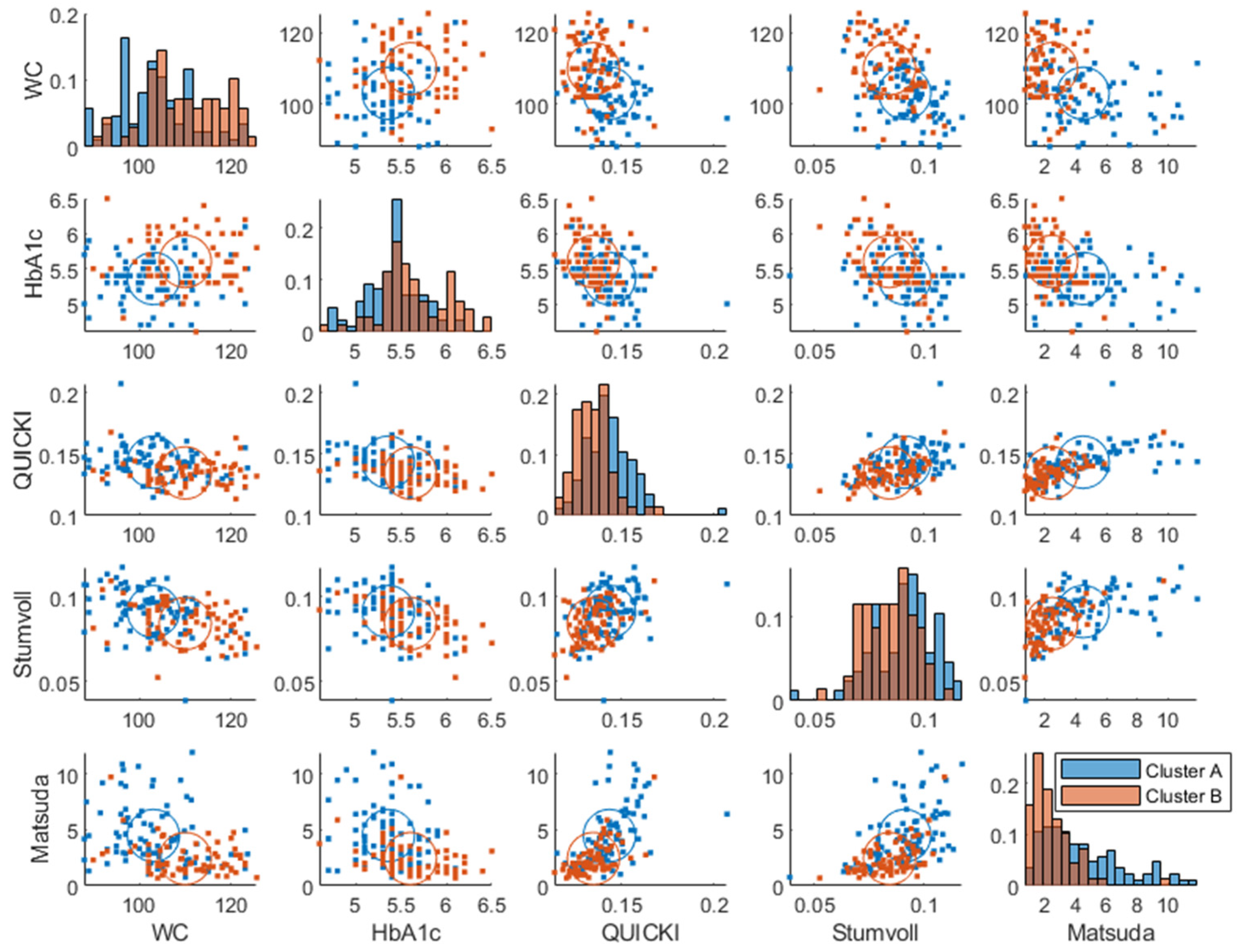
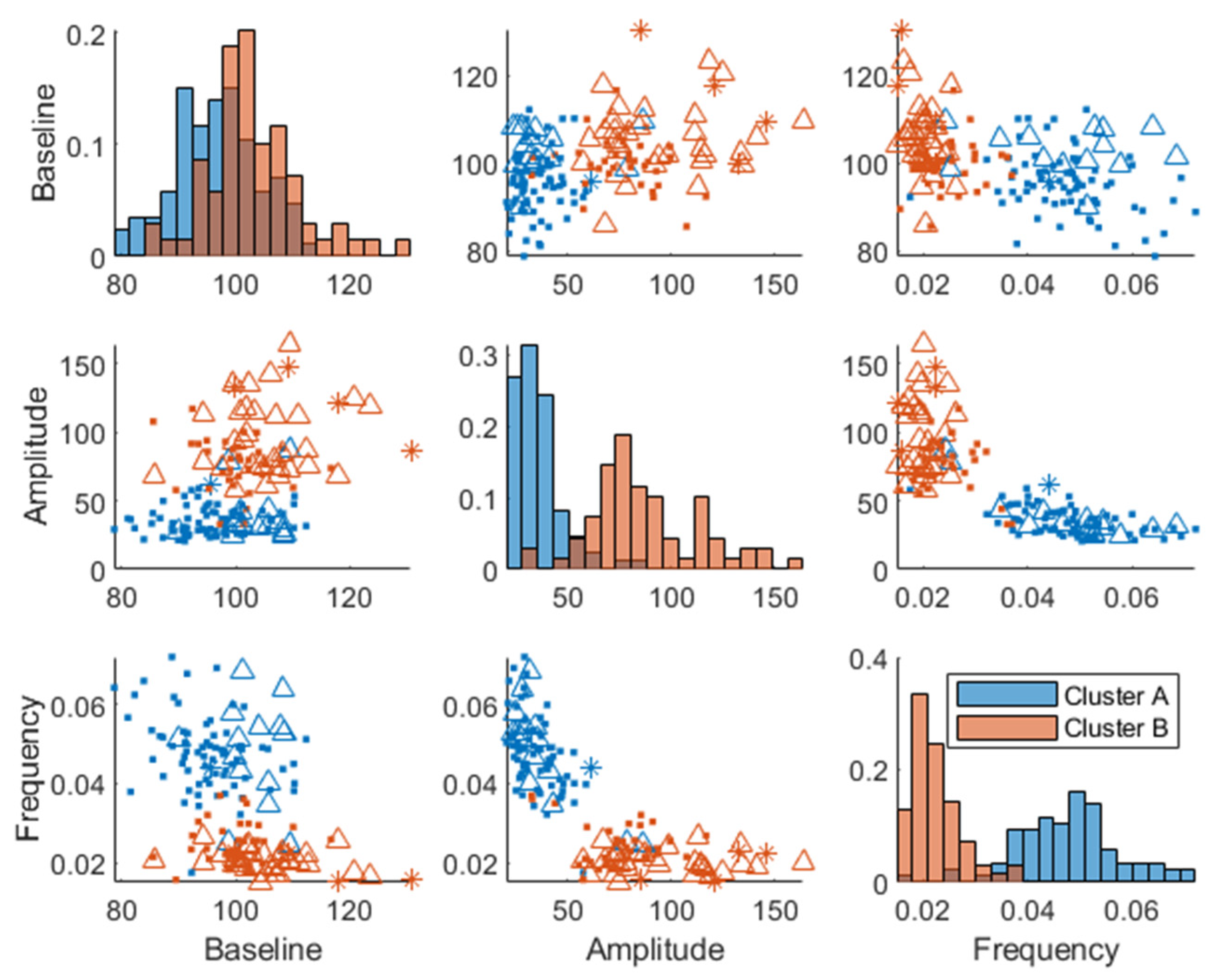
3. Results
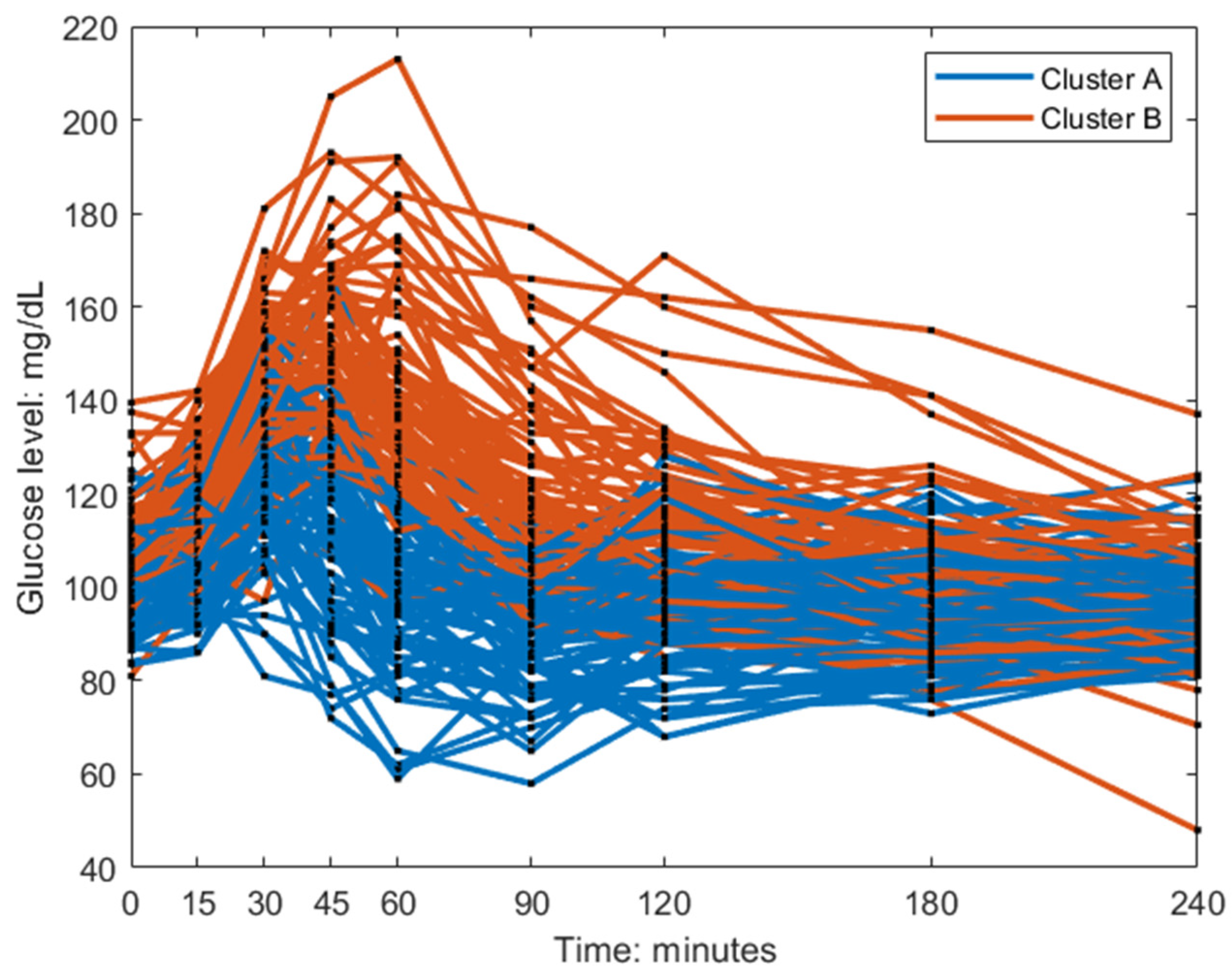
Postprandial MMTT Glucose Responses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yan, Y.; Wu, T.; Zhang, M.; Li, C.; Liu, Q.; Li, F. Prevalence, awareness and control of type 2 diabetes mellitus and risk factors in Chinese elderly population. BMC Public Health 2022, 22, 1382. [Google Scholar] [CrossRef] [PubMed]
- Balakumar, P.; Maung, U.K.; Jagadeesh, G. Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol. Res. 2016, 113, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Henning, R.J. Type-2 diabetes mellitus and cardiovascular disease. Future Cardiol. 2018, 14, 491–509. [Google Scholar] [CrossRef] [PubMed]
- Blaak, E.E.; Antoine, J.M.; Benton, D.; Björck, I.; Bozzetto, L.; Brouns, F.; Diamant, M.; Dye, L.; Hulshof, T.; Holst, J.J.; et al. Impact of postprandial glycaemia on health and prevention of disease. Obes. Rev. 2012, 13, 923–984. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; Colagiuri, S.; Gerich, J.; Tuomilehto, J. Guideline for management of postmeal glucose. Nutr. Metab. Cardiovasc. Dis. 2008, 18, S17–S33. [Google Scholar] [CrossRef] [PubMed]
- Zeevi, D.; Korem, T.; Zmora, N.; Israeli, D.; Rothschild, D.; Weinberger, A.; Ben-Yacov, O.; Lador, D.; Avnit-Sagi, T.; Lotan-Pompan, M.; et al. Personalized Nutrition by Prediction of Glycemic Responses. Cell 2015, 163, 1079–1094. [Google Scholar] [CrossRef] [PubMed]
- Hall, H.; Perelman, D.; Breschi, A.; Limcaoco, P.; Kellogg, R.; McLaughlin, T.; Snyder, M. Glucotypes reveal new patterns of glucose dysregulation. PLoS Biol. 2018, 16, e2005143. [Google Scholar] [CrossRef]
- Berry, S.E.; Valdes, A.M.; Drew, D.A.; Asnicar, F.; Mazidi, M.; Wolf, J.; Capdevila, J.; Hadjigeorgiou, G.; Davies, R.; Al Khatib, H.; et al. Human postprandial responses to food and potential for precision nutrition. Nat. Med. 2020, 26, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Ben-Yacov, O.; Godneva, A.; Rein, M.; Shilo, S.; Kolobkov, D.; Koren, N.; Cohen Dolev, N.; Travinsky Shmul, T.; Wolf, B.C.; Kosower, N.; et al. Personalized Postprandial Glucose Response-Targeting Diet Versus Mediterranean Diet for Glycemic Control in Prediabetes. Diabetes Care 2021, 44, 1980–1991. [Google Scholar] [CrossRef]
- Morris, C.; O’Grada, C.; Ryan, M.; Roche, H.M.; Gibney, M.J.; Gibney, E.R.; Brennan, L. Identification of Differential Responses to an Oral Glucose Tolerance Test in Healthy Adults. PLoS ONE 2013, 8, e72890. [Google Scholar] [CrossRef] [PubMed]
- Lages, M.; Barros, R.; Moreira, P.; Guarino, M.P. Metabolic Effects of an Oral Glucose Tolerance Test Compared to the Mixed Meal Tolerance Tests: A Narrative Review. Nutrients 2022, 14, 2032. [Google Scholar] [CrossRef] [PubMed]
- Bergia, R.E.; Biskup, I.; Giacco, R.; Costabile, G.; Gray, S.; Wright, A.; Vitale, M.; Campbell, W.W.; Landberg, R.; Riccardi, G. The MEDGICarb-Study: Design of a multi-center randomized controlled trial to determine the differential health-promoting effects of low- and high-glycemic index Mediterranean-style eating patterns. Contemp. Clin. Trials Commun. 2020, 19, 100640. [Google Scholar] [CrossRef] [PubMed]
- Bergia, R.E.; Giacco, R.; Hjorth, T.; Biskup, I.; Zhu, W.; Costabile, G.; Vitale, M.; Campbell, W.W.; Landberg, R.; Riccardi, G. Differential Glycemic Effects of Low- versus High-Glycemic Index Mediterranean-Style Eating Patterns in Adults at Risk for Type 2 Diabetes: The MEDGI-Carb Randomized Controlled Trial. Nutrients 2022, 14, 706. [Google Scholar] [CrossRef]
- Gutch, M.; Kumar, S.; Razi, S.M.; Gupta, K.K.; Gupta, A. Assessment of insulin sensitivity/resistance. Indian J. Endocrinol. Metab. 2015, 19, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Iversen, K.N.; Dicksved, J.; Zoki, C.; Fristedt, R.; Pelve, E.A.; Langton, M.; Landberg, R. The Effects of High Fiber Rye, Compared to Refined Wheat, on Gut Microbiota Composition, Plasma Short Chain Fatty Acids, and Implications for Weight Loss and Metabolic Risk Factors (the RyeWeight Study). Nutrients 2022, 14, 1669. [Google Scholar] [CrossRef]
- Palmnäs-Bédard, M.S.A.; Costabile, G.; Vetrani, C.; Åberg, S.; Hjalmarsson, Y.; Dicksved, J.; Riccardi, G.; Landberg, R. The human gut microbiota and glucose metabolism: A scoping review of key bacteria and the potential role of SCFAs. Am. J. Clin. Nutr. 2022, 116, 862–874. [Google Scholar] [CrossRef] [PubMed]
- Maskarinec, G.; Raquinio, P.; Kristal, B.S.; Setiawan, V.W.; Wilkens, L.R.; Franke, A.A.; Lim, U.; Le Marchand, L.; Randolph, T.W.; Lampe, J.W.; et al. The gut microbiome and type 2 diabetes status in the Multiethnic Cohort. PLoS ONE 2021, 16, e0250855. [Google Scholar] [CrossRef]
- Shen, N.; Dimitrova, N.; Ho, C.H.; Torres, P.J.; Camacho, F.R.; Cai, Y.; Vuyisich, M.; Tanton, D.; Banavar, G. Gut microbiome activity predicts risk of type 2 diabetes and metformin control in a large human cohort. medRxiv 2021. [Google Scholar] [CrossRef]
- Lippert, K.; Kedenko, L.; Antonielli, L.; Kedenko, I.; Gemeier, C.; Leitner, M.; Kautzky-Willer, A.; Paulweber, B.; Hackl, E. Gut microbiota dysbiosis associated with glucose metabolism disorders and the metabolic syndrome in older adults. Benef. Microbes 2017, 8, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Egshatyan, L.; Kashtanova, D.; Popenko, A.; Tkacheva, O.; Tyakht, A.; Alexeev, D.; Karamnova, N.; Kostryukova, E.; Babenko, V.; Vakhitova, M.; et al. Gut microbiota and diet in patients with different glucose tolerance. Endocr. Connect. 2016, 5, 1–9. [Google Scholar] [CrossRef]
- Liu, X.; Mao, B.; Gu, J.; Wu, J.; Cui, S.; Wang, G.; Zhao, J.; Zhang, H.; Chen, W. Blautia—A new functional genus with potential probiotic properties? Gut Microbes 2021, 13, 1875796. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Shen, D.; Fang, Z.; Jie, Z.; Qiu, X.; Zhang, C.; Chen, Y.; Ji, L. Human Gut Microbiota Changes Reveal the Progression of Glucose Intolerance. PLoS ONE 2013, 8, e71108. [Google Scholar] [CrossRef] [PubMed]
- Cobelli, C.; Dalla Man, C.; Sparacino, G.; Magni, L.; De Nicolao, G.; Kovatchev, B.P. Diabetes: Models, Signals, and Control. IEEE Rev. Biomed. Eng. 2009, 2, 54–96. [Google Scholar] [CrossRef] [PubMed]
- Bolie, V.W. Coefficients of normal blood glucose regulation. J. Appl. Physiol. 1961, 16, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, E.; Rosevear, J.W.; McGuckin, W.F. A Mathematical Model of the Glucose-tolerance test. Phys. Med. Biol. 1964, 9, 203. [Google Scholar] [CrossRef]
- Fowles, G.R.; Cassiday, G.L. Analytical Mechanics: Fifth Edition, 5th ed.; Saunders: Fort Worth, TX, USA, 1986. [Google Scholar]
- Shiang, K.-D.; Kandeel, F. A computational model of the human glucose-insulin regulatory system. J. Biomed. Res. 2010, 24, 347–364. [Google Scholar] [CrossRef]
- Lindstrom, M.J.; Bates, D.M. Nonlinear mixed effects models for repeated measures data. Biometrics 1990, 46, 673–687. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Westerhuis, J.A.; Rosén, J.; Landberg, R.; Brunius, C. Variable selection and validation in multivariate modelling. Bioinformatics 2019, 35, 972–980. [Google Scholar] [CrossRef] [PubMed]
- Petersmann, A.; Müller-Wieland, D.; Müller, U.A.; Landgraf, R.; Nauck, M.; Freckmann, G.; Heinemann, L.; Schleicher, E. Definition, Classification and Diagnosis of Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2019, 127, S1–S7. [Google Scholar] [CrossRef] [PubMed]
- Placzkowska, S.; Pawlik-Sobecka, L.; Kokot, I.; Piwowar, A. Indirect insulin resistance detection: Current clinical trends and laboratory limitations. Biomed. Pap. 2019, 163, 187–199. [Google Scholar] [CrossRef]
- Vitale, M.; Costabile, G.; Bergia, R.E.; Hjorth, T.; Campbell, W.W.; Landberg, R.; Riccardi, G.; Giacco, R. The effects of Mediterranean diets with low or high glycemic index on plasma glucose and insulin profiles are different in adult men and women: Data from MEDGI-Carb randomized clinical trial. Clin. Nutr. 2023, 42, 2022–2028. [Google Scholar] [CrossRef]
- Lachmann, E.H.; Fox, R.A.; Dennison, R.A.; Usher-Smith, J.A.; Meek, C.L.; Aiken, C.E. Barriers to completing oral glucose tolerance testing in women at risk of gestational diabetes. Diabet. Med. 2020, 37, 1482–1489. [Google Scholar] [CrossRef] [PubMed]
- Wolever, T.M.S.; Chiasson, J.-L.; Csima, A.; Hunt, J.A.; Palmason, C.; Ross, S.A.; Ryan, E.A. Variation of Postprandial Plasma Glucose, Palatability, and Symptoms Associated With a Standardized Mixed Test Meal Versus 75 g Oral Glucose. Diabetes Care 1998, 21, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Nuttall, F.Q.; Gannon, M.C.; Wald, J.L.; Ahmed, M. Plasma glucose and insulin profiles in normal subjects ingesting diets of varying carbohydrate, fat, and protein content. J. Am. Coll. Nutr. 1985, 4, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Nuttall, F.Q.; Mooradian, A.D.; Gannon, M.C.; Billington, C.; Krezowski, P. Effect of protein ingestion on the glucose and insulin response to a standardized oral glucose load. Diabetes Care 1984, 7, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.L.; Davies, I.G.; Waraksa, W.; Khayyatzadeh, S.S.; Al-Asmakh, M.; Mazidi, M. The Impact of Microbial Composition on Postprandial Glycaemia and Lipidaemia: A Systematic Review of Current Evidence. Nutrients 2021, 13, 3887. [Google Scholar] [CrossRef]
- Caumo, A.; Bergman, R.N.; Cobelli, C. Insulin sensitivity from meal tolerance tests in normal subjects: A minimal model index. J. Clin. Endocrinol. Metab. 2000, 85, 4396–4402. [Google Scholar] [CrossRef] [PubMed]
- Gentilcore, D.; Chaikomin, R.; Jones, K.L.; Russo, A.; Feinle-Bisset, C.; Wishart, J.M.; Rayner, C.K.; Horowitz, M. Effects of fat on gastric emptying of and the glycemic, insulin, and incretin responses to a carbohydrate meal in type 2 diabetes. J. Clin. Endocrinol. Metab. 2006, 91, 2062–2067. [Google Scholar] [CrossRef]
- Rijkelijkhuizen, J.M.; McQuarrie, K.; Girman, C.J.; Stein, P.P.; Mari, A.; Holst, J.J.; Nijpels, G.; Dekker, J.M. Effects of meal size and composition on incretin, alpha-cell, and beta-cell responses. Metabolism 2010, 59, 502–511. [Google Scholar] [CrossRef]

| High GI Meal | |||||||
| Foods Name | Serving Size (g) | Energy (Kilocalories) | Proteins (g) | Fat (g) | Total Carbohydrates (g) | Soluble Carbohydrates (g) | Total Dietary Fiber (g) |
| Breakfast | |||||||
| Cornflakes | 30 | 140.4 | 2.5 | 0.3 | 26.4 | 4.0 | 1.5 |
| Bread wholegrain, Pan Bauletto (Barilla) | 24 | 64.0 | 2.0 | 0.9 | 11.4 | 1.7 | 1.1 |
| Eggs, whole * | 50 | 77.5 | 6.3 | 5.3 | 0.6 | 0.0 | 0.0 |
| Extra virgin oil, olive | 18 | 162.0 | 0.0 | 18.0 | 0.0 | 0.0 | 0.0 |
| Ham, dry cured (country style), no visible fat eaten | 85 | 52.2 | 7.5 | 2.0 | 0.5 | 0.0 | 0.0 |
| Apple, fresh, without skin (Golden Delicious) * | 150 * | 78.0 | 0.4 | 0.3 | 20.7 | 20.7 | 3.6 |
| Milk, 1% fat or low-fat, lactose-free | 244 | 102.5 | 8.2 | 2.4 | 12.2 | 12.2 | 0.0 |
| TOTAL | 676.6 | 27.0 | 29.1 | 71.8 | 38.6 | 6.2 | |
| Low GI Meal | |||||||
| Foods Name | Serving Size (g) | Energy (Kilocalories) | Proteins (g) | Fat (g) | Total Carbohydrates (g) | Soluble Carbohydrates (g) | Total Dietary Fiber (g) |
| Breakfast | |||||||
| Piadella (Mulino Bianco—Barilla) | 75 | 255.0 | 5.6 | 8.4 | 38.3 | 2.3 | 2.0 |
| Extra virgin oil, olive | 10 | 90.0 | 0.0 | 10.0 | 0.0 | 0.0 | 0.0 |
| Eggs, whole * | 50 | 77.5 | 6.3 | 5.3 | 0.6 | 0.0 | 0.0 |
| Ham, dry cured (country style), no visible fat eaten | 38 | 60.9 | 7.7 | 3.1 | 0.0 | 0.0 | 0.0 |
| Apple, fresh, without skin (Golden Delicious) * | 150 * | 78.0 | 0.4 | 0.3 | 20.7 | 20.7 | 3.6 |
| Milk, 1% fat or low-fat, lactose-free | 244 | 102.5 | 8.2 | 2.4 | 12.2 | 12.2 | 0.0 |
| TOTAL | 663.9 | 28.2 | 29.4 | 71.7 | 35.2 | 5.6 | |
| High GI (MMTT and OGTT) | Low GI (MMTT and OGTT) | High GI (Fecal Microbiota) | Low GI (Fecal Microbiota) | |
|---|---|---|---|---|
| Number of participants | 72 (50% women) | 83 (54% women) | 57 (51% women) | 73 (53% women) |
| Age (years) | 55.8 ± 9.9 | 56.0 ± 10.5 | 57.0 ± 9.7 | 55.8 ± 10.7 |
| BMI (kg/m2) | 30.8 ± 3.0 | 31.1 ± 3.2 | 30.4 ± 3.1 | 30.9 ± 3.2 |
| Waist circumference (cm) | 107.3 ± 9.2 | 105.1 ± 8.6 | 106.5 ± 9.2 | 105.1 ± 8.4 |
| Glucose (mg/dL) | 105.5 ± 10.2 | 103.4 ± 10.3 | 106.4 ± 10.5 | 102.9 ± 10.2 |
| Total cholesterol (mg/dL) | 187.8 ± 30.8 | 192.2 ± 33.0 | 189.7 ± 30.5 | 192.7 ± 32.7 |
| Triglycerides (mg/dL) | 114.8 ± 44.6 | 122.2 ± 68.8 | 113.9 ± 45.5 | 117.6 ± 60.0 |
| HDL (mg/dL) | 48.4 ± 11.6 | 47.7 ± 11.8 | 50.2 ± 11.8 | 47.9 ± 11.8 |
| LDL (mg/dL) | 116.1 ± 27.6 | 119.8 ± 26.6 | 116.8 ± 27.4 | 120.6 ± 27.3 |
| Systolic blood pressure (mm Hg) | 124.6 ± 12.4 | 128.5 ± 13.7 | 124.1 ± 12.5 | 128.1 ± 13.8 |
| Diastolic blood pressure (mm Hg) | 80.9 ± 8.9 | 81.9 ± 8.5 | 81.1 ± 9.0 | 82.1 ± 8.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skantze, V.; Hjorth, T.; Wallman, M.; Brunius, C.; Dicksved, J.; Pelve, E.A.; Esberg, A.; Vitale, M.; Giacco, R.; Costabile, G.; et al. Differential Responders to a Mixed Meal Tolerance Test Associated with Type 2 Diabetes Risk Factors and Gut Microbiota—Data from the MEDGI-Carb Randomized Controlled Trial. Nutrients 2023, 15, 4369. https://doi.org/10.3390/nu15204369
Skantze V, Hjorth T, Wallman M, Brunius C, Dicksved J, Pelve EA, Esberg A, Vitale M, Giacco R, Costabile G, et al. Differential Responders to a Mixed Meal Tolerance Test Associated with Type 2 Diabetes Risk Factors and Gut Microbiota—Data from the MEDGI-Carb Randomized Controlled Trial. Nutrients. 2023; 15(20):4369. https://doi.org/10.3390/nu15204369
Chicago/Turabian StyleSkantze, Viktor, Therese Hjorth, Mikael Wallman, Carl Brunius, Johan Dicksved, Erik A. Pelve, Anders Esberg, Marilena Vitale, Rosalba Giacco, Giuseppina Costabile, and et al. 2023. "Differential Responders to a Mixed Meal Tolerance Test Associated with Type 2 Diabetes Risk Factors and Gut Microbiota—Data from the MEDGI-Carb Randomized Controlled Trial" Nutrients 15, no. 20: 4369. https://doi.org/10.3390/nu15204369
APA StyleSkantze, V., Hjorth, T., Wallman, M., Brunius, C., Dicksved, J., Pelve, E. A., Esberg, A., Vitale, M., Giacco, R., Costabile, G., Bergia, R. E., Jirstrand, M., Campbell, W. W., Riccardi, G., & Landberg, R. (2023). Differential Responders to a Mixed Meal Tolerance Test Associated with Type 2 Diabetes Risk Factors and Gut Microbiota—Data from the MEDGI-Carb Randomized Controlled Trial. Nutrients, 15(20), 4369. https://doi.org/10.3390/nu15204369








