Influence of Occupational Stress on the Body Mass Index of Hospital Workers: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria and Search Strategy
2.3. Study Selection and Data Extraction
2.4. Analysis of Methodological Quality, Risk of Bias and Certainty of Evidence
2.5. Data Synthesis Strategy
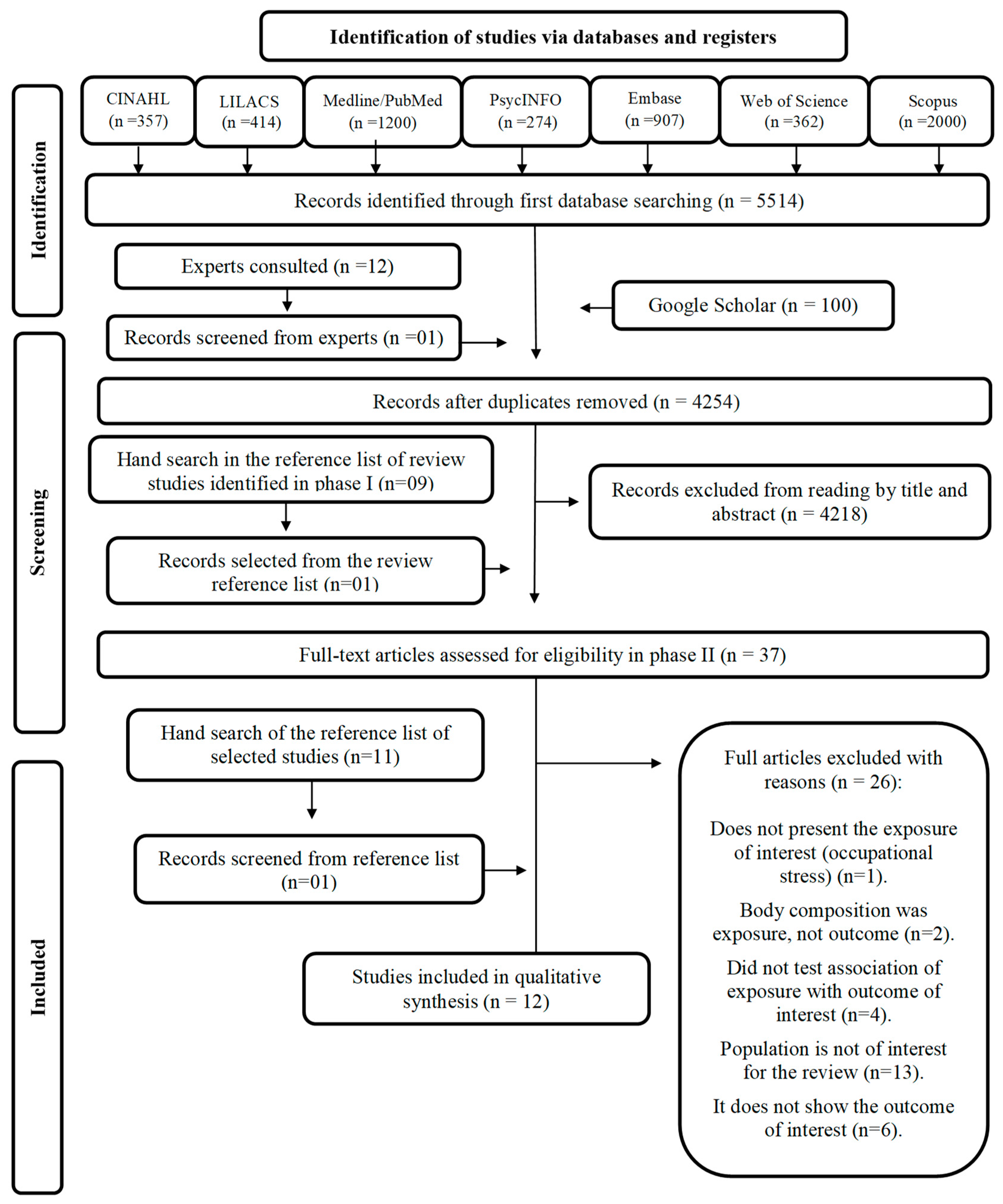
2.6. Selection Process
2.7. Characteristics of the Studies
2.8. Assessment of Occupational Stress and Body Composition
3. Results
3.1. Individual Study Results
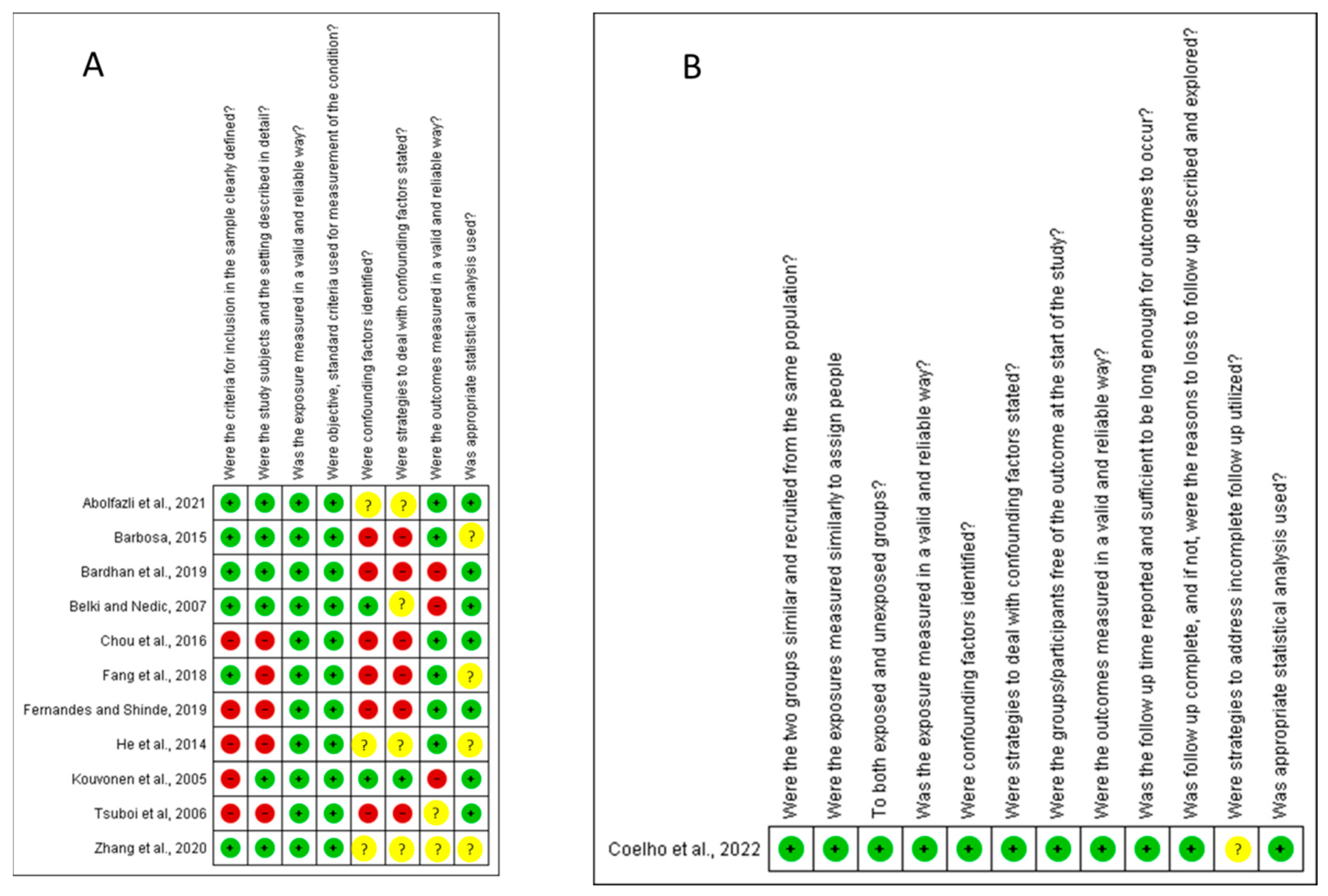
3.2. Assessment of Risk of Bias, Methodological Quality and Assessment of the Certainty of the Evidence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Labour Office. Workplace Stress: A Collective Challenge; ILO: Geneva, Switzerland, 2016. [Google Scholar]
- Ribeiro, R.P.; Marziale, M.H.P.; Martins, J.T.; Galdino, M.J.Q.; Ribeiro, P.H.V. Estresse ocupacional entre trabalhadores de saúde de um hospital universitário. Rev. Gauch. Enferm. 2018, 39, e65127. [Google Scholar] [CrossRef] [PubMed]
- Souza, M.P.G.; Sampaio, R.; Cavalcante, A.C.M.; Arruda, S.P.M.; Pinto, F.J.M. Comportamento alimentar e fatores associados em servidores: Contribuições para a saúde coletiva. Rev. Atenção à Saúde 2020, 18, 63. [Google Scholar] [CrossRef]
- Jung, H.; Dan, H.; Pang, Y.; Kim, B.; Jeong, H.; Lee, J.E.; Kim, O. Association between Dietary Habits, Shift Work, and the Metabolic Syndrome: The Korea Nurses’ Health Study. Int. J. Environ. Res. Public Health 2020, 17, 7697. [Google Scholar] [CrossRef] [PubMed]
- Tabing, E.V.P.; Atienza, L.M.; Africa, L.S.; Santos, R.A.B. Work Stress, Dietary Intake, and Nutritional Status of Night-Shift Call Center Employees in Lipa City, Batangas, Philippines. J. Nutr. Res. Food Sci. Res. 2020, 1, 1–22. [Google Scholar]
- Tawiah, P.A.; Baffour-Awuah, A.; Appiah-Brempong, E.; Afriyie-Gyawu, E. Identifying occupational health hazards among healthcare providers and ancillary staff in Ghana: A scoping review protocol. BMJ Publishing Group 2022, 12, e058048. [Google Scholar] [CrossRef]
- Kunyahamu, M.S.; Daud, A.; Jusoh, N. Obesity among Health-Care Workers: Which Occupations Are at Higher Risk of Being Obese? Int. J. Environ. Res. Public Health 2021, 18, 4381. [Google Scholar] [CrossRef]
- Moizuddin, K.M.; Sami, L.B.; Talib, S.H.; Dase, R.K. Prevalence of Occupational Stress among Doctors of Aurangabad city [MS], India. Int. J. Curr. Med. Appl. Sci. 2016, 11, 60–64. Available online: www.ijcmaas.com (accessed on 23 February 2023).
- Nguyen, A.N.; Nguyen, L.N.; Hoang, P.V.; Le, X.T.T. A Review of Occupational Stress among Certain Jobs in Vietnam. Res. Health Sci. 2019, 4, 258. [Google Scholar] [CrossRef]
- Ennis, S.A. What is the Prevalence of Occupational Stress among Post-Primary Teachers in Ireland? Institute of Technology: Carlow, Ireland, 2019. [Google Scholar]
- Illangasinghe, D.K.; Alagiyawanna, M.A.A.P.; Samaranayake, D.B.D.L.; Fernando, N. Prevalence and associated factors of occupational stress among bus drivers of Sri Lanka Transport Board in Colombo District. J. Coll. Community Physicians Sri Lanka 2021, 27, 411. [Google Scholar] [CrossRef]
- Lima, V.V.R.d.S.S.; Bádue, G.S.; Araújo, J.F.d.S.; Moraes, M.d.O.; Costa, C.R.B.; Martins-Filho, P.R.; de Moura, T.R. Estresse ocupacional dos profissionais de enfermagem durante a pandemia de COVID-19 no Brasil. Res. Soc. Dev. 2021, 10, e24410152202. [Google Scholar] [CrossRef]
- Girma, B.; Nigussie, J.; Molla, A.; Mareg, M. Occupational stress and associated factors among health care professionals in Ethiopia: A systematic review and meta-analysis. BMC Public Health 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Ibrahim, M.A.; Aziz, A.A.; Suhaili, N.-A.; Daud, A.Z.; Naing, L.; Rahman, H.A. A Study into Psychosocial Work Stressors and Health Care Productivity. Int. J. Occup. Environ. Med. 2019, 10, 185–193. [Google Scholar] [CrossRef]
- Dutheil, F.; Pereira, B.; Bouillon-Minois, J.-B.; Clinchamps, M.; Brousses, G.; Dewavrin, S.; Cornet, T.; Mermillod, M.; Mondillon, L.; Baker, J.S.; et al. Validation of Visual Analogue Scales of job demand and job control at the workplace: A cross-sectional study. BMJ Open 2022, 12, e046403. [Google Scholar] [CrossRef]
- Li, J.; Riedel, N.; Barrech, A.; Herr, R.M.; Aust, B.; Mörtl, K.; Siegrist, J.; Gündel, H.; Angerer, P. Long-Term Effectiveness of a Stress Management Intervention at Work: A 9-Year Follow-Up Study Based on a Randomized Wait-List Controlled Trial in Male Managers. BioMed Res. Int. 2017, 2017, 1–11. [Google Scholar] [CrossRef]
- Hwang, W.J.; Kim, M. Work-Related Stress, Health Status, and Status of Health Apps Use in Korean Adult Workers. Int. J. Environ. Res. Public Health 2022, 19, 3197. [Google Scholar] [CrossRef]
- Pena-Gralle, A.P.B.; Talbot, D.; Duchaine, C.S.; Lavigne-Robichaud, M.; Trudel, X.; Aubé, K.; Gralle, M.; Gilbert-Ouimet, M.; Milot, A.; Brisson, C. Job strain and effort-reward imbalance as risk factors for type 2 diabetes mellitus: A systematic review and meta-analysis of prospective studies. Scand. J. Work Environ. Health 2021, 48, 5–20. [Google Scholar] [CrossRef]
- Mahanta, J.; Medhi, G.; Hazarika, N.; Shah, B. Study of health problems and nutritional status of tea garden population of Assam. Indian J. Med. Sci. 2006, 60, 496–505. [Google Scholar] [CrossRef]
- Kawaharada, M.; Saijo, Y.; Yoshioka, E.; Sato, T.; Sato, H.; Kishi, R. Relations of Occupational Stress to Occupational Class in Japanese Civil Servants-Analysis by Two Occupational Stress Models. Ind. Health 2007, 45, 247–255. [Google Scholar] [CrossRef]
- Goetzel, R.Z.; Gibson, T.B.; Short, M.E.; Chu, B.-C.P.; Waddell, J.; Bowen, J.; Lemon, S.C.; Fernandez, I.D.; Ozminkowski, R.J.; Wilson, M.G.H.; et al. A Multi-Worksite Analysis of the Relationships Among Body Mass Index, Medical Utilization, and Worker Productivity. J. Occup. Environ. Med. 2010, 52 (Suppl. S1), S52–S58. [Google Scholar] [CrossRef]
- Li, W.; Yi, G.; Chen, Z.; Dai, X.; Wu, J.; Peng, Y.; Ruan, W.; Lu, Z.; Wang, D. Is job strain associated with a higher risk of type 2 diabetes mellitus? A systematic review and meta-analysis of prospective cohort studies. Scand. J. Work Environ. Health 2021, 47, 249–257. [Google Scholar] [CrossRef]
- Kivimäki, M.; Singh-Manoux, A.; Nyberg, S.; Jokela, M.; Virtanen, M. Job strain and risk of obesity: Systematic review and meta-analysis of cohort studies. Int. J. Obes. 2015, 39, 1597–1600. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, R.P.; Ribeiro, P.H.V.; Marziale, M.H.P.; Martins, M.B.; Santos, M.R.D. Obesidade e estresse entre trabalhadores de diversos setores de produção: Uma revisão integrativa. Acta Paul. Enferm. 2011, 24, 577–581. [Google Scholar] [CrossRef]
- Okuhara, M.; Sato, K.; Kodama, Y. The nurses’ occupational stress components and outcomes, findings from an integrative review. Nurs. Open 2021, 8, 2153–2174. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Glasziou, P.; Chalmers, I.; Nasser, M.; Bossuyt, P.M.M.; Korevaar, D.A.; Graham, I.D.; Ravaud, P.; Boutron, I. Increasing value and reducing waste in biomedical research: Who’s listening? Lancet 2015, 387, 1573–1586. [Google Scholar] [CrossRef] [PubMed]
- Booth, A.; Clarke, M.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. Comment An international registry of systematic-review protocols. Lancet 2011, 377, 108–109. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Sharmin, S.; Kypri, K.; Khanam, M.; Wadolowski, M.; Bruno, R.; Mattick, R.P. Parental Supply of Alcohol in Childhood and Risky Drinking in Adolescence: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2017, 14, 287. [Google Scholar] [CrossRef]
- Canto, G.d.L.; Stefani, C.M.; Massignan, C. Risco de Viés em Revisões Sistemáticas—Guia Prático; Brazil Publishing: Curitiba, Brazil, 2021; Volume 1. [Google Scholar]
- Guyatt, G.H.; Oxman, A.D.; Schuenemann, H.J.; Tugwell, P.; Knottnerus, A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J. Clin. Epidemiol. 2011, 64, 380–382. [Google Scholar] [CrossRef]
- Manheimer, E. Summary of Findings Tables: Presenting the Main Findings of Cochrane Complementary and Alternative Medicine-related Reviews in a Transparent and Simple Tabular Format. Glob. Adv. Health Med. 2012, 1, 90–91. Available online: www.gahmj.com (accessed on 23 February 2023).
- Higgins, J.P.; Thomas, J.; Chandler, J. Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2 (Updated February 2021); 2021; Available online: https://training.cochrane.org/handbook (accessed on 23 February 2023).
- Abolfazli, M.; Akbari, M.; Cheraghi, L.; Abbasinia, M.; Gaeeni, M.; Aghaiei, B. Assessment of Job Stress Level in Nurses with Overweight and Obesity and Its Relationship With Demographic Factors. Qom. Univ. Med. Sci. J. 2021, 15, 264–271. [Google Scholar] [CrossRef]
- Zhang, Z.; Lu, Y.; Yong, X.; Li, J.; Liu, J. Effects of Occupational Radiation Exposure on Job Stress and Job Burnout of Medical Staff in Xinjiang, China: A Cross-Sectional Study. Experiment 2020, 27, e927848-1. [Google Scholar] [CrossRef]
- Kouvonen, A.; Kivimäki, M.; Cox, S.J.; Cox, T.; Vahtera, J. Relationship Between Work Stress and Body Mass Index Among 45,810 Female and Male Employees. Psychosom. Med. 2005, 67, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Coelho, L.G.; Costa, P.R.d.F.; Kinra, S.; Mallinson, P.A.C.; Akutsu, R.d.C.C.d.A. Association between occupational stress, work shift and health outcomes in hospital workers of the Recôncavo of Bahia, Brazil: The impact of COVID-19 pandemic. Br. J. Nutr. 2022, 129, 147–156. [Google Scholar] [CrossRef]
- Barbosa, B.F.d.S. Associação Entre as Atividades Desenvolvidas e os Fatores de Risco para Doenças Cardiovasculares de Enfermeiros de um Hospital Universitário; Universidade do Estado do Rio de Janeiro: Rio de Janeiro, Brazil, 2015. [Google Scholar]
- Bardhan, R.; Heaton, K.; Davis, M.; Chen, P.; Dickinson, D.A.; Lungu, C.T. A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses. Int. J. Environ. Res. Public Health 2019, 16, 3243. [Google Scholar] [CrossRef] [PubMed]
- Belkić, K.; Nedic, O. Workplace stressors and lifestyle-related cancer risk factors among female physicians: Assessment using the Occupational Stress Index. J. Occup. Health 2007, 49, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.-P.; Tsai, C.-C.; Li, C.-Y.; Hu, S.C. Prevalence of cardiovascular health and its relationship with job strain: A cross-sectional study in Taiwanese medical employees. BMJ Open 2016, 6, e010467. [Google Scholar] [CrossRef]
- Fang, L.; Hsiao, L.-P.; Fang, S.-H.; Chen, B.-C. The associations with work stress, social support and overweight/obesity among hospital nurses: A cross-sectional study. Contemp. Nurse 2018, 54, 182–194. [Google Scholar] [CrossRef]
- Shinde, V.V. Relationship of body mass index to job stress and eating behaviour in health care professionals-an observational study. Obes. Med. 2019, 14, 100070. [Google Scholar] [CrossRef]
- He, S.; Chen, Y.; Zhan, J.; Wu, J.; Opler, M. Job Burnout, Mood State, and Cardiovascular Variable Changes of Doctors and Nurses in a Children’s Hospital in China. ISRN Nurs. 2014, 2014, 1–6. [Google Scholar] [CrossRef]
- Tsuboi, H.; Tatsumi, A.; Yamamoto, K.; Kobayashi, F.; Shimoi, K.; Kinae, N. Possible connections among job stress, depressive symptoms, lipid modulation and antioxidants. J. Affect. Disord. 2006, 91, 63–70. [Google Scholar] [CrossRef]
- Karasek, R.A. Job Demands, Job Decision Latitude, and Mental Strain: Implica-tions for Job Redesign. Adm. Sci. Q. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- Siegrist, J.; Li, J.; Montano, D. Psychometric Properties of the Effort-Reward Imbalance Questionnaire; Duesseldorf University: Duesseldorf, Germany, 2014. [Google Scholar]
- Holmes, C.J.; Racette, S.B. The Utility of Body Composition Assessment in Nutrition and Clinical Practice: An Overview of Current Methodology. Nutrients 2021, 13, 2493. [Google Scholar] [CrossRef] [PubMed]
- Ramos, L.B. Avaliação Nutricional: Escolares, Adultos, Idosos e Hospitalizados, 1st ed.; EDUFBA: Salvador, Brazil, 2021. [Google Scholar]
- Lee, E.-H. Review of the Psychometric Evidence of the Perceived Stress Scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Hellhammer, D.H.; Wüst, S.; Kudielka, B.M. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology 2009, 34, 163–171. [Google Scholar] [CrossRef]
- Kassim, M.S.A.B.; Ismail, A.; Ismail, R. A review of occupational stress prevalence and its predictors among selected working populations in Malaysia. Artic. Malaysian J. Pub. Health Med. 2018, 18, 1–6. Available online: https://www.researchgate.net/publication/334379832 (accessed on 13 March 2023).
- Chou, L.-P.; Li, C.-Y.; Hu, S.C. Job stress and burnout in hospital employees: Comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open 2014, 4, e004185. [Google Scholar] [CrossRef]
- Sedrez, J.A.; Da Silva Kasten, A.P.; De Oliveira Chaise, F.; Candotti, C.T. Fatores de risco para doenças cardiovasculares e osteomusculares relacionadas ao trabalho em profissionais do atendimento pré-hospitalar de urgência: Uma revisão sistemática. Rev. Bras. Med. Trab. 2017, 15, 355–363. [Google Scholar] [CrossRef]
- Selye, H. Stress and the General Adaptation Syndrome. Br. Med. J. 1950, 1, 1383–1392. [Google Scholar] [CrossRef]
- Dekkers, J.C.; van Wier, M.F.; Hendriksen, I.J.; Twisk, J.W.; van Mechelen, W. Accuracy of self-reported body weight, height and waist circumference in a Dutch overweight working population. BMC Med. Res. Methodol. 2008, 8, 69. [Google Scholar] [CrossRef]
- Craig, B.M.; Adams, A.K. Accuracy of Body Mass Index Categories Based on Self-Reported Height and Weight Among Women in the United States. Matern. Child Health J. 2008, 13, 489–496. [Google Scholar] [CrossRef][Green Version]
- Robins, R.W.; Fraley, R.C.; Krueger, R.F. Handbook of Research Methods in Personality Psychology; Guilford Press: New York, NY, USA, 2009. [Google Scholar]
- Del Duca, G.F.; González-Chica, D.A.; dos Santos, J.V.; Knuth, A.G.; Camargo, M.B.J.d.; Araújo, C.L. Self-reported weight and height for determining nutritional status of adults and elderly: Validity and implications for data analysis. Cad. Saúde Pública 2012, 28, 75–85. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Strasak, A.M.; Zaman, Q.; Pfeiffer, K.P.; Göbel, G.; Ulmer, H. Statistical errors in medical research—A review of common pitfalls. Swiss Med. Wkly. 2007, 137, 44–144. [Google Scholar] [PubMed]
- Harris, A.H.; Reeder, R.N.; Hyun, J.K. Common Statistical and Research Design Problems in Manuscripts Submitted to High-Impact Public Health Journals. Open Public Health J. 2009, 2, 44–48. [Google Scholar] [CrossRef]
- Wasserstein, R.L.; Lazar, N.A. The ASA Statement on p-Values: Context, Process, and Purpose. Am. Stat. 2016, 70, 129–133. [Google Scholar] [CrossRef]
- Amrhein, V.; Greenland, S.; McShane, B. Retire statistical significance. Nature 2019, 567, 305–307. [Google Scholar] [CrossRef] [PubMed]
- Rothman, K.; Greenland, S.; Lash, T. Fundamentals of epidemiologic data analysis. In Modern Epidemiology, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Gordis, L. Case-control studies and other study designs. In Epidemiology, 4th ed.; Saunders: Philadelphia, PA, USA, 2008; pp. 1–400. [Google Scholar]
| Author, Year | Country | Sample (Sex) | Age | Type of Worker | Diagnosis of Occupational Stress | Body Composition | Occupational Stress | Main Result |
|---|---|---|---|---|---|---|---|---|
| Abolfazli et al., 2021 [34] | Iran | 142 (men/women) | 20 to <50 years | Nurses Paramedics | Osipow Job Stress Questionnaire | BMI | Low: 1% Low to medium: 24% Moderate to severe: 82% Severe: 34% | Pearson’s correlation showed a positive relationship between overweight/obesity and stress at work (r = 0.023); however, a non-significant relationship (p > 0.05). |
| Barbosa, 2015 [38] | Brazil | 61 (11 men; 50 women) | 20 to 59 years | Nurses | Bianchi stress scale | BMI | Low: 34.65% Average: 64.36 High: 0.99% | The BMI variable was not associated with stress (r = 0.402; p = 0.084). |
| Bardhan et al., 2019 [39] | USA | 42 (13 men; 29 women) | Average 33.04 years | Nurses | ERI | BMI | ERR ≤ 1: 7% ERR > 1: 93% | Obesity: (OR = 2.653, CI = 0.026–34.15); and overweight (OR = 1.731, 95%CI = 0.208–14.39) were associated with an ERR > 1. |
| Belkić and Nedic, 2007 [40] | Serbia | 112 (men/women) | Average 48.9 years | Doctors | Occupational Stress Index | BMI | Mean = 77.3 (±11.8) | The total OSI explains the greatest variation for BMI ≥ 28 kg/m2 (OR = 1.09; 95%CI = 1.02; −1.16), whereas the sum of two OSI aspects [avoiding threats + conflict] produced the best model to explain obesity (OR = 1.29; 95%CI = 1.07; –1.55). |
| Chou et al., 2016 [41] | Taiwan | 1329 (1101 men; 228 women) | ≤30 to >50 years | Doctors Nurses Administrators | JCQ Chinese version | BMI | Low tension: 33.10% Passive work: 30.10% Active work: 17.09% High voltage: 19.71% | BMI did not correlate with work demand (regression coefficient = 0.007), work control (regression coefficient = −0.001) and work stress (regression coefficient = 0.000) p > 0.05. |
| Coelho et al., 2022 [37] | Brazil | 218 (54 men; 164 women) | Average 32.6 years | Health professionals and administration | JCQ | BMI WC BF | Before 14.2% After 29.4% | Considering changes in the level of occupational stress during the observed period, increased rates of high-level occupational stress were not significantly associated with any change in outcomes over time (BMI p = 0.944; WC p= 0.971; BF p = 0.186). |
| Fang et al., 2018 [42] | Taiwan | 237 (women) | Average 33.46 years | Nurses | ERI | BMI | ERR > 1: 20.5% ERR ≤: 78.7% | Overweight/obesity was associated with stress at work (p ≤ 0.01). The study showed that high stress at work (ERR > 1) was an important predictor of overweight/obesity. Nurses with high stress at work were 5.76 times (β = 5.764; p < 0.01) more likely to be overweight/obese. |
| Fernandes and Shinde, 2019 [43] | India | 262 (59 men; 203 women) | Average 26.2 years | Dentists Doctors Nurses Pharmacists Physiotherapists | BJSQ | BMI | With stress: 69.85% No stress: 30.15% | The value of the correlation between BMI and stress at work in the normal (r = 0.006; p = 0.939), overweight (r = −0.022; p = 0.852) and obesity (r = 0.227; p = 0.265) category of BMI was weakly correlated with job stress. |
| He et al., 2014 [44] | China | 316 (278 men; 38 women) | 20 to ≥40 years | Doctors Nurses | JSQ | BMI | Relaxed: 12.3% Normal: 45.9% Too much stress: 23.7% Overload: 18% | Statistically significant positive correlations were found between BMI and stress at work (r = 0.121; p ≤ 0.05). |
| Kouvonen et al., 2005 [36] | Finland | 6737 (men/women) | - | Nurses | JCQ | BMI | - | Greater work demands (standardized regression coefficient = 0.03; p ≤ 0.05) and greater strain (standardized regression coefficient = 0.02; p ≤ 0.05) were significantly associated with higher BMI among nurses. |
| Tsuboi et al., 2006 [45] | Japan | 33 (women) | - | Nurses | BJSQ | BMI | Low stress: 45.5% High stress: 54.5% | There was no significant difference in BMI (unpaired t-test = −0.03; p ≥ 0.05) between workers with high (20.6 ± 1.86) or low stress (20.6 ± 1.68). |
| Zhang et al., 2020 [35] | China | 1396 (796 men; 600 women) | <30 to ≥50 years | Radiation industry workers | ERI | BMI | ERI ≤ 1: 46.92% ERI > 1: 53.08% | There was a statistically significant difference in work stress in association with obesity (χ2 = 20.647; p ≤ 0.001). |
| Cross-Sectional Study | Selection | Comparability | Outcome | Total |
|---|---|---|---|---|
| Abolfazli et al., 2021 [34] | * * * * | * | * * * | 08 |
| Barbosa, 2015 [38] | * * * * | * | * | 06 |
| Bardhan et al., 2019 [39] | * * * * | * | * * | 07 |
| Belkić and Nedic, 2007 [40] | * * * * * | * | * * * | 09 |
| Chou et al., 2016 [41] | * * * * | * | * * * | 08 |
| Fang et al., 2018 [42] | * * * * * | * | * * | 08 |
| Fernandes and Shinde, 2019 [43] | * * * | * | * * * | 07 |
| He et al., 2014 [44] | * * * * | * | * * | 07 |
| Kouvonen et al., 2005 [36] | * * * * * | * | * * | 08 |
| Tsuboi et al., 2006 [45] | * * * * * | * | * | 07 |
| Zhang et al., 2020 [35] | * * * * * | * | * * | 08 |
| Cohort Study | Selection | Comparability | Outcome | Total |
| Coelho et al., 2022 [37] | * * * * | * | * * * | 08 |
| Certainty Assessment | Certainty | ||||||
|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | |
| Body Mass Index | |||||||
| 12 | Observational studies | Serious a | Serious b | Not serious | Not serious | None | ⨁◯◯◯ Very low |
| Waist Circumference | |||||||
| 01 | Observational studies | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯ Low |
| Body Fat | |||||||
| 01 | Observational studies | Not serious | Not serious | Not serious | Not serious | None | ⨁⨁◯◯ Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Lira, C.R.N.; Akutsu, R.d.C.; Coelho, L.G.; da Silva, K.B.B.; Pitangueira, J.C.D.; Zandonadi, R.P.; Costa, P.R.d.F. Influence of Occupational Stress on the Body Mass Index of Hospital Workers: A Systematic Review. Nutrients 2023, 15, 3944. https://doi.org/10.3390/nu15183944
de Lira CRN, Akutsu RdC, Coelho LG, da Silva KBB, Pitangueira JCD, Zandonadi RP, Costa PRdF. Influence of Occupational Stress on the Body Mass Index of Hospital Workers: A Systematic Review. Nutrients. 2023; 15(18):3944. https://doi.org/10.3390/nu15183944
Chicago/Turabian Stylede Lira, Carlos Rodrigo Nascimento, Rita de Cássia Akutsu, Lorene Gonçalves Coelho, Karine Brito Beck da Silva, Jacqueline Costa Dias Pitangueira, Renata Puppin Zandonadi, and Priscila Ribas de Farias Costa. 2023. "Influence of Occupational Stress on the Body Mass Index of Hospital Workers: A Systematic Review" Nutrients 15, no. 18: 3944. https://doi.org/10.3390/nu15183944
APA Stylede Lira, C. R. N., Akutsu, R. d. C., Coelho, L. G., da Silva, K. B. B., Pitangueira, J. C. D., Zandonadi, R. P., & Costa, P. R. d. F. (2023). Influence of Occupational Stress on the Body Mass Index of Hospital Workers: A Systematic Review. Nutrients, 15(18), 3944. https://doi.org/10.3390/nu15183944






