Evaluation of a New ‘Mix-In’ Style Glycomacropeptide-Based Protein Substitute for Food and Drinks in Patients with Phenylketonuria and Tyrosinemia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Recruitment and Study Population
2.3. Study Intervention and Study Product
2.4. Outcomes
2.4.1. Adherence to the Intervention
2.4.2. Gastrointestinal Tolerance
2.4.3. Palatability and Convenience
2.4.4. Metabolic Control and Safety
2.5. Statistics
3. Results
3.1. Recruitment and Patient Characteristics
3.2. Adherence to the Protein Substitute
3.3. Gastrointestinal Tolerance
3.4. Palatability and Convenience
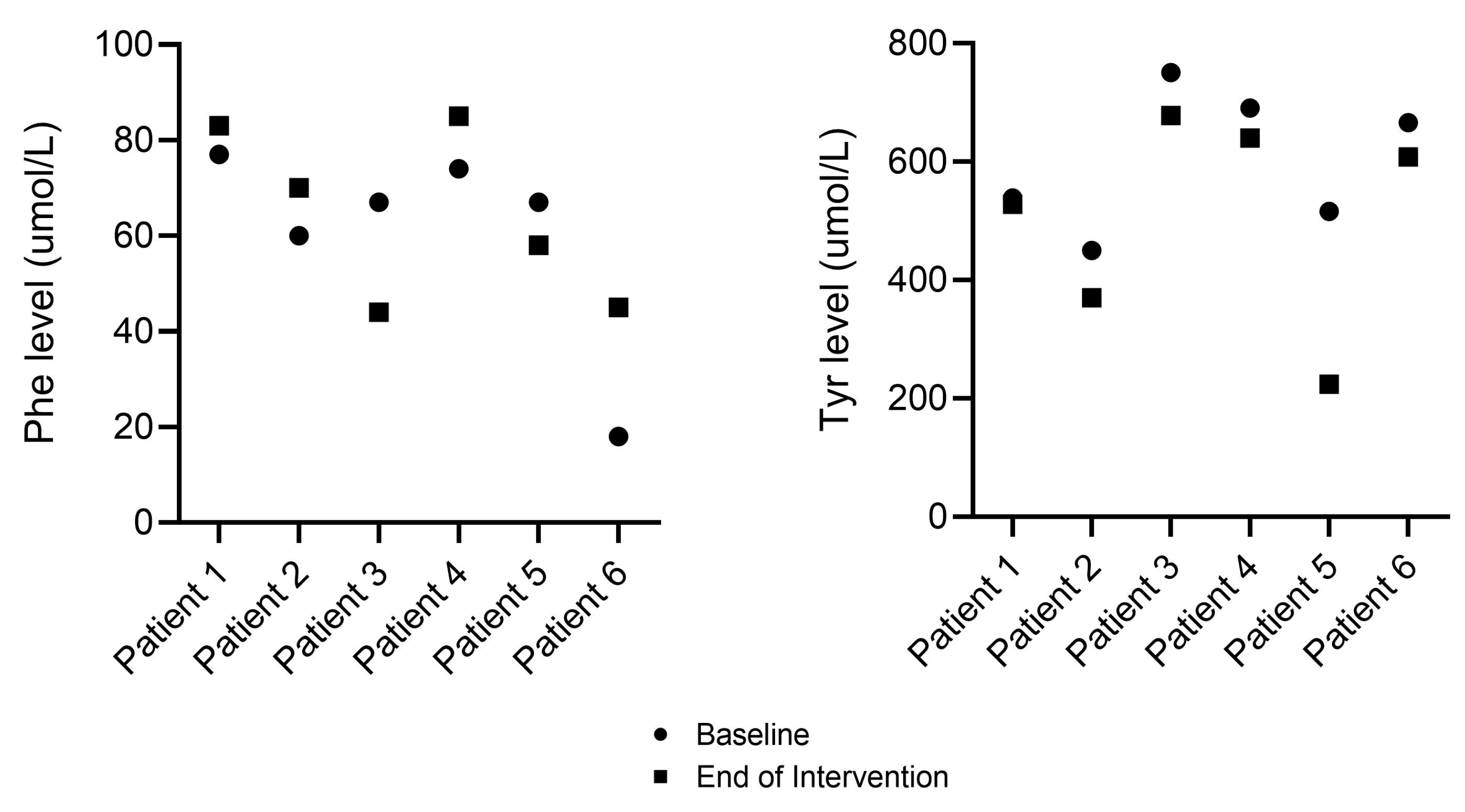
3.5. Metabolic Control and Safety
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| AVERAGE CONTENTS (per 12.5 g Serving) | PKU GMP-PS | TYR GMP-PS | |
|---|---|---|---|
| Energy | kcal | 42 | 40 |
| kJ | 177 | 172 | |
| Protein Equivalent | g | 10 | 10 |
| Carbohydrate | g | 0.43 | 0.10 |
| sugars | g | 0.04 | 0.01 |
| Fat | g | 0 | 0 |
| Fibre | g | 0 | 0 |
| Minerals | |||
| sodium | mg (mmol) | 141 (6.1) | 141 (6.1) |
| potassium | mg (mmol) | 124 (3.2) | 124 (3.2) |
| chloride | mg (mmol) | <8.8 (<0.25) | <8.8 (<0.25) |
| calcium | mg (mmol) | <16.3 (<0.41) | <16.3 (<0.41) |
| phosphorus | mg (mmol PO4) | 40.0 (1.3) | 40.0 (1.3) |
| magnesium | mg (mmol) | 0.8 (0.03) | 0.8 (0.03) |
| iron | mg | 0.02 | 0.02 |
| zinc | mg | 0.01 | 0.01 |
| selenium | μg | 1.2 | 1.2 |
| chromium | μg | 0.40 | 0.40 |
| iodine | μg | 1.5 | 1.5 |
| Amino Acids | |||
| L-alanine | g | 0.40 | 0.40 |
| L-arginine | g | 0.50 | 0.48 |
| L-aspartic acid | g | 0.60 | 0.59 |
| L-cystine | g | 0.29 | 0.14 |
| L-glutamic acid | g | 1.3 | 1.3 |
| Glycine | g | 0.07 | 0.94 |
| L-histidine | g | 0.40 | 0.49 |
| L-isoleucine | g | 0.73 | 0.72 |
| L-leucine | g | 1.5 | 1.4 |
| L-lysine | g | 0.43 | 0.78 |
| L-methionine | g | 0.13 | 0.23 |
| L-phenylalanine | mg | 18.0 | 18.0 |
| L-proline | g | 0.80 | 0.77 |
| L-serine | g | 0.50 | 0.51 |
| L-threonine | g | 1.1 | 1.1 |
| L-tryptophan | g | 0.24 | 0.24 |
| L-tyrosine | g | 1.0 | 3.5 |
| L-valine | g | 0.87 | 0.88 |
| L-carnitine | mg | 10.0 | 10.0 |
| Taurine | mg | 30.0 | 30.0 |
| Others | |||
| osmolality | mOsm/kg H2O | 170 | 250 |
| osmolarity | mOsmol/L | 160 | 240 |
| potential renal solute load | mOsmol/L | 351 | 351 |
References
- Chakrapani, A.; Gissen, P.; McKiernan, P. Disorders of tyrosine metabolism. In Inborn Metabolic Diseases: Diagnosis and Treatment; Springer: Berlin/Heidelberg, Germany, 2012; pp. 265–276. [Google Scholar]
- Vockley, J.; Andersson, H.C.; Antshel, K.M.; Braverman, N.E.; Burton, B.K.; Frazier, D.M.; Mitchell, J.; Smith, W.E.; Thompson, B.H.; Berry, S.A.; et al. Phenylalanine hydroxylase deficiency: Diagnosis and management guideline. Genet. Med. 2014, 16, 188–200. [Google Scholar] [CrossRef]
- Acosta, P.; Yannicelli, S. Protein intake affects phenylalanine requirements and growth of infants with phenylketonuria. Acta Paediatr. 1994, 83, 66–67. [Google Scholar] [CrossRef] [PubMed]
- Kindt, E.; Motzfeldt, K.; Halvorsen, S.; Lie, S.O. Protein requirements in infants and children: A longitudinal study of children treated for phenylketonuria. Am. J. Clin. Nutr. 1983, 37, 778–785. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, E.L.; Ney, D.M. Nutritional Management of Phenylketonuria. Ann. Nestle 2010, 68, 58–69. [Google Scholar] [CrossRef] [PubMed]
- De Laet, C.; Dionisi-Vici, C.; Leonard, J.V.; McKiernan, P.; Mitchell, G.; Monti, L.; de Baulny, H.O.; Pintos-Morell, G.; Spiekerkötter, U. Recommendations for the management of tyrosinaemia type 1. Orphanet J. Rare Dis. 2013, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Morrow, G.; Tanguay, R.M. Biochemical and Clinical Aspects of Hereditary Tyrosinemia Type 1. Adv. Exp. Med. Biol. 2017, 959, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Van Wegberg, A.M.J.; Macdonald, A.; Ahring, K.; BéLanger-Quintana, A.; Blau, N.; Bosch, A.M.; Burlina, A.; Campistol, J.; Feillet, F.; Giżewska, M.; et al. The complete European guidelines on phenylketonuria: Diagnosis and treatment. Orphanet J. Rare Dis. 2017, 12, 162. [Google Scholar] [CrossRef]
- Firman, S.; Witard, O.C.; O’Keeffe, M.; Ramachandran, R. Dietary protein and protein substitute requirements in adults with phenylketonuria: A review of the clinical guidelines. Clin. Nutr. 2020, 40, 702–709. [Google Scholar] [CrossRef]
- Brown, C.S.; Lichter-Konecki, U. Phenylketonuria (PKU): A problem solved? Mol. Genet. Metab. Rep. 2016, 6, 8–12. [Google Scholar] [CrossRef]
- McWhorter, N.; Ndugga-Kabuye, M.K.; Puurunen, M.; Ernst, S.L. Complications of the Low Phenylalanine Diet for Patients with Phenylketonuria and the Benefits of Increased Natural Protein. Nutrients 2022, 14, 4960. [Google Scholar] [CrossRef]
- Van Spronsen, F.J.; van Rijn, M.; Meyer, U.; Das, A.M. Dietary considerations in tyrosinemia type I. In Hereditary Tyrosinemia: Pathogenesis, Screening and Management; Springer: Cham, Switzerland, 2017; pp. 197–204. [Google Scholar]
- Giovannini, M.; Verduci, E.; Salvatici, E.; Paci, S.; Riva, E. Phenylketonuria: Nutritional advances and challenges. Nutr. Metab. 2012, 9, 7. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.H.; Cunningham, A.C.; Mofidi, S.; Douglas, T.D.; Frazier, D.M.; Hook, D.G.; Jeffers, L.; McCune, H.; Moseley, K.D.; Ogata, B.; et al. Updated, web-based nutrition management guideline for PKU: An evidence and consensus based approach. Mol. Genet. Metab. 2016, 118, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Walter, J.; White, F.; Hall, S.; MacDonald, A.; Rylance, G.; Boneh, A.; Francis, D.; Shortland, G.; Schmidt, M.; Vail, A. How practical are recommendations for dietary control in phenylketonuria? Lancet 2002, 360, 55–57. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, A.; Gokmen-Ozel, H.; van Rijn, M.; Burgard, P. The reality of dietary compliance in the management of phenylketonuria. J. Inherit. Metab. Dis. 2010, 33, 665–670. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, A.; van Rijn, M.; Feillet, F.; Lund, A.M.; Bernstein, L.; Bosch, A.; Gizewska, M.; van Spronsen, F.J. Adherence Issues in Inherited Metabolic Disorders Treated by Low Natural Protein Diets. Ann. Nutr. Metab. 2012, 61, 289–295. [Google Scholar] [CrossRef] [PubMed]
- González-Lamuño, D.; Sánchez-Pintos, P.; Andrade, F.; Couce, M.L.; Aldámiz-Echevarría, L. Treatment adherence in tyrosinemia type 1 patients. Orphanet J. Rare Dis. 2021, 16, 256. [Google Scholar] [CrossRef] [PubMed]
- Blau, N.; van Spronsen, F.J.; Levy, H.L. Phenylketonuria. Lancet 2010, 376, 1417–1427. [Google Scholar] [CrossRef]
- Levy, H.; Lamppu, D.; Anastosoaie, V.; Baker, J.L.; DiBona, K.; Hawthorne, S.; Lindenberger, J.; Kinch, D.; Seymour, A.; McIlduff, M.; et al. 5-year retrospective analysis of patients with phenylketonuria (PKU) and hyperphenylalaninemia treated at two specialized clinics. Mol. Genet. Metab. 2019, 129, 177–185. [Google Scholar] [CrossRef]
- Dean, A.J.; Walters, J.; Hall, A. A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Arch. Dis. Child. 2010, 95, 717–723. [Google Scholar] [CrossRef]
- Salema, N.-E.M.; Elliott, R.A.; Glazebrook, C. A Systematic Review of Adherence-Enhancing Interventions in Adolescents Taking Long-term Medicines. J. Adolesc. Health 2011, 49, 455–466. [Google Scholar] [CrossRef]
- Ford, S.; O’Driscoll, M.; MacDonald, A. Living with Phenylketonuria: Lessons from the PKU community. Mol. Genet. Metab. Rep. 2018, 17, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Jurecki, E.; Cederbaum, S.; Kopesky, J.; Perry, K.; Rohr, F.; Sanchez-Valle, A.; Viau, K.; Sheinin, M.; Cohen-Pfeffer, J. Adherence to clinic recommendations among patients with phenylketonuria in the United States. Mol. Genet. Metab. 2017, 120, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Bosch, A.M.; Burlina, A.; Cunningham, A.; Bettiol, E.; Moreau-Stucker, F.; Koledova, E.; Benmedjahed, K.; Regnault, A. Assessment of the impact of phenylketonuria and its treatment on quality of life of patients and parents from seven European countries. Orphanet J. Rare Dis. 2015, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- Lowe, T.B.; DeLuca, J.; Arnold, G.L. Similarities and differences in key diagnosis, treatment, and management approaches for PAH deficiency in the United States and Europe. Orphanet J. Rare Dis. 2020, 15, 266. [Google Scholar] [CrossRef] [PubMed]
- Ney, D.M.; Gleason, S.T.; van Calcar, S.C.; MacLeod, E.L.; Nelson, K.L.; Etzel, M.R.; Rice, G.M.; Wolff, J.A. Nutritional management of PKU with glycomacropeptide from cheese whey. J. Inherit. Metab. Dis. 2008, 32, 32–39. [Google Scholar] [CrossRef]
- Lim, K.; van Calcar, S.C.; Nelson, K.L.; Gleason, S.T.; Ney, D.M. Acceptable low-phenylalanine foods and beverages can be made with glycomacropeptide from cheese whey for individuals with PKU. Mol. Genet. Metab. 2007, 92, 176–178. [Google Scholar] [CrossRef]
- Ney, D.M.; Etzel, M.R. Designing medical foods for inherited metabolic disorders: Why intact protein is superior to amino acids. Curr. Opin. Biotechnol. 2017, 44, 39–45. [Google Scholar] [CrossRef]
- Ney, D.M.; Stroup, B.M.; Clayton, M.K.; Murali, S.G.; Rice, G.M.; Rohr, F.; Levy, H.L. Glycomacropeptide for nutritional management of phenylketonuria: A randomized, controlled, crossover trial. Am. J. Clin. Nutr. 2016, 104, 334–345. [Google Scholar] [CrossRef]
- Proserpio, C.; Pagliarini, E.; Zuvadelli, J.; Paci, S.; Dionigi, A.R.; Banderali, G.; Cattaneo, C.; Verduci, E. Exploring Drivers of Liking of Low-Phenylalanine Products in Subjects with Phenyilketonuria Using Check-All-That-Apply Method. Nutrients 2018, 10, 1179. [Google Scholar] [CrossRef]
- Pena, M.J.; Pinto, A.; de Almeida, M.F.; Barbosa, C.d.S.; Ramos, P.C.; Rocha, S.; Guimas, A.; Ribeiro, R.; Martins, E.; Bandeira, A.; et al. Continuous use of glycomacropeptide in the nutritional management of patients with phenylketonuria: A clinical perspective. Orphanet J. Rare Dis. 2021, 16, 84. [Google Scholar] [CrossRef]
- Ahring, K.K.; Lund, A.M.; Jensen, E.; Jensen, T.G.; Brøndum-Nielsen, K.; Pedersen, M.; Bardow, A.; Holst, J.J.; Rehfeld, J.F.; Møller, L.B. Comparison of Glycomacropeptide with Phenylalanine Free-Synthetic Amino Acids in Test Meals to PKU Patients: No Significant Differences in Biomarkers, Including Plasma Phe Levels. J. Nutr. Metab. 2018, 2018, 6352919. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, A.; Ferguson, C.; Rylance, G.; Morris, A.A.M.; Asplin, D.; Hall, S.K.; Booth, I.W. Are tablets a practical source of protein substitute in phenylketonuria? Arch. Dis. Child. 2003, 88, 327–329. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, A.; Manji, N.; Evans, S.; Davies, P.; Daly, A.; Hendriksz, C.; Chakrapani, A. Home delivery of dietary products in inherited metabolic disorders reduces prescription and dispensing errors. J. Hum. Nutr. Diet. 2006, 19, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Buist, N.; Prince, A.; Huntington, K.; Tuerck, J.; Waggoner, D. A new amino acid mixture permits new approaches to the treatment of phenylketonuria. Acta Paediatr. 1994, 83, 75–77. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, A.L.S.; Martins, A.M.; Ribeiro, E.M.; Specola, N.; Chiesa, A.; Vilela, D.; Jurecki, E.; Mesojedovas, D.; Schwartz, I.V.D. Burden of phenylketonuria in Latin American patients: A systematic review and meta-analysis of observational studies. Orphanet J. Rare Dis. 2022, 17, 302. [Google Scholar] [CrossRef] [PubMed]
- Cazzorla, C.; Bensi, G.; Biasucci, G.; Leuzzi, V.; Manti, F.; Musumeci, A.; Papadia, F.; Stoppioni, V.; Tummolo, A.; Vendemiale, M.; et al. Living with phenylketonuria in adulthood: The PKU ATTITUDE study. Mol. Genet. Metab. Rep. 2018, 16, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Cotugno, G.; Nicolò, R.; Cappelletti, S.; Goffredo, B.; Vici, C.D.; Di Ciommo, V. Adherence to diet and quality of life in patients with phenylketonuria. Acta Paediatr. 2011, 100, 1144–1149. [Google Scholar] [CrossRef]
- Freehauf, C.; Van Hove, J.L.; Gao, D.; Bernstein, L.; Thomas, J.A. Impact of geographic access to care on compliance and metabolic control in phenylketonuria. Mol. Genet. Metab. 2013, 108, 13–17. [Google Scholar] [CrossRef]
- Vieira, T.A.; Nalin, T.; Krug, B.C.; Bittar, C.M.; Netto, C.B.O.; Schwartz, I.V.D. Adherence to Treatment of Phenylketonuria: A Study in Southern Brazilian Patients. J. Inborn Errors Metab. Screen. 2015, 3, 2326409815579861. [Google Scholar] [CrossRef]
- Malik, S.; NiMhurchadha, S.; Jackson, C.; Eliasson, L.; Weinman, J.; Roche, S.; Walter, J.; Zschocke, J.; Baumgartner, M.; Gibson, K.M.; et al. Treatment Adherence in Type 1 Hereditary Tyrosinaemia (HT1): A Mixed-Method Investigation into the Beliefs, Attitudes and Behaviour of Adolescent Patients, Their Families and Their Health-Care Team. In JIMD Reports; Zschocke, J., Baumgartner, M., Morava, E., Patterson, M., Rahman, S., Peters, V., Eds.; Springer: Berlin/Heidelberg, Germany, 2015; Volume 18, pp. 13–22. [Google Scholar] [CrossRef]
- Burlina, A.; Leuzzi, V.; Spada, M.; Carbone, M.T.; Paci, S.; Tummolo, A. The management of phenylketonuria in adult patients in Italy: A survey of six specialist metabolic centers. Curr. Med. Res. Opin. 2021, 37, 411–421. [Google Scholar] [CrossRef]
- MacDonald, A.; Singh, R.H.; Rocha, J.C.; van Spronsen, F.J. Optimising amino acid absorption: Essential to improve nitrogen balance and metabolic control in phenylketonuria. Nutr. Res. Rev. 2018, 32, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Van Calcar, S.C.; MacLeod, E.L.; Gleason, S.T.; Etzel, M.R.; Clayton, M.K.; Wolff, J.A.; Ney, D.M. Improved nutritional management of phenylketonuria by using a diet containing glycomacropeptide compared with amino acids. Am. J. Clin. Nutr. 2009, 89, 1068–1077. [Google Scholar] [CrossRef]
- Walter, J.; White, F.J. Blood phenylalanine control in adolescents with phenylketonuria. Int. J. Adolesc. Med. Health 2004, 16, 41–46. [Google Scholar] [CrossRef]
- Daly, A.; Evans, S.; Chahal, S.; Santra, S.; Pinto, A.; Gingell, C.; Rocha, J.C.; van Spronsen, F.; Jackson, R.; MacDonald, A. The Effect of Glycomacropeptide versus Amino Acids on Phenylalanine and Tyrosine Variability over 24 Hours in Children with PKU: A Randomized Controlled Trial. Nutrients 2019, 11, 520. [Google Scholar] [CrossRef]


| PKU (n = 12) | TYR (n = 6) | Total (n = 18) | |
|---|---|---|---|
| Age *, years, mean (SD) [range] | 22 (15) [3–45] | 9 (3) [3–12] | 18 (14) [3–45] * |
| Height, cm, mean (SD) | 162.2 (24.6) | 134.9 (29.2) | 155.4 (27.7) |
| Weight, kg, mean (SD) | 64.0 (20.5) | 36.6 (14.7) | 55.9 (22.6) |
| Protein requirements, g/day, mean (SD) | 71.0 (18.8) | 54.7 (17.1) | 65.6 (19.4) |
| Protein from PS, g/day, mean (SD) | 65.4 (16.7) | 48.3 (11.2) | 59.7 (16.9) |
| PS format, n (%) | |||
| Liquid | 6 (50) | 3 (50) | 9 (50) |
| Powder | 4 (33) | 3 (50) | 7 (39) |
| Combination Liquid & Powder | 1 (8.5) | - | 1 (5.5) |
| Combination Liquid & Tablets | 1 (8.5) | - | 1 (5.5) |
| PS characteristics, n (%) | |||
| GMP-PS only | 3 (25) | 1 (17) | 4 (22) |
| AA-PS only | 7 (58) | 5 (83) | 12 (67) |
| Combination of GMP-PS + AA-PS | 2 (17) | - | 2 (11) |
| Metabolic control **, n (%) | PKU (n = 9) | TYR (n = 6) | Total (n = 15) |
| Within target | 7 (78) | - | 7 (46) |
| Above target | 2 (22) | 2 (33) | 4 (27) |
| Fluctuating around target | - | 4 (67) | 4 (27) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delsoglio, M.; Capener, R.; MacDonald, A.; Daly, A.; Ashmore, C.; Donald, S.; Gaff, L.; VanDorp, L.; Skeath, R.; Ellerton, C.; et al. Evaluation of a New ‘Mix-In’ Style Glycomacropeptide-Based Protein Substitute for Food and Drinks in Patients with Phenylketonuria and Tyrosinemia. Nutrients 2023, 15, 3598. https://doi.org/10.3390/nu15163598
Delsoglio M, Capener R, MacDonald A, Daly A, Ashmore C, Donald S, Gaff L, VanDorp L, Skeath R, Ellerton C, et al. Evaluation of a New ‘Mix-In’ Style Glycomacropeptide-Based Protein Substitute for Food and Drinks in Patients with Phenylketonuria and Tyrosinemia. Nutrients. 2023; 15(16):3598. https://doi.org/10.3390/nu15163598
Chicago/Turabian StyleDelsoglio, Marta, Rebecca Capener, Anita MacDonald, Anne Daly, Catherine Ashmore, Sarah Donald, Lisa Gaff, Louise VanDorp, Rachel Skeath, Charlotte Ellerton, and et al. 2023. "Evaluation of a New ‘Mix-In’ Style Glycomacropeptide-Based Protein Substitute for Food and Drinks in Patients with Phenylketonuria and Tyrosinemia" Nutrients 15, no. 16: 3598. https://doi.org/10.3390/nu15163598
APA StyleDelsoglio, M., Capener, R., MacDonald, A., Daly, A., Ashmore, C., Donald, S., Gaff, L., VanDorp, L., Skeath, R., Ellerton, C., Newby, C., Dunning, G., Dale, C., Hunjan, I., White, L., Allen, H., Hubbard, G. P., & Stratton, R. J. (2023). Evaluation of a New ‘Mix-In’ Style Glycomacropeptide-Based Protein Substitute for Food and Drinks in Patients with Phenylketonuria and Tyrosinemia. Nutrients, 15(16), 3598. https://doi.org/10.3390/nu15163598







