Association of Dietary Sodium-to-Potassium Ratio with Cardiometabolic Risk Factors in Korean Adults: Findings from the Korean National Health and Nutrition Examination Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Collection of Demographic, Anthropometric, and Biochemical Information
2.3. Classification According to Dietary Na/K Ratio
2.4. Definitions of Cardiometabolic Risk Factors
2.5. Assessment of Dietary Factors
2.6. Statistical Analysis
3. Results
3.1. Dietary Sodium and Potassium Intakes and General Characteristics of Study Population
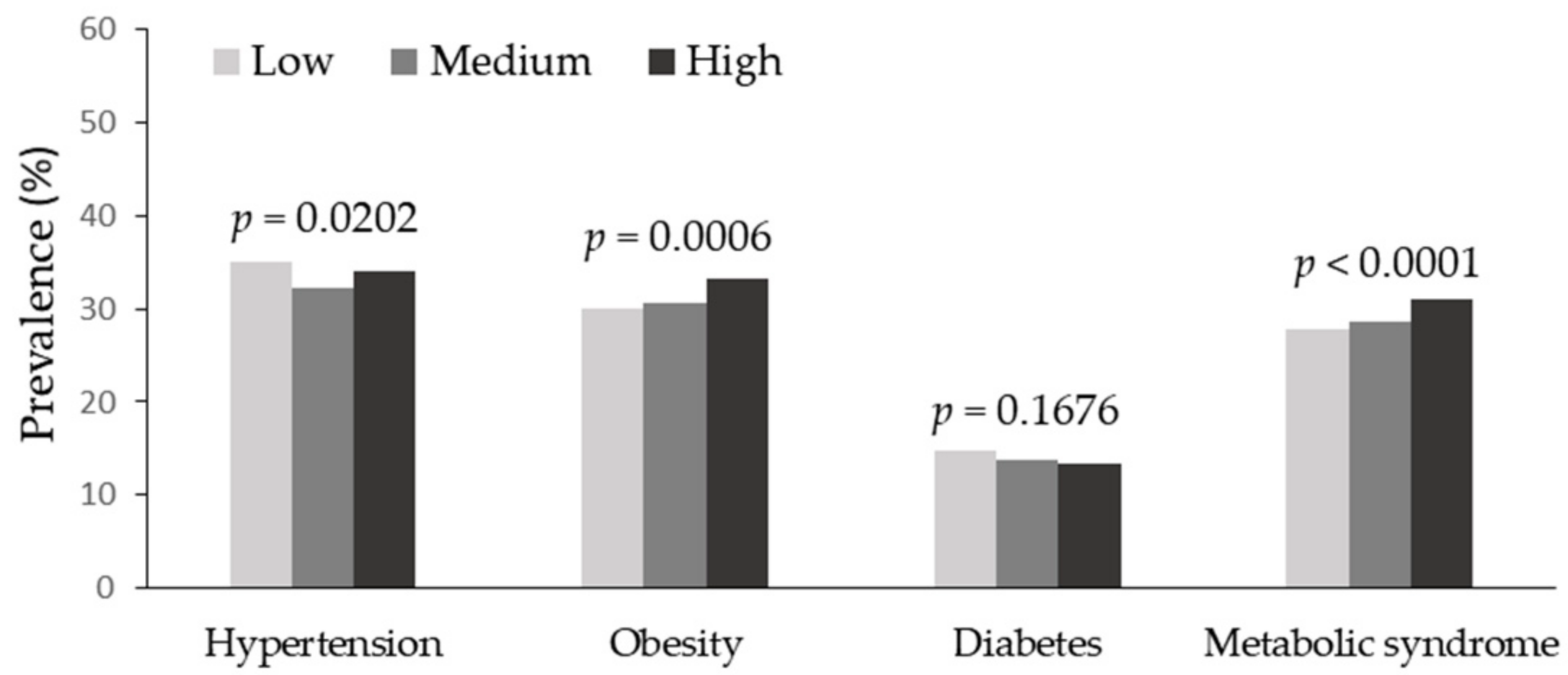
3.2. Distribution of Cardiometabolic Risk Factors and Biomarkers
3.3. Association of Dietary Na/K Ratio with Cardiometabolic Risk Factors
3.4. Association of Dietary Na/K Ratio with Intakes of Food Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 March 2023).
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas 2022 Reports. Available online: https://diabetesatlas.org/2022-reports/ (accessed on 28 March 2023).
- World Health Organization. Cardiovascular Diseases (CVDs). Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 20 March 2023).
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Mozumdar, A.; Liguori, G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care 2011, 34, 216–219. [Google Scholar] [CrossRef]
- Guembe, M.J.; Fernandez-Lazaro, C.I.; Sayon-Orea, C.; Toledo, E.; Moreno-Iribas, C.; RIVANA Study Investigators. Risk for cardiovascular disease associated with metabolic syndrome and its components: A 13-year prospective study in the RIVANA cohort. Cardiovasc. Diabetol. 2020, 19, 195. [Google Scholar] [CrossRef] [PubMed]
- James, M.; Varghese, T.P.; Sharma, R.; Chand, S. Association between metabolic syndrome and diabetes mellitus according to International Diabetic Federation and National Cholesterol Education Program Adult Treatment Panel III Criteria: A cross-sectional study. J. Diabetes Metab. Disord. 2020, 19, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Cook, N.R.; Cutler, J.A.; Obarzanek, E.; Buring, J.E.; Rexrode, K.M.; Kumanyika, S.K.; Appel, L.J.; Whelton, P.K. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: Observational follow-up of the trials of hypertension prevention (TOHP). BMJ 2007, 334, 885–888. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.L.; Cogswell, M.E.; Zhao, L.; Terry, A.L.; Wang, C.Y.; Wright, J.; Coleman King, S.M.; Bowman, B.; Chen, T.C.; Merritt, R.; et al. Association between urinary sodium and potassium excretion and blood pressure among adults in the United States: National Health and Nutrition Examination Survey, 2014. Circulation 2018, 137, 237–246. [Google Scholar] [CrossRef]
- Aburto, N.J.; Hanson, S.; Gutierrez, H.; Hooper, L.; Elliott, P.; Cappuccio, F.P. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ 2013, 346, f1378. [Google Scholar] [CrossRef]
- Perez, V.; Chang, E.T. Sodium-to-potassium ratio and blood pressure, hypertension, and related factors. Adv. Nutr. 2014, 5, 712–741. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Dietary Reference Intakes for Koreans; Ministry of Health and Welfare: Sejong, Republic of Korea, 2020. [Google Scholar]
- Tabara, Y.; Takahashi, Y.; Kumagai, K.; Setoh, K.; Kawaguchi, T.; Takahashi, M.; Muraoka, Y.; Tsujikawa, A.; Gotoh, N.; Terao, C.; et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: The Nagahama study. J. Hypertens. 2015, 33, 2407–2413. [Google Scholar] [CrossRef]
- Bhagavathula, A.S.; Refaat, S.A.; Bentley, B.L.; Rahmani, J. Association between intake of sodium, potassium, sodium-to-potassium ratio, and blood pressure among US adults. Int. J. Vitam. Nutr. Res. 2021. [Google Scholar] [CrossRef]
- Stamler, J.; Rose, G.; Stamler, R.; Elliott, P.; Dyer, A.; Marmot, M. INTERSALT study findings. Public health and medical care implications. Hypertension 1989, 14, 570–577. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases. In Report of a Joint WHO/FAO Expert Consultation; World Health Organization (WHO): Geneva, Switzerland, 2003. [Google Scholar]
- Nam, G.E.; Kim, S.M.; Choi, M.K.; Heo, Y.R.; Hyun, T.S.; Lyu, E.S.; Oh, S.Y.; Park, H.R.; Ro, H.K.; Han, K.; et al. Association between 24-h urinary sodium excretion and obesity in Korean adults: A multicenter study. Nutrition 2017, 41, 113–119. [Google Scholar] [CrossRef]
- Baudrand, R.; Campino, C.; Carvajal, C.A.; Olivieri, O.; Guidi, G.; Faccini, G.; Vöhringer, P.A.; Cerda, J.; Owen, G.; Kalergis, A.M.; et al. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin. Endocrinol. 2014, 80, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Ge, Z.; Guo, X.; Chen, X.; Tang, J.; Yan, L.; Ren, J.; Zhang, J.; Lu, Z.; Dong, J.; Xu, J.; et al. Association between 24 h urinary sodium and potassium excretion and the metabolic syndrome in Chinese adults: The Shandong and Ministry of Health Action on Salt and Hypertension (SMASH) study. Br. J. Nutr. 2015, 113, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Li, X.; Fan, W.; Yu, W.; Wang, S.; Li, Z.; Scott, E.M.; Li, X. Potassium and obesity/metabolic syndrome: A systematic review and meta-analysis of the epidemiological evidence. Nutrients 2016, 8, 183. [Google Scholar] [CrossRef]
- McLean, R.; Cameron, C.; Butcher, E.; Cook, N.R.; Woodward, M.; Campbell, N.R.C. Comparison of 24-hour urine and 24-hour diet recall for estimating dietary sodium intake in populations: A systematic review and meta-analysis. J. Clin. Hypertens. 2019, 21, 1753–1762. [Google Scholar] [CrossRef]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Lee, H.Y.; Shin, J.; Kim, G.H.; Park, S.; Ihm, S.H.; Kim, H.C.; Kim, K.I.; Kim, J.H.; Lee, J.H.; Park, J.M.; et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: Part II-diagnosis and treatment of hypertension. Clin. Hypertens. 2019, 25, 20. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for the Western Pacific. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000; Available online: https://apps.who.int/iris/handle/10665/206936 (accessed on 28 March 2023).
- Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2018: Korea National Health and Nutrition Survey (KNHANES VII-3); Ministry of Health and Welfare: Sejong, Republic of Korea, 2018. [Google Scholar]
- Lee, S.Y.; Park, H.S.; Kim, D.J.; Han, J.H.; Kim, S.M.; Cho, G.J.; Kim, D.Y.; Kwon, H.S.; Kim, S.R.; Lee, C.B.; et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res. Clin. Pract. 2007, 75, 72–80. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kang, M.S.; Kim, S.N.; Kim, J.B.; Cho, Y.S.; Park, H.J.; Kim, J.H. Food composition tables and national information network for food nutrition in Korea. Food Sci. Indusrty 2011, 44, 2–20. [Google Scholar] [CrossRef]
- Health Insurance Review & Assessment service (HIRA). 100 Disease Statistics in Living; HIRA: Wonju, Republic of Korea, 2018; Available online: https://www.hira.or.kr/ebooksc/ebook_472/ebook_472_201803281057049800.pdf (accessed on 30 June 2023).
- Hyun, T.; Choi, M.K.; Heo, Y.R.; Ro, H.; Han, Y.H.; Lee, Y.K. Comparison between 24-hour diet recall and 24-hour urine collection for estimating sodium and potassium intakes and their ratio among Korean adults. Nutr. Res. Pract. 2023, 17, 284–296. [Google Scholar] [CrossRef]
- Rhodes, D.G.; Murayi, T.; Clemens, J.C.; Baer, D.J.; Sebastian, R.S.; Moshfegh, A.J. The USDA Automated Multiple-Pass Method accurately assesses population sodium intakes. Am. J. Clin. Nutr. 2013, 97, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Zemel, M.B.; Sowers, J.R. Salt sensitivity and systemic hypertension in the elderly. Am. J. Cardiol. 1988, 61, 7H–12H. [Google Scholar] [CrossRef] [PubMed]
- Higo, Y.; Nagashima, S.; Tabara, Y.; Setoh, K.; Kawaguchi, T.; Takahashi, Y.; Kosugi, S.; Nakayama, T.; Matsuda, F.; Wakamura, T.; et al. Association of the spot urine sodium-to-potassium ratio with blood pressure is independent of urinary Na and K levels: The Nagahama study. Hypertens. Res. 2019, 42, 1624–1630. [Google Scholar] [CrossRef]
- Mulkerrin, E.C.; Brain, A.; Hampton, D.; Penney, M.D.; Sykes, D.A.; Williams, J.D.; Coles, G.A.; Woodhouse, K.W. Reduced renal hemodynamic response to atrial natriuretic peptide in elderly volunteers. Am. J. Kidney Dis. 1993, 22, 538–544. [Google Scholar] [CrossRef]
- He, F.J.; Marrero, N.M.; MacGregor, G.A. Salt intake is related to soft drink consumption in children and adolescents: A link to obesity? Hypertension 2008, 51, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Ge, Z.; Zhang, J.; Chen, X.; Yan, L.; Guo, X.; Lu, Z.; Xu, A.; Ma, J. Are 24 h urinary sodium excretion and sodium:potassium independently associated with obesity in Chinese adults? Public Health Nutr. 2016, 19, 1074–1080. [Google Scholar] [CrossRef]
- Jain, N.; Minhajuddin, A.T.; Neeland, I.J.; Elsayed, E.F.; Vega, G.L.; Hedayati, S.S. Association of urinary sodium-to-potassium ratio with obesity in a multiethnic cohort. Am. J. Clin. Nutr. 2014, 99, 992–998. [Google Scholar] [CrossRef]
- Ge, Z.; Zhang, J.; Chen, X.; Guo, X.; Yan, L.; Tang, J.; Cai, X.; Xu, J.; Hou, L.; Ma, J. Association between 24 h urinary sodium to potassium ratio and metabolic syndrome in Chinese adults. Zhonghua Liu Xing Bing Xue Za Zhi 2015, 36, 790–793. [Google Scholar]
- Oh, S.W.; Han, K.H.; Han, S.Y.; Koo, H.S.; Kim, S.; Chin, H.J. Association of sodium excretion with metabolic syndrome, insulin resistance, and body fat. Medicine 2015, 94, e1650. [Google Scholar] [CrossRef]
- Soltani, S.; Kolahdouz Mohammadi, R.; Shab-Bidar, S.; Vafa, M.; Salehi-Abargouei, A. Sodium status and the metabolic syndrome: A systematic review and meta-analysis of observational studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 196–206. [Google Scholar] [CrossRef]
- Buch, A.; Goldsmith, R.; Nitsan, L.; Margaliot, M.; Shefer, G.; Marcus, Y.; Stern, N. 24-h potassium excretion is associated with components of the metabolic syndrome: Results from a national survey based on urine collection in adults. Nutrients 2021, 13, 2689. [Google Scholar] [CrossRef] [PubMed]
- Tchernof, A.; Després, J.P. Pathophysiology of human visceral obesity: An update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef]
- Tian, Y.; Su, L.; Wang, J.; Duan, X.; Jiang, X. Fruit and vegetable consumption and risk of the metabolic syndrome: A meta-analysis. Public Health Nutr. 2018, 21, 756–765. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, J. Association between fruit and vegetable consumption and risk of hypertension in middle-aged and older Korean adults. J. Acad. Nutr. Diet. 2018, 118, 1438–1449.e5. [Google Scholar] [CrossRef]
- Lim, M.; Kim, J. Association between fruit and vegetable consumption and risk of metabolic syndrome determined using the Korean Genome and Epidemiology Study (KoGES). Eur. J. Nutr. 2020, 59, 1667–1678. [Google Scholar] [CrossRef]
- Institute of Medicine. DRI Dietary Reference Intakes: Applications in Dietary Assessment; The National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
| Total (n = 12,996) | Low (n = 4332) | Medium (n = 4332) | High (n = 4332) | p-Value | |
|---|---|---|---|---|---|
| Sodium (mg) | 3324 ± 2127 | 2039 ± 1124 c | 3239 ± 1473 b | 4694 ± 2569 a | <0.0001 |
| Potassium (mg) | 2867 ± 1413 | 3188 ± 1638 a | 2870 ± 1270 b | 2542 ± 1218 c | <0.0001 |
| Na/K (mmol/mmol) | 2.08 ± 0.10 | 1.11 ± 0.32 c | 1.92 ± 0.21 b | 3.21 ± 1.09 a | <0.0001 |
| Na/K ≤ 1.0 * (%) | 1476 (11.4) | 1476 (34.1) | 0 (0) | 0 (0) | <0.0001 |
| Characteristics | Low (n = 4332) | Medium (n = 4332) | High (n = 4332) | p-Value | |
|---|---|---|---|---|---|
| Sex | Men | 1365 (31.5) | 1894 (43.7) | 2155 (49.8) | <0.0001 |
| Age group (years) | 30–49 | 1234 (28.5) | 1796 (41.5) | 2024 (46.7) | |
| 50–64 | 1586 (36.6) | 1345 (31.0) | 1213 (28.0) | <0.0001 | |
| ≥65 | 1512 (34.9) | 1191 (27.5) | 1095 (25.3) | ||
| Body mass index (kg/m2) | 23.89 ± 3.31 b | 24.01 ± 3.37 b | 24.25 ± 3.60 a | <0.001 | |
| Household income | Lowest | 925 (21.4) | 784 (18.1) | 908 (21.0) | |
| Lower-middle | 1066 (24.6) | 1063 (24.5) | 1067 (24.6) | <0.0001 | |
| Upper-middle | 1084 (25.0) | 1201 (27.7) | 1214 (28.0) | ||
| Highest | 1257 (29.0) | 1284 (29.6) | 1143 (26.4) | ||
| Education | Middle school or less | 1702 (39.3) | 1407 (32.5) | 1412 (32.7) | |
| High school | 1234 (28.5) | 1211 (28.0) | 1309 (30.2) | <0.0001 | |
| College or above | 1396 (32.2) | 1714 (39.6) | 1611 (37.2) | ||
| Alcohol consumption | Yes | 2524 (58.4) | 1982 (45.8) | 1785 (41.3) | <0.0001 |
| Current smoking status | Yes | 443 (10.2) | 710 (16.4) | 969 (21.7) | <0.0001 |
| Physical activity | Yes | 1707 (39.5) | 1577 (36.5) | 1448 (33.5) | <0.0001 |
| Daily energy intake (kcal) | 1791 ± 791 c | 1966 ± 846 b | 2009 ± 928 a | <0.001 |
| Cardiometabolic Risk Biomarkers | Na/K Ratio Tertile | Total (n = 12,996) | Age 30–49 Years (n = 5054) | Age 50–64 Years (n = 4144) | Age ≥ 65 Years (n = 3798) |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | Low | 120.4 ± 17.1 | 111.2 ± 13.5 c | 120.5 ± 16.3 | 127.9 ± 17.1 |
| Medium | 119.7 ± 17.2 | 112.4 ± 13.5 b | 121.7 ± 16.3 | 128.7 ± 17.5 | |
| High | 119.9 ± 16.8 | 113.7 ± 13.6 a | 121.7 ± 16.3 | 129.6 ± 17.6 | |
| Correlation 1 | −0.013 | 0.075 *** | 0.026 | 0.042 * | |
| Diastolic blood pressure (mmHg) | Low | 74.9 ± 9.9 b | 75.0 ± 9.9 c | 77.3 ± 9.2 b | 72.1 ± 9.7 |
| Medium | 75.9 ± 10.2 a | 76.3 ± 10.4 b | 78.5 ± 9.6 a | 72.9 ± 10.1 | |
| High | 76.3 ± 10.5 a | 77.4 ± 10.6 a | 78.5 ± 9.9 a | 72.1 ± 10.0 | |
| Correlation | 0.054 *** | 0.087 *** | 0.049 ** | −0.007 | |
| Fasting blood glucose (mg/dL) | Low | 102.3 ± 23.8 | 95.7 ± 19.7 b | 102.6 ± 23.4 b | 107.2 ± 26.1 |
| Medium | 102.5 ± 25.2 | 96.7 ± 20.5 ab | 104.2 ± 24.7 ab | 108.9 ± 27.8 | |
| High | 103.0 ± 26.2 | 98.3 ± 21.7 a | 106.3 ± 30.2 a | 108.8 ± 28.1 | |
| Correlation | 0.010 | 0.038 ** | 0.059 *** | 0.022 | |
| Serum triglycerides (mg/dL) | Low | 129.8 ± 93.1 c | 125.1 ± 119.5 b | 130.5 ± 88.4 c | 131.9 ± 75.3 |
| Medium | 137.0 ± 111.1 b | 133.9 ± 122.4 b | 142.7 ± 106.2 b | 134.9 ± 77.5 | |
| High | 148.9 ± 128.2 a | 149.3 ± 128.9 a | 162.3 ± 149.9 a | 137.3 ± 97.6 | |
| Correlation | 0.070 *** | 0.084 *** | 0.095 *** | 0.024 | |
| Correlation | Low | 193.5 ± 37.9 | 194.8 ± 34.5 | 200.5 ± 38.5 | 186.4 ± 38.7 |
| Medium | 193.9 ± 38.8 | 195.8 ± 34.8 | 199.3 ± 38.8 | 184.0 ± 40.1 | |
| High | 193.5 ± 37.9 | 197.0 ± 34.8 | 197.9 ± 40.0 | 183.1 ± 40.9 | |
| Correlation | 0.001 | 0.032 * | −0.036 * | −0.023 | |
| Serum HDL cholesterol (mg/dL) | Low | 51.2 ± 12.7 a | 54.0 ± 13.2 a | 51.9 ± 12.5 a | 48.8 ± 11.5 a |
| Medium | 50.8 ± 12.8 ab | 52.3 ± 12.7 b | 50.9 ± 13.2 ab | 47.5 ± 12.1 b | |
| High | 50.3 ± 12.5 b | 51.8 ± 12.7 b | 50.0 ± 12.5 b | 47.9 ± 11.9 ab | |
| Correlation | −0.029 ** | −0.068 *** | −0.054 *** | −0.017 | |
| Serum LDL cholesterol (mg/dL) | Low | 116.5 ± 34.4 | 117.6 ± 33.5 | 121.4 ± 32.8 a | 107.2 ± 35.0 |
| Medium | 117.0 ± 36.5 | 122.2 ± 34.2 | 117.9 ± 35.6 ab | 110.3 ± 38.5 | |
| High | 115.9 ± 37.2 | 123.6 ± 34.5 | 111.0 ± 38.1 b | 109.0 ± 39.3 | |
| Correlation | −0.007 | 0.041 | −0.117 ** | −0.015 | |
| Waist circumference (cm) | Low | 82.1 ± 9.6 c | 79.3 ± 10.3 c | 81.9 ± 9.0 c | 84.9 ± 9.0 b |
| Medium | 82.9 ± 9.8 b | 81.0 ± 10.4 b | 83.1 ± 8.8 b | 85.7 ± 8.8 a | |
| High | 83.7 ± 10.1 a | 82.7 ± 10.7 a | 84.2 ± 9.4 a | 85.6 ± 9.1 a | |
| Correlation | 0.066 *** | 0.126 *** | 0.100 *** | 0.042 ** |
| Risk Factors | Na/K Ratio Tertile | Total (n = 12,996) | Age 30–49 Years (n = 5054) | Age 50–64 Years (n = 4144) | Age ≥ 65 Years (n = 3798) |
|---|---|---|---|---|---|
| Hypertension | Low | Reference | Reference | Reference | Reference |
| Medium | 0.99 (0.85–1.14) | 0.71 (0.46–1.09) | 0.99 (0.78–1.24) | 1.17 (0.95–1.44) | |
| High | 1.07 (0.92–1.24) | 0.80 (0.53–1.19) | 0.98 (0.78–1.24) | 1.38 (1.10–1.72) | |
| p for trend | 0.5370 | 0.3563 | 0.9849 | 0.0159 | |
| Obesity | Low | Reference | Reference | Reference | Reference |
| Medium | 0.98 (0.89–1.09) | 0.99 (0.82–1.19) | 1.00 (0.84–1.19) | 1.07 (0.88–1.29) | |
| High | 1.05 (0.94–1.17) | 1.10 (0.92–1.33) | 0.99 (0.82–1.21) | 1.09 (0.91–1.32) | |
| p for trend | 0.4183 | 0.3373 | 0.9987 | 0.6199 | |
| Diabetes | Low | Reference | Reference | Reference | Reference |
| Medium | 1.04 (0.91–1.20) | 0.98 (0.63–1.51) | 1.09 (0.85–1.39) | 1.06 (0.88–1.27) | |
| High | 1.07 (0.92–1.24) | 1.05 (0.68–1.60) | 1.21 (0.93–1.57) | 0.94 (0.76–1.16) | |
| p for trend | 0.5800 | 0.8907 | 0.3654 | 0.5702 | |
| Metabolic syndrome | Low | Reference | Reference | Reference | Reference |
| Medium | 1.05 (0.93–1.18) | 1.05 (0.85–1.30) | 0.96 (0.79–1.16) | 1.31 (1.09–1.56) | |
| High | 1.22 (1.08–1.38) | 1.29 (1.05–1.60) | 1.13 (0.93–1.38) | 1.28 (1.06–1.54) | |
| p for trend | 0.0020 | 0.0211 | 0.2729 | 0.0044 | |
| Components of metabolic syndrome | |||||
| Abdominal obesity | Low | Reference | Reference | Reference | Reference |
| Medium | 1.02 (0.92–1.14) | 1.05 (0.86–1.29) | 0.93 (0.77–1.12) | 1.24 (1.03–1.50) | |
| High | 1.16 (1.03–1.30) | 1.25 (1.02–1.53) | 1.05 (0.86–1.28) | 1.20 (0.99–1.45) | |
| p for trend | 0.0238 | 0.0383 | 0.4648 | 0.0560 | |
| Elevated triglyceride | Low | Reference | Reference | Reference | Reference |
| Medium | 0.99 (0.89–1.11) | 1.02 (0.83–1.26) | 0.98 (0.81–1.18) | 1.11 (0.93–1.34) | |
| High | 1.20 (1.07–1.34) | 1.30 (1.06–1.58) | 1.26 (1.03–1.53) | 0.99 (0.81–1.21) | |
| p for trend | 0.0008 | 0.0041 | 0.0253 | 0.4233 | |
| Reduced HDL cholesterol | Low | Reference | Reference | Reference | Reference |
| Medium | 0.96 (0.86–1.07) | 0.91 (0.76–1.09) | 0.91 (0.75–1.09) | 1.17 (0.98–1.40) | |
| High | 0.99 (0.88–1.10) | 0.97 (0.81–1.16) | 0.98 (0.81–1.19) | 1.01 (0.83–1.21) | |
| p for trend | 0.6952 | 0.5254 | 0.5211 | 0.1672 | |
| Elevated blood pressure | Low | Reference | Reference | Reference | Reference |
| Medium | 1.12 (1.01–1.25) | 1.24 (1.00–1.55) | 1.04 (0.86–1.27) | 1.24 (1.04–1.48) | |
| High | 1.12 (1.01–1.25) | 1.25 (1.02–1.53) | 0.97 (0.80–1.17) | 1.27 (1.04–1.55) | |
| p for trend | 0.0430 | 0.0546 | 0.7791 | 0.0190 | |
| Elevated fasting blood glucose | Low | Reference | Reference | Reference | Reference |
| Medium | 1.02 (0.91–1.14) | 0.94 (0.77–1.15) | 1.12 (0.93–1.35) | 1.04 (0.87–1.24) | |
| High | 1.10 (0.99–1.23) | 1.07 (0.87–1.31) | 1.16 (0.96–1.40) | 1.09 (0.91–1.32) | |
| p for trend | 0.1593 | 0.3631 | 0.2938 | 0.6383 | |
| Intakes by Food Groups (g/Day) | Low (n = 4332) | Medium (n = 4332) | High (n = 4332) | p for Trend |
|---|---|---|---|---|
| Cereal + grains | 238.5 ± 3.1 | 282.0 ± 2.8 | 305.2 ± 3.2 | 0.0001 |
| Whole grain + rice cakes | 201.1 ± 2.6 | 215.2 ± 2.5 | 201.7 ± 2.6 | 0.3725 |
| Breads + cookies | 23.1 ± 1.4 | 27.3 ± 1.2 | 29.6 ± 1.2 | 0.0346 |
| Breakfast cereals | 0.6 ± 0.1 | 0.8 ± 0.1 | 0.4 ± 0.1 | 0.0263 |
| Noodles | 12.3 ± 0.8 | 34.9 ± 1.6 | 62.5 ± 2.2 | 0.0001 |
| Potato + potato products | 65.6 ± 3.3 | 30.2 ± 1.2 | 18.1 ± 0.7 | 0.0001 |
| Sugar | 6.8 ± 0.3 | 7.7 ± 0.3 | 7.9 ± 0.3 | 0.3916 |
| Beans | 38.8 ± 1.4 | 40.2 ± 1.4 | 34.5 ± 1.4 | 0.0651 |
| Nuts | 10.0 ± 0.7 | 7.0 ± 0.4 | 6.1 ± 0.5 | 0.0003 |
| Vegetable | 302.8 ± 4.6 | 330.1 ± 3.8 | 332.9 ± 4.0 | 0.0021 |
| Salted vegetable | 80.5 ± 1.6 | 124.8 ± 2.0 | 148.4 ± 2.4 | 0.0001 |
| Unsalted vegetable | 222.3 ± 4.2 | 205.2 ± 3.1 | 184.5 ± 2.9 | 0.0001 |
| Mushroom | 6.3 ± 0.4 | 6.8 ± 0.4 | 5.8 ± 0.4 | 0.1454 |
| Fruits | 320.7 ± 7.1 | 184.9 ± 4.6 | 107.2 ± 3.5 | 0.0001 |
| Meat + meat dishes | 80.1 ± 2.4 | 118.6 ± 3.0 | 123.6 ± 3.6 | 0.0005 |
| Non-marinated meat | 53.5 ± 1.8 | 76.6 ± 2.1 | 74.0 ± 2.2 | 0.3047 |
| Meat dishes | 22.5 ± 1.4 | 33.5 ± 2.1 | 37.3 ± 2.5 | 0.0136 |
| Cured and processed meat | 2.9 ± 1.4 | 5.9 ± 0.4 | 7.1 ± 0.5 | 0.0001 |
| Eggs | 25.3 ± 0.8 | 28.1 ± 0.8 | 31.8 ± 1.1 | 0.0001 |
| Fish | 82.8 ± 2.4 | 120.0 ± 3.5 | 134.8 ± 3.6 | 0.0001 |
| Seaweed | 29.9 ± 1.8 | 33.4 ± 2.1 | 27.8 ± 1.6 | 0.7608 |
| Dairy | 107.3 ± 3.3 | 81.7 ± 2.9 | 52.1 ± 2.1 | 0.0001 |
| Milk | 71.1 ± 2.7 | 54.6 ± 2.4 | 32.4 ± 1.7 | 0.0001 |
| Yogurt | 26.4 ± 1.5 | 17.2 ± 1.2 | 10.9 ± 0.8 | 0.0001 |
| Oils | 4.9 ± 0.2 | 6.6 ± 0.2 | 7.4 ± 0.2 | 0.0001 |
| Beverage | 252.2 ± 8.6 | 327.6 ± 9.1 | 347.1 ± 9.6 | 0.4729 |
| Seasoning | 24.3 ± 0.5 | 35.5 ± 0.6 | 44.8 ± 0.8 | 0.0001 |
| Processed food | 8.7 ± 0.8 | 15.2 ± 1.1 | 22.6 ± 1.4 | 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baek, S.-Y.; Kim, H.-K. Association of Dietary Sodium-to-Potassium Ratio with Cardiometabolic Risk Factors in Korean Adults: Findings from the Korean National Health and Nutrition Examination Survey. Nutrients 2023, 15, 3134. https://doi.org/10.3390/nu15143134
Baek S-Y, Kim H-K. Association of Dietary Sodium-to-Potassium Ratio with Cardiometabolic Risk Factors in Korean Adults: Findings from the Korean National Health and Nutrition Examination Survey. Nutrients. 2023; 15(14):3134. https://doi.org/10.3390/nu15143134
Chicago/Turabian StyleBaek, Seo-Young, and Hye-Kyeong Kim. 2023. "Association of Dietary Sodium-to-Potassium Ratio with Cardiometabolic Risk Factors in Korean Adults: Findings from the Korean National Health and Nutrition Examination Survey" Nutrients 15, no. 14: 3134. https://doi.org/10.3390/nu15143134
APA StyleBaek, S.-Y., & Kim, H.-K. (2023). Association of Dietary Sodium-to-Potassium Ratio with Cardiometabolic Risk Factors in Korean Adults: Findings from the Korean National Health and Nutrition Examination Survey. Nutrients, 15(14), 3134. https://doi.org/10.3390/nu15143134





