Adaptation and Validation of the Child Eating Disorder Examination Questionnaire (ChEDE-Q) for Use in English among Adolescents in Urban India
Abstract
:1. Introduction
Present Study
2. Materials and Method
2.1. Participants
2.2. Measures
2.2.1. Disordered Eating
2.2.2. Body Esteem
2.2.3. Affect
2.2.4. Self-Esteem
2.3. Procedure
2.4. Analysis
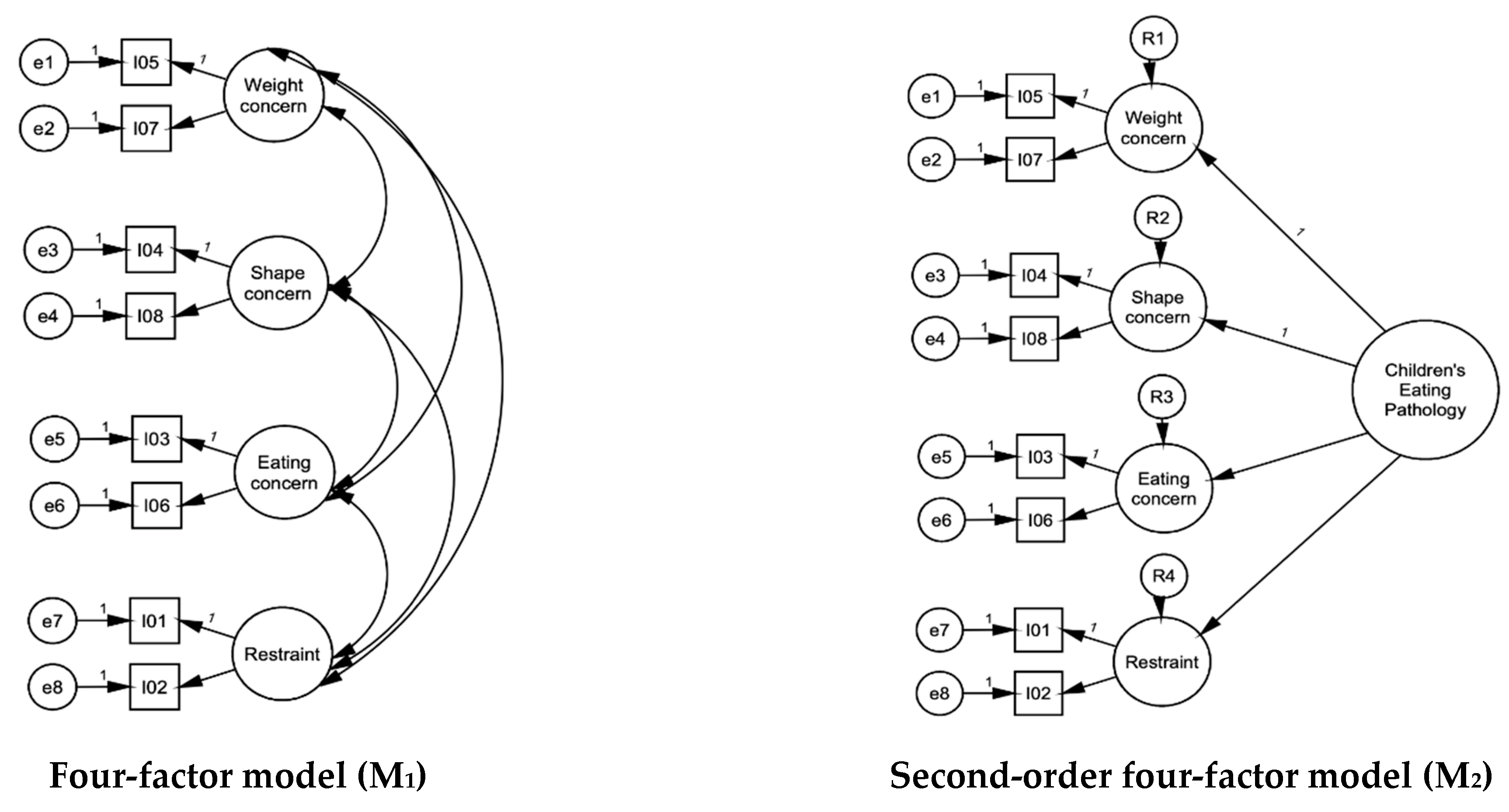
2.4.1. Dimensionality
2.4.2. Reliability
2.4.3. Validity
3. Results
3.1. Demographic Characteristics
3.2. Factor Structure
3.3. Measurement Invariance
3.4. Reliability
3.5. Concurrent Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pike, K.M.; Dunne, P.E. The rise of eating disorders in Asia: A review. J. Eat. Disord. 2015, 3, 33. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.M.; Parsekar, S.S. Body image, eating disorders and role of media among Indian adolescents. JIACAM 2016, 12, 9–35. [Google Scholar] [CrossRef]
- Ganguly, N.; Roy, S.; Mukhopadhyay, S. Association of socio-culture factors with disordered eating behavior: An empirical study on urban young girls of West Bengal, India. Anthropol. Rev. 2018, 81, 364–378. [Google Scholar] [CrossRef]
- Silén, Y.; Keski-Rahkonen, A. Worldwide prevalence of DSM-5 eating disorders among young people. Curr. Opin. Psychiatry 2022, 35, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Micali, N. What’s weighing us down: Closing the gap between the global burden of eating disorders and their representation. Eur. Child Adolesc. Psychiatry 2022, 31, 1653–1654. [Google Scholar] [CrossRef]
- Dikshit, R.; Karia, S.; Shah, N.; Sonavane, S.; DeSousa, A. A study on binge eating behavior in urban adolescents. Asian J. Psychiatr. 2020, 50, 101998. [Google Scholar] [CrossRef]
- Nivedita, N.; Sreenivasa, G.; Rao, T.S.; Malini, S.S. Eating disorders: Prevalence in the student population of Mysore, South India. Indian J. Psychiatry 2018, 60, 433–437. [Google Scholar]
- Raval, C.M.; Bhatt, R.B.; Tiwari, D.S.; Panchal, B.N. Prevalence and characteristics of eating disorders among college students of a nonmetro city of Gujarat. Ind. Psychiatry J. 2022, 31, 74–80. [Google Scholar] [CrossRef]
- Singh, M.; Amita, K. Prevalence and Determinants of Obesity/overweight and Undernutrition Among School Going Adolescents 10 to 17 years in Rural Area of South India. Online J. Health Allied Scs. 2021, 20, 1–7. [Google Scholar]
- Vaidyanathan, S.; Kuppili, P.P.; Menon, V. Eating disorders: An overview of Indian research. Indian J. Psychol. Med. 2019, 41, 311–317. [Google Scholar] [CrossRef]
- Ganesan, S.; Ravishankar, S.; Ramalingam, S. Are body image issues affecting our adolescents? A cross-sectional study among college going adolescent girls. Indian J. Community Med. 2018, 43, S42–S46. [Google Scholar] [CrossRef] [PubMed]
- Motwani, S.; Karia, S.; Mandalia, B.; Desousa, A. Eating disorders in India: An overview. Ann. Indian Psychiatry 2021, 5, 12–17. [Google Scholar]
- Sagar, R.; Dandona, R.; Gururaj, G.; Dhaliwal, R.; Singh, A.; Ferrari, A. The burden of mental disorders across the states of India: The Global Burden of Disease Study 1990–2017. Lancet Psychiatry 2020, 7, 148–161. [Google Scholar] [CrossRef]
- Sallis, J.F.; Owen, N.; Fotheringham, M.J. Behavioral epidemiology: A systematic framework to classify phases of research on health promotion and disease prevention. Ann. Behav. Med. 2000, 22, 294–298. [Google Scholar] [CrossRef]
- Morgan, J.F.; Reid, F.; Lacey, J.H. The SCOFF questionnaire: Assessment of a new screening tool for eating disorders. BMJ 1999, 319, 1467–1468. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Polivy, J. The Eating Disorder Inventory: A measure of cognitive-behavioral dimensions of anorexia nervosa and bulimia. Anorex. Nerv. Recent Dev. Res. 1983, 3, 173–184. [Google Scholar]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The eating attitudes test: Psychometric features and clinical correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.; Barron, D. Translation and validation of body image instruments: Challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image 2019, 31, 204–220. [Google Scholar] [CrossRef]
- Vijayalakshmi, P.; Thimmaiah, R.; Reddy, S.S.N.; Kathyayani, B.; Gandhi, S.; BadaMath, S. Gender differences in body mass index, body weight perception, weight satisfaction, disordered eating and weight control strategies among Indian medical and nursing undergraduates. Invest. Educ. Enferm. 2017, 35, 276–284. [Google Scholar] [CrossRef]
- Hill, L.S.; Reid, F.; Morgan, J.F.; Lacey, J.H. SCOFF, the development of an eating disorder screening questionnaire. Int. J. Eat. Disord. 2010, 43, 344–351. [Google Scholar] [CrossRef]
- Gupta, N.; Bhargava, R.; Chavan, B.S.; Sharan, P. Eating attitudes and body shape concerns among medical students in Chandigarh. Indian J. Soc. Psychiatry 2017, 33, 219–224. [Google Scholar]
- Lewis-Smith, H.; Garbett, K.M.; Chaudhry, A.; Uglik-Marucha, N.; Vitoratou, S.; Dhillon, M.; Shroff, H.; Diedrichs, P.C. Adaptation and validation of the Eating Disorder Examination-Questionnaire in English among urban Indian adolescents. Int. J. Eat. Disord. 2021, 54, 187–202. [Google Scholar] [CrossRef]
- Aggarwal, S.; Berk, M. Evolution of adolescent mental health in a rapidly changing socioeconomic environment: A review of mental health studies in adolescents in India over last 10 years. Asian J. Psychiatr. 2015, 13, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Van Hoeken, D.; Hoek, H.W. Review of the burden of eating disorders: Mortality, disability, costs, quality of life, and family burden. Curr. Opin. Psychiatry 2020, 33, 521–527. [Google Scholar] [CrossRef]
- Math, S.B.; Gowda, G.S.; Basavaraju, V.; Manjunatha, N.; Kumar, C.N.; Enara, A. Cost estimation for the implementation of the Mental Healthcare Act 2017. Indian J. Psychiatry 2019, 61, S650–S659. [Google Scholar] [CrossRef]
- Kliem, S.; Mößle, T.; Zenger, M.; Strauß, B.; Brähler, E.; Hilbert, A. The eating disorder examination-questionnaire 8: A brief measure of eating disorder psychopathology (EDE-Q8). Int. J. Eat. Disord. 2016, 49, 613–616. [Google Scholar] [CrossRef]
- Kliem, S.; Schmidt, R.; Vogel, M.; Hiemisch, A.; Kiess, W.; Hilbert, A. An 8-item short form of the Eating Disorder Examination Questionnaire adapted for children (ChEDE-Q8). Int. J. Eat. Disord. 2017, 50, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Language DoO. The Official Languages Act. 1963. Available online: https://rajbhasha.gov.in/en/official-languages-act-1963 (accessed on 1 June 2023).
- Mohanty, A.K.; Panda, M. Language Policy and Education in the Indian Subcontinent; TMSM; Springer International Publishing: Dordrecht, The Netherlands, 2017. [Google Scholar]
- Garbett, K.M.; Lewis-Smith, H.; Chaudhry, A.; Uglik-Marucha, N.; Vitoratou, S.; Shroff, H.; Dhillon, M.; Diedrichs, P.C. Cultural adaptation and validation of the Body Esteem Scale for Adults and Adolescents for use in English among adolescents in urban India. Body Image 2021, 37, 246–254. [Google Scholar] [CrossRef]
- Ebesutani, C.; Regan, J.; Smith, A.; Reise, S.; Higa-McMillan, C.; Chorpita, B.F. The 10-item positive and negative affect schedule for children, child and parent shortened versions: Application of item response theory for more efficient assessment. J. Psychopathol. Behav. Assess. 2012, 34, 191–203. [Google Scholar] [CrossRef]
- Rosenberg, M. Rosenberg self-esteem scale (RSE). Acceptance and commitment therapy. Meas. Package 1965, 61, 62. [Google Scholar]
- Sharan, P.; Sundar, A.S. Eating disorders in women. Indian J. Psychiatry 2015, 57, S286–S295. [Google Scholar] [CrossRef] [PubMed]
- Lewis-Smith, H.; Garbett, K.M.; Hasan, F.; Chaudhry, A.; Ahuja, L.; Pearson, O.; Uglik-Marucha, N.; Vitoratou, S.; Khanna, P.; Dhillon, M.; et al. Adaptation and Validation of the Rosendberg Self-Esteem Scale (RSES) for Use in English among Adolescents in Urban India; Centre for Appearance Research, University of West of England: Bristol, UK, 2023; in preparation; to be submitted. [Google Scholar]
- Lewis-Smith, H.; Garbett, K.M.; Hasan, F.; Chaudhry, A.; Ahuja, L.; Pearson, O.; Uglik-Marucha, N.; Vitoratou, S.; Khanna, P.; Dhillon, M.; et al. Adaptation and Validation of the Positive Affect and Negative Affect Scale for Children (PANAS-C) for use in English among Adolescents in Urban India; Centre for Appearance Research, University of West of England: Bristol, UK, 2023; in preparation; to be submitted. [Google Scholar]
- Mendelson, B.K.; Mendelson, M.J.; White, D.R. Body-esteem scale for adolescents and adults. J. Pers. Assess 2001, 76, 90–106. [Google Scholar] [CrossRef] [PubMed]
- Muthén, B.; Muthén, B.O. Statistical Analysis with Latent Variables; Wiley: New York, NY, USA, 2009. [Google Scholar]
- Arbuckle, J. SPSS Amos (Version 26.0) [Computer Program]; IBM SPSS: Chicago, IL, USA, 2019. [Google Scholar]
- Chou, C.P.; Bentler, P.M.; Satorra, A. Scaled test statistics and robust standard errors for non-normal data in covariance structure analysis: A Monte Carlo study. Br. J. Math. Stat. Psychol. 1991, 44, 347–357. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Reise, S.P.; Morizot, J.; Hays, R.D. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual. Life Res. 2007, 16, 19–31. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Cordon, S.L.; Finney, S.J. Measurement invariance of the Mindful Attention Awareness Scale across adult attachment style. Meas. Eval. Couns. Dev. 2008, 40, 228–245. [Google Scholar] [CrossRef]
- French, B.F.; Finch, W.H. Confirmatory factor analytic procedures for the determination of measurement invariance. Struct. Equ. Modeling 2006, 13, 378–402. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Goldberger, A.S. Estimation of a model with multiple indicators and multiple causes of a single latent variable. J. Am. Stat. Assoc. 1975, 70, 631–639. [Google Scholar]
- Muthén, B. A structural probit model with latent variables. J. Am. Stat. Assoc. 1979, 74, 807–811. [Google Scholar]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- McDonald, R.P. Test Theory: A Unified Approach; Erlbaum: Mahwah, NJ, USA, 1999. [Google Scholar]
- Green, S.B.; Yang, Y. Commentary on coefficient alpha: A cautionary tale. Psychometrika 2009, 74, 121–135. [Google Scholar] [CrossRef]
- Zinbarg, R.E.; Revelle, W.; Yovel, I. Estimating ωh for Structures Containing Two Group Factors: Perils and Prospects. Appl. Psychol. Meas. 2007, 31, 135–157. [Google Scholar] [CrossRef]
- Graham, J.M. Congeneric and (essentially) tau-equivalent estimates of score reliability: What they are and how to use them. Educ. Psychol. Meas. 2006, 66, 930–944. [Google Scholar] [CrossRef]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS; McGraw-Hill Education: London, UK, 2020. [Google Scholar]
- Becker, A.E.; Thomas, J.J.; Bainivualiku, A.; Richards, L.; Navara, K.; Roberts, A.L. Validity and reliability of a Fijian translation and adaptation of the Eating Disorder Examination Questionnaire. Int. J. Eat. Disord. 2010, 43, 171–178. [Google Scholar] [CrossRef]
- Penelo, E.; Negrete, A.; Portell, M.; Raich, R.M. Psychometric properties of the Eating Disorder Examination Questionnaire (EDE-Q) and norms for rural and urban adolescent males and females in Mexico. PLoS ONE 2013, 8, e83245. [Google Scholar] [CrossRef]
- Forsén Mantilla, E.; Birgegård, A.; Clinton, D. Factor analysis of the adolescent version of the Eating Disorders Examination Questionnaire (EDE-Q): Results from Swedish general population and clinical samples. J. Eat. Disord. 2017, 5, 19. [Google Scholar] [CrossRef]
- Hoek, H.W.; Van Hoeken, D. Review of the prevalence and incidence of eating disorders. Int. J. Eat. Disord. 2003, 34, 383–396. [Google Scholar] [CrossRef]
- Cash, T.F.; Smolak, L. Body Image: A Handbook of Science, Practice, and Prevention; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Allen, K.L.; Byrne, S.M.; Lampard, A.; Watson, H.; Fursland, A. Confirmatory factor analysis of the eating disorder examination-questionnaire (EDE-Q). Eat. Behav. 2011, 12, 143–151. [Google Scholar] [CrossRef]
- Calugi, S.; Milanese, C.; Sartirana, M.; El Ghoch, M.; Sartori, F.; Geccherle, E. The Eating Disorder Examination Questionnaire: Reliability and validity of the Italian version. Eat. Weight Disord. 2017, 22, 509–514. [Google Scholar] [CrossRef]
- Mallick, N.; Ray, S.; Mukhopadhyay, S. Eating behaviours and body weight concerns among adolescent girls. Adv. Public Health 2014, 2014, 257396. [Google Scholar] [CrossRef]
- Yucel, B.; Polat, A.; Ikiz, T.; Dusgor, B.P.; Elif Yavuz, A.; Sertel Berk, O. The Turkish version of the eating disorder examination questionnaire: Reliability and validity in adolescents. Eur. Eat. Disord. Rev. 2011, 19, 509–511. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, V.R.; Kulkarni, A.A. Body image and its relation with body mass index among Indian adolescents. Indian Pediatr. 2017, 54, 1025–1028. [Google Scholar] [CrossRef]
- Lewis-Smith, H.; Hasan, F.; Ahuja, L.; White, P.; Diedrichs, P.C. A comic-based body image intervention for adolescents in semi-rural Indian schools: Study protocol for a randomized controlled trial. Body Image 2022, 42, 183–196. [Google Scholar] [CrossRef]
- Shenoy, S.K.; Praharaj, S.K. Borderline personality disorder and its association with bipolar spectrum and binge eating disorder in college students from South India. Asian J. Psychiatr. 2019, 44, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Lal, M.; Abraham, S. Adolescent development and eating disorder related quality of life in Indian females. Eat. Weight Disord. 2011, 16, e56–e60. [Google Scholar] [CrossRef]
- Chaudhari, B.; Tewari, A.; Vanka, J.; Kumar, S.; Saldanha, D. The relationship of eating disorders risk with body mass index, body image and self-esteem among medical students. Ann. Med. Health Sci. Res. 2017, 7, 144–149. [Google Scholar]
- Suarez-Albor, C.L.; Galletta, M.; Gómez-Bustamante, E.M. Factors associated with eating disorders in adolescents: A systematic review. Acta Biomed. 2022, 93, e2022253. [Google Scholar]
- Satija, A.; Khandpur, N.; Satija, S.; Mathur Gaiha, S.; Prabhakaran, D.; Reddy, K.S. Physical activity among adolescents in India: A qualitative study of barriers and enablers. Health Educ. Behav. 2018, 45, 926–934. [Google Scholar] [CrossRef] [PubMed]

| Item | Label | Mean (SD) | Median (Min–Max) | 1-Factor Model (M4) | 2-Factor Model (M3) | Bifactor 2-Factor Model (M5) | |||
|---|---|---|---|---|---|---|---|---|---|
| General Factor | Eating Concern and Restraint | Weight and Shape Concerns | General Factor | Eating Concern and Restraint | Weight and Shape Concerns | ||||
| I02 | Avoidance of eating | 0.94 (1.46) | 0 (0–6) | 0.432 | 0.529 | 0.545 | 0.39 | ||
| I01 | Food avoidance | 1.24 (1.72) | 0 (0–6) | 0.486 | 0.6 | 0.612 | 0.313 | ||
| I06 | Guilt about eating | 0.98 (1.53) | 0 (0–6) | 0.571 | 0.636 | 0.776 | −0.456 * | ||
| I03 | Preoccupation with food | 1.46 (1.92) | 1 (0–6) | 0.396 | 0.491 | 0.473 | −0.038 * | ||
| I04 | Feelings of fatness | 1.13 (1.82) | 0 (0–6) | 0.824 | 0.836 | 0.592 | 0.589 | ||
| I07 | Dissatisfaction with weight | 1.38 (1.81) | 1 (0–6) | 0.675 | 0.685 | 0.443 | 0.538 | ||
| I05 | Desire to lose weight | 1.35 (2.07) | 0 (0–6) | 0.812 | 0.823 | 0.581 | 0.584 | ||
| I08 | Discomfort seeing body | 1.47 (1.85) | 1 (0–6) | 0.6 | 0.593 | 0.505 | 0.324 | ||
| Mean (SD) | Girls (n = 182) | Boys (n = 203) | Comparison | Total | Eating Concerns and Restraint | Weight and Shape Concerns | ||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Statistic | p-Value | |||||
| Child Eating Disorder Examination Questionnaire (ChEDE-Q; n = 385) | ||||||||
| Total | 9.96 (9.53) | 10.92 (10.88) | 9.56 (9.01) | U = 10,277.00 | 0.604 | 1 | ||
| Eating concerns and restraint | 4.63 (4.65) | 4.53 (4.9) | 4.8 (4.85) | U = 9581.500 | 0.615 | 0.872 ** | 1 | |
| Weight and shape concerns | 5.33 (6.12) | 6.39 (6.94) | 4.76 (5.41) | U = 9581.500 | 0.117 | 0.881 ** | 0.569 ** | 1 |
| Positive and Negative Affect Scale (PANAS; n = 282) | ||||||||
| Positive affect | 18.54 (4.39) | 18.58 (4.07) | 18.51 (4.69) | U = 9791.00 | 0.847 | −0.07 | −0.054 | −0.078 |
| Negative affect | 11.18 (3.74) | 11.57 (3.64) | 10.83 (3.8) | t(280) = −1.668 | 0.096 | 0.307 ** | 0.294 ** | 0.264 ** |
| Body Esteem Scale (BES; n = 282) | ||||||||
| Total | 3.79 (0.75) | 3.84 (0.79) | 3.75 (0.70) | t(280) = −1.091 | 0.276 | −0.434 ** | −0.360 ** | −0.421 ** |
| Negative appearance | 4.17 (0.76) | 4.18 (0.78) | 4.17 (0.75) | U = 10,032.000 | 0.871 | −0.463 ** | −0.360 ** | −0.473 ** |
| Positive appearance | 3.29 (1.11) | 3.4 (1.16) | 3.19 (1.06) | t(280) = −1.600 | 0.111 | −0.290 ** | −0.254 ** | −0.266 ** |
| Rosenberg Self-Esteem Scale (RSES; n = 282) | ||||||||
| Total | 20.26 (4.32) | 20.12 (4.36) | 20.38 (4.3) | t(280) = 0.509 | 0.611 | −0.307 ** | −0.297 ** | −0.267 ** |
| Item | Label | Average IIC | ITC | AID | OID |
|---|---|---|---|---|---|
| Weight and shape concerns (α = 0.825, ω = 0.825) | |||||
| I04 | Feelings of fatness | 0.51 | 0.71 | 0.75 | 0.76 |
| I07 | Dissatisfaction with weight | 0.54 | 0.66 | 0.78 | 0.79 |
| I05 | Desire to lose weight | 0.52 | 0.69 | 0.76 | 0.76 |
| I08 | Discomfort seeing body | 0.61 | 0.55 | 0.82 | 0.83 |
| Eating concern and restraint (α = 0.649, ω = 0.637) | |||||
| I01 | Food avoidance | 0.29 | 0.47 | 0.551 | 0.57 |
| I02 | Avoidance of eating | 0.33 | 0.425 | 0.587 | 0.59 |
| I03 | Preoccupation with food | 0.34 | 0.398 | 0.612 | 0.64 |
| I06 | Guilt about eating | 0.32 | 0.441 | 0.574 | 0.59 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahuja, L.; Diedrichs, P.C.; Garbett, K.M.; Chaudhry, A.; Hasan, F.; Uglik-Marucha, N.; Vitoratou, S.; Dhillon, M.; Shroff, H.; Lewis-Smith, H. Adaptation and Validation of the Child Eating Disorder Examination Questionnaire (ChEDE-Q) for Use in English among Adolescents in Urban India. Nutrients 2023, 15, 3836. https://doi.org/10.3390/nu15173836
Ahuja L, Diedrichs PC, Garbett KM, Chaudhry A, Hasan F, Uglik-Marucha N, Vitoratou S, Dhillon M, Shroff H, Lewis-Smith H. Adaptation and Validation of the Child Eating Disorder Examination Questionnaire (ChEDE-Q) for Use in English among Adolescents in Urban India. Nutrients. 2023; 15(17):3836. https://doi.org/10.3390/nu15173836
Chicago/Turabian StyleAhuja, Latika, Phillippa C. Diedrichs, Kirsty M. Garbett, Anshula Chaudhry, Farheen Hasan, Nora Uglik-Marucha, Silia Vitoratou, Megha Dhillon, Hemal Shroff, and Helena Lewis-Smith. 2023. "Adaptation and Validation of the Child Eating Disorder Examination Questionnaire (ChEDE-Q) for Use in English among Adolescents in Urban India" Nutrients 15, no. 17: 3836. https://doi.org/10.3390/nu15173836
APA StyleAhuja, L., Diedrichs, P. C., Garbett, K. M., Chaudhry, A., Hasan, F., Uglik-Marucha, N., Vitoratou, S., Dhillon, M., Shroff, H., & Lewis-Smith, H. (2023). Adaptation and Validation of the Child Eating Disorder Examination Questionnaire (ChEDE-Q) for Use in English among Adolescents in Urban India. Nutrients, 15(17), 3836. https://doi.org/10.3390/nu15173836








