Vitamin D Status, Vitamin D Receptor Polymorphisms, and the Risk of Incident Rosacea: Insights from Mendelian Randomization and Cohort Study in the UK Biobank
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Assessment of Serum 25OHD
2.3. Assessment of Rosacea
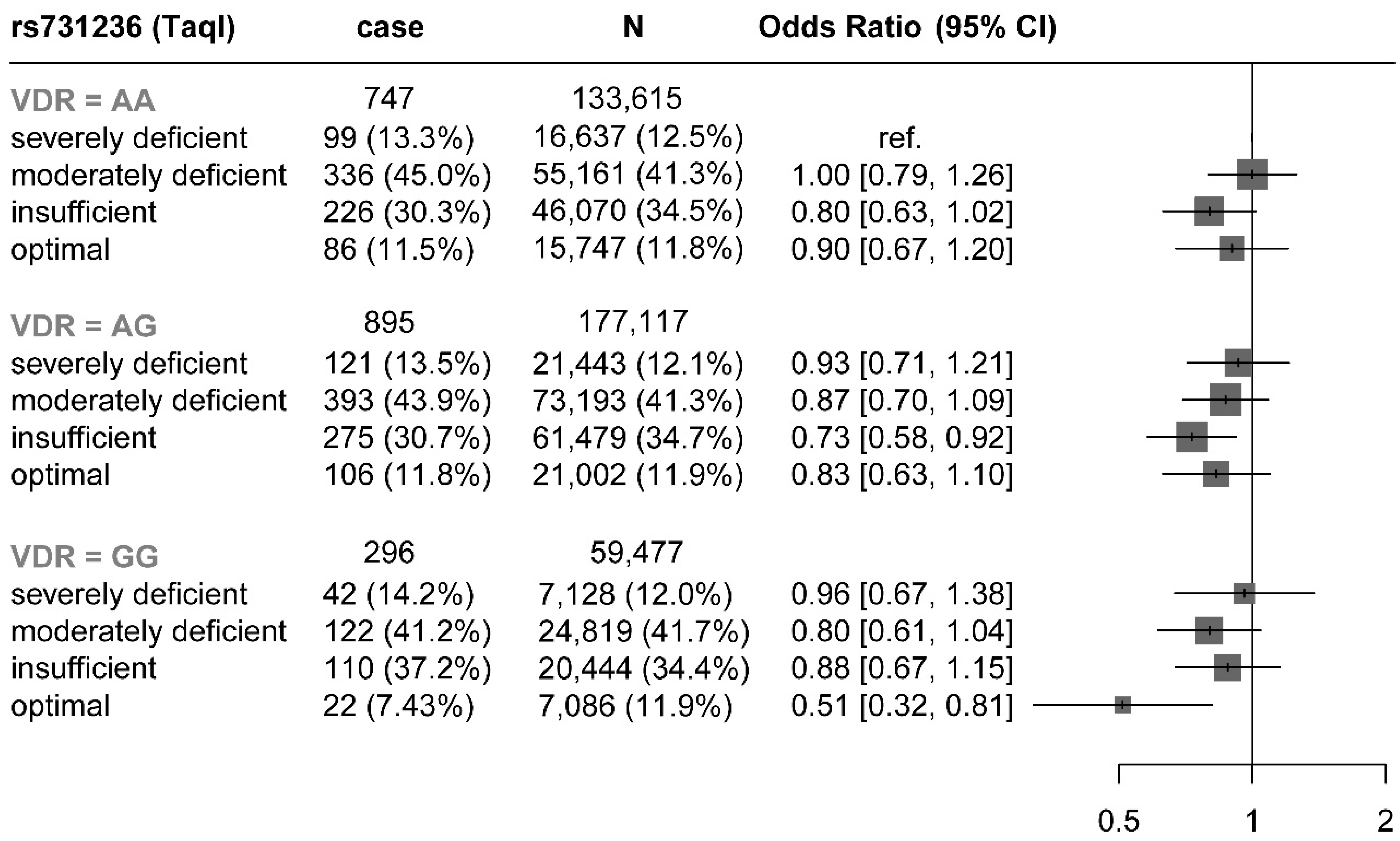
2.4. Polymorphisms in VDR
2.5. Assessment of Covariates
2.6. Statistical Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gether, L.; Overgaard, L.K.; Egeberg, A.; Thyssen, J.P. Incidence and Prevalence of Rosacea: A Systematic Review and Meta-Analysis. Br. J. Dermatol. 2018, 179, 282–289. [Google Scholar] [CrossRef]
- Aksoy, B.; Altaykan-Hapa, A.; Egemen, D.; Karagöz, F.; Atakan, N. The Impact of Rosacea on Quality of Life: Effects of Demographic and Clinical Characteristics and Various Treatment Modalities. Br. J. Dermatol. 2010, 163, 719–725. [Google Scholar] [CrossRef]
- Salamon, M.; Chodkiewicz, J.; Sysa-Jedrzejowska, A.; Wozniacka, A. Quality of life in patients with rosacea. Prz. Lek. 2008, 65, 385–389. [Google Scholar]
- Antal, A.S.; Dombrowski, Y.; Koglin, S.; Ruzicka, T.; Schauber, J. Impact of Vitamin D3 on Cutaneous Immunity and Antimicrobial Peptide Expression. Dermato-Endocrinology 2011, 3, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Christakos, S.; Dhawan, P.; Verstuyf, A.; Verlinden, L.; Carmeliet, G. Vitamin D: Metabolism, Molecular Mechanism of Action, and Pleiotropic Effects. Physiol. Rev. 2016, 96, 365–408. [Google Scholar] [CrossRef]
- DeLuca, H.F. Overview of General Physiologic Features and Functions of Vitamin D. Am. J. Clin. Nutr. 2004, 80, 1689S–1696S. [Google Scholar] [CrossRef]
- Park, B.W.; Ha, J.M.; Cho, E.B.; Jin, J.K.; Park, E.J.; Park, H.R.; Kang, H.J.; Ko, S.H.; Kim, K.H.; Kim, K.J. A Study on Vitamin D and Cathelicidin Status in Patients with Rosacea: Serum Level and Tissue Expression. Ann. Dermatol. 2018, 30, 136–142. [Google Scholar] [CrossRef]
- Ekiz, O.; Balta, I.; Sen, B.B.; Dikilitaş, M.C.; Ozuğuz, P.; Rifaioğlu, E.N. Vitamin D Status in Patients with Rosacea. Cutan. Ocul. Toxicol. 2014, 33, 60–62. [Google Scholar] [CrossRef]
- Akdogan, N.; Alli, N.; Incel Uysal, P.; Candar, T. Role of Serum 25-Hydroxyvitamin D Levels and Vitamin D Receptor Gene Polymorphisms in Patients with Rosacea: A Case-Control Study. Clin. Exp. Dermatol. 2019, 44, 397–403. [Google Scholar] [CrossRef]
- Valdivielso, J.M.; Fernandez, E. Vitamin D Receptor Polymorphisms and Diseases. Clin. Chim. Acta 2006, 371, 1–12. [Google Scholar] [CrossRef]
- Pike, J.W.; Meyer, M.B. The Vitamin D Receptor: New Paradigms for the Regulation of Gene Expression by 1,25-Dihydroxyvitamin D3. Rheum. Dis. Clin. N. Am. 2012, 38, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Fu, L.; Juras, D.J.; Karmali, M.; Wong, B.Y.L.; Gozdzik, A.; Cole, D.E.C. Common Variants of the Vitamin D Binding Protein Gene and Adverse Health Outcomes. Crit. Rev. Clin. Lab. Sci. 2013, 50, 1–22. [Google Scholar] [CrossRef]
- Jones, G.; Prosser, D.E.; Kaufmann, M. Cytochrome P450-Mediated Metabolism of Vitamin D. J. Lipid Res. 2014, 55, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK Biobank: An Open Access Resource for Identifying the Causes of a Wide Range of Complex Diseases of Middle and Old Age. PLoS Med. 2015, 12, e1001779. [Google Scholar] [CrossRef]
- Chen, X.; Wan, Z.; Geng, T.; Zhu, K.; Li, R.; Lu, Q.; Lin, X.; Liu, S.; Chen, L.; Guo, Y.; et al. Vitamin D Status, Vitamin D Receptor Polymorphisms, and Risk of Microvascular Complications Among Individuals with Type 2 Diabetes: A Prospective Study. Diabetes Care 2022, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Fry, D.; Almond, R. UK Biobank Biomarker Project Companion Document to Accompany Serum Biomarker Data. UK Biobank Showc. 2019, 1, 2019. [Google Scholar]
- International Statistical Classification of Diseases and Related Health Problems, 5th ed.; 10th revision; WHO: Geneva, Switzerland, 2016.
- Zmuda, J.M.; Cauley, J.A.; Ferrell, R.E. Molecular Epidemiology of Vitamin D Receptor Gene Variants. Epidemiol. Rev. 2000, 22, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Endocrine Society Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Manousaki, D.; Mitchell, R.; Dudding, T.; Haworth, S.; Harroud, A.; Forgetta, V.; Shah, R.L.; Luan, J.A.; Langenberg, C.; Timpson, N.J.; et al. Genome-wide Association Study for Vitamin D Levels Reveals 69 Independent Loci. Am. J. Hum. Genet. 2020, 106, 327–337. [Google Scholar] [CrossRef]
- Kurki, M.I.; Karjalainen, J.; Palta, P.; Sipilä, T.P.; Kristiansson, K.; Donner, K.; Reeve, M.P.; Laivuori, H.; Aavikko, M.; Kaunisto, M.A.; et al. FinnGen: Unique genetic insights from combining isolated population and national health register data. medRxiv 2022. [Google Scholar] [CrossRef]
- Revez, J.A.; Lin, T.; Qiao, Z.; Xue, A.; Holtz, Y.; Zhu, Z.; Zeng, J.; Wang, H.; Sidorenko, J.; Kemper, K.E.; et al. Genome-wide association study identifies 143 loci associated with 25 hydroxyvitamin D concentration. Nat. Commun. 2020, 11, 1647. [Google Scholar] [CrossRef] [PubMed]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Burgess, S. Sample size and power calculations in Mendelian randomization with a single instrumental variable and a binary outcome. Int. J. Epidemiol. 2014, 43, 922–929. [Google Scholar] [CrossRef]
- Doe, P.T.; Asiedu, A.; Acheampong, J.W.; Rowland Payne, C.M. Skin Diseases in Ghana and the UK. Int. J. Dermatol. 2001, 40, 323–326. [Google Scholar] [CrossRef]
- Zaki, M.; Kamal, S.; Basha, W.A.; Youness, E.; Ezzat, W.; El-Bassyouni, H.; Amr, K. Association of Vitamin D Receptor Gene Polymorphism (VDR) with Vitamin D Deficiency, Metabolic and Inflammatory Markers in Egyptian Obese Women. Genes Dis. 2017, 4, 176–182. [Google Scholar] [CrossRef]
- van Etten, E.; Mathieu, C. Immunoregulation by 1,25-Dihydroxyvitamin D3: Basic Concepts. J. Steroid Biochem. Mol. Biol. 2005, 97, 93–101. [Google Scholar] [CrossRef]
- Boonstra, A.; Barrat, F.J.; Crain, C.; Heath, V.L.; Savelkoul, H.F.; O’Garra, A. 1alpha,25-Dihydroxyvitamin D3 Has a Direct Effect on Naive CD4(+) T Cells to Enhance the Development of Th2 Cells. J. Immunol. 2001, 167, 4974–4980. [Google Scholar] [CrossRef] [PubMed]
- Braff, M.H.; Bardan, A.; Nizet, V.; Gallo, R.L. Cutaneous Defense Mechanisms by Antimicrobial Peptides. J. Investig. Dermatol. 2005, 125, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Schauber, J.; Gallo, R.L. Expanding the Roles of Antimicrobial Peptides in Skin: Alarming and Arming Keratinocytes. J. Investig. Dermatol. 2007, 127, 510–512. [Google Scholar] [CrossRef]
- Bikle, D.D.; Chang, S.; Crumrine, D.; Elalieh, H.; Man, M.-Q.; Dardenne, O.; Xie, Z.; Arnaud, R.S.; Feingold, K.; Elias, P.M. Mice Lacking 25OHD 1α-Hydroxylase Demonstrate Decreased Epidermal Differentiation and Barrier Function. J. Steroid Biochem. Mol. Biol. 2004, 89–90, 347–353. [Google Scholar] [CrossRef]
- Jamali, N.; Sorenson, C.M.; Sheibani, N. Vitamin D and Regulation of Vascular Cell Function. Am. J. Physiol. Heart Circ. Physiol. 2018, 314, H753–H765. [Google Scholar] [CrossRef] [PubMed]
- Haas, M.J.; Jafri, M.; Wehmeier, K.R.; Onstead-Haas, L.M.; Mooradian, A.D. Inhibition of Endoplasmic Reticulum Stress and Oxidative Stress by Vitamin D in Endothelial Cells. Free Radic. Biol. Med. 2016, 99, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-H.; Meza, C.A.; Clarke, H.; Kim, J.-S.; Hickner, R.C. Vitamin D and Endothelial Function. Nutrients 2020, 12, 575. [Google Scholar] [CrossRef]
- Schauber, J.; Gallo, R.L. Antimicrobial Peptides and the Skin Immune Defense System. J. Allergy Clin. Immunol. 2008, 122, 261–266. [Google Scholar] [CrossRef]
- Sun, Q.; Pan, A.; Hu, F.B.; Manson, J.E.; Rexrode, K.M. 25-Hydroxyvitamin D Levels and the Risk of Stroke: A Prospective Study and Meta-Analysis. Stroke 2012, 43, 1470–1477. [Google Scholar] [CrossRef]
- Hsu, S.; Hoofnagle, A.N.; Gupta, D.K.; Gutierrez, O.M.; Peralta, C.A.; Shea, S.; Allen, N.B.; Burke, G.; Michos, E.D.; Ix, J.H.; et al. Race, Ancestry, and Vitamin D Metabolism: The Multi-Ethnic Study of Atherosclerosis. J. Clin. Endocrinol. Metab. 2020, 105, e4337–e4350. [Google Scholar] [CrossRef]
- Thiboutot, D.; Anderson, R.; Cook-Bolden, F.; Draelos, Z.; Gallo, R.L.; Granstein, R.D.; Kang, S.; Macsai, M.; Gold, L.S.; Tan, J. Standard Management Options for Rosacea: The 2019 Update by the National Rosacea Society Expert Committee. J. Am. Acad. Dermatol. 2020, 82, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Powe, C.E.; Evans, M.K.; Wenger, J.; Zonderman, A.B.; Berg, A.H.; Nalls, M.; Tamez, H.; Zhang, D.; Bhan, I.; Karumanchi, S.A.; et al. Vitamin D-Binding Protein and Vitamin D Status of Black Americans and White Americans. N. Engl. J. Med. 2013, 369, 1991–2000. [Google Scholar] [CrossRef]

| Variable | Overall | Severely Deficient | Moderately Deficient | Insufficient | Optimal | p-Value 1 |
|---|---|---|---|---|---|---|
| N = 370,209 | N = 45,208 | N = 153,173 | N = 127,993 | N = 43,835 | ||
| Townsend, Mean(SD) | −1.54 (2.94) | −0.63 (3.33) | −1.42 (2.98) | −1.86 (2.74) | −1.93 (2.70) | <0.001 |
| BMI (kg/m2), Mean(SD) | 27.37 (4.74) | 28.55 (5.74) | 27.85 (4.89) | 26.86 (4.23) | 25.95 (3.83) | <0.001 |
| Times (y), Mean(SD) | 13.22 (2.01) | 13.22 (2.29) | 13.25(2.02) | 13.21 (1.92) | 13.16 (1.95) | <0.001 |
| status, n (%) | 0.007 | |||||
| Incident rosacea | 1938 (0.5%) | 262 (0.6%) | 851 (0.6%) | 611 (0.5%) | 214 (0.5%) | |
| Rosacea-free | 368,271 (99%) | 44,946 (99%) | 152,322 (99%) | 127,382 (100%) | 43,621 (100%) | |
| education, n (%) | <0.001 | |||||
| CSEs or equivalent | 20,720 (5.6%) | 2459 (5.4%) | 8333 (5.4%) | 7143 (5.6%) | 2785 (6.4%) | |
| A levels/AS levels or equivalent | 42,200 (11%) | 5257 (12%) | 17,500 (11%) | 14,621 (11%) | 4822 (11%) | |
| College or University degree | 118,709 (32%) | 15,908 (35%) | 51,700 (34%) | 38,982 (30%) | 12,119 (28%) | |
| none of the above | 62,287 (17%) | 7548 (17%) | 24,785 (16%) | 22,014 (17%) | 7940 (18%) | |
| NVQ or HND or HNC or equivalent | 25,104 (6.8%) | 2947 (6.5%) | 10,191 (6.7%) | 8868 (6.9%) | 3098 (7.1%) | |
| O levels/GCSEs or equivalent | 82,196 (22%) | 8984 (20%) | 32,895 (21%) | 29,519 (23%) | 10,798 (25%) | |
| professional qualifications | 18,993 (5.1%) | 2105 (4.7%) | 7769 (5.1%) | 6846 (5.3%) | 2273 (5.2%) | |
| sex, n (%) | 0.5 | |||||
| female | 195,341 (53%) | 23,850 (53%) | 80,605 (53%) | 67,731 (53%) | 23,155 (53%) | |
| male | 174,868 (47%) | 21,358 (47%) | 72,568 (47%) | 60,262 (47%) | 20,680 (47%) | |
| Time out summer, Mean(SD) | 3.81 (2.39) | 3.33 (2.32) | 3.65 (2.35) | 4.00 (2.38) | 4.30 (2.43) | <0.001 |
| Ethnic background, n (%) | <0.001 | |||||
| British | 362,177 (98%) | 41,763 (92%) | 149,733 (98%) | 127,018 (99%) | 43,663 (100%) | |
| Caribbean | 3248 (0.9%) | 1178 (2.6%) | 1561 (1.0%) | 436 (0.3%) | 73 (0.2%) | |
| Indian | 3945 (1.1%) | 2078 (4.6%) | 1505 (1.0%) | 320 (0.3%) | 42 (<0.1%) | |
| White | 363 (<0.1%) | 58 (0.1%) | 161 (0.1%) | 107 (<0.1%) | 37 (<0.1%) | |
| White and Black Caribbean | 476 (0.1%) | 131 (0.3%) | 213 (0.1%) | 112 (<0.1%) | 20 (<0.1%) | |
| sleeplessness, n (%) | <0.001 | |||||
| never | 90,406 (24%) | 10,922 (24%) | 37,730 (25%) | 31,145 (24%) | 10,609 (24%) | |
| sometimes | 176,065 (48%) | 21,204 (47%) | 72,821 (48%) | 61,325 (48%) | 20,715 (47%) | |
| usually | 103,738 (28%) | 13,082 (29%) | 42,622 (28%) | 35,523 (28%) | 12,511 (29%) | |
| Smoking status, n (%) | <0.001 | |||||
| current | 37,463 (10%) | 7509 (17%) | 15,869 (10%) | 10,388 (8.1%) | 3697 (8.4%) | |
| never | 203,000 (55%) | 23,633 (52%) | 84,589 (55%) | 71,191 (56%) | 23,587 (54%) | |
| previous | 129,746 (35%) | 14,066 (31%) | 52,715 (34%) | 46,414 (36%) | 16,551 (38%) | |
| Alcohol intake frequency, n (%) | <0.001 | |||||
| daily | 78,418 (21%) | 8808 (19%) | 30,886 (20%) | 28,007 (22%) | 10,717 (24%) | |
| month to week | 227,989 (62%) | 25,171 (56%) | 94,248 (62%) | 81,032 (63%) | 27,538 (63%) | |
| never | 63,802 (17%) | 11,229 (25%) | 28,039 (18%) | 18,954 (15%) | 5580 (13%) | |
| Age at recruitment, Mean(SD) | 56.65 (8.07) | 55.09 (8.09) | 56.34 (8.07) | 57.34 (7.97) | 57.30 (8.04) | <0.001 |
| income, n (%) | <0.001 | |||||
| 18,000 to 30,999 | 95,780 (26%) | 10,909 (24%) | 39,038 (25%) | 34,004 (27%) | 11,829 (27%) | |
| 31,000 to 51,999 | 97,560 (26%) | 11,547 (26%) | 40,685 (27%) | 33,784 (26%) | 11,544 (26%) | |
| 52,000 to 100,000 | 75,668 (20%) | 8905 (20%) | 31,970 (21%) | 25,948 (20%) | 8845 (20%) | |
| greater than 100,000 | 19,890 (5.4%) | 2111 (4.7%) | 8248 (5.4%) | 7042 (5.5%) | 2489 (5.7%) | |
| less than 18,000 | 81,311 (22%) | 11,736 (26%) | 33,232 (22%) | 27,215 (21%) | 9128 (21%) | |
| MET, Mean(SD) | 44.77 (45.34) | 37.59 (42.08) | 42.24 (43.96) | 47.73 (46.28) | 52.38 (48.69) | <0.001 |
| 25OHD supplement, n (%) | 67,728 (18%) | 3890 (8.6%) | 23,392 (15%) | 29,149 (23%) | 11,297 (26%) | <0.001 |
| Serum 25OHD (nmol/L), Mean(SD) | 49.63 (21.07) | 19.46 (3.85) | 38.01 (7.09) | 61.11 (6.95) | 87.82 (12.79) | <0.001 |
| 25OHD quantile (nmol/L), n (%) | <0.001 | |||||
| Q1 (<33.5) | 92,710 (25%) | 45,208 (100%) | 47,502 (31%) | 0 (0%) | 0 (0%) | |
| Q2 (33.5 to 48.0) | 92,818 (25%) | 0 (0%) | 92,818 (61%) | 0 (0%) | 0 (0%) | |
| Q3 (48.0 to 63.4) | 92,607 (25%) | 0 (0%) | 12,853 (8.4%) | 79,754 (62%) | 0 (0%) | |
| Q4 (>63.4) | 92,074 (25%) | 0 (0%) | 0 (0%) | 48,239 (38%) | 43,835 (100%) | |
| taql, n (%) | 0.018 | |||||
| GG | 59,477 (16%) | 7128 (16%) | 24,819 (16%) | 20,444 (16%) | 7086 (16%) | |
| AG | 177,117 (48%) | 21,443 (47%) | 73,193 (48%) | 61,479 (48%) | 21,002 (48%) | |
| AA | 133,615 (36%) | 16,637 (37%) | 55,161 (36%) | 46,070 (36%) | 15,747 (36%) | |
| apal, n (%) | 0.3 | |||||
| AA | 103,294 (28%) | 12,762 (28%) | 42,870 (28%) | 35,426 (28%) | 12,236 (28%) | |
| AC | 184,352 (50%) | 22,409 (50%) | 76,280 (50%) | 63,847 (50%) | 21,816 (50%) | |
| CC | 82,563 (22%) | 10,037 (22%) | 34,023 (22%) | 28,720 (22%) | 9783 (22%) | |
| bsml, n (%) | 0.4 | |||||
| TT | 61,293 (17%) | 7497 (17%) | 25,574 (17%) | 20,974 (16%) | 7248 (17%) | |
| TC | 178,118 (48%) | 21,657 (48%) | 73,607 (48%) | 61,740 (48%) | 21,114 (48%) | |
| CC | 130,798 (35%) | 16,054 (36%) | 53,992 (35%) | 45,279 (35%) | 15,473 (35%) | |
| fokl, n (%) | <0.001 | |||||
| GG | 141,007 (38%) | 17,894 (40%) | 58,231 (38%) | 48,326 (38%) | 16,556 (38%) | |
| AG | 174,736 (47%) | 20,948 (46%) | 72,536 (47%) | 60,683 (47%) | 20,569 (47%) | |
| AA | 54,466 (15%) | 6366 (14%) | 22,406 (15%) | 18,984 (15%) | 6710 (15%) |
| Variables | Person-Years | Incident Rate | Incident Rosacea | Unadjusted Model | Fully Adjusted Models | ||
|---|---|---|---|---|---|---|---|
| HR (95%CI) | p-Value | HR (95%CI) | p-Value | ||||
| Serum 25OHD (nmol/L) | |||||||
| severely deficient | 597,727 | 0.438 | 262 (13.5%) | Ref. | Ref. | Ref. | Ref. |
| moderately deficient | 2,030,024 | 0.419 | 851 (43.9%) | 0.95 [0.83;1.09] | 0.495 | 0.94 [0.82;1.08] | 0.383 |
| insufficient | 1,690,778 | 0.361 | 611 (31.5%) | 0.82 [0.71;0.95] | 0.007 | 0.81 [0.70;0.94] | 0.006 |
| optimal | 577,049 | 0.371 | 214 (11.0%) | 0.84 [0.70;1.00] | 0.056 | 0.83 [0.69;1.01] | 0.059 |
| p.trend | 0.006 | p.trend | 0.010 | ||||
| 25OHD (nmol/L) quantile | |||||||
| Q1 (<33.5) | 1,228,324 | 0.444 | 545 (28.1%) | Ref. | Ref. | Ref. | Ref. |
| Q2 (33.5 to 48.0) | 1,229,421 | 0.404 | 497 (25.6%) | 0.91 [0.80;1.03] | 0.120 | 0.90 [0.79;1.02] | 0.090 |
| Q3 (48.0 to 63.4) | 1,223,889 | 0.376 | 460 (23.7%) | 0.84 [0.74;0.95] | 0.007 | 0.84 [0.74;0.95] | 0.006 |
| Q4 (>63.4) | 1,213,944 | 0.359 | 436 (22.5%) | 0.80 [0.71;0.91] | 0.001 | 0.80 [0.70;0.91] | <0.001 |
| p.trend | 0.003 | p.trend | 0.006 | ||||
| 25OHD (per SD) | 4,895,578 | 0.396 | 1938 | 0.89 [0.83;0.95] | <0.001 | 0.88 [0.82;0.95] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mao, R.; Zhou, G.; Jing, D.; Liu, H.; Shen, M.; Li, J. Vitamin D Status, Vitamin D Receptor Polymorphisms, and the Risk of Incident Rosacea: Insights from Mendelian Randomization and Cohort Study in the UK Biobank. Nutrients 2023, 15, 3803. https://doi.org/10.3390/nu15173803
Mao R, Zhou G, Jing D, Liu H, Shen M, Li J. Vitamin D Status, Vitamin D Receptor Polymorphisms, and the Risk of Incident Rosacea: Insights from Mendelian Randomization and Cohort Study in the UK Biobank. Nutrients. 2023; 15(17):3803. https://doi.org/10.3390/nu15173803
Chicago/Turabian StyleMao, Rui, Guowei Zhou, Danrong Jing, Hong Liu, Minxue Shen, and Ji Li. 2023. "Vitamin D Status, Vitamin D Receptor Polymorphisms, and the Risk of Incident Rosacea: Insights from Mendelian Randomization and Cohort Study in the UK Biobank" Nutrients 15, no. 17: 3803. https://doi.org/10.3390/nu15173803
APA StyleMao, R., Zhou, G., Jing, D., Liu, H., Shen, M., & Li, J. (2023). Vitamin D Status, Vitamin D Receptor Polymorphisms, and the Risk of Incident Rosacea: Insights from Mendelian Randomization and Cohort Study in the UK Biobank. Nutrients, 15(17), 3803. https://doi.org/10.3390/nu15173803






