Feasibility, Acceptability, and Initial Efficacy of a Digital Intervention to Improve Consumption of Foods Received within a National Nutrition Assistance Program
Abstract
1. Introduction
2. Materials and Methods
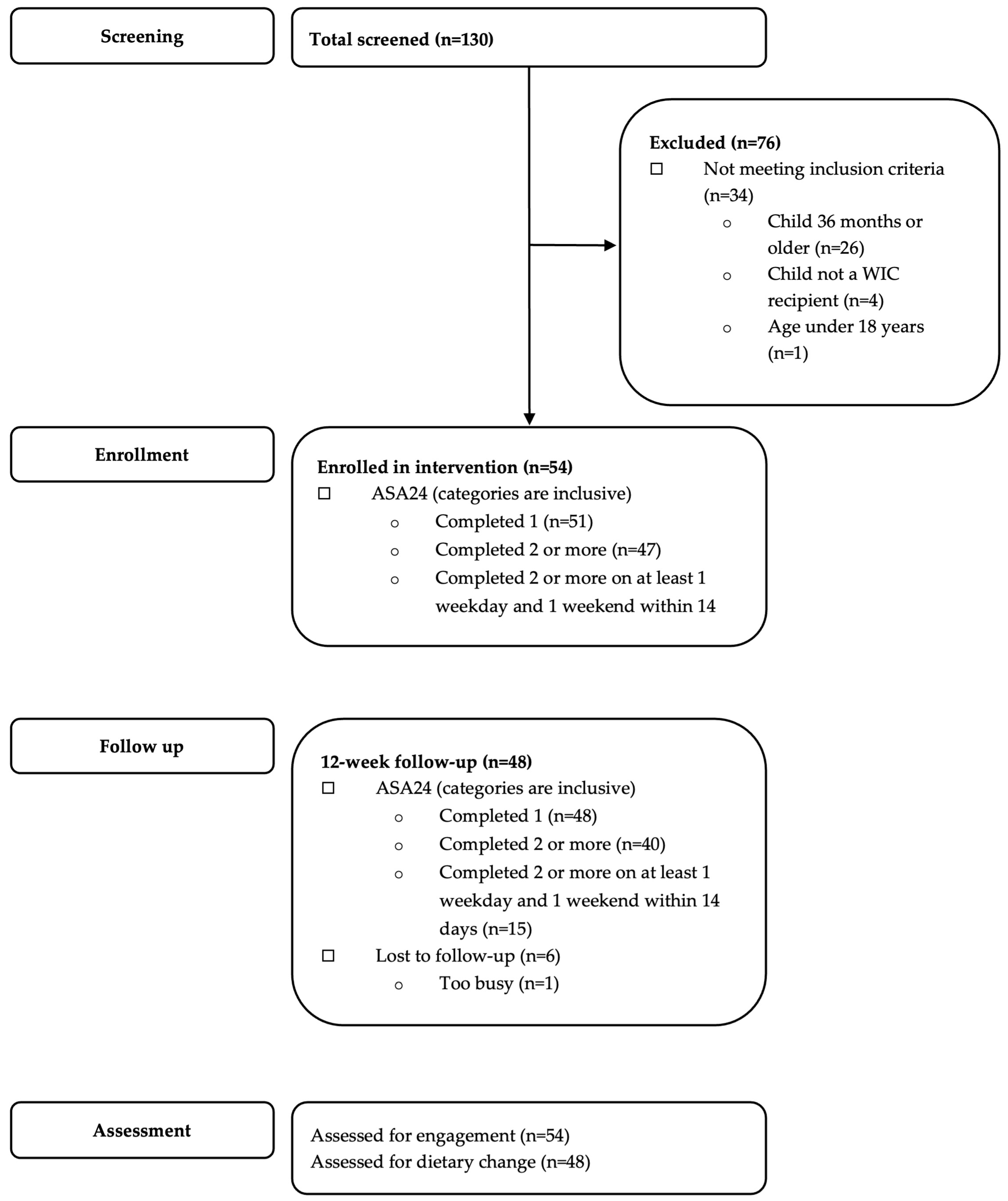
2.1. Study Design and Eligibility
2.2. Intervention Description
Behavioral Change Goals
2.3. Measures
2.4. Reach and Representativeness
2.5. Implementation
2.6. Acceptability
2.7. Preliminary Efficacy
2.8. Analysis
3. Results
3.1. Reach and Representativeness
Baseline Characteristics
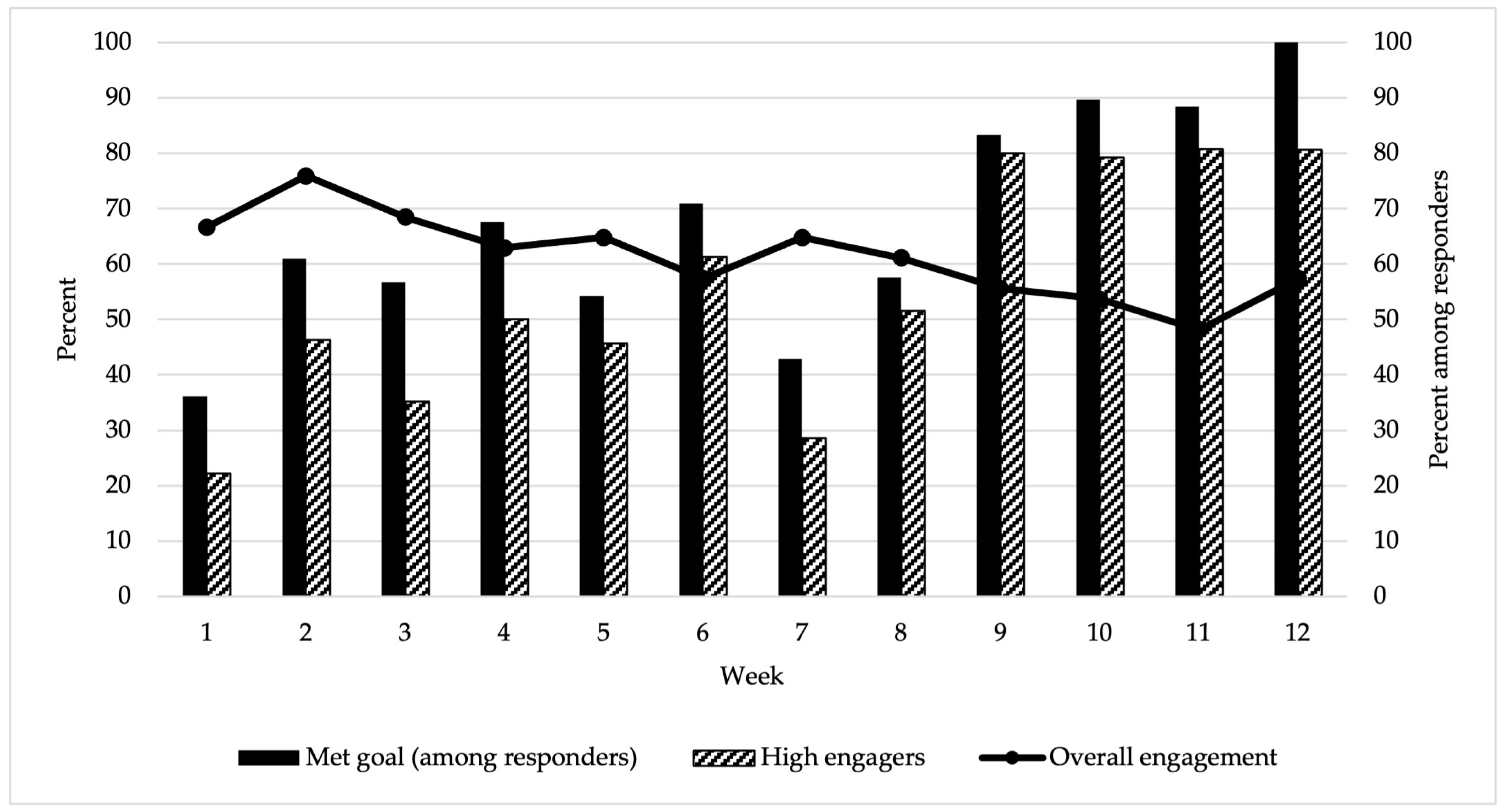
3.2. Implementation
3.3. Preliminary Efficacy
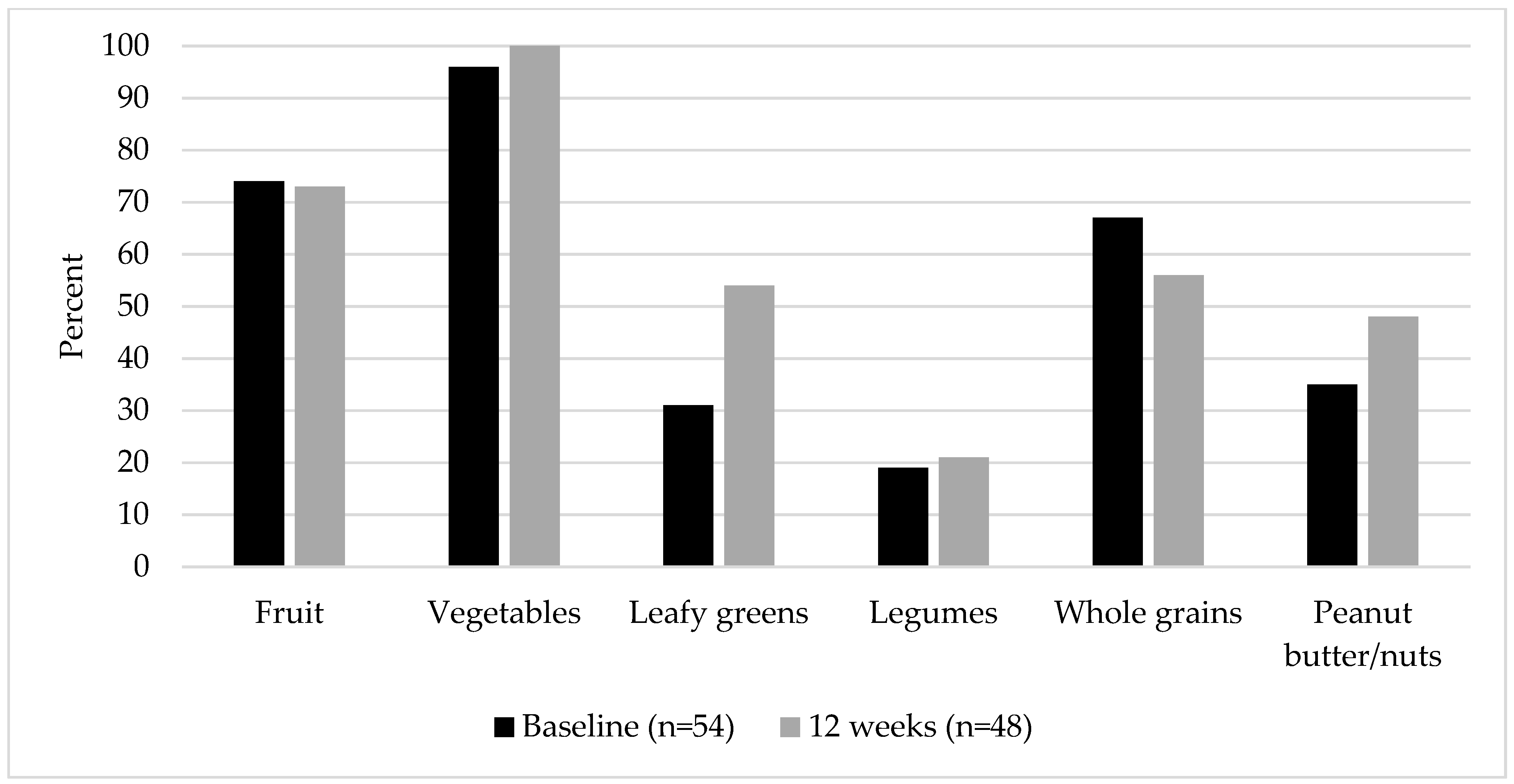
3.3.1. Consumption of WIC-Approved Food Groups
3.3.2. Diet Quality
3.3.3. Acceptability
“I was able to learn how to use what WIC offered me on certain vegetables that I wouldn’t have usually bought for my family”.
“Finding more ways to incorporate more ideas for the harder ingredients like the greens and stuff that kids don’t like”.
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Birch, L.L.; Doub, A.E. Learning to eat: Birth to age 2 y. Am. J. Clin. Nutr. 2014, 99, 723S–728S. [Google Scholar] [CrossRef]
- Thompson, A.L. Evaluating the pathways linking complementary feeding practices to obesity in early life. Nutr Rev. 2020, 78 (Suppl. 2), 13–24. [Google Scholar] [CrossRef] [PubMed]
- Pool, L.R.; Aguayo, L.; Brzezinski, M.; Perak, A.M.; Davis, M.M.; Greenland, P.; Hou, L.; Marino, B.S.; Van Horn, L.; Wakschlag, L.; et al. Childhood Risk Factors and Adulthood Cardiovascular Disease: A Systematic Review. J. Pediatr. 2021, 232, 118–126.e23. [Google Scholar] [CrossRef] [PubMed]
- Rose, C.M.; Birch, L.L.; Savage, J.S. Dietary patterns in infancy are associated with child diet and weight outcomes at 6 years. Int. J. Obes. 2017, 5, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Pan, L.; Sherry, B.; Li, R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014, 134 (Suppl. 1), S56–S62. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Agosti, M. Nutrition in the first 1000 days: Ten practices to minimize obesity emerging from published science. Int. J. Environ. Res. Public Health 2017, 14, 1491. [Google Scholar] [CrossRef]
- Skinner, J.D.; Carruth, B.R.; Wendy, B.; Ziegler, P.J. Children’s food preferences: A longitudinal analysis. J. Am. Diet. Assoc. 2002, 102, 1638–1647. [Google Scholar] [CrossRef]
- Howard, A.J.; Mallan, K.M.; Byrne, R.; Magarey, A.; Daniels, L.A. Toddlers’ food preferences. The impact of novel food exposure, maternal preferences and food neophobia. Appetite 2012, 59, 818–825. [Google Scholar] [CrossRef]
- Robinson, S.; Marriott, L.; Poole, J.; Crozier, S.; Borland, S.; Lawrence, W.; Law, C.; Godfrey, K.; Cooper, C.; Inskip, H.; et al. Dietary patterns in infancy: The importance of maternal and family influences on feeding practice. Br. J. Nutr. 2007, 98, 1029–1037. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Guenther, P.M.; Subar, A.F.; Kirkpatrick, S.I.; Dodd, K.W. Americans do not meet federal dietary recommendations. J. Nutr. 2010, 140, 1832–1838. [Google Scholar] [CrossRef]
- Kay, M.C.; Wasser, H.; Adair, L.S.; Thompson, A.L.; Siega-Riz, A.M.; Suchindran, C.M.; Bentley, M.E. Consumption of key food groups during the postpartum period in low-income, non-Hispanic black mothers. Appetite 2017, 117, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Jun, S.; Thuppal, S.V.; Maulding, M.K.; Eicher-Miller, H.A.; Savaiano, D.A.; Bailey, R.L. Poor Dietary Guidelines Compliance among Low-Income Women Eligible for Supplemental Nutrition Assistance Program-Education (SNAP-Ed). Nutrients 2018, 10, 327. [Google Scholar] [CrossRef]
- Ashman, A.M.; Collins, C.E.; Hure, A.J.; Jensen, M.; Oldmeadow, C. Maternal diet during early childhood, but not pregnancy, predicts diet quality and fruit and vegetable acceptance in offspring. Matern. Child Nutr. 2016, 12, 579–590. [Google Scholar] [CrossRef] [PubMed]
- US Department of Agriculture FNS. About WIC. Updated 02/14/2018. Available online: https://www.fns.usda.gov/wic/about-wic (accessed on 10 December 2018).
- United States Department of Agriculture. Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Available online: https://www.fns.usda.gov/wic (accessed on 29 March 2022).
- Li, X.; McLaughlin, P.W.; Saitone, T.L.; Sexton, R.J. The Magnitude and Determinants of Partial Redemptions of Food Benefits in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC). Am. J. Health Promot. 2021, 35, 775–783. [Google Scholar] [CrossRef]
- Gago, C.M.; Wynne, J.O.; Moore, M.J.; Cantu-Aldana, A.; Vercammen, K.; Zatz, L.Y.; May, K.; Andrade, T.; Mendoza, T.; Stone, S.L.; et al. Caregiver Perspectives on Underutilization of WIC: A Qualitative Study. Pediatrics 2022, 149, e2021053889. [Google Scholar] [CrossRef] [PubMed]
- Weber, S.; Uesugi, K.; Greene, H.; Bess, S.; Reese, L.; Odoms-Young, A. Preferences and Perceived Value of WIC Foods Among WIC Caregivers. J. Nutr. Educ. Behav. 2018, 50, 695–704. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Review of WIC Food Packages: Improving Balance and Choice; The National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- Pew Research Center. Internet/Broadband Fact Sheet. 5 February 2018. Available online: http://www.pewinternet.org/fact-sheet/internet-broadband/ (accessed on 2 November 2018).
- Pew Research Center. Mobile Fact Sheet. 5 February 2018. Available online: http://www.pewinternet.org/fact-sheet/mobile/ (accessed on 30 October 2018).
- Weber, S.J.; Dawson, D.; Greene, H.; Hull, P.C. Mobile Phone Apps for Low-Income Participants in a Public Health Nutrition Program for Women, Infants, and Children (WIC): Review and Analysis of Features. JMIR mHealth uHealth 2018, 11, e12261. [Google Scholar] [CrossRef]
- Bensley, R.J.; Anderson, J.V.; Brusk, J.J.; Mercer, N.; Rivas, J. Impact of internet vs traditional Special Supplemental Nutrition Program for Women, Infants, and Children nutrition education on fruit and vegetable intake. J. Am. Diet. Assoc. 2011, 111, 749–755. [Google Scholar] [CrossRef]
- Harari, N.; Rosenthal, M.S.; Bozzi, V.; Goeschel, L.; Jayewickreme, T.; Onyebeke, C.; Griswold, M.; Perez-Escamilla, R. Feasibility and acceptability of a text message intervention used as an adjunct tool by WIC breastfeeding peer counsellors: The LATCH pilot. Matern. Child Nutr. 2018, 14, e12488. [Google Scholar] [CrossRef]
- Gibby, C.L.; Palacios, C.; Campos, M.; Graulau, R.E.; Banna, J. Acceptability of a text message-based intervention for obesity prevention in infants from Hawai ‘i and Puerto Rico WIC. BMC Pregnancy Childbirth 2019, 19, 291. [Google Scholar] [CrossRef]
- Valdez, D.; Palacios, C.; Banna, J. Determining Acceptability of a Text-message Based Intervention to Prevent Excessive Gestational Weight Gain in Low-income Women in Hawai’i WIC (P04-029-19). Curr. Dev. Nutr. 2019, 3 (Suppl. 1), nzz051.P04-029-19. [Google Scholar] [CrossRef]
- Teasdale, N.; Elhussein, A.; Butcher, F.; Piernas, C.; Cowburn, G.; Hartmann-Boyce, J.; Saksena, R.; Scarborough, P. Systematic review and meta-analysis of remotely delivered interventions using self-monitoring or tailored feedback to change dietary behavior. Am. J. Clin. Nutr. 2018, 107, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Kay, M.C.; Hammad, N.M.; Herring, S.J.; Bennett, G.G. Using Interactive Text Messaging to Improve Diet Quality and Increase Redemption of Foods Approved by the Special Supplemental Nutrition Program for Women, Infants, and Children: Protocol for a Cohort Feasibility Study. JMIR Res. Protoc. 2021, 10, e32441. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Patridge, E.F.; Bardyn, T.P. Research electronic data capture (REDCap). J. Med. Libr. Assoc. JMLA 2018, 106, 142. [Google Scholar] [CrossRef]
- Subar, A.F.; Kirkpatrick, S.I.; Mittl, B.; Zimmerman, T.P.; Thompson, F.E.; Bingley, C.; Willis, G.; Islam, N.G.; Baranowski, T.; McNutt, S.; et al. The Automated Self-Administered 24-hour dietary recall (ASA24): A resource for researchers, clinicians, and educators from the National Cancer Institute. J. Acad. Nutr. Diet. 2012, 112, 1134–1137. [Google Scholar] [CrossRef]
- Berger, M.B.; Steinberg, D.M.; Askew, S.; Gallis, J.A.; Treadway, C.C.; Egger, J.R.; Kay, M.C.; Batch, B.C.; Finkelstein, E.A.; DeVries, A.; et al. The Balance protocol: A pragmatic weight gain prevention randomized controlled trial for medically vulnerable patients within primary care. BMC Public Health 2019, 19, 596. [Google Scholar] [CrossRef]
- Foley, P.; Levine, E.; Askew, S.; Puleo, E.; Whiteley, J.; Batch, B.; Heil, D.; Dix, D.; Lett, V.; Lanpher, M.; et al. Weight gain prevention among black women in the rural community health center setting: The Shape Program. BMC Public Health 2012, 12, 305. [Google Scholar] [CrossRef]
- Greaney, M.L.; Quintiliani, L.M.; Warner, E.T.; King, D.K.; Emmons, K.M.; Colditz, G.A.; Glasgow, R.E.; Bennett, G.G. Weight management among patients at community health centers: The “Be Fit, Be Well” study. Obes. Weight Manag. 2009, 5, 222–228. [Google Scholar] [CrossRef]
- Steinberg, D.M.; Levine, E.L.; Askew, S.; Foley, P.; Bennett, G.G. Daily text messaging for weight control among racial and ethnic minority women: Randomized controlled pilot study. J. Med. Internet Res. 2013, 15, e244. [Google Scholar] [CrossRef]
- Bennett, G.G.; Warner, E.T.; Glasgow, R.E.; Askew, S.; Goldman, J.; Ritzwoller, D.P.; Emmons, K.M.; Rosner, B.A.; Colditz, G.A. Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch. Intern. Med. 2012, 172, 565–574. [Google Scholar] [CrossRef]
- Bennett, G.G.; Foley, P.; Levine, E.; Whiteley, J.; Askew, S.; Steinberg, D.M.; Batch, B.; Greaney, M.L.; Miranda, H.; Wroth, T.H.; et al. Behavioral treatment for weight gain prevention among black women in primary care practice: A randomized clinical trial. JAMA Intern. Med. 2013, 173, 1770–1777. [Google Scholar] [CrossRef]
- Bennett, G.G.; Herring, S.J.; Puleo, E.; Stein, E.K.; Emmons, K.M.; Gillman, M.W. Web-based weight loss in primary care: A randomized controlled trial. Obesity 2010, 18, 308–313. [Google Scholar] [CrossRef]
- Kay, M.C.; Burroughs, J.; Askew, S.; Bennett, G.G.; Armstrong, S.; Steinberg, D.M. Digital weight loss intervention for parents of children being treated for obesity: A prospective cohort feasibility trial. J. Med. Internet Res. 2018, 20, e11093. [Google Scholar] [CrossRef]
- Foley, P.; Steinberg, D.; Levine, E.; Askew, S.; Batch, B.C.; Puleo, E.M.; Svetkey, L.P.; Bosworth, H.B.; DeVries, A.; Miranda, H.; et al. Track: A randomized controlled trial of a digital health obesity treatment intervention for medically vulnerable primary care patients. Contemp. Clin. Trials 2016, 48, 12–20. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action; SAGE: Englewood Cliffs, NJ, USA, 1986; pp. 23–28. [Google Scholar]
- Dietary Guidelines for Americans, 2020–2025; December 2020. Available online: https://www.dietaryguidelines.gov (accessed on 29 December 2020).
- Kroenke, K.; Strine, T.W.; Spitzer, R.L.; Williams, J.B.; Berry, J.T.; Mokdad, A.H. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 2009, 114, 163–173. [Google Scholar] [CrossRef]
- Hager, E.R.; Quigg, A.M.; Black, M.M.; Coleman, S.M.; Heeren, T.; Rose-Jacobs, R.; Cook, J.T.; de Cuba, S.A.E.; Casey, P.H.; Chilton, M.; et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010, 1, e26–e32. [Google Scholar] [CrossRef]
- Steinberg, D.M.; Levine, E.L.; Lane, I.; Askew, S.; Foley, P.B.; Puleo, E.; Bennett, G.G. Adherence to self-monitoring via interactive voice response technology in an eHealth intervention targeting weight gain prevention among Black women: Randomized controlled trial. J. Med. Internet Res. 2014, 16, e114. [Google Scholar] [CrossRef]
- Vincze, G.; Barner, J.C.; Lopez, D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ. 2004, 30, 112–125. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health Ment. Health Serv. Res. 2015, 42, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 9, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Thompson, F.E.; Kipnis, V.; Midthune, D.; Hurwitz, P.; McNutt, S.; McIntosh, A.; Rosenfeld, S. Comparative Validation of the Block, Willett, and National Cancer Institute Food Frequency Questionnaires: The Eating at America’s Table Study. Am. J. Epidemiol. 2001, 154, 1089–1099. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health, National Cancer Institute. Dietary Assessment Primer, Summary Tables: Recommendations on Potential Approaches to Dietary Assessment for Different Research Objectives Requiring Group-level Estimates. Available online: https://dietassessmentprimer.cancer.gov/approach/table.html#intake (accessed on 14 July 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Power, J.M.; Bersamin, A. A Text Messaging Intervention (Txt4HappyKids) to Promote Fruit and Vegetable Intake Among Families With Young Children: Pilot Study. JMIR Form. Res. 2018, 2, e13. [Google Scholar] [CrossRef]
- Brown, C.; Davis, K.E.; Habiba, N.; Massey-Stokes, M.; Warren, C. Parent preferences for text messages containing infant feeding advice. Mhealth 2020, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, Present, and Future of eHealth and mHealth Research to Improve Physical Activity and Dietary Behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228.e1. [Google Scholar] [CrossRef]
- Thorn, B.; Kline, N.; Tadler, C.; Budge, E.; Wilcox-Cook, E.; Michaels, J.; Mendelson, M.; Patlan, K.; Tran, V. WIC Participant and Program Characteristics 2016. 2018. Available online: https://fns-prod.azureedge.net/sites/default/files/ops/WICPC2016.pdf (accessed on 19 September 2018).
- Nestor, B.; McKenzie, J.; Hasan, N.; AbuSabha, R.; Achterberg, C. Client satisfaction with the nutrition education component of the California WIC program. J. Nutr. Educ. 2001, 33, 83–94. [Google Scholar] [CrossRef]
- Wardle, J.; Parmenter, K.; Waller, J. Nutrition knowledge and food intake. Appetite 2000, 34, 269–275. [Google Scholar] [CrossRef]
- Harnack, L.; Block, G.; Subar, A.; Lane, S.; Brand, R. Association of cancer prevention-related nutrition knowledge, beliefs, and attitudes to cancer prevention dietary behavior. J. Am. Diet. Assoc. 1997, 97, 957–965. [Google Scholar] [CrossRef]
- Blaylock, J.; Variyam, J.N.; Lin, B.-H. Maternal Nutrition Knowledge and Children’s Diet Quality and Nutrient Intakes; United States Department of Agriculture, ERS: Washington DC, USA, 1999. [Google Scholar]
- Bandura, A. Social Foundations of Thought And Action: A Social Cognitive Theory; Prentice-Hall: Hoboken, NJ, USA, 1986. [Google Scholar]
- Baranowski, T.; Lin, L.S.; Wetter, D.W.; Resnicow, K.; Hearn, M.D. Theory as mediating variables: Why aren’t community interventions working as desired? Ann. Epidemiol. 1997, 7 (Suppl. 7), S89–S95. [Google Scholar] [CrossRef]
- Contento, I.; Balch, G.I.; Bronner, Y.L.; Lytle, L.A.; Maloney, S.K.; Olson, C.M.; Swadener, S.S. The effectiveness of nutrition education and implications for nutrition education policy, programs, and research: A review of research. J. Nutr. Educ. 1995, 27, 284–481. [Google Scholar]
- Head, K.J.; Noar, S.M.; Iannarino, N.T.; Grant Harrington, N. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc. Sci. Med. 2013, 97, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Fitts Willoughby, J.; Furberg, R. Underdeveloped or underreported? Coverage of pretesting practices and recommendations for design of text message-based health behavior change interventions. J. Health Commun. 2015, 20, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Donkin, L.; Christensen, H.; Naismith, S.L.; Neal, B.; Hickie, I.B.; Glozier, N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 2011, 13, e52. [Google Scholar] [CrossRef] [PubMed]
- Kreuter, M.W.; Wray, R.J. Tailored and targeted health communication: Strategies for enhancing information relevance. Am. J. Health Behav. 2003, 27 (Suppl. 3), S227–S232. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and Promoting Effective Engagement With Digital Behavior Change Interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef]
- Mohr, D.C.; Cuijpers, P.; Lehman, K. Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011, 13, e30. [Google Scholar] [CrossRef]
- Cobos-Campos, R.; Mar, J.; Apiñaniz, A.; de Lafuente, A.S.; Parraza, N.; Aizpuru, F.; Orive, G. Cost-effectiveness analysis of text messaging to support health advice for smoking cessation. Cost Eff. Resour. Alloc. 2021, 19, 9. [Google Scholar] [CrossRef]
- Armanasco, A.A.; Miller, Y.D.; Fjeldsoe, B.S.; Marshall, A.L. Preventive Health Behavior Change Text Message Interventions: A Meta-analysis. Am. J. Prev. Med. 2017, 52, 391–402. [Google Scholar] [CrossRef]
- Cole-Lewis, H.; Kershaw, T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol. Rev. 2010, 32, 56–69. [Google Scholar] [CrossRef]
- Fjeldsoe, B.S.; Marshall, A.L.; Miller, Y.D. Behavior change interventions delivered by mobile telephone short-message service. Am. J. Prev. Med. 2009, 36, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Biden-Harris Administration. National Strategy On Hunger, Nutrition, And Health. 2022. Available online: https://www.whitehouse.gov/wp-content/uploads/2022/09/White-House-National-Strategy-on-Hunger-Nutrition-and-Health-FINAL.pdf (accessed on 25 November 2022).
- Bentley, M.E.; Johnson, S.L.; Wasser, H.; Creed-Kanashiro, H.; Shroff, M.; Fernandez Rao, S.; Cunningham, M. Formative research methods for designing culturally appropriate, integrated child nutrition and development interventions: An overview. Ann. N. Y. Acad. Sci. 2014, 1308, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Arain, M.; Campbell, M.J.; Cooper, C.L.; Lancaster, G.A. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med. Res. Methodol. 2010, 10, 67. [Google Scholar] [CrossRef] [PubMed]
- Kupis, J.; Johnson, S.; Hallihan, G.; Olstad, D.L. Assessing the Usability of the Automated Self-Administered Dietary Assessment Tool (ASA24) among Low-Income Adults. Nutrients 2019, 11, 132. [Google Scholar] [CrossRef] [PubMed]
| Week | WIC-Approved Food | Goal |
|---|---|---|
| 1, 2 | Fruit | Eat 2 fruits or more each day. |
| 3, 4 | Vegetables | Eat 3 vegetables or more each day. |
| 5, 6 | Legumes | Eat beans 2 times or more each week. |
| 7, 8 | 100% whole wheat bread, tortillas, pasta, cereal | Eat 3 or more whole grains each day. |
| 9, 10 | Legumes | Eat nuts or peanut butter 3 times or more each week. |
| 11, 12 | Vegetables | Eat leafy green vegetables 2 times or more each week. |
| Characteristic | N (%) or M (SD) | |
|---|---|---|
| Caregiver Age, years | 31.1 (7.7) | |
| Caregiver BMI, kg/m2 | 33.8 (9.7) | |
| Relationship to child | Mother | 53 (98) |
| Grandparent | 1 (2) | |
| Index Child Age, months | 11.6 (7.9) | |
| Caregiver Race and Ethnicity | Non-Hispanic white | 34 (63) |
| Non-Hispanic Black | 14 (26) | |
| Non-Hispanic two or more races | 2 (4) | |
| Hispanic | 2 (4) | |
| Did not respond | 2 (4) | |
| Education | Less than high school | 3 (6) |
| High school graduate | 17 (32) | |
| Some college/vocational | 16 (30) | |
| Associate’s degree or higher | 18 (33) | |
| Working full- or part-time/looking for work | Yes | 34 (63) |
| No | 15 (28) | |
| Did not respond | 5 (9) | |
| Married | Yes | 21 (39) |
| No | 31 (57) | |
| Did not respond | 2 (4) | |
| Caregiver with obesity | 35 (65) | |
| Household size | 3.9 (1.2) | |
| Number of children in household | 2.1 (1.0) | |
| Ever breastfed | 40 (74) | |
| Food-insecure | 24 (44) | |
| Depression | 16 (30) | |
| Characteristic | Engagement, n (%) | ||
|---|---|---|---|
| Low (<80%), n = 27 | High (≥80%), n = 27 | ||
| Caregiver Race and Ethnicity 1,2 | Non-Hispanic White | 14 (41) | 20 (59) |
| Non-Hispanic Black | 11 (79) | 3 (21) | |
| Education | ≤High school | 12 (60) | 8 (40) |
| Some college/vocational | 8 (50) | 8 (50) | |
| Associates degree or higher | 7 (39) | 11 (61) | |
| Employment 2 | No | 4 (27) | 11 (73) |
| Yes (full/part-time, looking) | 21 (62) | 13 (38) | |
| Married 2 | Yes | 6 (29) | 15 (71) |
| No | 20 (65) | 11 (35) | |
| Caregiver with obesity | Yes | 15 (43) | 20 (57) |
| No | 12 (63) | 7 (37) | |
| Food-insecure | Yes | 12 (50) | 12 (50) |
| No | 15 (50) | 15 (50) | |
| Depressed | Yes | 20 (47) | 23 (53) |
| No | 7 (64) | 4 (36) | |
| Component | Max Points | Standard for Max Score | Standard for Min Score | Baseline (n = 54) | 12-Weeks (n = 48) | Change (n = 48) |
|---|---|---|---|---|---|---|
| Food and Nutrients to Increase | ||||||
| Total Fruits 1 | 5 | ≥0.8 cup eq per 1000 kcal | No fruit | 2.0 (1.9) | 1.9 (1.9) | 0.0 (1.9) |
| Whole Fruits 2 | 5 | ≥0.4 cup eq per 1000 kcal | No whole fruit | 2.0 (2.2) | 2.1 (2.2) | 0.1 (2.3) |
| Total Vegetables | 5 | ≥1.1 cup eq per 1000 kcal | No vegetables | 2.7 (1.7) | 3.4 (1.6) | 0.5 (1.8) |
| Greens and Beans | 5 | ≥0.2 cup eq per 1000 kcal | No dark green vegetables or legumes | 1.6 (2.0) | 2.5 (2.3) | 0.8 (2.4) * |
| Whole Grains | 10 | ≥1.5 oz eq per 1000 kcal | No whole grains | 2.9 (3.5) | 3.2 (3.8) | 0.4 (4.2) |
| Dairy 3 | 10 | ≥1.3 cup eq per 1000 kcal | No dairy | 4.9 (3.1) | 5.5 (2.9) | 0.5 (3.6) |
| Total Protein Foods | 5 | ≥2.5 oz eq per 1000 kcal | No protein foods | 4.5 (1.0) | 4.6 (0.9) | 0.1 (1.0) |
| Seafood and Plant Proteins 4 | 5 | ≥0.8 oz eq per 1000 kcal | No seafood or plant proteins | 2.0 (2.1) | 2.3 (2.2) | 0.3 (2.7) |
| Fatty Acids 5 | 10 | (PUFAs + MUFAs)/SFAs ≥2.5 | (PUFAs + MUFAs)/SFAs ≤1.2 | 5.2 (3.4) | 4.7 (2.9) | −0.4 (4.1) |
| Food and Nutrients to Limit or Decrease | ||||||
| Refined Grains | 10 | ≤1.8 oz eq per 1000 kcal | ≥4.3 oz eq per 1000 kcal | 6.6 (3.3) | 6.0 (3.4) | −0.9 (4.5) |
| Sodium | 10 | ≤1.1 g per 1000 kcal | ≥2.0 g per 1000 kcal | 3.8 (2.9) | 2.5 (2.6) | −1.4 (3.9) * |
| Added Sugars | 10 | ≤6.5% of energy | ≥26% of energy | 6.3 (3.3) | 7.5 (2.6) | 1.3 (3.1)* |
| Saturated Fats | 10 | ≤8% of energy | ≥16% of energy | 5.1 (3.7) | 4.3 (3.0) | −0.5 (4.0) |
| Total Score | 100 | 49.7 (12.4) | 50.5 (13.8) | 0.8 (12.9) | ||
| Satisfaction Question | Agreement, n (%) |
|---|---|
| Overall, the feedback received on the automated text messages was helpful. | 44 (94) |
| The text messages felt personalized. | 35 (74) |
| The text messages were sent at a convenient time each day. | 42 (89) |
| I found the tips easy to understand. | 46 (98) |
| I applied the skills I learned from the tips to my routine. | 42 (89) |
| It was easy to understand my goals. | 45 (96) |
| I found the goals too difficult to meet. | 7 (15) |
| The tips helped me to meet my goals. | 41 (87) |
| I felt confident that I could follow the goals I was given. | 40 (85) |
| My goals were what I needed to work on for choosing healthy foods for me and my family. | 44 (94) |
| I think that I would like to continue to receive text messages from the Healthy Roots program. | 32 (68) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kay, M.C.; Hammad, N.M.; Truong, T.; Herring, S.J.; Bennett, G.G. Feasibility, Acceptability, and Initial Efficacy of a Digital Intervention to Improve Consumption of Foods Received within a National Nutrition Assistance Program. Nutrients 2023, 15, 438. https://doi.org/10.3390/nu15020438
Kay MC, Hammad NM, Truong T, Herring SJ, Bennett GG. Feasibility, Acceptability, and Initial Efficacy of a Digital Intervention to Improve Consumption of Foods Received within a National Nutrition Assistance Program. Nutrients. 2023; 15(2):438. https://doi.org/10.3390/nu15020438
Chicago/Turabian StyleKay, Melissa C., Nour M. Hammad, Tracy Truong, Sharon J. Herring, and Gary G. Bennett. 2023. "Feasibility, Acceptability, and Initial Efficacy of a Digital Intervention to Improve Consumption of Foods Received within a National Nutrition Assistance Program" Nutrients 15, no. 2: 438. https://doi.org/10.3390/nu15020438
APA StyleKay, M. C., Hammad, N. M., Truong, T., Herring, S. J., & Bennett, G. G. (2023). Feasibility, Acceptability, and Initial Efficacy of a Digital Intervention to Improve Consumption of Foods Received within a National Nutrition Assistance Program. Nutrients, 15(2), 438. https://doi.org/10.3390/nu15020438






