Exploring Health Behaviours, Attitudes and Beliefs of Women and Men during the Preconception and Interconception Periods: A Cross-Sectional Study of Adults on the Island of Ireland
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethics
2.2. Questionnaire Development
2.3. Measures
2.3.1. Demographic Characteristics and Health Status
2.3.2. Current Health Behaviours
2.3.3. Attitudes towards Preconception Health and Care
2.3.4. Preconception Health Beliefs
2.4. Statistical Analysis
3. Results
3.1. Demographics
3.2. Health Status and Current Health Behaviours
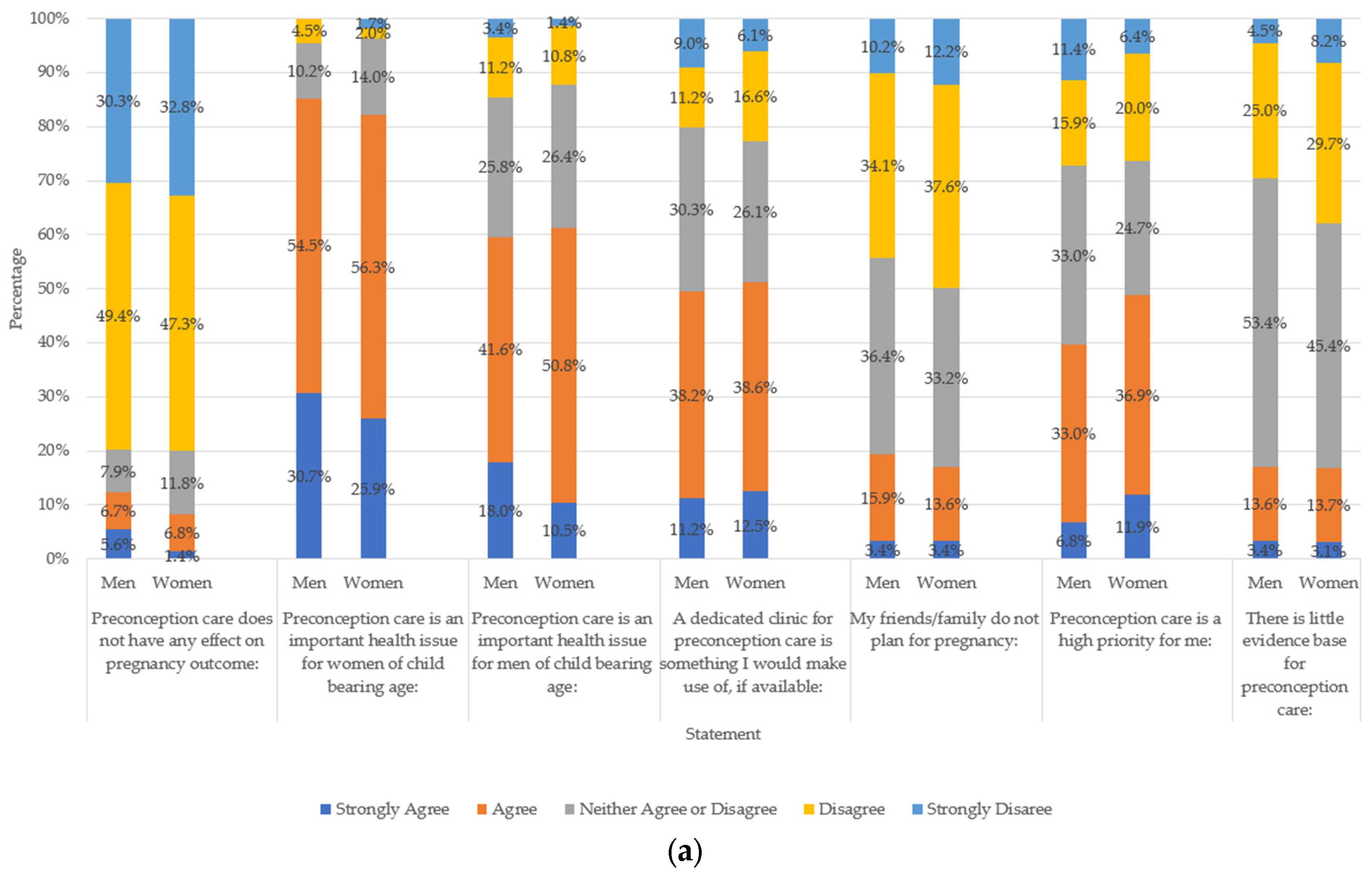
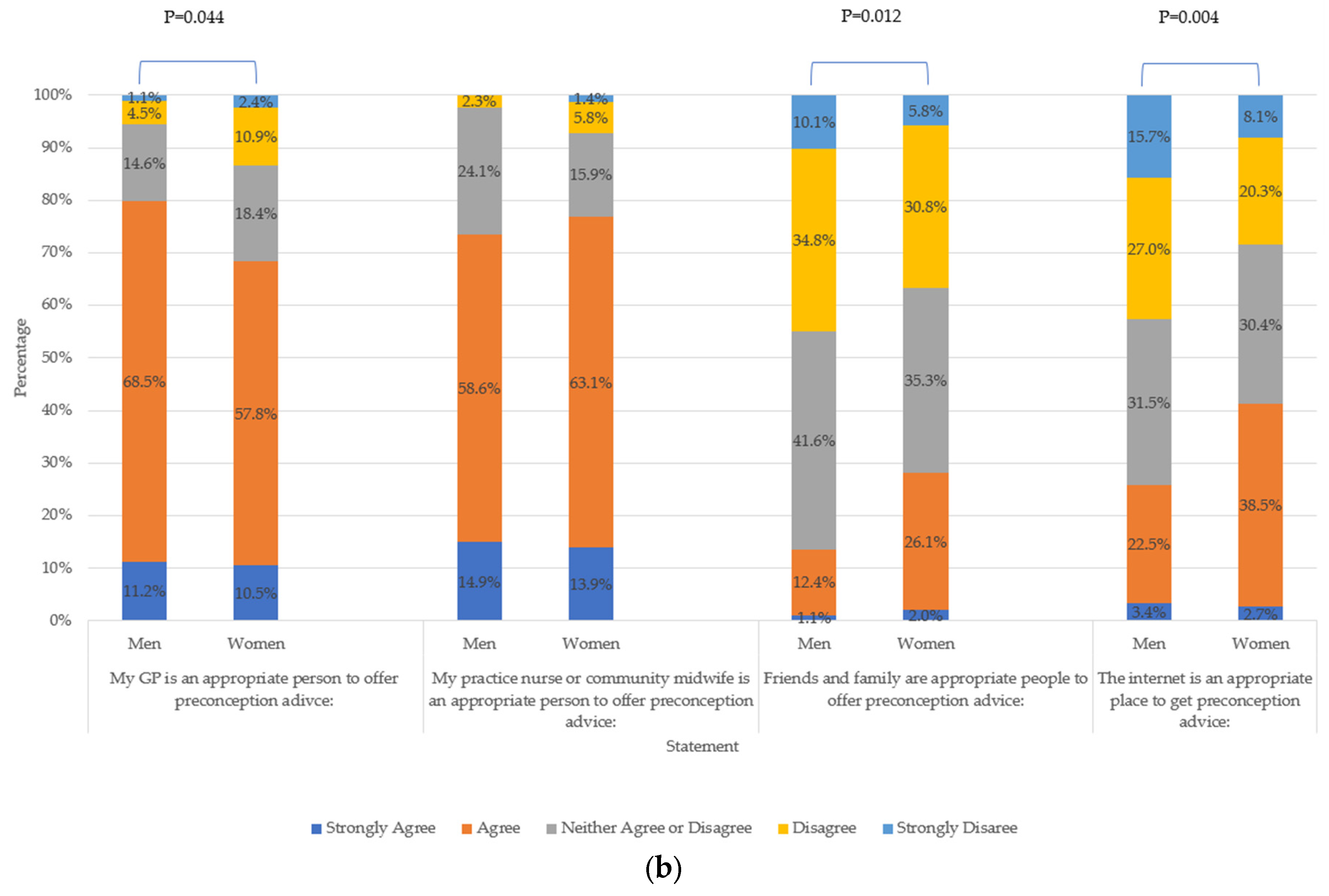
3.3. Attitudes towards Preconception Health and Care
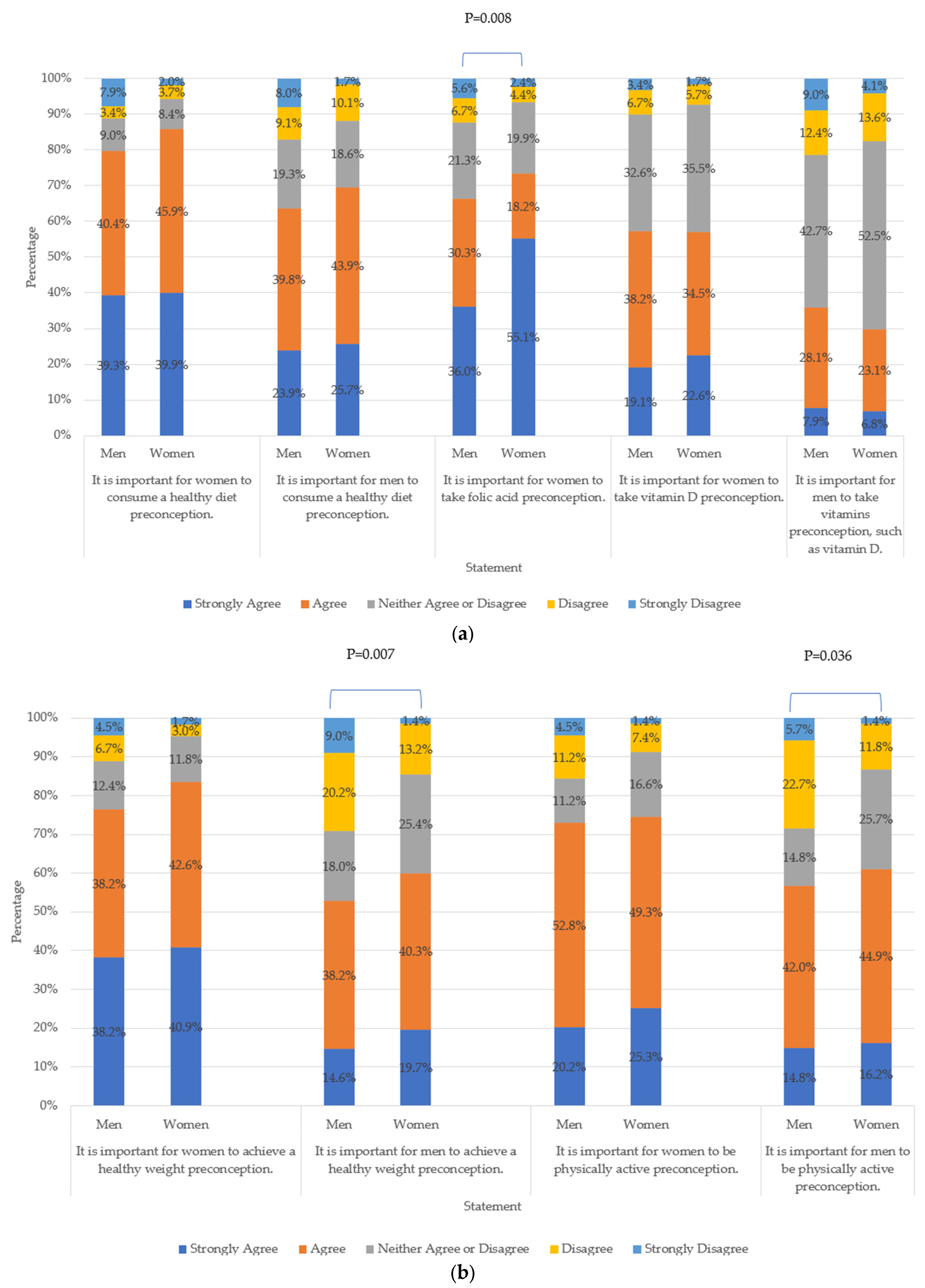
3.4. Preconception Health Beliefs
4. Discussion
4.1. Health Status and Current Health Behaviours
Comparisons with Current Preconception and/or Interconception Recommendations
4.2. Attitudes towards Preconception Health and Care
4.2.1. Importance of Preconception Care
4.2.2. Pregnancy Planning
4.2.3. Sources of Information
4.3. Preconception Health Beliefs
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robbins, C.L.; D’Angelo, D.; Zapata, L.; Boulet, S.L.; Sharma, A.J.; Adamski, A.; Farfalla, J.; Stampfel, C.; Verbiest, S.; Kroelinger, C. Preconception Health Indicators for Public Health Surveillance. J. Womens Health 2018, 27, 430–443. [Google Scholar] [CrossRef] [PubMed]
- Robbins, C.; Boulet, S.L.; Morgan, I.; D’Angelo, D.V.; Zapata, L.B.; Morrow, B.; Sharma, A.; Kroelinger, C.D. Disparities in Preconception Health Indicators—Behavioral Risk Factor Surveillance System, 2013–2015, and Pregnancy Risk Assessment Monitoring System, 2013–2014. MMWR Surveill. Summ. 2018, 67, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Pre-conception—Advice and Management. Available online: https://cks.nice.org.uk/topics/pre-conception-advice-management/ (accessed on 2 June 2022).
- Yang, H.; Chryssikos, T.; Houseni, M.; Alzeair, S.; Sansovini, M.; Iruvuri, S.; Torigian, D.A.; Zhuang, H.; Dadparvar, S.; Basu, S.; et al. The effects of aging on testicular volume and glucose metabolism: An investigation with ultrasonography and FDG-PET. Mol. Imaging Biol. 2011, 13, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Birth Statistics. Available online: https://www.nisra.gov.uk/publications/birth-statistics (accessed on 24 May 2023).
- Ireland—Overview. Available online: https://www.unfpa.org/data/world-population/IE (accessed on 23 June 2022).
- Toivonen, K.I.; Oinonen, K.A.; Duchene, K.M. Preconception health behaviours: A scoping review. Prev. Med. 2017, 96, 1–15. [Google Scholar] [CrossRef]
- Schoenaker, D.A.J.M.; Stephenson, J.; Connolly, A.; Shillaker, S.; Fishburn, S.; Barker, M.; Godfrey, K.M.; Alwan, N.A.; UK Preconception Partnership. Characterising and monitoring preconception health in England: A review of national population-level indicators and core data sources. J. Dev. Orig. Health Dis. 2021, 13, 137–150. [Google Scholar] [CrossRef]
- Khan, N.N.; Boyle, J.A.; Lang, A.Y.; Harrison, C.L. Preconception Health Attitudes and Behaviours of Women: A Qualitative Investigation. Nutrients 2019, 11, 1490. [Google Scholar] [CrossRef]
- Chuang, C.H.; Velott, D.L.; Weisman, C.S. Exploring knowledge and attitudes related to pregnancy and preconception health in women with chronic medical conditions. Matern. Child. Health J. 2010, 14, 713–719. [Google Scholar] [CrossRef]
- Mello, S.; Tan, A.S.L.; Sanders-Jackson, A.; Bigman, C.A. Gender Stereotypes and Preconception Health: Men’s and Women’s Expectations of Responsibility and Intentions to Engage in Preventive Behaviors. Matern. Child. Health J. 2019, 23, 459–469. [Google Scholar] [CrossRef]
- Dennis, C.L.; Brennenstuhl, S.; Brown, H.K.; Bell, R.C.; Marini, F.; Birken, C.S. High-risk health behaviours of pregnancy-planning women and men: Is there a need for preconception care? Midwifery 2022, 106, 103244. [Google Scholar] [CrossRef]
- D’Angelo, D.; Williams, L.; Morrow, B.; Cox, S.; Harris, N.; Harrison, L.; Posner, S.F.; Hood, J.R.; Zapata, L.; Centers for Disease Control and Prevention (CDC). Preconception and interconception health status of women who recently gave birth to a live-born infant--Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas, 2004. MMWR Surveill. Summ 2007, 56, 1–35. [Google Scholar]
- Chilukuri, N.; Cheng, T.L.; Psoter, K.J.; Mistry, K.B.; Connor, K.A.; Levy, D.J.; Upadhya, K.K. Effectiveness of a Pediatric Primary Care Intervention to Increase Maternal Folate Use: Results from a Cluster Randomized Controlled Trial. J. Pediatr. 2018, 192, 247–252.e1. [Google Scholar] [CrossRef] [PubMed]
- de Smit, D.J.; Weinreich, S.S.; Cornel, M.C. Effects of a simple educational intervention in well-baby clinics on women’s knowledge about and intake of folic acid supplements in the periconceptional period: A controlled trial. Public. Health Nutr. 2015, 18, 1119–1126. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nascimento, S.L.; Pudwell, J.; Surita, F.G.; Adamo, K.B.; Smith, G.N. The effect of physical exercise strategies on weight loss in postpartum women: A systematic review and meta-analysis. Int. J. Obes. 2014, 38, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Oteng-Ntim, E.; Mononen, S.; Sawicki, O.; Seed, P.T.; Bick, D.; Poston, L. Interpregnancy weight change and adverse pregnancy outcomes: A systematic review and meta-analysis. BMJ Open 2018, 8, e018778. [Google Scholar] [CrossRef] [PubMed]
- Musgrave, L.; Homer, C.; Gordon, A. Knowledge, attitudes and behaviours surrounding preconception and pregnancy health: An Australian cross-sectional survey. BMJ Open 2023, 13, e065055. [Google Scholar] [CrossRef]
- Schoenaker, D.A.J.M.; Stephenson, J.; Smith, H.; Thurland, K.; Duncan, H.; Godfrey, K.M.; Barker, M.; Singh, C.; Alwan, N.A.; UK Preconception Partnership. Women’s preconception health in England: A report card based on cross-sectional analysis of national maternity services data from 2018/2019. BJOG Int. J. Obstet. Gynaecol. 2023, 130, 1187–1195. [Google Scholar] [CrossRef]
- Shawe, J.; Patel, D.; Joy, M.; Howden, B.; Barrett, G.; Stephenson, J. Preparation for fatherhood: A survey of men’s preconception health knowledge and behaviour in England. PLoS ONE 2022, 14, e0213897. [Google Scholar] [CrossRef]
- McGowan, L.; Lennon-Caughey, E.; Chun, C.; McKinley, M.C.; Woodside, J.V. Exploring preconception health beliefs amongst adults of childbearing age in the UK: A qualitative analysis. BMC Pregnancy Childbirth 2020, 20, 41. [Google Scholar] [CrossRef]
- Agricola, E.; Gesualdo, F.; Carloni, E.; D’Ambrosio, A.; Russo, L.; Campagna, I.; Pandolfi, E.; Tozzi, A.E. Investigating paternal preconception risk factors for adverse pregnancy outcomes in a population of internet users. Reprod. Health 2016, 13, 37. [Google Scholar] [CrossRef]
- Frey, K.A.; Engle, R.; Noble, B. Preconception healthcare: What do men know and believe? J. Men’s Health 2012, 9, 25–35. [Google Scholar] [CrossRef]
- Wellings, K.; Jones, K.G.; Mercer, C.H.; Tanton, C.; Clifton, S.; Datta, J.; Copas, A.J.; Erens, B.; Gibson, L.J.; Macdowall, W.; et al. The prevalence of unplanned pregnancy and associated factors in Britain: Findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet 2013, 382, 1807–1816. [Google Scholar] [CrossRef]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.J.M.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M.; et al. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef] [PubMed]
- Standard Alcoholic Drink. Available online: https://www.drinkaware.ie/facts/what-is-a-standard-drink (accessed on 1 March 2020).
- Gribble, K.D.; Bewley, S.; Bartick, M.C.; Mathisen, R.; Walker, S.; Gamble, J.; Bergman, N.J.; Gupta, A.; Hocking, J.J.; Dahlen, H.G. Effective Communication About Pregnancy, Birth, Lactation, Breastfeeding and Newborn Care: The Importance of Sexed Language. Front. Glob. Womens Health 2022, 3, 818856. [Google Scholar] [CrossRef] [PubMed]
- National Statistics Socio-Economic Classification (NS-SEC). Available online: https://www.ons.gov.uk/methodology/classificationsandstandards/otherclassifications/thenationalstatisticssocioeconomicclassificationnssecrebasedonsoc2010 (accessed on 20 February 2023).
- ISCED-UK: Northern Ireland. Available online: http://gpseducation.oecd.org/Content/MapOfEducationSystem/GBR/GBR_2011_EN.pdf (accessed on 12 June 2023).
- Obesity. Available online: https://cks.nice.org.uk/topics/obesity/ (accessed on 20 February 2023).
- Pot, G.K.; Richards, M.; Prynne, C.J.; Stephen, A.M. Development of the Eating Choices Index (ECI): A four-item index to measure healthiness of diet. Public. Health Nutr. 2014, 17, 2660–2666. [Google Scholar] [CrossRef] [PubMed]
- Wanner, M.; Probst-Hensch, N.; Kriemler, S.; Meier, F.; Bauman, A.; Martin, B.W. What physical activity surveillance needs: Validity of a single-item questionnaire. Br. J. Sports Med. 2014, 48, 1570–1576. [Google Scholar] [CrossRef]
- Planning Your Pregnancy. Available online: https://www.nhs.uk/pregnancy/trying-for-a-baby/planning-your-pregnancy/ (accessed on 20 February 2023).
- Adult Smoking Habits in the UK. 2019. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2019 (accessed on 20 February 2023).
- Heyes, T.; Long, S.; Mathers, N. Preconception care: Practice and beliefs of primary care workers. Fam. Pract. 2004, 21, 22–27. [Google Scholar] [CrossRef]
- Lindgren, K. Testing the Health Practices in Pregnancy Questionnaire-II. J. Obstet. Gynecol. Neonatal Nurs. 2005, 34, 465–472. [Google Scholar] [CrossRef]
- Corder, K.; Winpenny, E.M.; Foubister, C.; Guagliano, J.M.; Hartwig, X.M.; Love, R.; Clifford Astbury, C.; van Sluijs, E.M.F. Becoming a parent: A systematic review and meta-analysis of changes in BMI, diet, and physical activity. Obes. Rev. 2020, 21, e12959. [Google Scholar] [CrossRef]
- Parenting and Family Diversity Issues. Available online: https://pdfs.semanticscholar.org/0d32/b02bfd07c4b58e32b18be3b6ef2889555e52.pdf (accessed on 23 August 2023).
- Stewart, C.; Hall, J. Pregnancy preparation amongst women and their partners in the UK; how common is it and what do people do? medRxiv 2022, 12, 22283057. [Google Scholar] [CrossRef]
- The Eatwell Guide. Available online: https://www.gov.uk/government/publications/the-eatwell-guide (accessed on 9 June 2023).
- Chivers, B.R.; Boyle, J.A.; Lang, A.Y.; Teede, H.J.; Moran, L.J.; Harrison, C.L. Preconception Health and Lifestyle Behaviours of Women Planning a Pregnancy: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 1701. [Google Scholar] [CrossRef]
- Inskip, H.M.; Crozier, S.R.; Godfrey, K.M.; Borland, S.E.; Cooper, C.; Robinson, S.M. Southampton Women’s Survey Study Group. Women’s compliance with nutrition and lifestyle recommendations before pregnancy: General population cohort study. BMJ 2009, 338, b481. [Google Scholar] [CrossRef]
- Wallace, M.; Hurwitz, B. Preconception care: Who needs it, who wants it, and how should it be provided? Br. J. Gen. Pract. 1998, 48, 963–966. [Google Scholar] [CrossRef][Green Version]
- Dunney, C.; Murphy, D.J. Healthy lifestyle behaviours in pregnancy: A prospective cohort study in Ireland. Br. J. Midwifery 2015, 23, 874–884. [Google Scholar] [CrossRef]
- Kent, L.; Cardwell, C.; Young, I.; Eastwood, K.A. Trends in maternal body mass index in Northern Ireland: A cross-sectional and longitudinal study. Fam. Med. Community Health 2021, 9, e001310. [Google Scholar] [CrossRef] [PubMed]
- Grace, B.; Shawe, J.; Stephenson, J. A mixed methods study investigating sources of fertility and reproductive health information in the UK. Sex. Reprod. Healthc. 2023, 36, 100826. [Google Scholar] [CrossRef]
- Kahlor, L.; Mackert, M. Perceptions of infertility information and support sources among female patients who access the Internet. Fertil. Steril. 2009, 91, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Brochu, F.; Robins, S.; Miner, S.A.; Grunberg, P.H.; Chan, P.; Lo, K.; Holzer, H.E.G.; Mahutte, N.; Ouhilal, S.; Tulandi, T.; et al. Searching the Internet for Infertility Information: A Survey of Patient Needs and Preferences. J. Med. Internet Res. 2019, 21, e15132. [Google Scholar] [CrossRef]
- Zillien, N.; Haake, G.; Fröhlich, G.; Bense, T.; Souren, D. Internet Use of Fertility Patients: A Systemic Review of the Literature. J. Reproduktionsmed. Endokrinol. 2011, 8, 281–287. [Google Scholar]
- Evaluation of #ReadyforPregnancy Campaign in the South East. Available online: https://www.southeastclinicalnetworks.nhs.uk/wp-content/uploads/2021/12/Ready-for-Pregnancy-Evaluation-Report.pdf (accessed on 9 June 2023).
- Ekstrand Ragnar, M.; Grandahl, M.; Stern, J.; Mattebo, M. Important but far away: Adolescents’ beliefs, awareness and experiences of fertility and preconception health. Eur. J. Contracept. Reprod. Health Care 2018, 23, 265–273. [Google Scholar] [CrossRef]
- Carter, T.; Schoenaker, D.; Adams, J.; Steel, A. Paternal preconception modifiable risk factors for adverse pregnancy and offspring outcomes: A review of contemporary evidence from observational studies. BMC Public. Health 2023, 23, 509. [Google Scholar] [CrossRef]
- Thomas, M.; Cheney, K.; Black, K.I. Scoping review into models of interconception care delivered at well-child visits for the Australian context. Aust. J. Prim. Health 2023, 29, 195–206. [Google Scholar] [CrossRef]
- Census 2021 Main Statistics Ethnicity Tables. Available online: https://www.nisra.gov.uk/publications/census-2021-main-statistics-ethnicity-tables (accessed on 12 June 2023).
- Census 2016 Reports. Available online: https://www.cso.ie/en/census/census2016reports/ (accessed on 12 June 2023).
- Meader, N.; King, K.; Moe-Byrne, T.; Wright, K.; Graham, H.; Petticrew, M.; Power, C.; White, M.; Sowden, A.J. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health 2016, 16, 657. [Google Scholar] [CrossRef] [PubMed]
- Women and Men in Ireland 2019. Available online: https://www.cso.ie/en/releasesandpublications/ep/p-wamii/womenandmeninireland2019/health/ (accessed on 24 May 2023).
- Luo, J.; Thomson, C.A.; Hendryx, M.; Tinker, L.F.; Manson, J.E.; Li, Y.; Nelson, D.A.; Vitolins, M.Z.; Seguin, R.A.; Eaton, C.B.; et al. Accuracy of self-reported weight in the Women’s Health Initiative. Public. Health Nutr. 2019, 22, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean(SD)/n(%) All | Mean(SD)/ n(Column %) Men | Mean(SD)/ n(Column %) Women | p-Value | Mean(SD)/ n(Column %) with Children | Mean(SD)/ n(Column %) without Children | p-Value |
|---|---|---|---|---|---|---|---|
| Sex (n = 385) c | |||||||
| Men (n = 89) | 89 (23.1%) | — | — | 34 (24.1%) c | 52 (21.8%) c | 0.613 | |
| Women (n = 296) | 296 (76.9%) | — | — | 107 (75.9%) c | 187 (78.2%) c | ||
| Parental Status (n = 380) | |||||||
| With Children (n = 141) | 141 (37.1%) | 34 (39.5%) | 107 (36.4%) | 0.613 | — | — | |
| Without Children (n = 239) | 239 (62.9%) | 52 (60.5%) | 187 (63.6%) | — | — | ||
| Age (n = 333) | |||||||
| Overall age in years (n = 333) | 29.9 (10.3) | 32.8 (13.1) | 29.2 (9.3) | 0.029 | 40.4 (8.2) | 24.0 (5.6) | 0.029 |
| 18–27 years (n = 167) | 167 (50.2%) | 39 (53.4%) | 128 (49.2%) | 0.617 | 1 (0.8%) c | 164 (78.1%) c | <0.001 |
| 28–60 years (n = 166) | 166 (49.8%) | 34 (46.6%) | 132 (50.8%) | 119 (99.2%) c | 46 (21.9%) c | ||
| Country of Residence (n = 385) | |||||||
| United Kingdom (incl. Northern Ireland) (n = 300) | 300 (77.9%) | 36 (40.4%) | 264 (89.2%) | <0.001 | 102 (72.3%) c | 196 (82%) c | 0.086 |
| Republic of Ireland (n = 68) | 68 (17.7%) | 49 (55.1%) | 19 (6.4%) | 31 (22.0%) c | 34 (14.2%) c | ||
| Other (n = 17) a | 17 (4.4%) | 4 (4.5%) | 13 (4.4%) | 8 (5.7%) | 9 (3.8%) | ||
| Education status (n = 385) | |||||||
| No qualifications or compulsory level (n = 11) | 11 (2.9%) | 3 (3.4%) | 8 (2.7%) | 0.091 | 6 (4.3%) | 5 (2.1%) | <0.001 |
| Secondary/ further education (e.g., NVQ) (n = 92) | 92 (23.9%) | 30 (33.7%) | 62 (20.9%) | 31 (22%) c | 59 (24.7%) c | ||
| University or higher (UG or PG degree) (n = 205) | 205 (53.2%) | 41 (46.1%) | 164 (55.4%) | 102 (72.3%) c | 100 (41.8%) c | ||
| Still in full-time education (n = 77) | 77 (20%) | 15 (16.9%) | 62 (20.9%) | 2 (1.4%) | 75 (31.4%) | ||
| Socio-economic class (n = 309) c | |||||||
| Higher managerial, administrative and professional occupations (n = 187) | 187 (60.5%) | 46 (66.7%) | 141 (58.8%) | 0.426 | 84 (68.9%) | 100 (54.9%) | 0.008 |
| Intermediate occupations (n = 77) | 77 (24.9%) | 13 (18.8%) | 64 (26.7%) | 30 (24.6%) c | 45 (24.7%) c | ||
| Routine and manual occupations (n = 28) b | 28 (9.1%) | 8 (11.6%) | 20 (8.3%) | 7 (5.7%) | 21 (11.5%) | ||
| Not working (n = 17) d | 17 (5.5%) | 2 (2.8%) | 15 (6.3%) | 1 (0.8%) | 16 (8.8%) | ||
| Variable | Overall Mean (SD)/n(Column %) | Mean (SD)/n(Column %) Males | Mean (SD)/n(Column %) Females | p-Value | Mean (SD)/ n(Column %) with Children | Mean (SD)/ n(Column %) without Children | p-Value |
|---|---|---|---|---|---|---|---|
| Self-reported BMI (n = 362) a | |||||||
| Overall (n = 362) | 24.7 (4.5) | 25.3 (3.9) | 24.6 (4.7) | 0.167 | 26.2 (4.5) | 23.9 (4.4) | <0.001 |
| Underweight <18.49 (n = 12) | 12 (3.3%) | 2 (2.3%) | 10 (3.6%) | 0.011 | - | 12 (5.3%) | <0.001 |
| Healthy weight 18.5–24.99 (n = 201) | 201 (55.5%) | 39 (44.8%) | 162 (58.9%) | 59 (45.0%) d | 138 (61.1%) d | ||
| Overweight 25.0–29.99 (n = 103) | 103 (28.5%) | 37 (42.5%) | 66 (24.0%) | 48 (36.6%) | 55 (24.3%) | ||
| Living with obesity ≥30 (n = 46) | 46 (12.7%) | 9 (10.3%) | 37 (13.5%) | 24 (18.3%) d | 21 (9.3%) d | ||
| Self-perceived weight (n = 383) | |||||||
| Underweight (n = 17) | 17 (4.4%) | 4 (4.5%) | 13 (4.4%) | 0.156 | 3 (2.1%) | 14 (5.9%) | <0.001 |
| About the right weight (n = 194) | 194 (50.7%) | 52 (58.4%) | 142 (48.3%) | 49 (34.8%) d | 142 (59.9%) d | ||
| Slightly overweight (n = 133) | 133 (34.7%) | 29 (32.6%) | 104 (35.4%) | 66 (46.8%) d | 65 (27.4%) d | ||
| Very overweight (n = 39) | 39 (10.2%) | 4 (4.5%) | 35 (11.9%) | 23 (16.3%) | 16 (6.8%) | ||
| Vitamin and mineral supplement use (n = 384) | |||||||
| Yes (n = 164) | 164 (42.7%) | 30 (33.7%) | 134 (45.4%) | 0.066 | 59 (42.1%) d | 102 (42.7%) d | 1.000 |
| No (n = 220) | 220 (57.3%) | 59 (66.3%) | 161 (54.6%) | 81 (57.9%) d | 137 (57.3%) d | ||
| ECI score (n = 382) | |||||||
| Overall (n = 382) | 13.3 (2.8) | 12.9 (2.9) | 13.4 (2.7) | 0.127 | 13.7 (2.7) | 13.1 (2.8) | 0.037 |
| Tertile 1 (n = 137) b | 137 (35.9%) | 39 (44.8%) | 98 (33.2%) | 0.067 | 42 (29.8%) d | 94 (39.8%) d | 0.102 |
| Tertile 2 (n = 107) | 107 (28.0%) | 17 (19.5%) | 90 (30.5%) | 40 (28.4%) d | 65 (27.5%) d | ||
| Tertile 3 (n = 138) | 138 (36.1%) | 31 (35.6%) | 107 (36.3%) | 59 (41.8%) d | 77 (32.6%) d | ||
| In the past week, on how many days have you done a total of 30 min or more of physical activity? (n = 385) | |||||||
| Overall ( = 385) | 3.0 (2.0) | 3.3 (1.8) | 2.9 (2.0) | 0.116 | 2.7 (2.0) | 3.1 (1.9) | 0.082 |
| None (n = 55) | 55 (14.3%) | 8 (9.0%) | 47 (15.9%) | 0.227 | 25 (17.7%) | 30 (12.6%) | 0.217 |
| <5 (n = 236) | 236 (61.3%) | 56 (62.9%) | 180 (60.8%) | 87 (61.7%) d | 145 (60.7%) d | ||
| ≥5 (n = 121) | 94 (24.4%) | 25 (28.1%) | 69 (23.3%) | 29 (20.6%) d | 64 (26.8%) d | ||
| Smoking Status (n = 382) | |||||||
| Never smoked (n = 268) | 268 (70.2%) | 53 (60.2%) | 215 (73.1%) | 0.063 | 97 (69.8%) d | 168 (70.6%) d | <0.001 |
| Former smoker (n = 55) | 55 (14.4%) | 16 (18.2%) | 39 (13.3%) | 32 (23.0%) d | 22 (9.2%) d | ||
| Current smoker (n = 59) c | 59 (15.4%) | 19 (21.6%) | 40 (13.6%) | 10 (7.2%) d | 48 (20.2%) d | ||
| How often do you normally drink alcohol? (n = 385) | |||||||
| Never (n = 54) | 54 (14.0%) | 5 (5.6%) | 49 (16.6%) | 0.031 | 21 (14.9%) | 33 (13.8%) | <0.001 |
| Occasionally (n = 183) | 183 (47.5%) | 41 (46.1%) | 142 (48.0%) | 49 (34.8%) d | 131 (54.8%) d | ||
| 1–2 times a week (n = 115) | 115 (29.9%) | 34 (38.2%) | 81 (27.4%) | 49 (34.8%) d | 64 (26.8%) d | ||
| 3–7 times a week (n = 33) | 33 (8.6%) | 9 (10.1%) | 24 (8.1%) | 22 (15.6%) | 11 (4.6%) | ||
| How many alcoholic drinks, on average, would you consume each week? (n = 385) | |||||||
| None (n = 71) | 71 (18.4%) | 12 (13.5%) | 59 (19.9%) | 0.365 | 25 (17.7%) d | 45 (18.8%) d | 0.504 |
| 1–10 (n = 221) | 221 (57.4%) | 53 (59.6%) | 168 (56.8%) | 86 (61.0%) d | 132 (55.2%) d | ||
| 11+ (n = 93) | 93 (24.2%) | 24 (27.0%) | 69 (23.3%) | 30 (21.3%) d | 62 (25.9%) d | ||
| How many hours a night do you sleep? (n = 383) | |||||||
| Meeting sleep requirement (7–9 h and >9 h) (n = 278) | 278 (72.6%) | 63 (71.6%) | 215 (72.9%) | 0.919 | 88 (63.3%) d | 185 (77.4%) d | 0.005 |
| Not meeting sleep requirement (<7 h) (n = 105) | 105 (27.4%) | 25 (28.4%) | 80 (27.1%) | 51 (36.7%) | 54 (22.6%) | ||
| Do you consider yourself to be under continual stress? (n = 382) | |||||||
| Yes (n = 170) | 170 (44.5%) | 32 (36.4%) | 138 (46.9%) | 0.103 | 53 (37.6%) d | 115 (48.7%) d | 0.046 |
| No (n = 212) | 212 (55.5%) | 56 (63.6%) | 156 (53.1%) | 88 (62.4%) d | 121 (51.3%) d | ||
| Preconception Practice for Women (Rated by Women) a | Overall Ranking | Mean (SD) | Preconception Practice for Men (Rated by Men) | Overall Ranking | Mean (SD) |
|---|---|---|---|---|---|
| Stop smoking cigarettes | 1 | 3.18 (2.69) | Stop smoking cigarettes | 1 | 2.68 (2.03) |
| Consume a healthy diet | 2 | 4.30 (2.18) | Consume a healthy diet | 2 | 3.65 (2.04) |
| Take folic acid | 3 | 5.43 (3.67) | Achieve a healthy weight | 3 | 4.96 (2.24) |
| Achieve a healthy weight | 4 | 5.81 (2.76) | Be physically active | 4 | 5.83 (2.47) |
| Address mental health issues | 5 | 6.29 (3.38) | Stop using e-cigarettes | 5 | 5.88 (3.02) |
| Stop using e-cigarettes | 6 | 6.45 (3.39) | Cut out alcohol | 6 | 6.26 (3.08) |
| Cut out alcohol | 7 | 6.88 (3.40) | Address mental health issues | 7 | 6.95 (2.50) |
| Be physically active | 8 | 7.2 (2.69) | Visit a healthcare professional | 8 | 6.69 (3.85) |
| Actively reduce/manage stress | 9 | 7.35 (2.87) | Actively reduce/manage stress | 9 | 6.95 (2.50) |
| Visit a healthcare professional | 10 | 7.7 (3.99) | Take vitamin D | 10 | 7.88 (2.51) |
| Take vitamin D | 11 | 8.03 (2.75) | Get adequate amounts of sleep | 11 | 8.74 (2.20) |
| Get adequate amounts of sleep | 12 | 9.38 (2.43) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cassinelli, E.H.; McClure, A.; Cairns, B.; Griffin, S.; Walton, J.; McKinley, M.C.; Woodside, J.V.; McGowan, L. Exploring Health Behaviours, Attitudes and Beliefs of Women and Men during the Preconception and Interconception Periods: A Cross-Sectional Study of Adults on the Island of Ireland. Nutrients 2023, 15, 3832. https://doi.org/10.3390/nu15173832
Cassinelli EH, McClure A, Cairns B, Griffin S, Walton J, McKinley MC, Woodside JV, McGowan L. Exploring Health Behaviours, Attitudes and Beliefs of Women and Men during the Preconception and Interconception Periods: A Cross-Sectional Study of Adults on the Island of Ireland. Nutrients. 2023; 15(17):3832. https://doi.org/10.3390/nu15173832
Chicago/Turabian StyleCassinelli, Emma H., Abby McClure, Ben Cairns, Sally Griffin, Janette Walton, Michelle C. McKinley, Jayne V. Woodside, and Laura McGowan. 2023. "Exploring Health Behaviours, Attitudes and Beliefs of Women and Men during the Preconception and Interconception Periods: A Cross-Sectional Study of Adults on the Island of Ireland" Nutrients 15, no. 17: 3832. https://doi.org/10.3390/nu15173832
APA StyleCassinelli, E. H., McClure, A., Cairns, B., Griffin, S., Walton, J., McKinley, M. C., Woodside, J. V., & McGowan, L. (2023). Exploring Health Behaviours, Attitudes and Beliefs of Women and Men during the Preconception and Interconception Periods: A Cross-Sectional Study of Adults on the Island of Ireland. Nutrients, 15(17), 3832. https://doi.org/10.3390/nu15173832







