Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Course Detail
2.3. Data Collection and Statistical Analysis
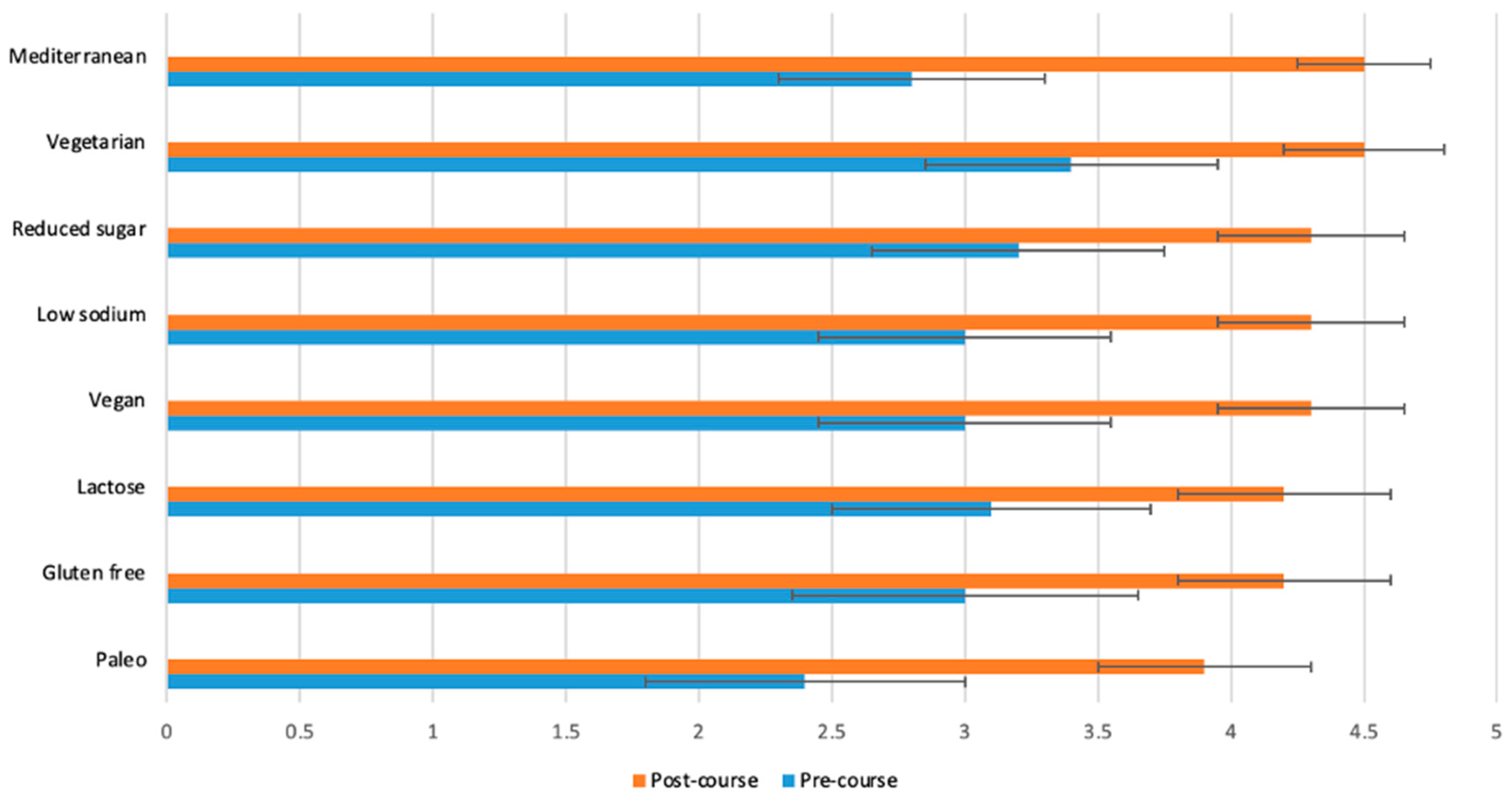
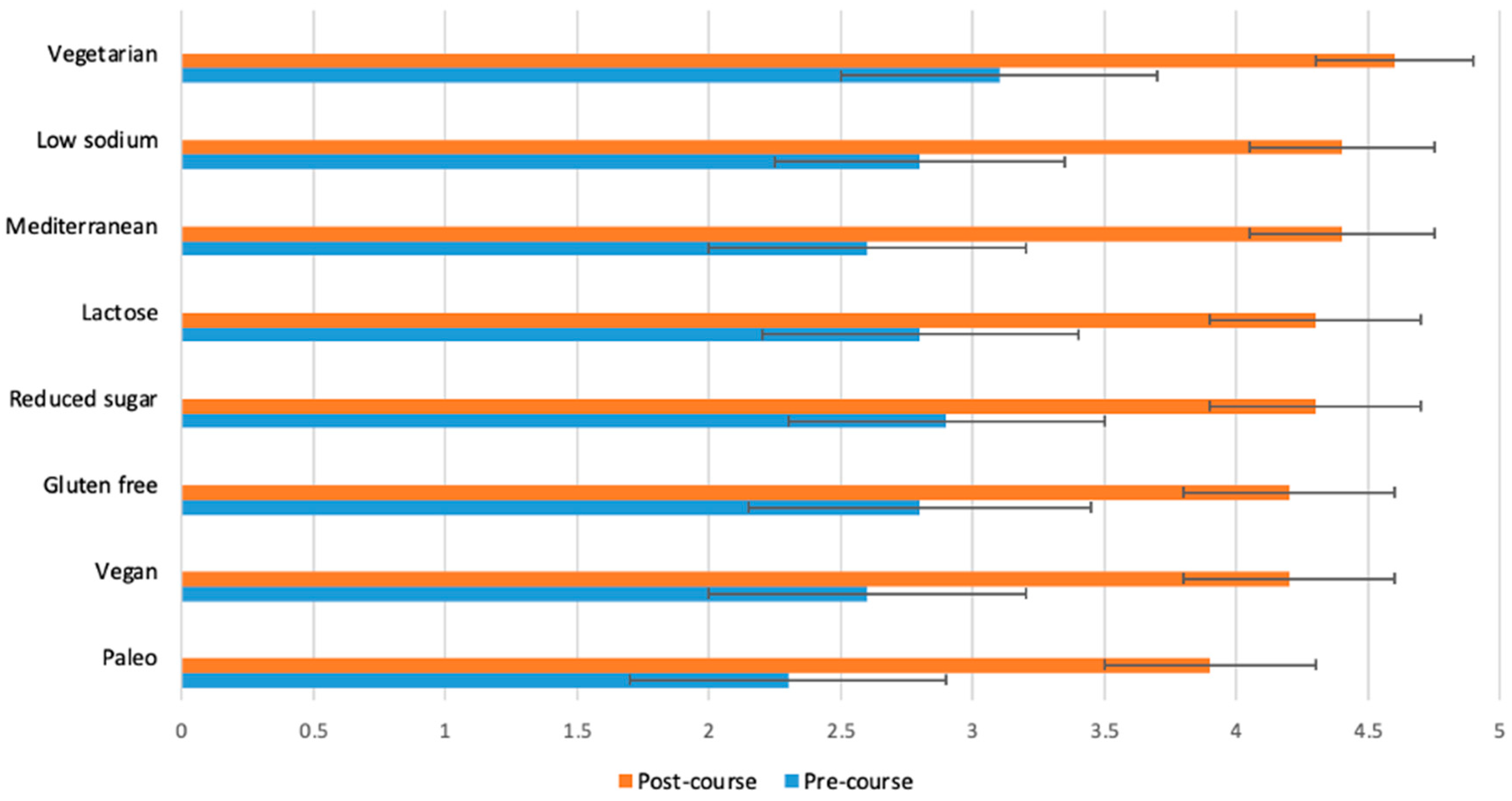
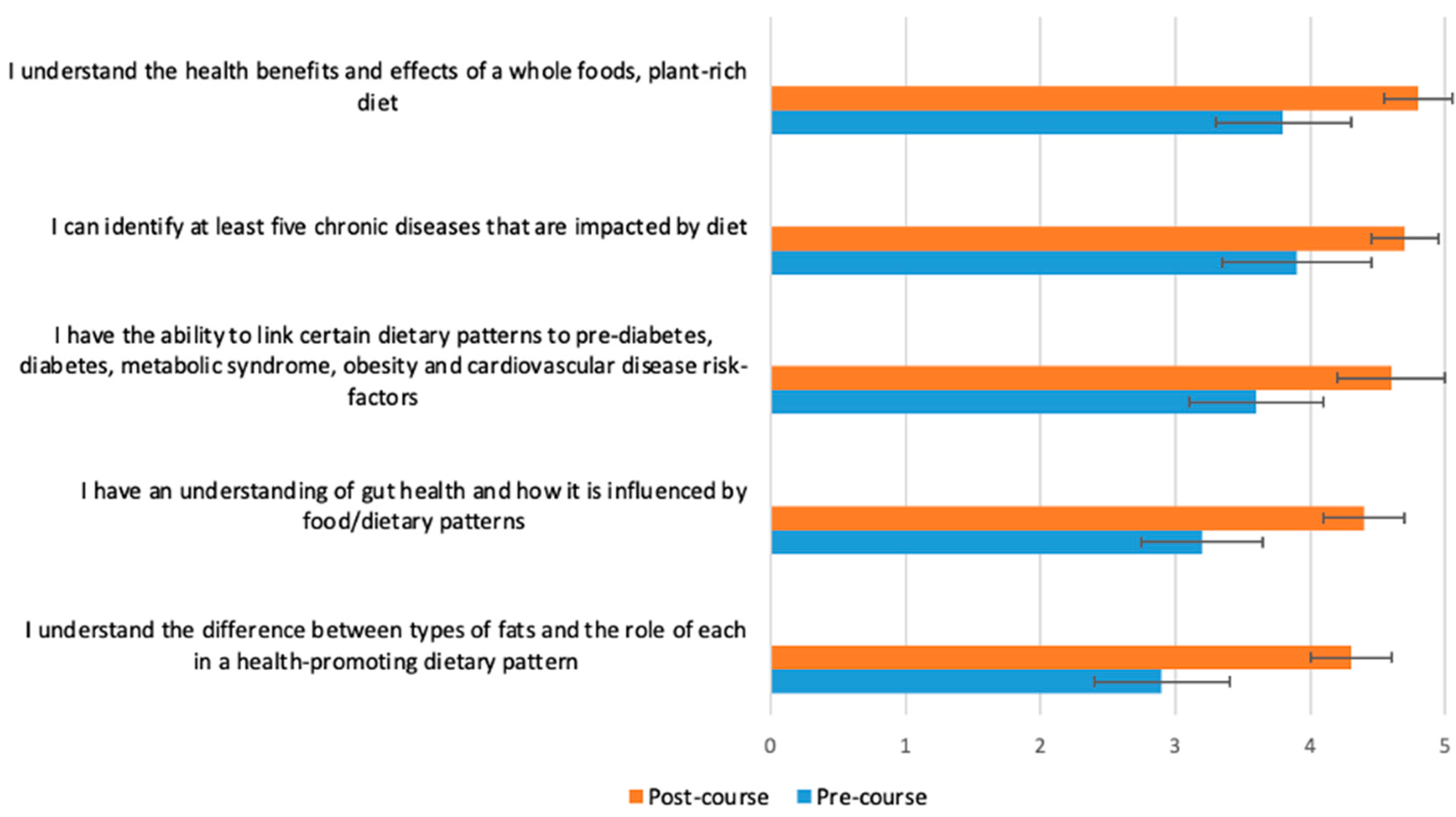
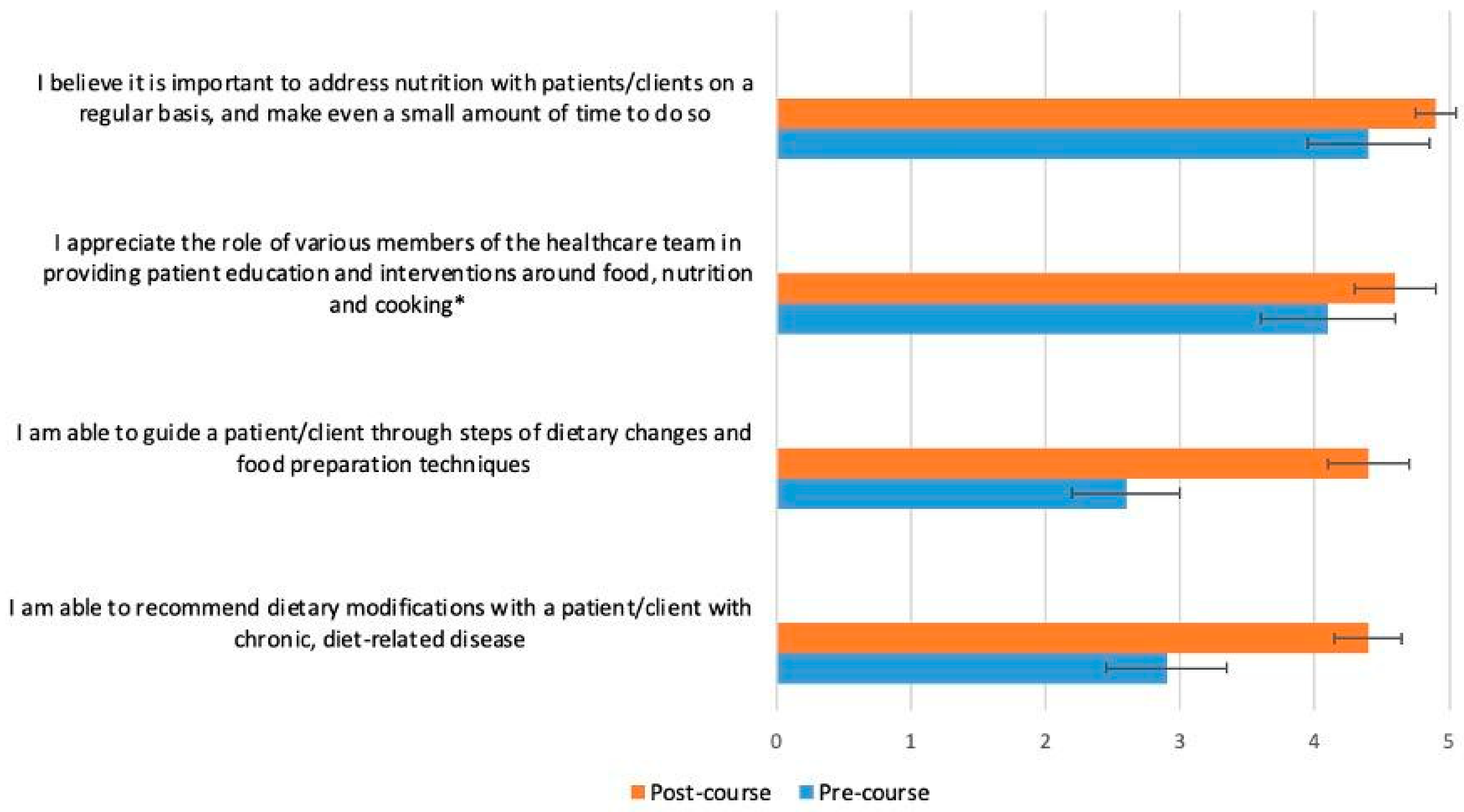
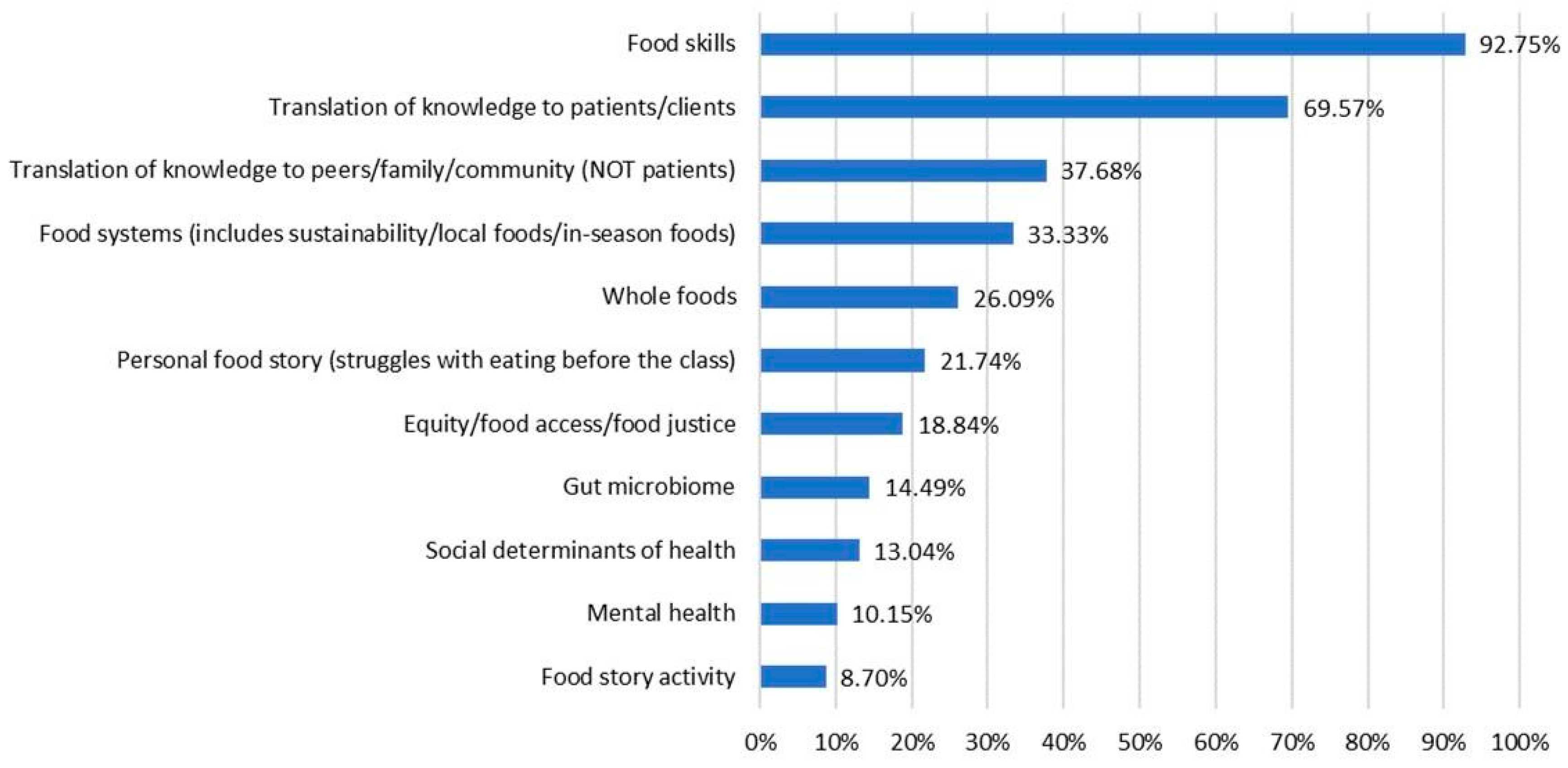
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Food Systems—OECD. Available online: https://www.oecd.org/food-systems/ (accessed on 13 August 2023).
- Nguyen, H. Sustainable Food Systems: Concept and Framework; Food and Agriculture Organization of the United Nations: Rome, Italy, 2018. [Google Scholar]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Haines, A.; Ebi, K. The Imperative for Climate Action to Protect Health. N. Engl. J. Med. 2019, 380, 263–273. [Google Scholar] [CrossRef]
- Food Product Development. Available online: https://www.ksre.k-state.edu/kvafl/development.html (accessed on 15 August 2023).
- Zheng, L.; Sun, J.; Yu, X.; Zhang, D. Ultra-Processed Food Is Positively Associated With Depressive Symptoms Among United States Adults. Front. Nutr. 2020, 7, 600449. [Google Scholar] [CrossRef]
- Menichetti, G.; Ravandi, B.; Mozaffarian, D.; Barabási, A.-L. Machine Learning Prediction of the Degree of Food Processing. Nat. Commun. 2023, 14, 2312. [Google Scholar] [CrossRef] [PubMed]
- Juul, F.; Vaidean, G.; Lin, Y.; Deierlein, A.L.; Parekh, N. Ultra-Processed Foods and Incident Cardiovascular Disease in the Framingham Offspring Study. J. Am. Coll. Cardiol. 2021, 77, 1520–1531. [Google Scholar] [CrossRef] [PubMed]
- Elizabeth, L.; Machado, P.; Zinöcker, M.; Baker, P.; Lawrence, M. Ultra-Processed Foods and Health Outcomes: A Narrative Review. Nutrients 2020, 12, 1955. [Google Scholar] [CrossRef] [PubMed]
- Byrne, C.; Kurmas, N.; Burant, C.J.; Utech, A.; Steiber, A.; Julius, M. Cooking Classes: A Diabetes Self-Management Support Intervention Enhancing Clinical Values. Diabetes Educ. 2017, 43, 600–607. [Google Scholar] [CrossRef]
- Wolfson, J.A.; Bleich, S.N. Is Cooking at Home Associated with Better Diet Quality or Weight-Loss Intention? Public Health Nutr. 2015, 18, 1397–1406. [Google Scholar] [CrossRef]
- Gregory, C.A. Food Insecurity, Chronic Disease, and Health Among Working-Age Adults. Economic Research Report, 31 July 2017. [Google Scholar]
- Rivera, R.L.; Adams, M.; Dawkins, E.; Carter, A.; Zhang, X.; Tu, W.; Peña, A.; Holden, R.J.; Clark, D.O. Delivering Food Resources and Kitchen Skills (FoRKS) to Adults with Food Insecurity and Hypertension: A Pilot Study. Nutrients 2023, 15, 1452. [Google Scholar] [CrossRef] [PubMed]
- Pooler, J.A.; Srinivasan, M.; Wong, K.; Blitstein, J.L. Food Skills Education and Low-Income Adults’ Healthy Food Choices. Community Health Equity Res. Policy 2022, 43, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Lepre, B.; Mansfield, K.J.; Ray, S.; Beck, E.J. Nutrition Competencies for Medicine: An Integrative Review and Critical Synthesis. BMJ Open 2021, 11, e043066. [Google Scholar] [CrossRef] [PubMed]
- Teaching Kitchen Collaborative Research Day Abstracts. The Estate Yountville, Napa Valley, CA, USA February 7, 2018 A Day of Original Research and Innovative Strategies Involving Teaching Kitchens and Their Potential to Positively Impact Behaviors, Improve Health Outcomes, and Reduce Costs. J. Altern. Complement. Med. 2018, 24, A1–A21. [CrossRef]
- Kibakaya, E.C.; Oyeku, S.O. Cultural Humility: A Critical Step in Achieving Health Equity. Pediatrics 2022, 149, e2021052883. [Google Scholar] [CrossRef] [PubMed]
- Nasreddine, L.; Shatila, H.; Itani, L.; Hwalla, N.; Jomaa, L.; Naja, F. A Traditional Dietary Pattern Is Associated with Lower Odds of Overweight and Obesity among Preschool Children in Lebanon: A Cross-Sectional Study. Eur. J. Nutr. 2019, 58, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Why Traditional Diets? Available online: https://oldwayspt.org/traditional-diets/why-traditional-diets (accessed on 23 August 2023).
- Kromhout, D.; Menotti, A.; Alberti-Fidanza, A.; Puddu, P.E.; Hollman, P.; Kafatos, A.; Tolonen, H.; Adachi, H.; Jacobs, D.R. Comparative Ecologic Relationships of Saturated Fat, Sucrose, Food Groups, and a Mediterranean Food Pattern Score to 50-Year Coronary Heart Disease Mortality Rates among 16 Cohorts of the Seven Countries Study. Eur. J. Clin. Nutr. 2018, 72, 1103–1110. [Google Scholar] [CrossRef] [PubMed]
- “Confidence”. Available online: https://dictionary.cambridge.org/us/dictionary/english/confidence (accessed on 6 September 2023).
- Crowley, J.; Ball, L.; Hiddink, G.J. Nutrition in Medical Education: A Systematic Review. Lancet Planet. Health 2019, 3, e379–e389. [Google Scholar] [CrossRef] [PubMed]
- Rep. McGovern, J.P. [D-M.-2 Text—H.Res.1118—117th Congress (2021–2022): Expressing the Sense of the House of Representatives That the United States Recognizes the Mounting Personal and Financial Burden of Diet-Related Disease in the United States and Calls on Medical Schools, Graduate Medical Education Programs, and Other Health Professional Training Programs to Provide Meaningful Physician and Health Professional Education on Nutrition and Diet. Available online: http://www.congress.gov/bill/117th-congress/house-resolution/1118/text (accessed on 23 August 2023).

| Variable | Characteristic | Frequency | Percent (%) | |
|---|---|---|---|---|
| Role | Student | 51 | 78.5 | |
| Both | 12 | 18.5 | ||
| Clinician | 2 | 3.1 | ||
| Gender | Female | 60 | 92.3 | |
| Male | 5 | 7.7 | ||
| Program of study or clinical area | Doctor of Nursing Practice | 18 | 27.7 | |
| Integrative Health and Healing | 9 | 13.8 | ||
| Family Nurse Practitioner | 4 | 6.2 | ||
| Specialty not specified | 4 | 6.2 | ||
| Psychiatry | 1 | 1.5 | ||
| Public Health | 10 | 15.4 | ||
| Healthcare Administration | 3 | 4.6 | ||
| Nutrition/Dietetics | 3 | 4.6 | ||
| Community Health Promotion | 1 | 1.5 | ||
| Epidemiology | 1 | 1.5 | ||
| Maternal and Child Health | 1 | 1.5 | ||
| Specialty not specified | 1 | 1.5 | ||
| Pharmacy | 9 | 13.8 | ||
| Integrative Health and Wellbeing Coaching | 6 | 9.2 | ||
| Health Coaching | 3 | 4.6 | ||
| Family Nurse Practitioner | 2 | 3.1 | ||
| Integrative Health and Healing | 2 | 3.1 | ||
| Nursing | 2 | 3.1 | ||
| Women’s Health | 2 | 3.1 | ||
| Health and Wellbeing Sciences | 1 | 1.5 | ||
| Integrative and Functional Medicine | 1 | 1.5 | ||
| Medical Student | 1 | 1.5 | ||
| Nutrition | 1 | 1.5 | ||
| Occupational Therapy | 2 | 3.1 | ||
| Oncology | 1 | 1.5 | ||
| Psychology | 1 | 1.5 | ||
| Senior Citizen Education | 1 | 1.5 | ||
| Unknown | 1 | 1.5 | ||
| Youth Development Leadership | 1 | 1.5 | ||
| Mean | SD | |||
| If clinician, number of years in practice | 13 | 9.9 | ||
| Week | Course Content |
|---|---|
| Week 1 | Introductions; Food Story; culinary basics including knife skills, salad dressing formula, dry heat cooking methods, use of seasonal and local ingredients; overview of local/regional and global food systems and their relationships to health and social/structural determinants of health. |
| Week 2 | Overview of digestive physiology; mindful eating in practice; overview of macronutrients; comparison of food plates/graphics; Western dietary pattern and chronic disease relationships; incorporating whole grains, legumes and vegetables into a variety of recipes; moist heat cooking methods. |
| Week 3 | Quality and sources of macronutrients, dietary patterns and metabolic syndrome; case examples; functions of fat in culinary and nutritional context; soups/stews formula, nutrient-dense dessert examples. |
| Week 4 | Gut microbiome foundations, influence of diet on gut health, dietary pattern influence on gut health/mental health/gut–brain axis; food and inflammation; identifying, preparing and incorporating fermented foods. |
| Week 5 | Cost and time considerations, building a pantry, budgeting, using leftovers; examining literature around popular dietary patterns; the animal protein flip, food preservation techniques, build-a-bowl formula. |
| Week 6 | Final group case presentations and peer teaching opportunity, application to professional practice, personal and group reflection. |
| Course Learning Objectives | |
| 1. | Describe and assess the interconnections between environmental, cultural, economic, social, nutritional and personal issues within the food system as it relates to production, processing, purchasing, consumption and food choices. |
| 2. | Demonstrate an understanding of the diversity of perspectives of various participants in the food system and critically evaluate information with an understanding of these various perspectives. |
| 3. | Critically examine personal cultural perspectives and roles in the food system, both professionally and personally, and describe opportunities for public engagement in issues of personal importance. |
| 4. | Demonstrate basic cooking skills, including troubleshooting and problem solving in the context of meal preparation. |
| 5. | Demonstrate a working understanding of basic nutritional and food safety guidelines. |
| 6. | Create weekly/monthly menus within a realistic food budget. |
| 7. | Demonstrate how to adapt and create nutritionally balanced meals within a variety of constraints (e.g., using available ingredients, budget constraints, and dietary and cultural preferences, etc.). |
| Theme | Quote |
|---|---|
| Food skills | The cooking skills and practices made me a lot more comfortable in the kitchen and broadened my horizons on what foods to cook. |
| Translation of knowledge to patients or clients | While I know what foods are generally healthy, I didn’t have a good understanding of how I could help patients with their nutrition. This class gave me the opportunity to focus on just that, and I feel better equipped to discuss diet and nutrition with my future patients. One of the main lessons I took away from this course was how to meet your patients where they are at, and see what small adjustments the patient is comfortable with. |
| Translation of knowledge to peers, family, or community (NOT patients) | I think that this class was helpful in reaffirming my attitude towards medication, and it will allow me to be an advocate for diet/lifestyle modifications within the pharmacy community. |
| Food systems (includes sustainability, local foods, and in-season foods) | Due to this expansion in my understanding, I now have a greater awareness of figuring out the true source of the organic food products I am purchasing. “Was it grown locally?” “How far did it have to travel from farm to store?” These are some of the questions I now ask myself while grocery shopping. |
| Whole foods | My first takeaway is the emphasis on whole foods and how that benefits health. |
| Personal food story (struggles with eating before the class) | Another lesson that resonated with me was how oversimplified calories in/calories out is. I have struggled with my weight in the past and have always bought into the notion that calorie restriction was really the only way to lose weight. I think it really comes down to the idea that losing weight and eating/being healthy are two very different things. |
| Equity, food access, and food justice | I am grateful this class allowed and fostered a space to discuss inequities and inequalities in our food systems. |
| Gut microbiome | Secondly, our discussions and lessons on how to maintain a healthy gut were so great! It is very cool to see more and more research about how important it is to maintain, how it changes over time, and how it differs from person to person. I do notice that when I eat well and eat fermented food regularly, my gut is happier! |
| Social determinants of health | The class highlighted that eating healthy isn’t exactly difficult. However, there are many factors that may contribute towards an individual making poor food decisions. Stress, access to healthy grocers, financial resources, and health literacy are just a few reasons for bad eating habits. It can be very easy to recommend foods to a patient, however it can be very difficult to address all factors that may contribute to a person or family’s difficulty in eating healthy. |
| Mental health | Utilizing the resources for gut health, the microbiome and inflammation connection as well as the link between real food and brain health are also key elements to bring to my coaching practice when working with clients contending with inflammatory and mental health issues. |
| Food story activity | We have discussed mindful eating in my coursework already, but it was very helpful to remember the elements and also experience it for myself to speak to clients about my own experience around it. I am looking forward to adding the Food Mood diary and the Food Story into my coaching toolbox to use with clients. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shafto, K.; Vandenburgh, N.; Wang, Q.; Breen, J. Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals. Nutrients 2023, 15, 3994. https://doi.org/10.3390/nu15183994
Shafto K, Vandenburgh N, Wang Q, Breen J. Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals. Nutrients. 2023; 15(18):3994. https://doi.org/10.3390/nu15183994
Chicago/Turabian StyleShafto, Katherine, Natalie Vandenburgh, Qi Wang, and Jenny Breen. 2023. "Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals" Nutrients 15, no. 18: 3994. https://doi.org/10.3390/nu15183994
APA StyleShafto, K., Vandenburgh, N., Wang, Q., & Breen, J. (2023). Experiential Culinary, Nutrition and Food Systems Education Improves Knowledge and Confidence in Future Health Professionals. Nutrients, 15(18), 3994. https://doi.org/10.3390/nu15183994