Changes in Diet Quality over 10 Years and Subsequent Mortality from Cardiovascular Disease in the Multiethnic Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Dietary Assessment and Calculation of Dietary Quality
2.3. Death Ascertainment
2.4. Statistical Analysis
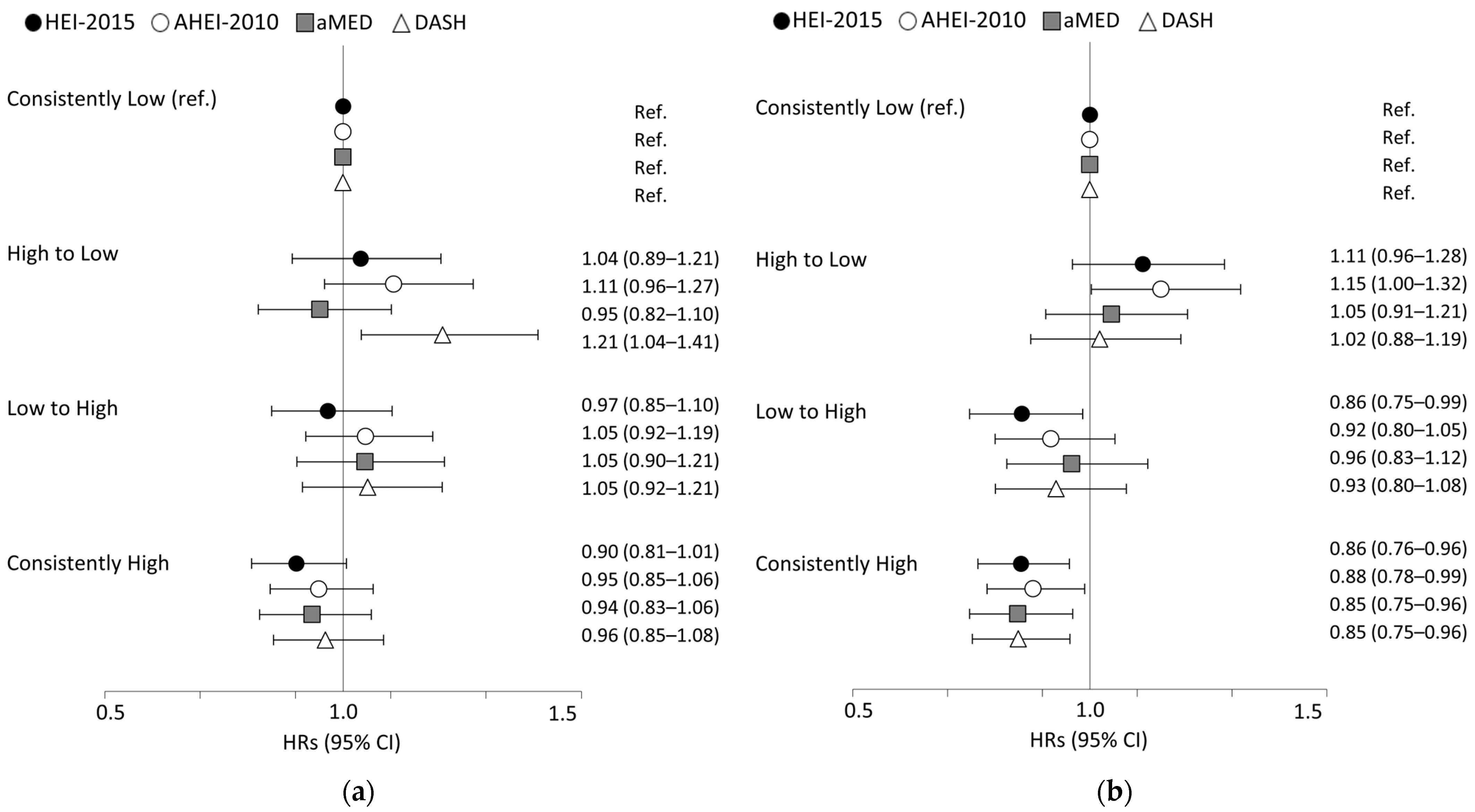
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N. Heart disease and stroke statistics—2021 update: A report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; U.S. Government Printing Office: Washington, DC, USA, 2015. [Google Scholar]
- Reedy, J.; Lerman, J.L.; Krebs-Smith, S.M.; Kirkpatrick, S.I.; Pannucci, T.E.; Wilson, M.M.; Subar, A.F.; Kahle, L.L.; Tooze, J.A. Evaluation of the Healthy Eating Index-2015. J. Acad. Nutr. Diet. 2018, 118, 1622–1633. [Google Scholar] [CrossRef] [PubMed]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; McCullough, M.L.; Newby, P.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Ballard-Barbash, R.; Manson, J.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: Evidence to inform national dietary guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef]
- Harmon, B.E.; Boushey, C.J.; Shvetsov, Y.B.; Ettienne, R.; Reedy, J.; Wilkens, L.R.; Le Marchand, L.; Henderson, B.E.; Kolonel, L.N. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: The Dietary Patterns Methods Project. Am. J. Clin. Nutr. 2015, 101, 587–597. [Google Scholar] [CrossRef]
- Panizza, C.E.; Shvetsov, Y.B.; Harmon, B.E.; Wilkens, L.R.; Le Marchand, L.; Haiman, C.; Reedy, J.; Boushey, C.J. Testing the Predictive Validity of the Healthy Eating Index-2015 in the Multiethnic Cohort: Is the Score Associated with a Reduced Risk of All-Cause and Cause-Specific Mortality? Nutrients 2018, 10, 452. [Google Scholar] [CrossRef]
- Reedy, J.; Krebs-Smith, S.M.; Miller, P.E.; Liese, A.D.; Kahle, L.L.; Park, Y.; Subar, A.F. Higher Diet Quality Is Associated with Decreased Risk of All-Cause, Cardiovascular Disease, and Cancer Mortality among Older Adults. J. Nutr. 2014, 144, 881–889. [Google Scholar] [CrossRef]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Bogensberger, B.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2018, 118, 74–100. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation 2015, 132, 2212–2219. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Association of changes in diet quality with total and cause-specific mortality. N. Engl. J. Med. 2017, 377, 143–153. [Google Scholar] [CrossRef]
- Kolonel, L.N.; Henderson, B.E.; Hankin, J.H.; Nomura, A.M.; Wilkens, L.R.; Pike, M.C.; Stram, D.O.; Monroe, K.R.; Earle, M.E.; Nagamine, F.S. A multiethnic cohort in Hawaii and Los Angeles: Baseline characteristics. Am. J. Epidemiol. 2000, 151, 346–357. [Google Scholar] [CrossRef]
- Stram, D.O.; Hankin, J.H.; Wilkens, L.R.; Pike, M.C.; Monroe, K.R.; Park, S.; Henderson, B.E.; Nomura, A.M.; Earle, M.E.; Nagamine, F.S. Calibration of the dietary questionnaire for a multiethnic cohort in Hawaii and Los Angeles. Am. J. Epidemiol. 2000, 151, 358–370. [Google Scholar] [CrossRef]
- Wilkens, L.R.; Kang, M.; Park, S.Y.; Sawyer, A.; Boushey, C.J.; Au, D.L.M.; Paik, H.Y.; Marchand, L.L.; Haiman, C.A.; Kolonel, L.N.; et al. Validation and comparison of nutrient intakes from two dietary questionnaires developed for the Multiethnic Cohort Study. J. Acad. Nutr. Diet. 2023, 123, 655–663. [Google Scholar] [CrossRef]
- Murphy, S.P. Unique nutrition support for research at the Cancer Research Center of Hawaii. Hawaii. Med. J. 2002, 61, 15–17. [Google Scholar]
- Sharma, S.; Murphy, S.P.; Wilkens, L.R.; Au, D.; Shen, L.; Kolonel, L.N. Extending a multiethnic food composition table to include standardized food group servings. J. Food Compos. Anal. 2003, 16, 485–495. [Google Scholar] [CrossRef]
- Liese, A.D.; Krebs-Smith, S.M.; Subar, A.F.; George, S.M.; Harmon, B.E.; Neuhouser, M.L.; Boushey, C.J.; Schap, T.E.; Reedy, J. The Dietary Patterns Methods Project: Synthesis of findings across cohorts and relevance to dietary guidance. J. Nutr. 2015, 145, 393–402. [Google Scholar] [CrossRef]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The healthy eating index: Design and applications. J. Acad. Nutr. Diet. 1995, 95, 1103–1108. [Google Scholar]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the healthy eating index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- McCullough, M.L.; Feskanich, D.; Stampfer, M.J.; Giovannucci, E.L.; Rimm, E.B.; Hu, F.B.; Spiegelman, D.; Hunter, D.J.; Colditz, G.A.; Willett, W.C. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. Am. J. Clin. Nutr. 2002, 76, 1261–1271. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Your Guide to Lowering Your Blood Pressure with DASH; U.S. Department of Health and Human Services: Bethesda, MD, USA, 2006. [Google Scholar]
- Park, S.Y.; Shvetsov, Y.B.; Kang, M.; Setiawan, V.W.; Wilkens, L.R.; Le Marchand, L.; Boushey, C.J. Changes in diet quality over 10 years are associated with baseline sociodemographic and lifestyle factors in the multiethnic cohort study. J. Nutr. 2020, 150, 1880–1888. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. International Classification of Diseases, 9th Revision. 2014. Available online: https://www.cdc.gov/nchs/icd/icd9.htm (accessed on 15 May 2022).
- National Center for Health Statistics. International Statistical Classification of Diseases and Related Health Problems, 5th ed.; 10th Revision; World Health Organization: Geneva, Switzerland, 2016; Available online: http://apps.who.int/classifications/icd10/browse/Content/statichtml/ICD10Volume2_en_2016.pdf (accessed on 15 May 2022).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; WHO Technical Report Series 894; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Haiman, C.A.; Stram, D.O.; Wilkens, L.R.; Pike, M.C.; Kolonel, L.N.; Henderson, B.E.; Le Marchand, L. Ethnic and racial differences in the smoking-related risk of lung cancer. N. Engl. J. Med. 2006, 354, 333–342. [Google Scholar] [CrossRef]
- Grambsch, P.M.; Therneau, T.M. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994, 81, 515–526. [Google Scholar] [CrossRef]
- Aigner, A.; Becher, H.; Jacobs, S.; Wilkens, L.R.; Boushey, C.J.; Le Marchand, L.; Haiman, C.A.; Maskarinec, G. Low diet quality and the risk of stroke mortality: The multiethnic cohort study. Eur. J. Clin. Nutr. 2018, 72, 1035–1045. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Rimm, E.B.; Appel, L.J.; Chiuve, S.E.; Djousse, L.; Engler, M.B.; Kris-Etherton, P.M.; Mozaffarian, D.; Siscovick, D.S.; Lichtenstein, A.H.; on behalf of the American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; et al. Seafood Long-Chain n-3 Polyunsaturated Fatty Acids and Cardiovascular Disease: A Science Advisory from the American Heart Association. Circulation 2018, 138, e35–e47. [Google Scholar] [CrossRef]
- Micha, R.; Penalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association Between Dietary Factors and Mortality from Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef]
- Yang, Q.; Zhang, Z.; Gregg, E.W.; Flanders, W.D.; Merritt, R.; Hu, F.B. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern. Med. 2014, 174, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Mente, A.; Teo, K.K.; Gao, P.; Sleight, P.; Dagenais, G.; Avezum, A.; Probstfield, J.L.; Dans, T.; Yusuf, S.; et al. Relationship between healthy diet and risk of cardiovascular disease among patients on drug therapies for secondary prevention: A prospective cohort study of 31,546 high-risk individuals from 40 countries. Circulation 2012, 126, 2705–2712. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Garcia, E.; Rodriguez-Artalejo, F.; Li, T.Y.; Fung, T.T.; Li, S.; Willett, W.C.; Rimm, E.B.; Hu, F.B. The Mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. Am. J. Clin. Nutr. 2014, 99, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R.A.; Wallentin, L.; Benatar, J.; Danchin, N.; Hagstrom, E.; Held, C.; Husted, S.; Lonn, E.; Stebbins, A.; Chiswell, K.; et al. Dietary patterns and the risk of major adverse cardiovascular events in a global study of high-risk patients with stable coronary heart disease. Eur. Heart J. 2016, 37, 1993–2001. [Google Scholar] [CrossRef]
- Freedman, L.S.; Schatzkin, A.; Midthune, D.; Kipnis, V. Dealing with dietary measurement error in nutritional cohort studies. J. Natl. Cancer Inst. 2011, 103, 1086–1092. [Google Scholar] [CrossRef]
| All | Change in Healthy Eating Index (HEI)-2015 1 | |||||
|---|---|---|---|---|---|---|
| Greatest Decline | Moderate Decline | Stable | Moderate Increase | Greatest Increase | ||
| Men, n | 26,624 | 2262 | 2886 | 10,355 | 4815 | 6306 |
| HEI-2015 score at baseline | 65.8 ± 10.3 | 73.9 ± 8.9 | 70.5 ± 9.2 | 67.2 ± 9.7 | 64.1 ± 9.5 | 59.7 ± 9.1 |
| HEI-2015 score at 10-year follow-up | 68.9 ± 10.6 | 59.2 ± 9.2 | 63.5 ± 9.2 | 67.5 ± 9.8 | 71.3 ± 9.4 | 75.6 ± 8.9 |
| Age at baseline (years) | 57.4 ± 8.3 | 59.4 ± 8.6 | 58.2 ± 8.5 | 57.8 ± 8.4 | 57.0 ± 8.2 | 55.9 ± 7.7 |
| Age at 10-year follow-up (years) | 68.4 ± 8.3 | 70.4 ± 8.6 | 69.1 ± 8.5 | 68.8 ± 8.4 | 67.9 ± 8.2 | 66.9 ± 7.7 |
| Race and ethnicity (%) | ||||||
| African American | 7.9 | 12.3 | 9.9 | 8.0 | 7.1 | 6.0 |
| Japanese American | 36.2 | 24.8 | 28.0 | 34.6 | 39.2 | 44.2 |
| Latino | 18.5 | 19.1 | 20.3 | 19.0 | 17.9 | 17.1 |
| Native Hawaiian | 7.1 | 6.5 | 7.6 | 6.7 | 7.2 | 7.9 |
| White | 30.3 | 37.2 | 34.1 | 31.8 | 28.6 | 24.8 |
| Education (%) | ||||||
| ≤High school | 28.3 | 31.7 | 27.9 | 28.2 | 26.9 | 28.4 |
| Vocational school | 30.7 | 30.3 | 30.8 | 30.4 | 30.4 | 31.5 |
| ≥Graduated college | 41.0 | 38.0 | 41.3 | 41.4 | 42.8 | 40.1 |
| Body mass index at baseline (kg/m2) | 26.4 ± 3.8 | 26.5 ± 3.9 | 26.4 ± 3.8 | 26.3 ± 3.7 | 26.3 ± 3.8 | 26.5 ± 3.8 |
| Body mass index at 10-year follow-up (kg/m2) | 26.7 ± 4.2 | 26.7 ± 4.5 | 26.7 ± 4.3 | 26.7 ± 4.2 | 26.6 ± 4.1 | 26.6 ± 4.2 |
| Smoking status at baseline (%) | ||||||
| Never | 36.9 | 34.2 | 37.4 | 37.1 | 39.0 | 35.6 |
| Former | 50.0 | 52.8 | 49.1 | 50.4 | 47.9 | 50.3 |
| Current | 13.1 | 13.1 | 13.5 | 12.5 | 13.1 | 14.0 |
| Smoking status at 10-year follow-up (%) | ||||||
| Never | 37.0 | 34.3 | 37.5 | 37.2 | 39.2 | 35.8 |
| Former | 55.8 | 57.3 | 54.2 | 55.4 | 54.0 | 58.1 |
| Current | 7.2 | 8.4 | 8.3 | 7.4 | 6.8 | 6.2 |
| Physical activity at baseline (h/d) | 1.5 ± 1.5 | 1.4 ± 1.5 | 1.5 ± 1.5 | 1.5 ± 1.5 | 1.5 ± 1.5 | 1.4 ± 1.5 |
| Physical activity at 10-year follow-up (h/d) | 1.7 ± 1.6 | 1.4 ± 1.6 | 1.6 ± 1.6 | 1.7 ± 1.6 | 1.7 ± 1.6 | 1.7 ± 1.6 |
| Alcohol intake at baseline (g/day) | 14.9 ± 28.3 | 16.0 ± 32.0 | 16.1 ± 28.3 | 15.2 ± 27.7 | 14.1 ± 26.6 | 14.1 ± 29.1 |
| Alcohol intake at 10-year follow-up (g/day) | 11.6 ± 20.5 | 9.5 ± 20.4 | 11.2 ± 20.8 | 11.7 ± 20.2 | 12.0 ± 20.4 | 11.8 ± 20.9 |
| History of hypertension at either survey | 52.5 | 55.0 | 52.6 | 52.1 | 52.9 | 52.0 |
| Women, n | 34,737 | 3152 | 3776 | 13,588 | 6335 | 7886 |
| HEI-2015 score at baseline | 69.6 ± 10.3 | 76.5 ± 8.7 | 74.3 ± 9.2 | 71.4 ± 9.7 | 68.1 ± 9.4 | 63.0 ± 9.0 |
| HEI-2015 score at 10-year follow-up | 72.6 ± 10.6 | 61.5 ± 9.1 | 67.1 ± 9.2 | 71.6 ± 9.7 | 75.4 ± 9.4 | 78.9 ± 8.6 |
| Age at baseline (years) | 57.3 ± 8.3 | 59.2 ± 8.5 | 58.6 ± 8.5 | 57.7 ± 8.3 | 56.9 ± 8.1 | 55.4 ± 7.8 |
| Age at 10-year follow-up (years) | 68.3 ± 8.3 | 70.2 ± 8.6 | 69.6 ± 8.5 | 68.7 ± 8.3 | 67.8 ± 8.1 | 66.5 ± 7.8 |
| Race and ethnicity (%) | ||||||
| African American | 11.6 | 15.2 | 14.0 | 12.1 | 9.9 | 9.3 |
| Japanese American | 34.7 | 24.7 | 28.2 | 33.3 | 38.5 | 41.0 |
| Latino | 15.6 | 17.1 | 15.9 | 14.3 | 14.8 | 17.6 |
| Native Hawaiian | 7.7 | 7.5 | 7.8 | 7.5 | 8.2 | 7.7 |
| White | 30.5 | 35.5 | 34.0 | 32.7 | 28.6 | 24.3 |
| Education (%) | ||||||
| ≤High school | 33.1 | 35.5 | 35.1 | 32.7 | 31.7 | 33.0 |
| Vocational school | 32.2 | 32.5 | 32.5 | 32.2 | 32.4 | 31.8 |
| ≥Graduated college | 34.7 | 32.0 | 32.4 | 35.1 | 35.9 | 35.2 |
| Body mass index at baseline (kg/m2) | 25.5 ± 5 | 26.0 ± 5.0 | 25.8 ± 5.1 | 25.5 ± 5.0 | 25.3 ± 4.9 | 25.5 ± 5.1 |
| Body mass index at 10-year follow-up (kg/m2) | 26 ± 5.4 | 26.6 ± 5.7 | 26.3 ± 5.6 | 25.9 ± 5.4 | 25.8 ± 5.3 | 25.9 ± 5.3 |
| Smoking status at baseline (%) | ||||||
| Never | 61.4 | 56.3 | 60.3 | 60.6 | 62.7 | 64.5 |
| Former | 27.8 | 31.6 | 29.3 | 28.3 | 27.3 | 24.9 |
| Current | 10.8 | 12.1 | 10.4 | 11.1 | 9.9 | 10.6 |
| Smoking status at 10-year follow-up (%) | ||||||
| Never | 61.6 | 56.5 | 60.4 | 60.7 | 62.9 | 64.7 |
| Former | 32.8 | 36.0 | 33.5 | 33.2 | 32.2 | 30.8 |
| Current | 5.7 | 7.5 | 6.1 | 6.0 | 5.0 | 4.5 |
| Physical activity at baseline (h/d) | 1.2 ± 1.3 | 1.3 ± 1.3 | 1.3 ± 1.3 | 1.3 ± 1.3 | 1.2 ± 1.3 | 1.1 ± 1.2 |
| Physical activity at 10-year follow-up (h/d) | 1.4 ± 1.5 | 1.3 ± 1.4 | 1.4 ± 1.4 | 1.4 ± 1.5 | 1.5 ± 1.4 | 1.4 ± 1.5 |
| Alcohol intake at baseline (g/day) | 4.8 ± 14 | 5.5 ± 15.1 | 5.2 ± 14.1 | 5.3 ± 14.9 | 4.5 ± 14.1 | 3.5 ± 11.7 |
| Alcohol intake at 10-year follow-up (g/day) | 4.1 ± 10.5 | 4.0 ± 11.6 | 4.1 ± 10.3 | 4.5 ± 11.1 | 3.9 ± 9.8 | 3.3 ± 9.8 |
| History of hypertension at either survey | 51.6 | 55.6 | 52.8 | 51.8 | 50.8 | 49.8 |
| Diet Quality Change 1 | Men (n = 26,624) | Women (n = 34,737) | P for Heterogeneity 3 | ||
|---|---|---|---|---|---|
| CVD Death | HR (95% CI) 2 | CVD Death | HR (95% CI) 2 | ||
| HEI-2015 | |||||
| Greatest decline | 240 | 1.13 (0.97–1.31) | 303 | 1.42 (1.24–1.62) | |
| Moderate decline | 250 | 1.01 (0.88–1.17) | 275 | 1.15 (1.00–1.32) | |
| Stable | 858 | 1.00 (ref.) | 812 | 1.00 (ref.) | |
| Moderate increase | 360 | 0.99 (0.87–1.12) | 320 | 0.95 (0.83–1.08) | |
| Greatest increase | 425 | 1.01 (0.89–1.14) | 331 | 0.89 (0.78–1.02) | |
| Per 1 SD increase | 2133 | 0.96 (0.92–1.01) | 2041 | 0.88 (0.84–0.92) | 0.0066 |
| AHEI-2010 | |||||
| Greatest decline | 246 | 1.12 (0.96–1.30) | 310 | 1.33 (1.16–1.52) | |
| Moderate decline | 288 | 1.07 (0.93–1.23) | 261 | 1.00 (0.87–1.15) | |
| Stable | 842 | 1.00 (ref.) | 814 | 1.00 (ref.) | |
| Moderate increase | 339 | 0.98 (0.87–1.12) | 294 | 0.89 (0.78–1.02) | |
| Greatest increase | 418 | 1.01 (0.89–1.15) | 362 | 0.97 (0.85–1.10) | |
| Per 1 SD increase | 2133 | 0.96 (0.91–1.01) | 2041 | 0.90 (0.85–0.95) | 0.1617 |
| aMED | |||||
| Greatest decline | 437 | 1.12 (0.97–1.29) | 481 | 1.29 (1.12–1.48) | |
| Moderate decline | 401 | 1.07 (0.93–1.22) | 365 | 0.97 (0.84–1.11) | |
| Stable | 441 | 1.00 (ref.) | 450 | 1.00 (ref.) | |
| Moderate increase | 402 | 1.07 (0.93–1.23) | 357 | 0.95 (0.82–1.10) | |
| Greatest increase | 452 | 1.09 (0.94–1.25) | 388 | 0.94 (0.81–1.08) | |
| Per 1 SD increase | 2133 | 0.99 (0.94–1.04) | 2041 | 0.89 (0.84–0.95) | 0.1224 |
| DASH | |||||
| Greatest decline | 218 | 1.38 (1.18–1.62) | 227 | 1.30 (1.11–1.51) | |
| Moderate decline | 240 | 1.18 (1.02–1.37) | 252 | 1.17 (1.01–1.34) | |
| Stable | 964 | 1.00 (ref.) | 963 | 1.00 (ref.) | |
| Moderate increase | 339 | 1.09 (0.96–1.24) | 316 | 1.07 (0.94–1.21) | |
| Greatest increase | 372 | 1.07 (0.94–1.21) | 283 | 0.92 (0.80–1.05) | |
| Per 1 SD increase | 2133 | 0.94 (0.89–0.99) | 2041 | 0.92 (0.87–0.96) | 0.6647 |
| HEI-2015 | AHEI-2010 | aMED | DASH | ||
|---|---|---|---|---|---|
| Subgroups | CVD Death | HR (95% CI) 1 | HR (95% CI) 1 | HR (95% CI) 1 | HR (95% CI) 1 |
| Men | |||||
| Race and ethnicity | |||||
| African American | 274 | 0.94 (0.82–1.08) | 0.99 (0.86–1.15) | 1.02 (0.88–1.18) | 0.90 (0.77–1.04) |
| Japanese American | 688 | 0.97 (0.89–1.06) | 0.99 (0.90–1.08) | 1.02 (0.92–1.12) | 0.99 (0.90–1.08) |
| Latino | 419 | 0.90 (0.80–1.00) | 0.97 (0.86–1.08) | 0.94 (0.83–1.07) | 0.88 (0.79–0.99) |
| Native Hawaiian | 126 | 0.98 (0.80–1.19) | 0.90 (0.73–1.11) | 0.82 (0.65–1.03) | 0.89 (0.73–1.09) |
| White | 626 | 1.00 (0.91–1.09) | 0.92 (0.84–1.01) | 1.01 (0.92–1.12) | 0.94 (0.86–1.04) |
| P for heterogeneity 2 | 0.3856 | 0.5888 | 0.1247 | 0.4624 | |
| Age at 10-year follow-up | |||||
| <65 years | 234 | 1.00 (0.86–1.16) | 0.95 (0.81–1.10) | 1.00 (0.84–1.18) | 0.89 (0.76–1.04) |
| 65–74 years | 616 | 0.91 (0.83–0.99) | 0.95 (0.86–1.04) | 0.95 (0.86–1.05) | 0.89 (0.81–0.98) |
| ≥75 years | 1283 | 0.99 (0.92–1.05) | 0.97 (0.91–1.04) | 1.00 (0.94–1.08) | 0.97 (0.91–1.04) |
| P for heterogeneity 2 | 0.4139 | 0.2707 | 0.2501 | 0.0391 | |
| Body mass index at 10-year follow-up | |||||
| <25 kg/m2 | 885 | 0.96 (0.89–1.04) | 0.97 (0.89–1.05) | 1.02 (0.94–1.12) | 0.93 (0.86–1.01) |
| 25–30 kg/m2 | 868 | 0.97 (0.89–1.05) | 0.98 (0.90–1.06) | 0.97 (0.89–1.05) | 0.95 (0.88–1.03) |
| ≥30 kg/m2 | 380 | 0.99 (0.88–1.11) | 0.92 (0.81–1.04) | 1.00 (0.87–1.14) | 0.96 (0.85–1.08) |
| P for heterogeneity 2 | 0.7485 | 0.2386 | 0.2440 | 0.7195 | |
| Smoking status at 10-year follow-up | |||||
| Never | 709 | 0.95 (0.87–1.04) | 0.96 (0.88–1.05) | 1.01 (0.92–1.11) | 0.93 (0.85–1.02) |
| Ever | 1424 | 0.97 (0.91–1.03) | 0.96 (0.90–1.02) | 0.98 (0.92–1.05) | 0.94 (0.88–1.00) |
| P for heterogeneity 2 | 0.9804 | 0.6452 | 0.1742 | 0.9198 | |
| Hypertension | |||||
| Without hypertension | 719 | 0.97 (0.89–1.06) | 1.06 (0.97–1.15) | 1.05 (0.96–1.16) | 0.97 (0.89–1.06) |
| With hypertension | 1414 | 0.96 (0.90–1.02) | 0.92 (0.86–0.97) | 0.96 (0.90–1.03) | 0.92 (0.87–0.98) |
| P for heterogeneity 2 | 0.7577 | 0.0059 | 0.2536 | 0.1871 | |
| Women | |||||
| Race and ethnicity | |||||
| African American | 360 | 0.82 (0.73–0.92) | 0.76 (0.67–0.86) | 0.79 (0.69–0.91) | 0.89 (0.78–1.00) |
| Japanese American | 642 | 0.90 (0.82–0.98) | 0.92 (0.83–1.02) | 0.89 (0.80–0.99) | 0.99 (0.90–1.08) |
| Latino | 313 | 0.93 (0.83–1.06) | 1.01 (0.88–1.15) | 1.00 (0.86–1.15) | 0.97 (0.84–1.10) |
| Native Hawaiian | 121 | 0.77 (0.62–0.94) | 0.91 (0.73–1.13) | 0.90 (0.70–1.16) | 0.93 (0.76–1.14) |
| White | 605 | 0.92 (0.84–1.01) | 0.91 (0.83–1.00) | 0.91 (0.82–1.01) | 0.84 (0.76–0.93) |
| P for heterogeneity 2 | 0.3776 | 0.1909 | 0.7574 | 0.1906 | |
| Age at 10-year follow-up | |||||
| <65 years | 176 | 0.82 (0.69–0.96) | 0.85 (0.71–1.01) | 0.77 (0.63–0.93) | 0.75 (0.63–0.90) |
| 65–74 years | 483 | 0.95 (0.85–1.05) | 0.91 (0.82–1.01) | 0.92 (0.82–1.03) | 0.99 (0.89–1.11) |
| ≥75 years | 1382 | 0.87 (0.82–0.92) | 0.91 (0.85–0.97) | 0.90 (0.84–0.97) | 0.92 (0.86–0.98) |
| P for heterogeneity 2 | 0.1161 | 0.4538 | 0.2496 | 0.0742 | |
| Body mass index at 10-year follow-up | |||||
| <25 kg/m2 | 1108 | 0.88 (0.82–0.94) | 0.92 (0.85–0.99) | 0.89 (0.83–0.97) | 0.90 (0.84–0.97) |
| 25–30 kg/m2 | 555 | 0.85 (0.77–0.94) | 0.86 (0.77–0.95) | 0.85 (0.76–0.95) | 0.92 (0.83–1.02) |
| ≥30 kg/m2 | 378 | 0.94 (0.84–1.05) | 0.93 (0.82–1.05) | 0.98 (0.86–1.12) | 0.97 (0.85–1.09) |
| P for heterogeneity 2 | 0.3601 | 0.1366 | 0.2537 | 0.7224 | |
| Smoking status at 10-year follow-up | |||||
| Never | 1255 | 0.90 (0.84–0.95) | 0.92 (0.86–0.99) | 0.92 (0.85–0.99) | 0.93 (0.87–0.99) |
| Ever | 786 | 0.86 (0.79–0.93) | 0.87 (0.80–0.94) | 0.85 (0.78–0.94) | 0.89 (0.82–0.97) |
| P for heterogeneity 2 | 0.6351 | 0.4875 | 0.3065 | 0.8453 | |
| Hypertension | |||||
| Without hypertension | 608 | 0.92 (0.84–1.02) | 0.94 (0.85–1.03) | 0.89 (0.80–0.99) | 0.94 (0.85–1.04) |
| With hypertension | 1433 | 0.86 (0.81–0.91) | 0.88 (0.83–0.94) | 0.90 (0.84–0.96) | 0.91 (0.85–0.97) |
| P for heterogeneity 2 | 0.2886 | 0.4189 | 0.9976 | 0.8884 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, M.; Boushey, C.J.; Shvetsov, Y.B.; Setiawan, V.W.; Paik, H.-Y.; Wilkens, L.R.; Le Marchand, L.; Park, S.-Y. Changes in Diet Quality over 10 Years and Subsequent Mortality from Cardiovascular Disease in the Multiethnic Cohort Study. Nutrients 2023, 15, 3482. https://doi.org/10.3390/nu15153482
Kang M, Boushey CJ, Shvetsov YB, Setiawan VW, Paik H-Y, Wilkens LR, Le Marchand L, Park S-Y. Changes in Diet Quality over 10 Years and Subsequent Mortality from Cardiovascular Disease in the Multiethnic Cohort Study. Nutrients. 2023; 15(15):3482. https://doi.org/10.3390/nu15153482
Chicago/Turabian StyleKang, Minji, Carol J. Boushey, Yurii B. Shvetsov, Veronica W. Setiawan, Hee-Young Paik, Lynne R. Wilkens, Loïc Le Marchand, and Song-Yi Park. 2023. "Changes in Diet Quality over 10 Years and Subsequent Mortality from Cardiovascular Disease in the Multiethnic Cohort Study" Nutrients 15, no. 15: 3482. https://doi.org/10.3390/nu15153482
APA StyleKang, M., Boushey, C. J., Shvetsov, Y. B., Setiawan, V. W., Paik, H.-Y., Wilkens, L. R., Le Marchand, L., & Park, S.-Y. (2023). Changes in Diet Quality over 10 Years and Subsequent Mortality from Cardiovascular Disease in the Multiethnic Cohort Study. Nutrients, 15(15), 3482. https://doi.org/10.3390/nu15153482






