Targeted Application of Functional Foods as Immune Fitness Boosters in the Defense against Viral Infection
Abstract
:1. Introduction
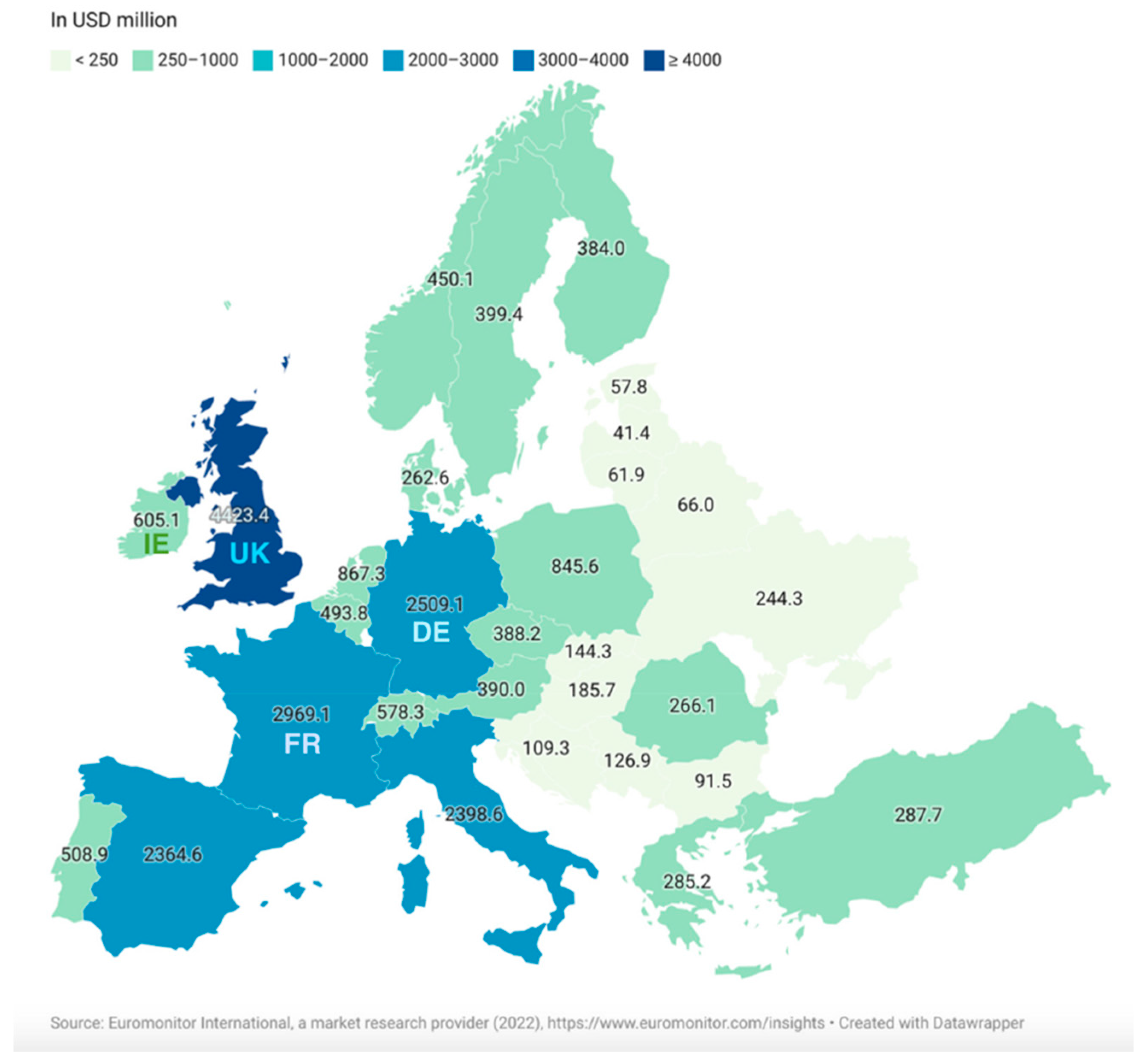
2. Trends in Health and Wellbeing: A Focus on Functional Foods
3. Boosting Immune Fitness in High-Risk Individuals
3.1. Immune Fitness
3.1.1. Immune Response in the Elderly
3.1.2. Immune Response in Obese Individuals
3.1.3. Immune Response in People with Underlying Chronic Conditions
4. Functional Foods as Immune Fitness Boosters in the Context of Viral Infection
4.1. Whole Milk Proteins and Hydrolysates
4.1.1. Whey
4.1.2. Casein
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| Whey/Lactoferrin | Antiviral |
| [132,134,135] |
| Immunomodulator |
| [136,137,146,147] | |
| Anti-inflammatory |
| [44] | |
| Casein | Antiviral |
| [142,144,145] |
4.2. Fermented Dairy Products
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| Kefir | Antiviral |
| [148,149,153] |
| Immunomodulator |
| [148,150,151] | |
| Anti-inflammatory |
| [148] | |
| Yogurt | Antiviral |
| [166] |
| Immunomodulator |
| [153,154,155] | |
| Anti-inflammatory |
| [157,158] | |
| Koumiss | Antiviral |
| [161,162] |
| Immunomodulator |
| [161,167] | |
| Anti-inflammatory |
| [161] |
4.3. Plant-Derived Functional Foods
4.4. Polyunsaturated Fatty Acids (PUFA)-Rich Foods
4.5. Vitamin-D-Enriched Foods
4.6. Zinc-Enriched Foods
4.7. Selenium-Enriched Foods
5. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fadnes, L.T.; Økland, J.-M.; Haaland, Ø.A.; Johansson, K.A. Estimating Impact of Food Choices on Life Expectancy: A Modeling Study. PLoS Med. 2022, 19, e1003889. [Google Scholar] [CrossRef]
- Koithan, M.; Devika, J. New Approaches to Nutritional Therapy. J. Nurse Pract. 2010, 6, 805–806. [Google Scholar] [CrossRef] [Green Version]
- Wu, D.; Lewis, E.D.; Pae, M.; Meydani, S.N. Nutritional Modulation of Immune Function: Analysis of Evidence, Mechanisms, and Clinical Relevance. Front. Immunol. 2018, 9, 3160. [Google Scholar] [CrossRef] [Green Version]
- Atherton, J.G.; Kratzing, C.C.; Fisher, A. The Effect of Ascorbic Acid on Infection of Chick-Embryo Ciliated Tracheal Organ Cultures by Coronavirus. Arch. Virol. 1978, 56, 195–199. [Google Scholar] [CrossRef] [Green Version]
- Chihara, G.O.R.O. Medical Aspects of Lentinan Isolated from Lentinus Edodes (Berk.) Sing. In Mushroom Biology and Mushroom Products; Chinese University Press: Hong Kong, 1993; pp. 261–266. [Google Scholar]
- Tochikura, T.S.; Nakashima, H.; Hirose, K.; Yamamoto, N. A Biological Response Modifier, PSK, Inhibits Human Immunodeficiency Virus Infection in Vitro. Biochem. Biophys. Res. Commun. 1987, 148, 726–733. [Google Scholar] [CrossRef]
- Takehara, M.; Kuida, K.; Mori, K. Antiviral Activity of Virus-like Particles FromLentinus Edodes (Shiitake). Arch. Virol. 1979, 59, 269–274. [Google Scholar] [CrossRef]
- Hayashi, T.; Hayashi, K.; Maeda, M.; Kojima, I. Calcium Spirulan, an Inhibitor of Enveloped Virus Replication, from a Blue-Green Alga Spirulina Platensis. J. Nat. Prod. 1996, 59, 83–87. [Google Scholar] [CrossRef]
- Khan, Z.; Bhadouria, P.; Bisen, P.S. Nutritional and Therapeutic Potential of Spirulina. Curr. Pharm. Biotechnol. 2005, 6, 373–379. [Google Scholar] [CrossRef] [Green Version]
- Schandalik, R.; Gatti, G.; Perucca, E. Pharmacokinetics of Silybin in Bile Following Administration of Silipide and Silymarin in Cholecystectomy Patients. Arzneimittelforschung 1992, 42, 964–968. [Google Scholar]
- Rahman, M.M.; Mosaddik, A.; Alam, A.K. Traditional Foods with Their Constituent’s Antiviral and Immune System Modulating Properties. Heliyon 2021, 7, e05957. [Google Scholar] [CrossRef]
- Wellness Creative Co Health & Wellness Industry Statistics 2022 [Latest Market Data & Trends]. Wellness Creative Co 2019. Available online: https://www.wellnesscreatives.com/wellness-industry-statistics/ (accessed on 1 July 2022).
- Euromonitor International, a Market Research Provider Market Sizes. 2022. Available online: https://www-portal-euromonitor-com.dcu.idm.oclc.org/portal/statisticsevolution/index (accessed on 1 July 2022).
- Sørensen, H.M.; Rochfort, K.D.; Maye, S.; MacLeod, G.; Brabazon, D.; Loscher, C.; Freeland, B. Exopolysaccharides of Lactic Acid Bacteria: Production, Purification and Health Benefits towards Functional Food. Nutrients 2022, 14, 2938. [Google Scholar] [CrossRef] [PubMed]
- Research and Markets. Immune Health Supplements Market—Global Outlook and Forecast 2020–2025; Research and Markets: Dublin, Ireland, 2021. [Google Scholar]
- Health Service Executive. How Long Does Immunity Last after COVID-19 Vaccination? Does Immunity Wane Faster in Certain Sub-Populations? How Safe and Effective Are Booster Doses of COVID-19 Vaccine? HLI (Health Library Ireland): Dublin, Ireland, 2021. [Google Scholar]
- Thomas, S.J.; Moreira, E.D.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Polack, F.P.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine through 6 Months. N. Engl. J. Med. 2021, 385, 1761–1773. [Google Scholar] [CrossRef]
- van de Loo, A.J.A.E.; Kerssemakers, N.; Scholey, A.; Garssen, J.; Kraneveld, A.D.; Verster, J.C. Perceived Immune Fitness, Individual Strength and Hangover Severity. Int. J. Environ. Res. Public Health 2020, 17, 4039. [Google Scholar] [CrossRef]
- Danone Nutricia Research. Immune Fitness: Working towards a Resilient Immune System; Danone Nutricia Research: Utrecht, The Netherlands, 2022. [Google Scholar]
- Villar-Álvarez, F.; de la Rosa-Carrillo, D.; Fariñas-Guerrero, F.; Jiménez-Ruiz, C.A. Immunosenescence, Immune Fitness and Vaccination Schedule in the Adult Respiratory Patient. Open Respir. Arch. 2022, 4, 100181. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Garagnani, P.; Parini, P.; Giuliani, C.; Santoro, A. Inflammaging: A New Immune–Metabolic Viewpoint for Age-Related Diseases. Nat. Rev. Endocrinol. 2018, 14, 576–590. [Google Scholar] [CrossRef]
- Christ, A.; Lauterbach, M.; Latz, E. Western Diet and the Immune System: An Inflammatory Connection. Immunity 2019, 51, 794–811. [Google Scholar] [CrossRef]
- Pérez-Cano, F.J. Mediterranean Diet, Microbiota and Immunity. Nutrients 2022, 14, 273. [Google Scholar] [CrossRef]
- Cordain, L.; Eaton, S.B.; Sebastian, A.; Mann, N.; Lindeberg, S.; Watkins, B.A.; O’Keefe, J.H.; Brand-Miller, J. Origins and Evolution of the Western Diet: Health Implications for the 21st Century. Am. J. Clin. Nutr. 2005, 81, 341–354. [Google Scholar] [CrossRef] [Green Version]
- Bach, J.-F. The Effect of Infections on Susceptibility to Autoimmune and Allergic Diseases. N. Engl. J. Med. 2002, 347, 911–920. [Google Scholar] [CrossRef]
- Eder, W.; Ege, M.J.; von Mutius, E. The Asthma Epidemic. N. Engl. J. Med. 2006, 355, 2226–2235. [Google Scholar] [CrossRef] [Green Version]
- Lewis, J.D. The Role of Diet in Inflammatory Bowel Disease. Gastroenterol. Hepatol. 2016, 12, 51–53. [Google Scholar]
- Wypych, T.P.; Marsland, B.J.; Ubags, N.D.J. The Impact of Diet on Immunity and Respiratory Diseases. Ann. ATS 2017, 14, S339–S347. [Google Scholar] [CrossRef]
- NIH Definition of Immunocompromised—NCI Dictionary of Cancer Terms—NCI. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/immunocompromised (accessed on 22 July 2022).
- CDC CDC—Cryptosporidiosis—Fact Sheets—Infection—Immunocompromised Persons. Available online: https://www.cdc.gov/parasites/crypto/gen_info/infect_ic.html (accessed on 22 July 2022).
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is Suspected: Interim Guidance, 13 March 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Suardi, C.; Cazzaniga, E.; Graci, S.; Dongo, D.; Palestini, P. Link between Viral Infections, Immune System, Inflammation and Diet. Int. J. Environ. Res. Public Health 2021, 18, 2455. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, S.; Aziz, R.; Al Mahri, S.; Malik, S.S.; Haji, E.; Khan, A.H.; Khatlani, T.S.; Bouchama, A. Obesity and COVID-19: What Makes Obese Host so Vulnerable? Immun. Ageing 2021, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- Ashan, Maria., What is immune fitness, July 2022, News Medical Life Sciences. Available online: https://www.news-medical.net/health/What-is-Immune-Fitness.aspx (accessed on 26 July 2023).
- Ioannidis, J.P.A.; Axfors, C.; Contopoulos-Ioannidis, D.G. Population-Level COVID-19 Mortality Risk for Non-Elderly Individuals Overall and for Non-Elderly Individuals without Underlying Diseases in Pandemic Epicenters. Environ. Res. 2020, 188, 109890. [Google Scholar] [CrossRef]
- Oh, S.-J.; Lee, J.K.; Shin, O.S. Aging and the Immune System: The Impact of Immunosenescence on Viral Infection, Immunity and Vaccine Immunogenicity. Immune Netw. 2019, 19, e37. [Google Scholar] [CrossRef]
- Pae, M.; Meydani, S.N.; Wu, D. The Role of Nutrition in Enhancing Immunity in Aging. Aging Dis. 2011, 3, 91–129. [Google Scholar]
- Palmer, D.B. The Effect of Age on Thymic Function. Front. Immunol. 2013, 4, 316. [Google Scholar] [CrossRef] [Green Version]
- Müller, L.; Pawelec, G. Aging and Immunity—Impact of Behavioral Intervention. Brain Behav. Immun. 2014, 39, 8–22. [Google Scholar] [CrossRef]
- Mabbott, N.A.; Kobayashi, A.; Sehgal, A.; Bradford, B.M.; Pattison, M.; Donaldson, D.S. Aging and the Mucosal Immune System in the Intestine. Biogerontology 2015, 16, 133–145. [Google Scholar] [CrossRef]
- Faria, A.M.C.; Mucida, D.; McCafferty, D.-M.; Tsuji, N.M.; Verhasselt, V. Tolerance and Inflammation at the Gut Mucosa. Clin. Dev. Immunol. 2012, 2012, 738475. [Google Scholar] [CrossRef]
- Magrone, T.; Jirillo, E. The Interaction between Gut Microbiota and Age-Related Changes in Immune Function and Inflammation. Immun. Ageing 2013, 10, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shemtov, S.J.; Emani, R.; Bielska, O.; Covarrubias, A.J.; Verdin, E.; Andersen, J.K.; Winer, D.A. The Intestinal Immune System and Gut Barrier Function in Obesity and Ageing. FEBS J. 2022. [Google Scholar] [CrossRef] [PubMed]
- Zimecki, M.; Właszczyk, A.; Zagulski, T.; Kübler, A. Lactoferrin Lowers Serum Interleukin 6 and Tumor Necrosis Factor Alpha Levels in Mice Subjected to Surgery. Arch. Immunol. Ther. Exp. 1998, 46, 97–104. [Google Scholar]
- Wu, Y.; Xu, J.; Rong, X.; Wang, F.; Wang, H.; Zhao, C. Gut Microbiota Alterations and Health Status in Aging Adults: From Correlation to Causation. Aging Med. 2021, 4, 206–213. [Google Scholar] [CrossRef]
- Walker, E.M.; Slisarenko, N.; Gerrets, G.L.; Kissinger, P.J.; Didier, E.S.; Kuroda, M.J.; Veazey, R.S.; Jazwinski, S.M.; Rout, N. Inflammaging Phenotype in Rhesus Macaques Is Associated with a Decline in Epithelial Barrier-Protective Functions and Increased pro-Inflammatory Function in CD161-Expressing Cells. Geroscience 2019, 41, 739–757. [Google Scholar] [CrossRef]
- Thevaranjan, N.; Puchta, A.; Schulz, C.; Naidoo, A.; Szamosi, J.C.; Verschoor, C.P.; Loukov, D.; Schenck, L.P.; Jury, J.; Foley, K.P.; et al. Age-Associated Microbial Dysbiosis Promotes Intestinal Permeability, Systemic Inflammation, and Macrophage Dysfunction. Cell Host Microbe 2017, 21, 455–466.e4. [Google Scholar] [CrossRef] [Green Version]
- Ragonnaud, E.; Biragyn, A. Gut Microbiota as the Key Controllers of “Healthy” Aging of Elderly People. Immun. Ageing 2021, 18, 2. [Google Scholar] [CrossRef]
- Jeffery, I.B.; Lynch, D.B.; O’Toole, P.W. Composition and Temporal Stability of the Gut Microbiota in Older Persons. ISME J. 2016, 10, 170–182. [Google Scholar] [CrossRef] [Green Version]
- Pae, M.; Wu, D. Nutritional Modulation of Age-Related Changes in the Immune System and Risk of Infection. Nutr. Res. 2017, 41, 14–35. [Google Scholar] [CrossRef] [Green Version]
- Frasca, D.; Blomberg, B.B. Aging Induces B Cell Defects and Decreased Antibody Responses to Influenza Infection and Vaccination. Immun. Ageing 2020, 17, 37. [Google Scholar] [CrossRef]
- Colonna-Romano, G.; Bulati, M.; Aquino, A.; Pellicanò, M.; Vitello, S.; Lio, D.; Candore, G.; Caruso, C. A Double-Negative (IgD−CD27−) B Cell Population Is Increased in the Peripheral Blood of Elderly People. Mech. Ageing Dev. 2009, 130, 681–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thangavelu, G.; Smolarchuk, C.; Anderson, C.C. Co-Inhibitory Molecules. Self Nonself 2010, 1, 77–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dillon, S.M.; Liu, J.; Purba, C.M.; Christians, A.J.; Kibbie, J.J.; Castleman, M.J.; McCarter, M.D.; Wilson, C.C. Age-Related Alterations in Human Gut CD4 T Cell Phenotype, T Helper Cell Frequencies, and Functional Responses to Enteric Bacteria. J. Leukoc. Biol. 2020, 107, 119–132. [Google Scholar] [CrossRef]
- Dillon, S.M.; Thompson, T.A.; Christians, A.J.; McCarter, M.D.; Wilson, C.C. Reduced Immune-Regulatory Molecule Expression on Human Colonic Memory CD4 T Cells in Older Adults. Immun. Ageing 2021, 18, 6. [Google Scholar] [CrossRef] [PubMed]
- Sugahara, H.; Okai, S.; Odamaki, T.; Wong, C.B.; Kato, K.; Mitsuyama, E.; Xiao, J.-Z.; Shinkura, R. Decreased Taxon-Specific IgA Response in Relation to the Changes of Gut Microbiota Composition in the Elderly. Front. Microbiol. 2017, 8, 1757. [Google Scholar] [CrossRef] [Green Version]
- Peterson, D.A.; McNulty, N.P.; Guruge, J.L.; Gordon, J.I. IgA Response to Symbiotic Bacteria as a Mediator of Gut Homeostasis. Cell Host Microbe 2007, 2, 328–339. [Google Scholar] [CrossRef] [Green Version]
- Nagafusa, H.; Sayama, K. Age-Related Chemokine Alterations Affect IgA Secretion and Gut Immunity in Female Mice. Biogerontology 2020, 21, 609–618. [Google Scholar] [CrossRef]
- Nakajima, A.; Vogelzang, A.; Maruya, M.; Miyajima, M.; Murata, M.; Son, A.; Kuwahara, T.; Tsuruyama, T.; Yamada, S.; Matsuura, M.; et al. IgA Regulates the Composition and Metabolic Function of Gut Microbiota by Promoting Symbiosis between Bacteria. J. Exp. Med. 2018, 215, 2019–2034. [Google Scholar] [CrossRef]
- Childs, C.E.; Calder, P.C.; Miles, E.A. Diet and Immune Function. Nutrients 2019, 11, 1933. [Google Scholar] [CrossRef] [Green Version]
- González-Muniesa, P.; Mártinez-González, M.-A.; Hu, F.B.; Després, J.-P.; Matsuzawa, Y.; Loos, R.J.F.; Moreno, L.A.; Bray, G.A.; Martinez, J.A. Obesity. Nat. Rev. Dis. Primers 2017, 3, 17034. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and Comorbidities: Deleterious Impact on Infected Patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Nam, J.-H. Insight into the Relationship between Obesity-Induced Low-Level Chronic Inflammation and COVID-19 Infection. Int. J. Obes. 2020, 44, 1541–1542. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Na, H.; Kim, J.-A.; Nam, J.-H. What We Know and What We Need to Know about Adenovirus 36-Induced Obesity. Int. J. Obes. 2020, 44, 1197–1209. [Google Scholar] [CrossRef]
- Hulme, K.D.; Noye, E.C.; Short, K.R.; Labzin, L.I. Dysregulated Inflammation During Obesity: Driving Disease Severity in Influenza Virus and SARS-CoV-2 Infections. Front. Immunol. 2021, 12, 4356. [Google Scholar] [CrossRef]
- Antunes, A.E.C.; Vinderola, G.; Xavier-Santos, D.; Sivieri, K. Potential Contribution of Beneficial Microbes to Face the COVID-19 Pandemic. Food Res. Int. 2020, 136, 109577. [Google Scholar] [CrossRef]
- Wadman, M. Why COVID-19 Is More Deadly in People with Obesity—Even If They’re Young. Available online: https://www.science.org/content/article/why-covid-19-more-deadly-people-obesity-even-if-theyre-young (accessed on 4 July 2022).
- Neidich, S.D.; Green, W.D.; Rebeles, J.; Karlsson, E.A.; Schultz-Cherry, S.; Noah, T.L.; Chakladar, S.; Hudgens, M.G.; Weir, S.S.; Beck, M.A. Increased Risk of Influenza among Vaccinated Adults Who Are Obese. Int. J. Obes. 2017, 41, 1324–1330. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, T.; Ackerman, S.E.; Shen, L.; Engleman, E. Role of Innate and Adaptive Immunity in Obesity-Associated Metabolic Disease. J. Clin. Investig. 2017, 127, 5–13. [Google Scholar] [CrossRef] [Green Version]
- Weisberg, S.P.; McCann, D.; Desai, M.; Rosenbaum, M.; Leibel, R.L.; Ferrante, A.W. Obesity Is Associated with Macrophage Accumulation in Adipose Tissue. J. Clin. Investig. 2003, 112, 1796–1808. [Google Scholar] [CrossRef]
- Winer, D.A.; Luck, H.; Tsai, S.; Winer, S. The Intestinal Immune System in Obesity and Insulin Resistance. Cell Metab. 2016, 23, 413–426. [Google Scholar] [CrossRef] [Green Version]
- Maynard, C.L.; Elson, C.O.; Hatton, R.D.; Weaver, C.T. Reciprocal Interactions of the Intestinal Microbiota and Immune System. Nature 2012, 489, 231–241. [Google Scholar] [CrossRef] [Green Version]
- Cani, P.D.; Amar, J.; Iglesias, M.A.; Poggi, M.; Knauf, C.; Bastelica, D.; Neyrinck, A.M.; Fava, F.; Tuohy, K.M.; Chabo, C.; et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes 2007, 56, 1761–1772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cani, P.D.; Bibiloni, R.; Knauf, C.; Waget, A.; Neyrinck, A.M.; Delzenne, N.M.; Burcelin, R. Changes in Gut Microbiota Control Metabolic Endotoxemia-Induced Inflammation in High-Fat Diet–Induced Obesity and Diabetes in Mice. Diabetes 2008, 57, 1470–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luck, H.; Tsai, S.; Chung, J.; Clemente-Casares, X.; Ghazarian, M.; Revelo, X.S.; Lei, H.; Luk, C.T.; Shi, S.Y.; Surendra, A.; et al. Regulation of Obesity-Related Insulin Resistance with Gut Anti-Inflammatory Agents. Cell Metab. 2015, 21, 527–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Sadi, R.; Ye, D.; Dokladny, K.; Ma, T.Y. Mechanism of IL-1β-Induced Increase in Intestinal Epithelial Tight Junction Permeability. J. Immunol. 2008, 180, 5653–5661. [Google Scholar] [CrossRef] [Green Version]
- Russo, L.; Lumeng, C.N. Properties and Functions of Adipose Tissue Macrophages in Obesity. Immunology 2018, 155, 407–417. [Google Scholar] [CrossRef] [Green Version]
- Bredella, M.A.; Gill, C.M.; Gerweck, A.V.; Landa, M.G.; Kumar, V.; Daley, S.M.; Torriani, M.; Miller, K.K. Ectopic and Serum Lipid Levels Are Positively Associated with Bone Marrow Fat in Obesity. Radiology 2013, 269, 534–541. [Google Scholar] [CrossRef]
- Dicker, D.; Salook, M.A.; Marcoviciu, D.; Djaldetti, M.; Bessler, H. Role of Peripheral Blood Mononuclear Cells in the Predisposition of Obese Individuals to Inflammation and Infection. Obes. Facts 2013, 6, 146–151. [Google Scholar] [CrossRef]
- Teran-Cabanillas, E.; Montalvo-Corral, M.; Caire-Juvera, G.; Moya-Camarena, S.Y.; Hernández, J. Decreased Interferon-α and Interferon-β Production in Obesity and Expression of Suppressor of Cytokine Signaling. Nutrition 2013, 29, 207–212. [Google Scholar] [CrossRef]
- Bruun, J.M.; Lihn, A.S.; Pedersen, S.B.; Richelsen, B. Monocyte Chemoattractant Protein-1 Release Is Higher in Visceral than Subcutaneous Human Adipose Tissue (AT): Implication of Macrophages Resident in the AT. J. Clin. Endocrinol. Metab. 2005, 90, 2282–2289. [Google Scholar] [CrossRef]
- Field, C.S.; Baixauli, F.; Kyle, R.L.; Puleston, D.J.; Cameron, A.M.; Sanin, D.E.; Hippen, K.L.; Loschi, M.; Thangavelu, G.; Corrado, M.; et al. Mitochondrial Integrity Regulated by Lipid Metabolism Is a Cell-Intrinsic Checkpoint for Treg Suppressive Function. Cell Metab. 2020, 31, 422–437.e5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, H.; Wang, L.; Liu, F. Immunological Impact of Intestinal T Cells on Metabolic Diseases. Front. Immunol. 2021, 12, 639902. [Google Scholar] [CrossRef]
- Khan, S.; Luck, H.; Winer, S.; Winer, D.A. Emerging Concepts in Intestinal Immune Control of Obesity-Related Metabolic Disease. Nat. Commun. 2021, 12, 2598. [Google Scholar] [CrossRef]
- Luck, H.; Khan, S.; Kim, J.H.; Copeland, J.K.; Revelo, X.S.; Tsai, S.; Chakraborty, M.; Cheng, K.; Tao Chan, Y.; Nøhr, M.K.; et al. Gut-Associated IgA+ Immune Cells Regulate Obesity-Related Insulin Resistance. Nat. Commun. 2019, 10, 3650. [Google Scholar] [CrossRef] [Green Version]
- CDC People with Certain Medical Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 27 July 2022).
- NIAID. The Effects of Highly Active Antiretroviral Therapy (HAART) on the Recovery of Immune Function in HIV-Infected Children and Young Adults. 2013. Available online: clinicaltrials.gov (accessed on 12 July 2023).
- HIV.Gov Global Statistics. Available online: https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics (accessed on 27 July 2022).
- WHO HIV/AIDS. Available online: https://www.who.int/data/gho/data/themes/hiv-aids (accessed on 27 July 2022).
- HIV Ireland Treatment; HIV Ireland: Dublin, Ireland, 2022.
- Liu, J.; Williams, B.; Frank, D.; Dillon, S.M.; Wilson, C.C.; Landay, A.L. Inside Out: HIV, the Gut Microbiome, and the Mucosal Immune System. J. Immunol. 2017, 198, 605–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neuhaus, J.; Jacobs, D.R., Jr.; Baker, J.V.; Calmy, A.; Duprez, D.; La Rosa, A.; Kuller, L.H.; Pett, S.L.; Ristola, M.; Ross, M.J.; et al. Markers of Inflammation, Coagulation, and Renal Function Are Elevated in Adults with HIV Infection. J. Infect. Dis. 2010, 201, 1788–1795. [Google Scholar] [CrossRef] [PubMed]
- Hunt, P.W.; Sinclair, E.; Rodriguez, B.; Shive, C.; Clagett, B.; Funderburg, N.; Robinson, J.; Huang, Y.; Epling, L.; Martin, J.N.; et al. Gut Epithelial Barrier Dysfunction and Innate Immune Activation Predict Mortality in Treated HIV Infection. J. Infect. Dis. 2014, 210, 1228–1238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandes, S.M.; Pires, A.R.; Ferreira, C.; Foxall, R.B.; Rino, J.; Santos, C.; Correia, L.; Poças, J.; Veiga-Fernandes, H.; Sousa, A.E. Enteric Mucosa Integrity in the Presence of a Preserved Innate Interleukin 22 Compartment in HIV Type 1–Treated Individuals. J. Infect. Dis. 2014, 210, 630–640. [Google Scholar] [CrossRef] [Green Version]
- Lapenta, C.; Boirivant, M.; Marini, M.; Santini, S.M.; Logozzi, M.; Viora, M.; Belardelli, F.; Fais, S. Human Intestinal Lamina Propria Lymphocytes Are Naturally Permissive to HIV-1 Infection. Eur. J. Immunol. 1999, 29, 1202–1208. [Google Scholar] [CrossRef]
- Hazenberg, M.D.; Hamann, D.; Schuitemaker, H.; Miedema, F. T Cell Depletion in HIV-1 Infection: How CD4+ T Cells Go out of Stock. Nat. Immunol. 2000, 1, 285–289. [Google Scholar] [CrossRef]
- Unutmaz, D.; Pileri, P.; Abrignani, S. Antigen-Independent Activation of Naive and Memory Resting T Cells by a Cytokine Combination. J. Exp. Med. 1994, 180, 1159–1164. [Google Scholar] [CrossRef] [PubMed]
- Swingler, S.; Mann, A.; Jacqué, J.-M.; Brichacek, B.; Sasseville, V.G.; Williams, K.; Lackner, A.A.; Janoff, E.N.; Wang, R.; Fisher, D.; et al. HIV-1 Nef Mediates Lymphocyte Chemotaxis and Activation by Infected Macrophages. Nat. Med. 1999, 5, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- de Mattos, B.R.R.; Garcia, M.P.G.; Nogueira, J.B.; Paiatto, L.N.; Albuquerque, C.G.; Souza, C.L.; Fernandes, L.G.R.; Tamashiro, W.M.d.S.C.; Simioni, P.U. Inflammatory Bowel Disease: An Overview of Immune Mechanisms and Biological Treatments. Mediat. Inflamm. 2015, 2015, 493012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC Prevalence of IBD|CDC. Available online: https://www.cdc.gov/ibd/data-and-statistics/prevalence.html (accessed on 19 July 2022).
- Alatab, S.; Sepanlou, S.G.; Ikuta, K.; Vahedi, H.; Bisignano, C.; Safiri, S.; Sadeghi, A.; Nixon, M.R.; Abdoli, A.; Abolhassani, H.; et al. The Global, Regional, and National Burden of Inflammatory Bowel Disease in 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30. [Google Scholar] [CrossRef] [Green Version]
- EFCCA About IBD (Inflammatory Bowel Diseases) Organisations|World IBD Day. Available online: https://worldibdday.org/about-us (accessed on 19 July 2022).
- Hisamatsu, T.; Kanai, T.; Mikami, Y.; Yoneno, K.; Matsuoka, K.; Hibi, T. Immune Aspects of the Pathogenesis of Inflammatory Bowel Disease. Pharmacol. Ther. 2013, 137, 283–297. [Google Scholar] [CrossRef]
- Silva, F.A.R.; Rodrigues, B.L.; Ayrizono, M.d.L.S.; Leal, R.F. The Immunological Basis of Inflammatory Bowel Disease. Gastroenterol. Res. Pract. 2016, 2016, e2097274. [Google Scholar] [CrossRef] [Green Version]
- Franke, A.; Balschun, T.; Karlsen, T.H.; Sventoraityte, J.; Nikolaus, S.; Mayr, G.; Domingues, F.S.; Albrecht, M.; Nothnagel, M.; Ellinghaus, D.; et al. Sequence Variants in IL10, ARPC2 and Multiple Other Loci Contribute to Ulcerative Colitis Susceptibility. Nat. Genet. 2008, 40, 1319–1323. [Google Scholar] [CrossRef]
- Negroni, A.; Pierdomenico, M.; Cucchiara, S.; Stronati, L. NOD2 and Inflammation: Current Insights. J. Inflamm. Res. 2018, 11, 49–60. [Google Scholar] [CrossRef] [Green Version]
- Neurath, M.F.; Fuss, I.; Kelsall, B.L.; Presky, D.H.; Waegell, W.; Strober, W. Experimental Granulomatous Colitis in Mice Is Abrogated by Induction of TGF-Beta-Mediated Oral Tolerance. J. Exp. Med. 1996, 183, 2605–2616. [Google Scholar] [CrossRef] [Green Version]
- Kam, L.Y.; Targan, S.R. TNF-Alpha Antagonists for the Treatment of Crohn’s Disease. Expert Opin. Pharmacother. 2000, 1, 615–622. [Google Scholar] [CrossRef]
- Monteleone, G.; Boirivant, M.; Pallone, F.; MacDonald, T.T. TGF-Beta1 and Smad7 in the Regulation of IBD. Mucosal Immunol. 2008, 1 (Suppl. S1), S50–S53. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, S.; Chaudhary, R.; Carpani, M.; Playford, R. Interfering with Interferons in Inflammatory Bowel Disease. Gut 2006, 55, 1071–1073. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Chen, Z. Inflammatory Bowel Disease Related Innate Immunity and Adaptive Immunity. Am. J. Transl. Res. 2016, 8, 2490–2497. [Google Scholar] [PubMed]
- Monteleone, I.; Sarra, M.; Pallone, F.; Monteleone, G. Th17-Related Cytokines in Inflammatory Bowel Diseases: Friends or Foes? Curr. Mol. Med. 2012, 12, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Yamada, A.; Arakaki, R.; Saito, M.; Tsunematsu, T.; Kudo, Y.; Ishimaru, N. Role of Regulatory T Cell in the Pathogenesis of Inflammatory Bowel Disease. World J. Gastroenterol. 2016, 22, 2195–2205. [Google Scholar] [CrossRef]
- Izcue, A.; Coombes, J.L.; Powrie, F. Regulatory T Cells Suppress Systemic and Mucosal Immune Activation to Control Intestinal Inflammation. Immunol. Rev. 2006, 212, 256–271. [Google Scholar] [CrossRef]
- Boden, E.K.; Snapper, S.B. Regulatory T Cells in Inflammatory Bowel Disease. Curr. Opin. Gastroenterol. 2008, 24, 733–741. [Google Scholar] [CrossRef]
- MacDermott, R.P.; Nash, G.S.; Bertovich, M.J.; Seiden, M.V.; Bragdon, M.J.; Beale, M.G. Alterations of IgM, IgG, and IgA Synthesis and Secretion by Peripheral Blood and Intestinal Mononuclear Cells from Patients with Ulcerative Colitis and Crohn’s Disease. Gastroenterology 1981, 81, 844–852. [Google Scholar] [CrossRef]
- Uo, M.; Hisamatsu, T.; Miyoshi, J.; Kaito, D.; Yoneno, K.; Kitazume, M.T.; Mori, M.; Sugita, A.; Koganei, K.; Matsuoka, K.; et al. Mucosal CXCR4+ IgG Plasma Cells Contribute to the Pathogenesis of Human Ulcerative Colitis through FcγR-Mediated CD14 Macrophage Activation. Gut 2013, 62, 1734–1744. [Google Scholar] [CrossRef]
- Tsianos, E.V.; Katsanos, K. Do We Really Understand What the Immunological Disturbances in Inflammatory Bowel Disease Mean? World J. Gastroenterol. 2009, 15, 521–525. [Google Scholar] [CrossRef]
- Hodgson, H.J.F.; Jewell, D.P. The Humoral Immune System in Inflammatory Bowel Disease. Dig. Dis. Sci. 1978, 23, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Arai, S.; Osawa, T.; Ohigashi, H.; Yoshikawa, M.; Kaminogawa, S.; Watanabe, M.; Ogawa, T.; Okubo, K.; Watanabe, S.; Nishino, H.; et al. A Mainstay of Functional Food Science in Japan—History, Present Status, and Future Outlook. Biosci. Biotechnol. Biochem. 2001, 65, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, C.L. Regulatory Frameworks for Functional Foods and Dietary Supplements. Nutr. Rev. 2004, 62, 55–59. [Google Scholar] [CrossRef]
- FSAI. Functional Food; Food Safety Authority of Ireland: Dublin, Ireland, 2007. [Google Scholar]
- Martirosyan, D.M.; Singh, J. A New Definition of Functional Food by FFC: What Makes a New Definition Unique? Funct. Foods Health Dis. 2015, 5, 209. [Google Scholar] [CrossRef]
- FUFOSE. Scientific Concepts of Functional Foods in Europe Consensus Document. Br. J. Nutr. 1999, 81, S1–S27. [Google Scholar] [CrossRef] [Green Version]
- ISI North America Technical Committee. Safety Assessment and Potential Health Benefits of Food Components Based on Selected Scientific Criteria. Crit. Rev. Food Sci. Nutr. 1999, 39, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Canada Health ARCHIVED. Policy Paper—Nutraceuticals/Functional Foods and Health Claims on Foods. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-labelling/health-claims/nutraceuticals-functional-foods-health-claims-foods-policy-paper.html (accessed on 12 August 2022).
- Arai, S.; Morinaga, Y.; Yoshikawa, T.; Ichiishi, E.; KISO, Y.; Yamazaki, M.; Morotomi, M.; Shimizu, M.; Kuwata, T.; Kaminogawa, S. Recent Trends in Functional Food Science and the Industry in Japan. Biosci. Biotechnol. Biochem. 2002, 66, 2017–2029. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Liu, Y. Potential Interventions for Novel Coronavirus in China: A Systematic Review. J. Med. Virol. 2020, 92, 479–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akintola, C.; Finnegan, D.; Hunt, N.; Lalor, R.; O’Neill, S.; Loscher, C. Nutrition Nutraceuticals: A Proactive Approach for Healthcare. In Advances in Nutraceuticals and Functional Foods; Apple Academic Press: Ontario, CA, USA, 2022; pp. 123–172. ISBN 978-1-00-327708-8. [Google Scholar]
- Sun, H.; Jenssen, H.; Sun, H.; Jenssen, H. Milk Derived Peptides with Immune Stimulating Antiviral Properties. In Milk Protein; IntechOpen: London, UK, 2012. [Google Scholar]
- Gallo, V.; Giansanti, F.; Arienzo, A.; Antonini, G. Antiviral Properties of Whey Proteins and Their Activity against SARS-CoV-2 Infection. J. Funct. Foods 2022, 89, 104932. [Google Scholar] [CrossRef]
- Fan, H.; Hong, B.; Luo, Y.; Peng, Q.; Wang, L.; Jin, X.; Chen, Y.; Hu, Y.; Shi, Y.; Li, T.; et al. The Effect of Whey Protein on Viral Infection and Replication of SARS-CoV-2 and Pangolin Coronavirus in Vitro. Signal Transduct. Target. Ther. 2020, 5, 275. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, Q.; Guo, D. Emerging Coronaviruses: Genome Structure, Replication, and Pathogenesis. J. Med. Virol. 2020, 92, 418–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wajs, J.; Król, K.; Brodziak, A. Milk and Dairy Products as a Source of Antiviral Compounds; E-Wydawnictwo. Prawnicza i Ekonomiczna Biblioteka Cyfrowa. Wydział Prawa, Administracji i Ekonomii Uniwersytetu Wrocławskiego: Wroclaw, Poland, 2021. [Google Scholar] [CrossRef]
- Senapathi, J.; Bommakanti, A.; Mallepalli, S.; Mukhopadhyay, S.; Kondapi, A.K. Sulfonate Modified Lactoferrin Nanoparticles as Drug Carriers with Dual Activity against HIV-1. Colloids Surf. B Biointerfaces 2020, 191, 110979. [Google Scholar] [CrossRef] [PubMed]
- Legrand, D.; Elass, E.; Carpentier, M.; Mazurier, J. Interactions of Lactoferrin with Cells Involved in Immune FunctionThis Paper Is One of a Selection of Papers Published in This Special Issue, Entitled 7th International Conference on Lactoferrin: Structure, Function, and Applications, and Has Undergone the Journal’s Usual Peer Review Process. Biochem. Cell Biol. 2006, 84, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Puddu, P.; Carollo, M.G.; Belardelli, F.; Valenti, P.; Gessani, S. Role of Endogenous Interferon and LPS in the Immunomodulatory Effects of Bovine Lactoferrin in Murine Peritoneal Macrophages. J. Leukoc. Biol. 2007, 82, 347–353. [Google Scholar] [CrossRef]
- Bakhshandeh, B.; Sorboni, S.G.; Javanmard, A.-R.; Mottaghi, S.S.; Mehrabi, M.; Sorouri, F.; Abbasi, A.; Jahanafrooz, Z. Variants in ACE2; Potential Influences on Virus Infection and COVID-19 Severity. Infect. Genet. Evol. 2021, 90, 104773. [Google Scholar] [CrossRef]
- Duan, L.; Zheng, Q.; Zhang, H.; Niu, Y.; Lou, Y.; Wang, H. The SARS-CoV-2 Spike Glycoprotein Biosynthesis, Structure, Function, and Antigenicity: Implications for the Design of Spike-Based Vaccine Immunogens. Front. Immunol. 2020, 11, 576622. [Google Scholar] [CrossRef]
- Serrano, G.; Kochergina, I.; Albors, A.; Diaz, E.; Oroval, M.; Hueso, G.; Serrano, J.M. Liposomal Lactoferrin as Potential Preventative and Cure for COVID-19. Int. J. Res. Health Sci. 2020, 8, 8–15. [Google Scholar] [CrossRef]
- Chang, R.; Ng, T.B.; Sun, W.-Z. Lactoferrin as Potential Preventative and Adjunct Treatment for COVID-19. Int. J. Antimicrob. Agents 2020, 56, 106118. [Google Scholar] [CrossRef]
- Inagaki, M.; Muranishi, H.; Yamada, K.; Kakehi, K.; Uchida, K.; Suzuki, T.; Yabe, T.; Nakagomi, T.; Nakagomi, O.; Kanamaru, Y. Bovine κ-Casein Inhibits Human Rotavirus (HRV) Infection via Direct Binding of Glycans to HRV. J. Dairy Sci. 2014, 97, 2653–2661. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Ye, X.; Ng, T.B. First Demonstration of an Inhibitory Activity of Milk Proteins against Human Immunodeficiency Virus-1 Reverse Transcriptase and the Effect of Succinylation. Life Sci. 2000, 67, 2745–2752. [Google Scholar] [CrossRef]
- Ng, T.B.; Ye, X.Y. A Polymeric Immunoglobulin Receptor-like Milk Protein with Inhibitory Activity on Human Immunodeficiency Virus Type 1 Reverse Transcriptase. Int. J. Biochem. Cell Biol. 2004, 36, 2242–2249. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.B.; Cheung, R.C.F.; Wong, J.H.; Wang, Y.; Ip, D.T.M.; Wan, D.C.C.; Xia, J. Antiviral Activities of Whey Proteins. Appl. Microbiol. Biotechnol. 2015, 99, 6997–7008. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, P.; Wang, H.; Luo, Y.; Wan, L.; Jiang, M.; Chu, Y. Lactoferrin for the Treatment of COVID-19 (Review). Exp. Ther. Med. 2020, 20, 272. [Google Scholar] [CrossRef]
- Siqueiros-Cendón, T.; Arévalo-Gallegos, S.; Iglesias-Figueroa, B.F.; García-Montoya, I.A.; Salazar-Martínez, J.; Rascón-Cruz, Q. Immunomodulatory Effects of Lactoferrin. Acta Pharmacol. Sin. 2014, 35, 557–566. [Google Scholar] [CrossRef]
- Hamida, R.S.; Shami, A.; Ali, M.A.; Almohawes, Z.N.; Mohammed, A.E.; Bin-Meferij, M.M. Kefir: A Protective Dietary Supplementation against Viral Infection. Biomed. Pharmacother. 2021, 133, 110974. [Google Scholar] [CrossRef] [PubMed]
- Al Kassaa, I.; Hober, D.; Hamze, M.; Chihib, N.E.; Drider, D. Antiviral Potential of Lactic Acid Bacteria and Their Bacteriocins. Probiotics Antimicrob. Proteins 2014, 6, 177–185. [Google Scholar] [CrossRef]
- Peluzio, M.d.C.G.; Dias, M.d.M.e.; Martinez, J.A.; Milagro, F.I. Kefir and Intestinal Microbiota Modulation: Implications in Human Health. Front. Nutr. 2021, 8, 638740. [Google Scholar] [CrossRef]
- Pražnikar, Z.J.; Kenig, S.; Vardjan, T.; Bizjak, M.Č.; Petelin, A. Effects of Kefir or Milk Supplementation on Zonulin in Overweight Subjects. J. Dairy Sci. 2020, 103, 3961–3970. [Google Scholar] [CrossRef]
- Freitas, M. Chapter 24—The Benefits of Yogurt, Cultures, and Fermentation. In The Microbiota in Gastrointestinal Pathophysiology; Floch, M.H., Ringel, Y., Allan Walker, W., Eds.; Academic Press: Boston, MA, USA, 2017; pp. 209–223. ISBN 978-0-12-804024-9. [Google Scholar]
- Gouda, A.S.; Adbelruhman, F.G.; Sabbah Alenezi, H.; Mégarbane, B. Theoretical Benefits of Yogurt-Derived Bioactive Peptides and Probiotics in COVID-19 Patients—A Narrative Review and Hypotheses. Saudi J. Biol. Sci. 2021, 28, 5897–5905. [Google Scholar] [CrossRef]
- Pei, R.; Martin, D.A.; DiMarco, D.M.; Bolling, B.W. Evidence for the Effects of Yogurt on Gut Health and Obesity. Crit. Rev. Food Sci. Nutr. 2017, 57, 1569–1583. [Google Scholar] [CrossRef]
- Popovic, N.; Brdarić, E.; Djokic, J.; Dinic, M.; Veljovic, K.; Golić, N.; Terzic-Vidojevic, A. Yogurt Produced by Novel Natural Starter Cultures Improves Gut Epithelial Barrier In Vitro. Microorganisms 2020, 8, 1586. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, T.; Sequoia, J. Probiotics for Gastrointestinal Conditions: A Summary of the Evidence. Am. Fam. Physician 2017, 96, 170–178. [Google Scholar] [PubMed]
- Mohamadshahi, M.; Veissi, M.; Haidari, F.; Shahbazian, H.; Kaydani, G.-A.; Mohammadi, F. Effects of Probiotic Yogurt Consumption on Inflammatory Biomarkers in Patients with Type 2 Diabetes. Bioimpacts 2014, 4, 83–88. [Google Scholar] [CrossRef] [PubMed]
- De Moreno De Leblanc, A.; Chaves, S.; Perdigón, G. Effect of Yoghurt on the Cytokine Profile Using a Murine Model of Intestinal Inflammation. Eur. J. Inflamm. 2009, 7, 97–109. [Google Scholar] [CrossRef] [Green Version]
- Yao, G.; Yu, J.; Hou, Q.; Hui, W.; Liu, W.; Kwok, L.-Y.; Menghe, B.; Sun, T.; Zhang, H.; Zhang, W. A Perspective Study of Koumiss Microbiome by Metagenomics Analysis Based on Single-Cell Amplification Technique. Front. Microbiol. 2017, 8, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, H.; Ma, H.; Hou, Q.; Li, W.; Xu, H.; Liu, W.; Sun, Z.; Haobisi, H.; Menghe, B. Profiling of Koumiss Microbiota and Organic Acids and Their Effects on Koumiss Taste. BMC Microbiol. 2020, 20, 85. [Google Scholar] [CrossRef]
- Ya, T.; Zhang, Q.; Chu, F.; Merritt, J.; Bilige, M.; Sun, T.; Du, R.; Zhang, H. Immunological Evaluation of Lactobacillus Casei Zhang: A Newly Isolated Strain from Koumiss in Inner Mongolia, China. BMC Immunol. 2008, 9, 68. [Google Scholar] [CrossRef] [Green Version]
- Fukushima, Y.; Kawata, Y.; Hara, H.; Terada, A.; Mitsuoka, T. Effect of a Probiotic Formula on Intestinal Immunoglobulin A Production in Healthy Children. Int. J. Food Microbiol. 1998, 42, 39–44. [Google Scholar] [CrossRef]
- Mathur, H.; Beresford, T.P.; Cotter, P.D. Health Benefits of Lactic Acid Bacteria (LAB) Fermentates. Nutrients 2020, 12, 1679. [Google Scholar] [CrossRef]
- Moyad, M.A.; Robinson, L.E.; Zawada, E.T.; Kittelsrud, J.M.; Chen, D.-G.; Reeves, S.G.; Weaver, S.E. Effects of a Modified Yeast Supplement on Cold/Flu Symptoms. Urol. Nurs. 2008, 28, 50–55. [Google Scholar]
- Moyad, M.A.; Robinson, L.E.; Zawada, E.T.; Kittelsrud, J.; Chen, D.-G.; Reeves, S.G.; Weaver, S. Immunogenic Yeast-Based Fermentate for Cold/Flu-like Symptoms in Nonvaccinated Individuals. J. Altern. Complement. Med. 2010, 16, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.S.; Martinussen, T.; Flambard, B.; Sørensen, K.I.; Otte, J. Peptide Profiles and Angiotensin-I-Converting Enzyme Inhibitory Activity of Fermented Milk Products: Effect of Bacterial Strain, Fermentation PH, and Storage Time. Int. Dairy J. 2009, 19, 155–165. [Google Scholar] [CrossRef]
- Kırdar, S.S. Therapeutics Effects and Health Benefits of the Caucasus Koumiss: A Review. Annu. Res. Rev. Biol. 2021, 36, 47–56. [Google Scholar] [CrossRef]
- Jiang, L.-L.; Gong, X.; Ji, M.-Y.; Wang, C.-C.; Wang, J.-H.; Li, M.-H. Bioactive Compounds from Plant-Based Functional Foods: A Promising Choice for the Prevention and Management of Hyperuricemia. Foods 2020, 9, 973. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, I.C.F.R.; Morales, P.; Barros, L. Wild Plants, Mushrooms and Nuts: Functional Food Properties and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2017; ISBN 978-1-118-94462-2. [Google Scholar]
- Jiang, L.; Zhang, G.; Li, Y.; Shi, G.; Li, M. Potential Application of Plant-Based Functional Foods in the Development of Immune Boosters. Front. Pharmacol. 2021, 12, 637782. [Google Scholar] [CrossRef]
- Angeles-Agdeppa, I.; Nacis, J.S.; Capanzana, M.V.; Dayrit, F.M.; Tanda, K.V. Virgin Coconut Oil Is Effective in Lowering C-Reactive Protein Levels among Suspect and Probable Cases of COVID-19. J. Funct. Foods 2021, 83, 104557. [Google Scholar] [CrossRef]
- WebMD Coconut Oil: Is It Good for You? Available online: https://www.webmd.com/diet/coconut-oil-good-for-you (accessed on 3 August 2022).
- Joshi, S.; Kaushik, V.; Gode, V.; Mhaskar, S. Coconut Oil and Immunity: What Do We Really Know about It so Far? J. Assoc. Phys. India 2020, 68, 67–72. [Google Scholar]
- Intahphuak, S.; Khonsung, P.; Panthong, A. Anti-Inflammatory, Analgesic, and Antipyretic Activities of Virgin Coconut Oil. Pharm. Biol. 2010, 48, 151–157. [Google Scholar] [CrossRef] [Green Version]
- Djurasevic, S.; Bojic, S.; Nikolić, B.; Dimkić, I.; Todorovic, Z.; Djordjevic, J.; Mitić-Ćulafić, D. Beneficial Effect of Virgin Coconut Oil on Alloxan-Induced Diabetes and Microbiota Composition in Rats. Plant Foods Hum. Nutr. 2018, 73, 295–301. [Google Scholar] [CrossRef]
- Yeap, S.K.; Beh, B.K.; Ali, N.M.; Yusof, H.M.; Ho, W.Y.; Koh, S.P.; Alitheen, N.B.; Long, K. Antistress and Antioxidant Effects of Virgin Coconut Oil in Vivo. Exp. Ther. Med. 2015, 9, 39–42. [Google Scholar] [CrossRef] [Green Version]
- Dumancas, G.; Viswanath, L.; Leon, A.; Ramasahayam, S.; Maples, R.; Hikkaduwa Koralege, R.; Don, U.; Perera, U.D.N.; Langford, J.; Shakir, A.; et al. Health Benefits of Virgin Coconut Oil. In Vegetable Oil: Properties, Uses and Benefits; Lybrate: Delhi, India, 2016. [Google Scholar]
- Widianingrum, D.C.; Noviandi, C.T.; Salasia, S.I.O. Antibacterial and Immunomodulator Activities of Virgin Coconut Oil (VCO) against Staphylococcus Aureus. Heliyon 2019, 5, e02612. [Google Scholar] [CrossRef] [Green Version]
- Varma, S.R.; Sivaprakasam, T.O.; Arumugam, I.; Dilip, N.; Raghuraman, M.; Pavan, K.B.; Rafiq, M.; Paramesh, R. In Vitro Anti-Inflammatory and Skin Protective Properties of Virgin Coconut Oil. J. Tradit. Complement. Med. 2018, 9, 5–14. [Google Scholar] [CrossRef]
- Widhiarta, D.K.D. Virgin Coconut Oil for HIV—Positive People. CORD 2016, 32, 8. [Google Scholar] [CrossRef]
- Silalahi, J.; Rosidah, R.; Yuandani, Y.; Satria, D. Virgin Coconut Oil Modulates Tcd4+ and Tcd8+ Cell Profile of Doxorubicin-Induced Immune-Suppressed Rats. Asian J. Pharm. Clin. Res. 2018, 11, 37. [Google Scholar] [CrossRef] [Green Version]
- Komatsuzaki, N.; Arai, S.; Fujihara, S.; Wijesekara, R. Effect of Intake of Virgin Coconut Oil (Cocos nucifera L.) on the Spleen and Small Intestinal Immune Cells and Liver Lipid of Mice. Ceylon J. Sci. 2021, 50, 103. [Google Scholar] [CrossRef]
- Link, R. Why Extra Virgin Olive Oil Is the Healthiest Fat on Earth. Available online: https://www.healthline.com/nutrition/extra-virgin-olive-oil (accessed on 3 August 2022).
- Omar, S.H. Oleuropein in Olive and Its Pharmacological Effects. Sci. Pharm. 2010, 78, 133–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jimenez-Lopez, C.; Carpena, M.; Lourenço-Lopes, C.; Gallardo-Gomez, M.; Lorenzo, J.M.; Barba, F.J.; Prieto, M.A.; Simal-Gandara, J. Bioactive Compounds and Quality of Extra Virgin Olive Oil. Foods 2020, 9, 1014. [Google Scholar] [CrossRef]
- Vrdoljak, J.; Kumric, M.; Vilovic, M.; Martinovic, D.; Tomic, I.J.; Krnic, M.; Ticinovic Kurir, T.; Bozic, J. Effects of Olive Oil and Its Components on Intestinal Inflammation and Inflammatory Bowel Disease. Nutrients 2022, 14, 757. [Google Scholar] [CrossRef]
- Fredrickson, W.R. Method and Composition for Antiviral Therapy; World Intellectual Property Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Olalla, J.; García de Lomas, J.M.; Chueca, N.; Pérez-Stachowski, X.; De Salazar, A.; Del Arco, A.; Plaza-Díaz, J.; De la Torre, J.; Prada, J.L.; García-Alegría, J.; et al. Effect of Daily Consumption of Extra Virgin Olive Oil on the Lipid Profile and Microbiota of HIV-Infected Patients over 50 Years of Age. Medicine 2019, 98, e17528. [Google Scholar] [CrossRef]
- Kozić Dokmanović, S.; Kolovrat, K.; Laškaj, R.; Jukić, V.; Vrkić, N.; Begovac, J. Effect of Extra Virgin Olive Oil on Biomarkers of Inflammation in HIV-Infected Patients: A Randomized, Crossover, Controlled Clinical Trial. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 2406. [Google Scholar] [CrossRef] [Green Version]
- Millman, J.F.; Okamoto, S.; Teruya, T.; Uema, T.; Ikematsu, S.; Shimabukuro, M.; Masuzaki, H. Extra-Virgin Olive Oil and the Gut-Brain Axis: Influence on Gut Microbiota, Mucosal Immunity, and Cardiometabolic and Cognitive Health. Nutr. Rev. 2021, 79, 1362–1374. [Google Scholar] [CrossRef] [PubMed]
- Martín-Peláez, S.; Castañer, O.; Solà, R.; Motilva, M.J.; Castell, M.; Pérez-Cano, F.J.; Fitó, M. Influence of Phenol-Enriched Olive Oils on Human Intestinal Immune Function. Nutrients 2016, 8, 213. [Google Scholar] [CrossRef] [Green Version]
- Alvarez-Laderas, I.; Ramos, T.L.; Medrano, M.; Caracuel-García, R.; Barbado, M.V.; Sánchez-Hidalgo, M.; Zamora, R.; Alarcón-de-la-Lastra, C.; Hidalgo, F.J.; Piruat, J.I.; et al. Polyphenolic Extract (PE) from Olive Oil Exerts a Potent Immunomodulatory Effect and Prevents Graft-versus-Host Disease in a Mouse Model. Biol. Blood Marrow Transplant. 2020, 26, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Selverajah, M.; Zakaria, Z.A.; Long, K.; Ahmad, Z.; Yaacob, A.; Somchit, M.N. Anti-Ulcerogenic Activity of Virgin Coconut Oil Contribute to the Stomach Health of Humankind. CELLMED 2016, 6, 11.1–11.7. [Google Scholar] [CrossRef] [Green Version]
- Tangney, C.C.; Rasmussen, H.E. Polyphenols, Inflammation, and Cardiovascular Disease. Curr. Atheroscler. Rep. 2013, 15, 324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menicacci, B.; Cipriani, C.; Margheri, F.; Mocali, A.; Giovannelli, L. Modulation of the Senescence-Associated Inflammatory Phenotype in Human Fibroblasts by Olive Phenols. Int. J. Mol. Sci. 2017, 18, 2275. [Google Scholar] [CrossRef] [Green Version]
- Serra, G.; Incani, A.; Serreli, G.; Porru, L.; Melis, M.P.; Tuberoso, C.I.G.; Rossin, D.; Biasi, F.; Deiana, M. Olive Oil Polyphenols Reduce Oxysterols -Induced Redox Imbalance and pro-Inflammatory Response in Intestinal Cells. Redox Biol. 2018, 17, 348–354. [Google Scholar] [CrossRef]
- Hathaway, D.; Pandav, K.; Patel, M.; Riva-Moscoso, A.; Singh, B.M.; Patel, A.; Min, Z.C.; Singh-Makkar, S.; Sana, M.K.; Sanchez-Dopazo, R.; et al. Omega 3 Fatty Acids and COVID-19: A Comprehensive Review. Infect. Chemother. 2020, 52, 478–495. [Google Scholar] [CrossRef]
- Chiang, N.; Serhan, C.N. Specialized Pro-Resolving Mediator Network: An Update on Production and Actions. Essays Biochem. 2020, 64, 443–462. [Google Scholar] [CrossRef]
- Arnardottir, H.; Pawelzik, S.-C.; Öhlund Wistbacka, U.; Artiach, G.; Hofmann, R.; Reinholdsson, I.; Braunschweig, F.; Tornvall, P.; Religa, D.; Bäck, M. Stimulating the Resolution of Inflammation Through Omega-3 Polyunsaturated Fatty Acids in COVID-19: Rationale for the COVID-Omega-F Trial. Front. Physiol. 2021, 11, 1748. [Google Scholar] [CrossRef]
- Calder, P.C. Marine Omega-3 Fatty Acids and Inflammatory Processes: Effects, Mechanisms and Clinical Relevance. Biochim. Biophys. Acta 2015, 1851, 469–484. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Bi, Z.; Yang, C.; Guo, Y.; Yuan, J.; Li, L.; Guo, Y. Effects of Different Doses of Omega-3 Polyunsaturated Fatty Acids on Gut Microbiota and Immunity. Food Nutr. Res. 2021, 65. [Google Scholar] [CrossRef] [PubMed]
- Eslamloo, K.; Xue, X.; Hall, J.R.; Smith, N.C.; Caballero-Solares, A.; Parrish, C.C.; Taylor, R.G.; Rise, M.L. Transcriptome Profiling of Antiviral Immune and Dietary Fatty Acid Dependent Responses of Atlantic Salmon Macrophage-like Cells. BMC Genom. 2017, 18, 706. [Google Scholar] [CrossRef] [PubMed]
- Willemsen, L.E.M.; Koetsier, M.A.; Balvers, M.; Beermann, C.; Stahl, B.; van Tol, E.A.F. Polyunsaturated Fatty Acids Support Epithelial Barrier Integrity and Reduce IL-4 Mediated Permeability in Vitro. Eur. J. Nutr. 2008, 47, 183–191. [Google Scholar] [CrossRef]
- Hillier, K.; Jewell, R.; Dorrell, L.; Smith, C.L. Incorporation of Fatty Acids from Fish Oil and Olive Oil into Colonic Mucosal Lipids and Effects upon Eicosanoid Synthesis in Inflammatory Bowel Disease. Gut 1991, 32, 1151–1155. [Google Scholar] [CrossRef] [Green Version]
- Bellenger, J.; Bellenger, S.; Bourragat, A.; Escoula, Q.; Weill, P.; Narce, M. Intestinal Microbiota Mediates the Beneficial Effects of N-3 Polyunsaturated Fatty Acids during Dietary Obesity. OCL 2021, 28, 21. [Google Scholar] [CrossRef]
- Watson, H.; Mitra, S.; Croden, F.C.; Taylor, M.; Wood, H.M.; Perry, S.L.; Spencer, J.A.; Quirke, P.; Toogood, G.J.; Lawton, C.L.; et al. A Randomised Trial of the Effect of Omega-3 Polyunsaturated Fatty Acid Supplements on the Human Intestinal Microbiota. Gut 2018, 67, 1974–1983. [Google Scholar] [CrossRef]
- Costantini, L.; Molinari, R.; Farinon, B.; Merendino, N. Impact of Omega-3 Fatty Acids on the Gut Microbiota. Int. J. Mol. Sci. 2017, 18, 2645. [Google Scholar] [CrossRef] [Green Version]
- Rivollier, A.; He, J.; Kole, A.; Valatas, V.; Kelsall, B.L. Inflammation Switches the Differentiation Program of Ly6Chi Monocytes from Antiinflammatory Macrophages to Inflammatory Dendritic Cells in the Colon. J. Exp. Med. 2012, 209, 139–155. [Google Scholar] [CrossRef] [Green Version]
- Jackiewicz, A.; Czarnecki, M.; Knysz, B. Effect of Diet on Lipid Profile in HIV-Infected Patients. HIV AIDS Rev. 2018, 17, 159–163. [Google Scholar] [CrossRef]
- Imai, Y. Role of Omega-3 PUFA-Derived Mediators, the Protectins, in Influenza Virus Infection. Biochim. Biophys. Acta (BBA)—Mol. Cell Biol. Lipids 2015, 1851, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Darwesh, A.M.; Bassiouni, W.; Sosnowski, D.K.; Seubert, J.M. Can N-3 Polyunsaturated Fatty Acids Be Considered a Potential Adjuvant Therapy for COVID-19-Associated Cardiovascular Complications? Pharmacol. Ther. 2021, 219, 107703. [Google Scholar] [CrossRef]
- Thul, S.; Labat, C.; Temmar, M.; Benetos, A.; Bäck, M. Low Salivary Resolvin D1 to Leukotriene B4 Ratio Predicts Carotid Intima Media Thickness: A Novel Biomarker of Non-Resolving Vascular Inflammation. Eur. J. Prev. Cardiol. 2017, 24, 903–906. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C.; Bosco, N.; Bourdet-Sicard, R.; Capuron, L.; Delzenne, N.; Doré, J.; Franceschi, C.; Lehtinen, M.J.; Recker, T.; Salvioli, S.; et al. Health Relevance of the Modification of Low Grade Inflammation in Ageing (Inflammageing) and the Role of Nutrition. Ageing Res. Rev. 2017, 40, 95–119. [Google Scholar] [CrossRef] [PubMed]
- Mullen, A.; Loscher, C.E.; Roche, H.M. Anti-Inflammatory Effects of EPA and DHA Are Dependent upon Time and Dose-Response Elements Associated with LPS Stimulation in THP-1-Derived Macrophages. J. Nutr. Biochem. 2010, 21, 444–450. [Google Scholar] [CrossRef]
- Draper, E.; Reynolds, C.M.; Canavan, M.; Mills, K.H.; Loscher, C.E.; Roche, H.M. Omega-3 Fatty Acids Attenuate Dendritic Cell Function via NF-ΚB Independent of PPARγ. J. Nutr. Biochem. 2011, 22, 784–790. [Google Scholar] [CrossRef]
- Endres, S.; Meydani, S.N.; Ghorbani, R.; Schindler, R.; Dinarello, C.A. Dietary Supplementation with N-3 Fatty Acids Suppresses Interleukin-2 Production and Mononuclear Cell Proliferation. J. Leukoc. Biol. 1993, 54, 599–603. [Google Scholar] [CrossRef]
- Meydani, S.N.; Endres, S.; Woods, M.M.; Goldin, B.R.; Soo, C.; Morrill-Labrode, A.; Dinarello, C.A.; Gorbach, S.L. Oral (n-3) Fatty Acid Supplementation Suppresses Cytokine Production and Lymphocyte Proliferation: Comparison between Young and Older Women. J. Nutr. 1991, 121, 547–555. [Google Scholar] [CrossRef]
- Kim, W.; Khan, N.A.; McMurray, D.N.; Prior, I.A.; Wang, N.; Chapkin, R.S. Regulatory Activity of Polyunsaturated Fatty Acids in T-Cell Signaling. Prog. Lipid Res. 2010, 49, 250–261. [Google Scholar] [CrossRef] [Green Version]
- Mizota, T.; Fujita-Kambara, C.; Matsuya, N.; Hamasaki, S.; Fukudome, T.; Goto, H.; Nakane, S.; Kondo, T.; Matsuo, H. Effect of Dietary Fatty Acid Composition on Th1/Th2 Polarization in Lymphocytes. JPEN J. Parenter. Enter. Nutr. 2009, 33, 390–396. [Google Scholar] [CrossRef] [Green Version]
- Cao, W.; Wang, C.; Chin, Y.; Chen, X.; Gao, Y.; Yuan, S.; Xue, C.; Wang, Y.; Tang, Q. DHA-Phospholipids (DHA-PL) and EPA-Phospholipids (EPA-PL) Prevent Intestinal Dysfunction Induced by Chronic Stress. Food Funct. 2019, 10, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Weldon, S.M.; Mullen, A.C.; Loscher, C.E.; Hurley, L.A.; Roche, H.M. Docosahexaenoic Acid Induces an Anti-Inflammatory Profile in Lipopolysaccharide-Stimulated Human THP-1 Macrophages More Effectively than Eicosapentaenoic Acid. J. Nutr. Biochem. 2007, 18, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Dennis, E.A.; Norris, P.C. Eicosanoid Storm in Infection and Inflammation. Nat. Rev. Immunol. 2015, 15, 511–523. [Google Scholar] [CrossRef] [Green Version]
- Hammock, B.D.; Wang, W.; Gilligan, M.M.; Panigrahy, D. Eicosanoids: The Overlooked Storm in Coronavirus Disease 2019 (COVID-19)? Am. J. Pathol. 2020, 190, 1782–1788. [Google Scholar] [CrossRef]
- Calder, P.C. Omega-3 Fatty Acids and Inflammatory Processes: From Molecules to Man. Biochem. Soc. Trans. 2017, 45, 1105–1115. [Google Scholar] [CrossRef] [Green Version]
- Health Service Executive. Vitamins and Minerals—Vitamin D. Available online: https://www2.hse.ie/conditions/vitamins-and-minerals/vitamin-d/ (accessed on 4 July 2022).
- National Institute of Health Office of Dietary Supplements. Vitamin D. Available online: https://ods.od.nih.gov/factsheets/VitaminD-Consumer/ (accessed on 4 July 2022).
- Aranow, C. Vitamin D and the Immune System. J. Investig. Med. 2011, 59, 881–886. [Google Scholar] [CrossRef] [Green Version]
- Faul, J.L.; Kerley, C.P.; Love, B.; O’Neill, E.; Cody, C.; Tormey, W.; Hutchinson, K.; Cormican, L.J.; Burke, C.M. Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection. Ir. Med. J. 2021, 113, 84. [Google Scholar]
- McCartney, D.M.; Byrne, D.G. Optimisation of Vitamin D Status for Enhanced Immuno-Protection against COVID-19. Ir. Med. J. 2020, 113, 58. [Google Scholar] [PubMed]
- Walsh, L. Please Take Vitamin D to Protect against COVID-19, Say Irish Experts. Available online: https://www.breakingnews.ie/ireland/please-take-vitamin-d-to-protect-against-covid-19-say-irish-experts-1069537.html (accessed on 4 July 2022).
- Sundararaman, A.; Ray, M.; Ravindra, P.V.; Halami, P.M. Role of Probiotics to Combat Viral Infections with Emphasis on COVID-19. Appl. Microbiol. Biotechnol. 2020, 104, 8089–8104. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-G.; Wu, S.; Sun, J. Vitamin D, Vitamin D Receptor, and Tissue Barriers. Tissue Barriers 2013, 1, e23118. [Google Scholar] [CrossRef]
- Battistini, C.; Ballan, R.; Herkenhoff, M.E.; Saad, S.M.I.; Sun, J. Vitamin D Modulates Intestinal Microbiota in Inflammatory Bowel Diseases. Int. J. Mol. Sci. 2021, 22, 362. [Google Scholar] [CrossRef]
- Zhang, Y.-G.; Lu, R.; Xia, Y.; Zhou, D.; Petrof, E.; Claud, E.C.; Sun, J. Lack of Vitamin D Receptor Leads to Hyperfunction of Claudin-2 in Intestinal Inflammatory Responses. Inflamm. Bowel Dis. 2019, 25, 97–110. [Google Scholar] [CrossRef]
- Wang, J.; Thingholm, L.B.; Skiecevičienė, J.; Rausch, P.; Kummen, M.; Hov, J.R.; Degenhardt, F.; Heinsen, F.-A.; Rühlemann, M.C.; Szymczak, S.; et al. Genome-Wide Association Analysis Identifies Variation in Vitamin D Receptor and Other Host Factors Influencing the Gut Microbiota. Nat. Genet. 2016, 48, 1396–1406. [Google Scholar] [CrossRef]
- Rigby, W.F.; Denome, S.; Fanger, M.W. Regulation of Lymphokine Production and Human T Lymphocyte Activation by 1,25-Dihydroxyvitamin D3. Specific Inhibition at the Level of Messenger RNA. J. Clin. Investig. 1987, 79, 1659–1664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, W.-C.; Hanauer, S.B.; Li, Y.C. Mechanisms of Disease: Vitamin D and Inflammatory Bowel Disease. Nat. Rev. Gastroenterol. Hepatol. 2005, 2, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Sims, G.P.; Chen, X.X.; Gu, Y.Y.; Chen, S.; Lipsky, P.E. Modulatory Effects of 1,25-Dihydroxyvitamin D3 on Human B Cell Differentiation. J. Immunol. 2007, 179, 1634–1647. [Google Scholar] [CrossRef]
- Gammoh, N.Z.; Rink, L. Zinc in Infection and Inflammation. Nutrients 2017, 9, 624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute of Health Office of Dietary Supplements. Zinc. Available online: https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/ (accessed on 4 July 2022).
- Liu, M.-J.; Bao, S.; Bolin, E.R.; Burris, D.L.; Xu, X.; Sun, Q.; Killilea, D.W.; Shen, Q.; Ziouzenkova, O.; Belury, M.A.; et al. Zinc Deficiency Augments Leptin Production and Exacerbates Macrophage Infiltration into Adipose Tissue in Mice Fed a High-Fat Diet123. J. Nutr. 2013, 143, 1036–1045. [Google Scholar] [CrossRef] [Green Version]
- Siva, S.; Rubin, D.T.; Gulotta, G.; Wroblewski, K.; Pekow, J. Zinc Deficiency Is Associated with Poor Clinical Outcomes in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 152–157. [Google Scholar] [CrossRef] [Green Version]
- Read, S.A.; Obeid, S.; Ahlenstiel, C.; Ahlenstiel, G. The Role of Zinc in Antiviral Immunity. Adv. Nutr. 2019, 10, 696–710. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. The World Health Report 2002. Midwifery 2003, 19, 72–73. [Google Scholar] [CrossRef]
- Wessels, I.; Rolles, B.; Rink, L. The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis. Front. Immunol. 2020, 11, 1712. [Google Scholar] [CrossRef] [PubMed]
- de Almeida Brasiel, P.G. The Key Role of Zinc in Elderly Immunity: A Possible Approach in the COVID-19 Crisis. Clin. Nutr. ESPEN 2020, 38, 65–66. [Google Scholar] [CrossRef] [PubMed]
- Ibs, K.-H.; Rink, L. Zinc-Altered Immune Function. J. Nutr. 2003, 133, 1452S–1456S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skrovanek, S.; DiGuilio, K.; Bailey, R.; Huntington, W.; Urbas, R.; Mayilvaganan, B.; Mercogliano, G.; Mullin, J.M. Zinc and Gastrointestinal Disease. World J. Gastrointest. Pathophysiol. 2014, 5, 496–513. [Google Scholar] [CrossRef]
- Finamore, A.; Massimi, M.; Conti Devirgiliis, L.; Mengheri, E. Zinc Deficiency Induces Membrane Barrier Damage and Increases Neutrophil Transmigration in Caco-2 Cells. J. Nutr. 2008, 138, 1664–1670. [Google Scholar] [CrossRef] [Green Version]
- Baum, M.K.; Lai, S.; Sales, S.; Page, J.B.; Campa, A. Randomized Controlled Clinical Trial of Zinc Supplementation to Prevent Immunological Failure in HIV-Positive Adults. Clin. Infect. Dis. 2010, 50, 1653–1660. [Google Scholar] [CrossRef]
- Fenstermacher, K.J.; DeStefano, J.J. Mechanism of HIV Reverse Transcriptase Inhibition by Zinc. J. Biol. Chem. 2011, 286, 40433–40442. [Google Scholar] [CrossRef] [Green Version]
- te Velthuis, A.J.W.; van den Worm, S.H.E.; Sims, A.C.; Baric, R.S.; Snijder, E.J.; van Hemert, M.J. Zn(2+) Inhibits Coronavirus and Arterivirus RNA Polymerase Activity in Vitro and Zinc Ionophores Block the Replication of These Viruses in Cell Culture. PLoS Pathog. 2010, 6, e1001176. [Google Scholar] [CrossRef]
- Haase, H.; Rink, L. Zinc Signals and Immune Function. BioFactors 2014, 40, 27–40. [Google Scholar] [CrossRef]
- Hasegawa, H.; Suzuki, K.; Suzuki, K.; Nakaji, S.; Sugawara, K. Effects of Zinc on the Reactive Oxygen Species Generating Capacity of Human Neutrophils and on the Serum Opsonic Activity in Vitro. Luminescence 2000, 15, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Skalny, A.V.; Rink, L.; Ajsuvakova, O.P.; Aschner, M.; Gritsenko, V.A.; Alekseenko, S.I.; Svistunov, A.A.; Petrakis, D.; Spandidos, D.A.; Aaseth, J.; et al. Zinc and Respiratory Tract Infections: Perspectives for COVID-19 (Review). Int. J. Mol. Med. 2020, 46, 17–26. [Google Scholar] [CrossRef]
- Wessels, I.; Rink, L. Micronutrients in Autoimmune Diseases: Possible Therapeutic Benefits of Zinc and Vitamin D. J. Nutr. Biochem. 2020, 77, 108240. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Iñigo-Figueroa, G.; Maldonado-Fonllem, G.; Quihui-Cota, L.; Mendez-Estrada, R.O.; Velasquez-Contreras, C.; Canett-Romero, R.; Rascon-Duran, L.; Garibay-Escobar, A.; Robles-Zepeda, R.; Astiazaran-Garcia, H. The Effect of Dietary Zinc Level over the IgG Response in a Murine Model of Giardiasis. FASEB J. 2012, 26, 1027.12. [Google Scholar] [CrossRef]
- Kieliszek, M.; Błażejak, S. Selenium: Significance, and Outlook for Supplementation. Nutrition 2013, 29, 713–718. [Google Scholar] [CrossRef]
- Ross, A.C.; Caballero, B.H.; Cousins, R.J.; Tucker, K.L.; Ziegler, T.R. Modern Nutrition in Health and Disease, 11th ed.; Wolters Kluwer Health Adis (ESP): Waltham, MA, USA, 2012; ISBN 978-1-60547-461-8. [Google Scholar]
- Majeed, M.; Nagabhushanam, K.; Gowda, S.; Mundkur, L. An Exploratory Study of Selenium Status in Healthy Individuals and in Patients with COVID-19 in a South Indian Population: The Case for Adequate Selenium Status. Nutrition 2021, 82, 111053. [Google Scholar] [CrossRef]
- Rayman, M.P. Selenium and Human Health. Lancet 2012, 379, 1256–1268. [Google Scholar] [CrossRef]
- Speckmann, B.; Steinbrenner, H. Selenium and Selenoproteins in Inflammatory Bowel Diseases and Experimental Colitis. Inflamm. Bowel Dis. 2014, 20, 1110–1119. [Google Scholar] [CrossRef]
- Wang, Y.; Gao, X.; Pedram, P.; Shahidi, M.; Du, J.; Yi, Y.; Gulliver, W.; Zhang, H.; Sun, G. Significant Beneficial Association of High Dietary Selenium Intake with Reduced Body Fat in the CODING Study. Nutrients 2016, 8, 24. [Google Scholar] [CrossRef]
- Liu, K.; Zhao, Y.; Chen, F.; Gu, Z.; Bu, G. Enhanced Glutathione Peroxidases (GPx) Activity in Young Barley Seedlings Enriched with Selenium. Afr. J. Biotechnol. 2011, 10, 11482–11487. [Google Scholar] [CrossRef]
- Hrdina, J.; Banning, A.; Kipp, A.; Loh, G.; Blaut, M.; Brigelius-Flohé, R. The Gastrointestinal Microbiota Affects the Selenium Status and Selenoprotein Expression in Mice. J. Nutr. Biochem. 2009, 20, 638–648. [Google Scholar] [CrossRef]
- Zhai, Q.; Cen, S.; Li, P.; Tian, F.; Zhao, J.; Zhang, H.; Chen, W. Effects of Dietary Selenium Supplementation on Intestinal Barrier and Immune Responses Associated with Its Modulation of Gut Microbiota. Environ. Sci. Technol. Lett. 2018, 5, 724–730. [Google Scholar] [CrossRef]
- Kasaikina, M.V.; Kravtsova, M.A.; Cheon Lee, B.; Seravalli, J.; Peterson, D.A.; Walter, J.; Legge, R.; Benson, A.K.; Hatfield, D.L.; Gladyshev, V.N. Dietary Selenium Affects Host Selenoproteome Expression by Influencing the Gut Microbiota. FASEB J. 2011, 25, 2492–2499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ribière, C.; Peyret, P.; Parisot, N.; Darcha, C.; Déchelotte, P.J.; Barnich, N.; Peyretaillade, E.; Boucher, D. Oral Exposure to Environmental Pollutant Benzo[a]Pyrene Impacts the Intestinal Epithelium and Induces Gut Microbial Shifts in Murine Model. Sci. Rep. 2016, 6, 31027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saulnier, D.M.; Riehle, K.; Mistretta, T.; Diaz, M.; Mandal, D.; Raza, S.; Weidler, E.M.; Qin, X.; Coarfa, C.; Milosavljevic, A.; et al. Gastrointestinal Microbiome Signatures of Pediatric Patients With Irritable Bowel Syndrome. Gastroenterology 2011, 141, 1782–1791. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.; Jiang, L.-Q. Research Progress on the Immunomodulatory Effect of Trace Element Selenium and Its Effect on Immune-Related Diseases. Food Ther. Health Care 2020, 2, 86–98. [Google Scholar] [CrossRef]
- Martinez, S.S.; Huang, Y.; Acuna, L.; Laverde, E.; Trujillo, D.; Barbieri, M.A.; Tamargo, J.; Campa, A.; Baum, M.K. Role of Selenium in Viral Infections with a Major Focus on SARS-CoV-2. Int. J. Mol. Sci. 2021, 23, 280. [Google Scholar] [CrossRef]
- Lubos, E.; Kelly, N.J.; Oldebeken, S.R.; Leopold, J.A.; Zhang, Y.-Y.; Loscalzo, J.; Handy, D.E. Glutathione Peroxidase-1 Deficiency Augments Proinflammatory Cytokine-Induced Redox Signaling and Human Endothelial Cell Activation. J. Biol. Chem. 2011, 286, 35407–35417. [Google Scholar] [CrossRef] [Green Version]
- Guillin, O.M.; Vindry, C.; Ohlmann, T.; Chavatte, L. Selenium, Selenoproteins and Viral Infection. Nutrients 2019, 11, E2101. [Google Scholar] [CrossRef] [Green Version]
- Stone, C.A.; Kawai, K.; Kupka, R.; Fawzi, W.W. The Role of Selenium in HIV Infection Cosby A Stone, Kosuke Kawai, Roland Kupka, Wafaie W Fawzi Harvard School of Public Health. Nutr. Rev. 2010, 68, 671–681. [Google Scholar] [CrossRef] [Green Version]
- Khan, M.S.; Dilawar, S.; Ali, I.; Rauf, N. The Possible Role of Selenium Concentration in Hepatitis B and C Patients. Saudi J. Gastroenterol. 2012, 18, 106–110. [Google Scholar] [CrossRef]
- Kieliszek, M.; Lipinski, B. Selenium Supplementation in the Prevention of Coronavirus Infections (COVID-19). Med. Hypotheses 2020, 143, 109878. [Google Scholar] [CrossRef] [PubMed]
- Diwaker, D.; Mishra, K.P.; Ganju, L. Potential Roles of Protein Disulphide Isomerase in Viral Infections. Acta Virol. 2013, 57, 293–304. [Google Scholar] [PubMed]
- Zhang, J.; Taylor, E.W.; Bennett, K.; Saad, R.; Rayman, M.P. Association between Regional Selenium Status and Reported Outcome of COVID-19 Cases in China. Am. J. Clin. Nutr. 2020, 111, 1297–1299. [Google Scholar] [CrossRef] [PubMed]
- Moghaddam, A.; Heller, R.A.; Sun, Q.; Seelig, J.; Cherkezov, A.; Seibert, L.; Hackler, J.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Selenium Deficiency Is Associated with Mortality Risk from COVID-19. Nutrients 2020, 12, 2098. [Google Scholar] [CrossRef]
- Hirano, T.; Murakami, M. COVID-19: A New Virus, but a Familiar Receptor and Cytokine Release Syndrome. Immunity 2020, 52, 731–733. [Google Scholar] [CrossRef]
- Hiffler, L.; Rakotoambinina, B. Selenium and RNA Virus Interactions: Potential Implications for SARS-CoV-2 Infection (COVID-19). Front. Nutr. 2020, 7, 164. [Google Scholar] [CrossRef]
- Khoso, P.A.; Yang, Z.; Liu, C.; Li, S. Selenium Deficiency Downregulates Selenoproteins and Suppresses Immune Function in Chicken Thymus. Biol. Trace Elem. Res. 2015, 167, 48–55. [Google Scholar] [CrossRef]
- Zhang, Z.; Gao, X.; Cao, Y.; Jiang, H.; Wang, T.; Song, X.; Guo, M.; Zhang, N. Selenium Deficiency Facilitates Inflammation Through the Regulation of TLR4 and TLR4-Related Signaling Pathways in the Mice Uterus. Inflammation 2015, 38, 1347–1356. [Google Scholar] [CrossRef]
- Kaushal, N.; Kudva, A.K.; Patterson, A.D.; Chiaro, C.; Kennett, M.J.; Desai, D.; Amin, S.; Carlson, B.A.; Cantorna, M.T.; Prabhu, K.S. Crucial Role of Macrophage Selenoproteins in Experimental Colitis. J. Immunol. 2014, 193, 3683–3692. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Year | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | 2025 | 2026 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ireland | 494.97 | 510.65 | 519.51 | 531.83 | 554.24 | 584.79 | 585.71 | 591.82 | 617.89 | 646.61 | 679 |
| Eastern Europe | 4142 | 4727.30 | 4967.70 | 4999 | 4921 | 5211.80 | 5530.50 | 5745.60 | 5977.00 | 6234.30 | 6498.10 |
| Western Europe | 20,689.50 | 20,695.50 | 21,568.80 | 20,661.60 | 21,537.40 | 23,032.30 | 23,526.50 | 23,906.90 | 24,444.30 | 25,130.70 | 25,803.50 |
| USA | 31,902.50 | 31,708.50 | 31,007.50 | 30,956.90 | 32,053.90 | 31,512.30 | 32,940.60 | 34,148.30 | 35,239.50 | 36,210.90 | 37,164.30 |
| World | 159,040.10 | 164,365.30 | 168,157.20 | 168,477.90 | 168,919.00 | 177,395.00 | 184,464.70 | 192,846.20 | 201,417.00 | 201,355.60 | 219,467.80 |
| Country | Definition | Reference |
|---|---|---|
| EU | A product which is shown in a satisfactory manner that, in addition to adequate nutritional effects, induces beneficial effects on one or more target functions of the organism, significantly improving the health status and welfare or reducing the risk of disease. | [124] |
| USA | Foods that, by virtue of the presence of physiologically active components, provide a health benefit beyond basic nutrition | [125] |
| Canada | Similar in appearance to conventional food, consumed as part of the usual diet, with demonstrated physiological benefits, and/or to reduce the risk of chronic disease beyond basic nutritional functions | [126] |
| Japan | Known as Foods for Specified Health Use, these are foods composed of functional ingredients that affect the structure and/or function of the body and are used to maintain or regulate specific health conditions, such as gastrointestinal health, blood pressure, and blood cholesterol levels | [127] |
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| Virgin Coconut Oil | Antiviral |
| [171,173,193] |
| Immunomodulator |
| [178,180,181,182,193] | |
| Anti-inflammatory |
| [171,179] | |
| Extra Virgin Olive Oil | Antiviral |
| [194]. |
| Immunomodulator |
| [188,190,191,192] | |
| Anti-inflammatory |
| [189,190,192,195,196] |
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| Omega-3 PUFA e.g., EPA, DHA Omega-6 PUFA e.g., AA | Antiviral |
| [199,210] |
| Immunomodulator |
| [197,199,201,202,203,205,206,209,211,215] | |
| Anti-inflammatory |
| [3,199,201,203,214,215,216,217,218,219,220,224] |
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| 1,25-dihydroxyvitamin D and vitamin D receptor (1,25OHD or VDR) | Antiviral |
| [229], |
| Immunomodulator |
| [231,232,233,234,238] | |
| Anti-inflammatory |
| [229,231,236] |
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| Zn2+ | Antiviral |
| [243,245,251,252] |
| Immunomodulator |
| [239,246,247,249,254,258] | |
| Anti-inflammatory |
| [239,243,246,249,255] |
| Immune-Active Components | Immune-Boosting Functions | Mechanism | Reference |
|---|---|---|---|
| Selenite Selenoproteins | Antiviral |
| [262,272,274,275,276,277,278] |
| Immunomodulator |
| [266,267,268,271] | |
| Anti-inflammatory |
| [271,281,282,283,284,285] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Finnegan, D.; Tocmo, R.; Loscher, C. Targeted Application of Functional Foods as Immune Fitness Boosters in the Defense against Viral Infection. Nutrients 2023, 15, 3371. https://doi.org/10.3390/nu15153371
Finnegan D, Tocmo R, Loscher C. Targeted Application of Functional Foods as Immune Fitness Boosters in the Defense against Viral Infection. Nutrients. 2023; 15(15):3371. https://doi.org/10.3390/nu15153371
Chicago/Turabian StyleFinnegan, Dearbhla, Restituto Tocmo, and Christine Loscher. 2023. "Targeted Application of Functional Foods as Immune Fitness Boosters in the Defense against Viral Infection" Nutrients 15, no. 15: 3371. https://doi.org/10.3390/nu15153371
APA StyleFinnegan, D., Tocmo, R., & Loscher, C. (2023). Targeted Application of Functional Foods as Immune Fitness Boosters in the Defense against Viral Infection. Nutrients, 15(15), 3371. https://doi.org/10.3390/nu15153371






