Prevalence of Vitamin B12 and Folate Deficiencies in Indian Children and Adolescents
Abstract
1. Introduction
2. Methodology
2.1. CNNS Survey, Serum B12 and Erythrocyte FA Analysis
2.2. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
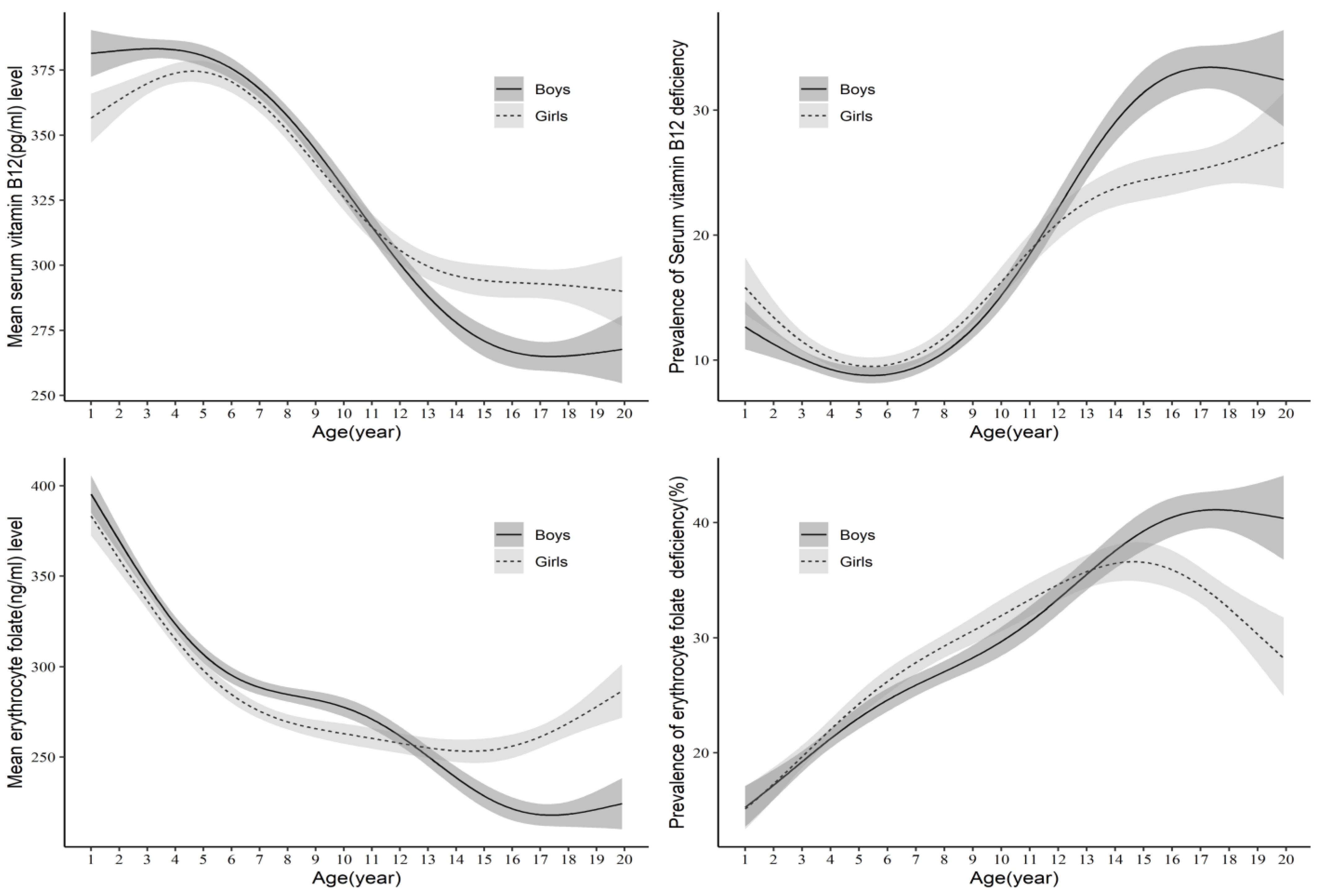
3.2. Serum B12 and Erythrocyte FA Concentration and Prevalence of B12 and FA Deficiency by Age and Sex
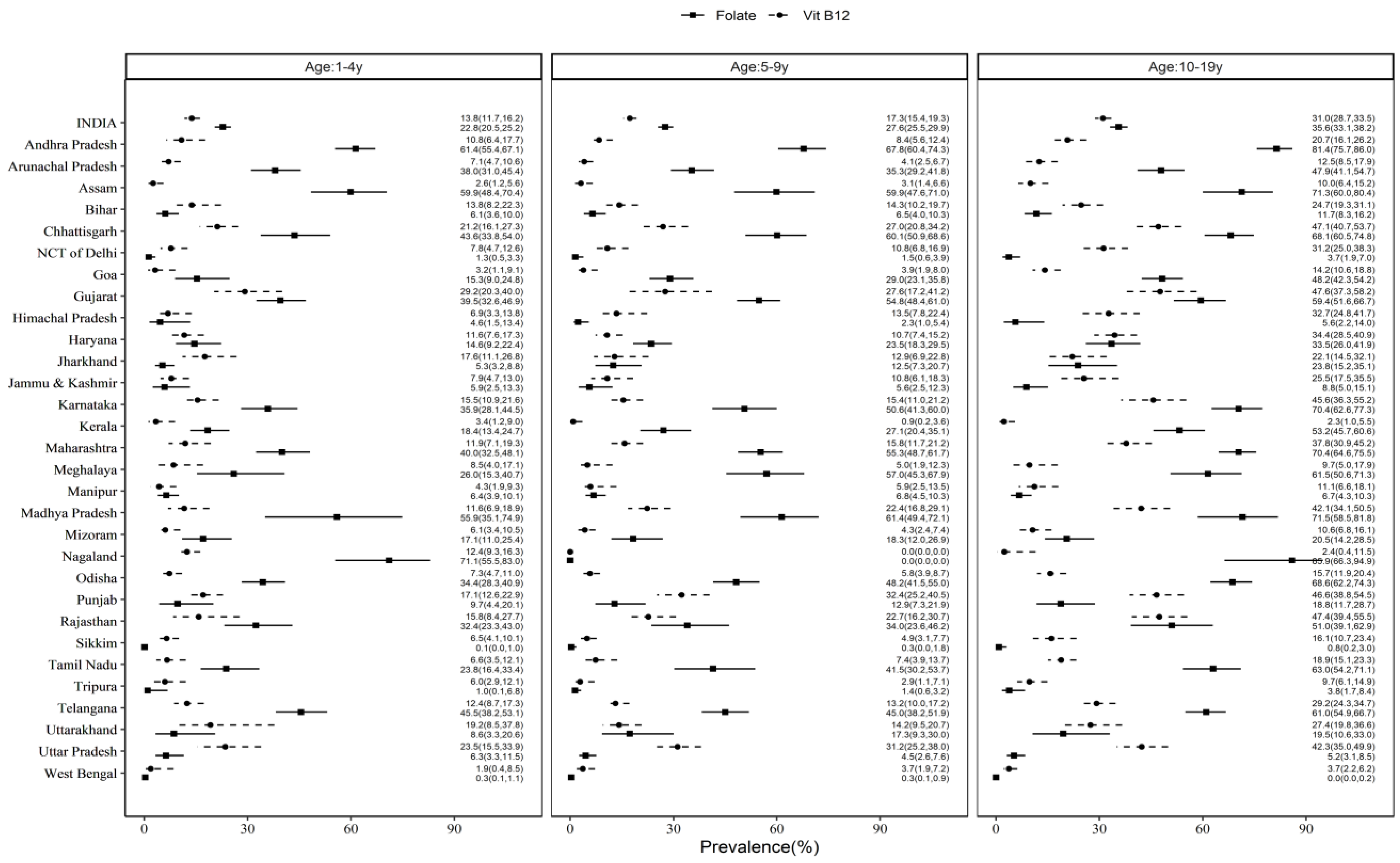
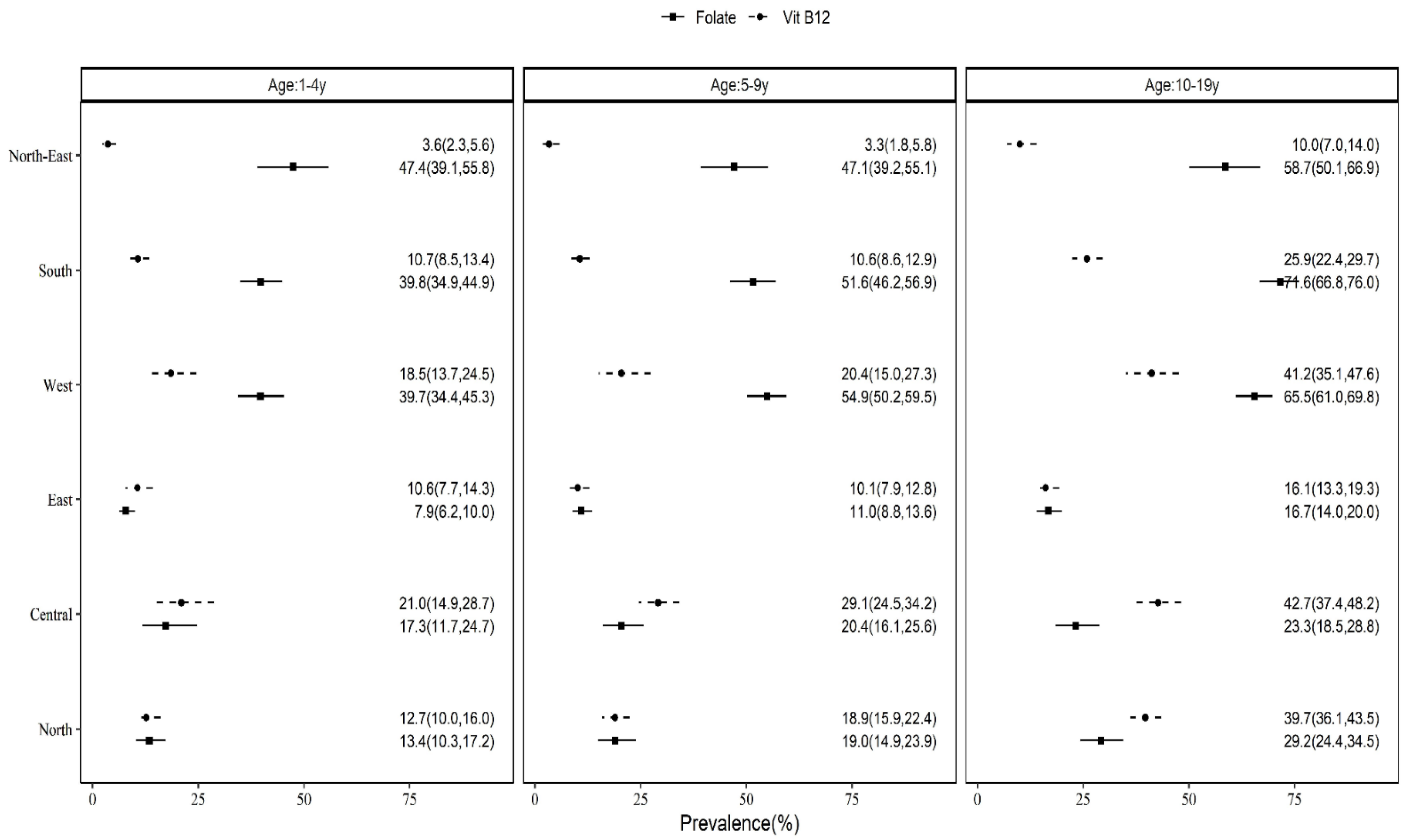
3.3. State-Based, Rural–Urban and Regional Differences in Prevalence of B12 and FA Deficiency
3.4. B12 and FA Deficiency by Sociodemographics, WASH Characteristics, Undernutrition and Morbidity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Lyon, P.; Strippoli, V.; Fang, B.; Cimmino, L. B Vitamins and One-Carbon Metabolism: Implications in Human Health and Disease. Nutrients 2020, 12, 2867. [Google Scholar] [CrossRef] [PubMed]
- Stover, P.J. Physiology of folate and vitamin B12 in health and disease. Nutr. Rev. 2004, 62 Pt 2, S3–S12; discussion S13. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.H.; Miller, J.W.; Groot, L.D.; Rosenberg, I.H.; Smith, A.D.; Refsum, H.; Raiten, D.J. Biomarkers of Nutrition for Development (BOND): Vitamin B-12 Review. J. Nutr. 2018, 148 (Suppl. S4), 1995S–2027S. [Google Scholar] [CrossRef] [PubMed]
- Bailey, L.B.; Stover, P.J.; McNulty, H.; Fenech, M.F.; Gregory, J.F., III; Mills, J.L.; Pfeiffer, C.M.; Fazili, Z.; Zhang, M.; Ueland, P.M.; et al. Biomarkers of Nutrition for Development-Folate Review. J. Nutr. 2015, 145, 1636S–1680S. [Google Scholar] [CrossRef]
- Dwarkanath, P.; Barzilay, J.R.; Thomas, T.; Thomas, A.; Bhat, S.; Kurpad, A.V. High folate and low vitamin B-12 intakes during pregnancy are associated with small-for-gestational age infants in South Indian women: A prospective observational cohort study. Am. J. Clin. Nutr. 2013, 98, 1450–1458. [Google Scholar] [CrossRef]
- Puri, M.; Kaur, L.; Walia, G.K.; Mukhopadhhyay, R.; Sachdeva, M.P.; Trivedi, S.S.; Ghosh, P.K.; Saraswathy, K.N. MTHFR C677T polymorphism, folate, vitamin B12 and homocysteine in recurrent pregnancy losses: A case control study among North Indian women. J. Perinat. Med. 2013, 41, 549–554. [Google Scholar] [CrossRef]
- Wong, E.; Molina-Cruz, R.; Rose, C.; Bailey, L.; Kauwell, G.P.A.; Rosenthal, J. Prevalence and Disparities in Folate and Vitamin B12 Deficiency Among Preschool Children in Guatemala. Matern. Child Health J. 2022, 26, 156–167. [Google Scholar] [CrossRef]
- Veena, S.R.; Krishnaveni, G.V.; Srinivasan, K.; Wills, A.K.; Muthayya, S.; Kurpad, A.V.; Yajnik, C.S.; Fall, C.H.D. Higher maternal plasma folate but not vitamin B-12 concentrations during pregnancy are associated with better cognitive function scores in 9- to 10- year-old children in South India. J. Nutr. 2010, 140, 1014–1022. [Google Scholar] [CrossRef]
- Sachdev, H.S.; Porwal, A.; Sarna, A.; Acharya, R.; Ramesh, S.; Kapil, U.; Kurpad, A.V. Intraindividual double-burden of anthropometric undernutrition and metabolic obesity in Indian children: A paradox that needs action. Eur. J. Clin. Nutr. 2021, 75, 1205–1217. [Google Scholar] [CrossRef]
- Gadgil, M.; Joshi, K.; Pandit, A.; Otiv, S.; Joshi, R.; Brenna, J.T.; Patwardhan, B. Imbalance of folic acid and vitamin B12 is associated with birth outcome: An Indian pregnant women study. Eur. J. Clin. Nutr. 2014, 68, 726–729. [Google Scholar] [CrossRef]
- Sivaprasad, M.; Shalini, T.; Balakrishna, N.; Sudarshan, M.; Lopamudra, P.; Suryanarayana, P.; Arlappa, N.; Ravikumar, B.P.; Radhika, M.S.; Reddy, G.B. Status of Vitamin B12 and Folate among the Urban Adult Population in South India. Ann. Nutr. Metab. 2016, 68, 94–102. [Google Scholar] [CrossRef]
- Sivaprasad, M.; Shalini, T.; Reddy, P.Y.; Seshacharyulu, M.; Madhavi, G.; Kumar, B.N.; Reddy, G.B. Prevalence of vitamin deficiencies in an apparently healthy urban adult population: Assessed by subclinical status and dietary intakes. Nutrition 2019, 63–64, 106–113. [Google Scholar] [CrossRef]
- Yajnik, C.S.; Deshpande, S.S.; Jackson, A.A.; Refsum, H.; Rao, S.; Fisher, D.J.; Bhat, D.S.; Naik, S.S.; Coyaji, K.J.; Joglekar, C.V.; et al. Vitamin B12 and folate concentrations during pregnancy and insulin resistance in the offspring: The Pune Maternal Nutrition Study. Diabetologia 2008, 51, 29–38. [Google Scholar] [CrossRef]
- Strand, T.A.; Taneja, S.; Ueland, P.M.; Refsum, H.; Bahl, R.; Schneede, J.; Sommerfelt, H.; Bhandari, N. Cobalamin and folate status predicts mental development scores in North Indian children 12-18 mo of age. Am. J. Clin. Nutr. 2013, 97, 310–317. [Google Scholar] [CrossRef]
- Kapil, U.; Sareen, N. Prevalence of ferritin, folate and vitamin B12 deficiencies amongst children in 5–18 years of age in Delhi. Indian J. Pediatr. 2014, 8, 312. [Google Scholar] [CrossRef]
- Shalini, T.; Sivaprasad, M.; Balakrishna, N.; Madhavi, G.; Radhika, M.S.; Boiroju, N.K.; Pullakhandam, R.; Reddy, G.B. Micronutrient intakes and status assessed by probability approach among the urban adult population of Hyderabad city in South India. Eur. J. Nutr. 2019, 58, 3147–3159. [Google Scholar] [CrossRef]
- Chakraborty, S.; Chopra, M.; Mani, K.; Giri, A.K.; Banerjee, P.; Sahni, N.S.; Siddhu, A.; Tandon, N.; Bharadwaj, D. Prevalence of vitamin B12 deficiency in healthy Indian school-going adolescents from rural and urban localities and its relationship with various anthropometric indices: A cross-sectional study. J. Hum. Nutr. Diet. 2018, 31, 513–522. [Google Scholar] [CrossRef]
- Comprehensive National Nutrition Survey (CNNS). National Report, Ministry of Health and Family Welfare (MoHFW); Government of India: New Delhi, India, 2019.
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4) 2015–2016; IIPS: Mumbai, India, 2017. [Google Scholar]
- World Health Organization (WHO)/United Nations International Children’s Emergency Fund (UNICEF). Joint Monitoring Programme (JMP) for Water Supply, Sanitation and Hygiene, JMP Methodology. Update & SDG Baselines. 2018. Available online: https://washdata.org/sites/default/files/documents/reports/2018-04/JMP-2017-update-methodology.pdf (accessed on 3 March 2021).
- World Health Organization (WHO). World Health Organization Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Sachdev, H.S.; Porwal, A.; Acharya, R.; Ashraf, S.; Ramesh, S.; Khan, N.; Kapil, U.; Kurpad, A.V.; Sarna, A. Haemoglobin thresholds to define anaemia in a national sample of healthy children and adolescents aged 1–19 years in India: A population-based study. Lancet. Glob. Health 2021, 9, e822–e831. [Google Scholar] [CrossRef]
- de Benoist, B. Conclusions of a WHO Technical Consultation on folate and vitamin B12 deficiencies. Food. Nutr. Bull. 2008, 29 (Suppl. 2), S238–S244. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; WHO: Geneva, Switzerland, 2011; Available online: https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf?ua=1 (accessed on 3 March 2021).
- Young, M.F.; Guo, J.; Williams, A.; Whitfield, K.C.; Nasrin, S.; Kancherla, V.; Suchdev, P.S.; Crider, K.S.; Pfeiffer, C.M.; Serdula, M. Interpretation of vitamin B-12 and folate concentrations in population-based surveys does not require adjustment for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am. J. Clin. Nutr. 2020, 111, 919–926. [Google Scholar] [CrossRef]
- Ulak, M.; Chandyo, R.K.; Adhikari, R.K.; Sharma, P.R.; Sommerfelt, H.; Refsum, H.; Strand, T.A. Cobalamin and folate status in 6 to 35 months old children presenting with acute diarrhea in Bhaktapur, Nepal. PLoS ONE 2014, 9, e90079. [Google Scholar] [CrossRef]
- Shahab-Ferdows, S.; Engle-Stone, R.; Hampel, D.; Ndjebayi, A.O.; Nankap, M.; Brown, K.H.; Allen, L.H. Regional, Socioeconomic, and Dietary Risk Factors for Vitamin B-12 Deficiency Differ from Those for Folate Deficiency in Cameroonian Women and Children. J. Nutr. 2015, 145, 2587–2595. [Google Scholar] [CrossRef] [PubMed]
- Ng’eno, B.N.; Perrine, C.G.; Whitehead, R.D.; Subedi, G.R.; Mebrahtu, S.; Dahal, P.; Jefferds, M.E.D. High Prevalence of Vitamin B12 Deficiency and No Folate Deficiency in Young Children in Nepal. Nutrients 2017, 9, 72. [Google Scholar] [CrossRef] [PubMed]
- Awasthi, S.; Kumar, D.; Mahdi, A.A.; Agarwal, G.G.; Pandey, A.K.; Parveen, H.; Singh, S.; Awasthi, R.; Pande, H.; Anish, T.S.; et al. Prevalence of specific micronutrient deficiencies in urban school going children and adolescence of India: A multicenter cross-sectional study. PLoS ONE 2022, 17, e0267003. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Nasu, L.; Mundo-Rosas, V.; Shamah-Levy, T.; Méndez-Gómez Humaran, I.; Avila-Arcos, M.A.; Rebollar-Campos, M.R.; Villalpando, S. Prevalence of folate and vitamin B12 deficiency in Mexican children aged 1 to 6 years in a population-based survey. Salud. Publica Mex. 2012, 54, 116–124. [Google Scholar] [CrossRef]
- Garcia-Casal, M.N.; Osorio, C.; Landaeta, M.; Leets, I.; Matus, P.; Fazzino, F.; Marcos, E. High prevalence of folic acid and vitamin B12 deficiencies in infants, children, adolescents and pregnant women in Venezuela. Eur. J. Clin. Nutr. 2005, 59, 1064–1070. [Google Scholar] [CrossRef]
- McLean, E.; de Benoist, B.; Allen, L.H. Review of the magnitude of folate and vitamin B12 deficiencies worldwide. Food Nutr. Bull. 2008, 29 (Suppl. S2), S38–S51. [Google Scholar] [CrossRef]
- Siekmann, J.H.; Allen, L.H.; Bwibo, N.O.; Demment, M.W.; Murphy, S.P.; Neumann, C.G. Kenyan school children have multiple micronutrient deficiencies, but increased plasma vitamin B-12 is the only detectable micronutrient response to meat or milk supplementation. J. Nutr. 2003, 133 (Suppl. S2), 3972S–3980S. [Google Scholar] [CrossRef]
- Herrmann, W.; Obeid, R. Causes and early diagnosis of vitamin B12 deficiency. Dtsch. Arztebl. Int. 2008, 105, 680–685. [Google Scholar] [CrossRef]
- Hvas, A.M.; Nexo, E. Holotranscobalamin—A first choice assay for diagnosing early vitamin B deficiency? J. Intern. Med. 2005, 257, 289–298. [Google Scholar] [CrossRef]
- Nexo, E.; Hoffmann-Lucke, E. Holotranscobalamin, a marker of vitamin B-12 status: Analytical aspects and clinical utility. Am. J. Clin. Nutr. 2011, 94, 359S–365S. [Google Scholar] [CrossRef]
- Green, R.; Allen, L.H.; Bjørke-Monsen, A.L.; Brito, A.; Guéant, J.L.; Miller, J.W.; Molloy, A.M.; Nexo, E.; Stabler, S.; Toh, B.H.; et al. Vitamin B12 deficiency. Nat. Rev. Dis. Primers 2017, 3, 17040. [Google Scholar] [CrossRef]
- Bawaskar, H.S.; Bawaksar, P.H. Profile of Vitamin B12 and Vitamin D in Rural School children in Raigad, India. Indian Pediatr. 2020, 57, 871. [Google Scholar] [CrossRef]
- Sarna, A.; Porwal, A.; Ramesh, S.; Agrawal, P.K.; Acharya, R.; Johnston, R.; Khan, N.; Sachdev, H.P.S.; Madhavan Nair, K.; Ramakrishnan, L.; et al. Characterisation of the types of anaemia prevalent among children and adolescents aged 1-19 years in India: A population-based study. Lancet Child Adolesc. Health 2020, 4, 515–525. [Google Scholar] [CrossRef]
- Scott, S.; Lahiri, A.; Sethi, V.; de Wagt, A.; Menon, P.; Yadav, K.; Varghese, M.; Joe, W.; Vir, S.C.; Nguyen, P.H. Anaemia in Indians aged 10-19 years: Prevalence, burden and associated factors at national and regional levels. Matern. Child Nutr. 2022, 18, e13391. [Google Scholar] [CrossRef]
- Oussalah, A.; Levy, J.; Berthezène, C.; Alpers, D.H.; Guéant, J.L. Health outcomes associated with vegetarian diets: An umbrella review of systematic reviews and meta-analyses. Clin. Nutr. 2020, 39, 3283–3307. [Google Scholar] [CrossRef]
- Villamor, E.; Mora-Plazas, M.; Forero, Y.; Lopez-Arana, S.; Baylin, A. Vitamin B-12 status is associated with socioeconomic level and adherence to an animal food dietary pattern in Colombian school children. J. Nutr. 2008, 138, 1391–1398. [Google Scholar] [CrossRef]
- Ganpule-Rao, A.V.; Bhat, D.; Yajnik, C.S.; Rush, E. Dietary diversity scores, nutrient intakes and biomarkers vitamin B12, folate and Hb in rural youth from the Pune Maternal Nutrition Study. Br. J. Nutr. 2021, 126, 236–243. [Google Scholar] [CrossRef]

| Characteristics | 1–4 Years | 5–9 Years | 10–19 Years | ||||
|---|---|---|---|---|---|---|---|
| Vitamin B12 (n = 9976) % (95% CI) | Folate (n = 11,004) % (95% CI) | Vitamin B12 (n = 12,156) % (95% CI) | Folate (n = 14,125) % (95% CI) | Vitamin B12 (n = 11,748) % (95% CI) | Folate (n = 13,621) % (95% CI) | ||
| Age in years | Mean (95% CI) | 2.78 (2.74–2.83) | 2.78 (2.74–2.83) | 7.02 (6.97–7.06) | 7.02 (6.98–7.07) | 14.3 (14.2–14.4) | 14.3 (14.2–14.4) |
| Sex | Boys | 52.9 (50.3–55.4) | 52.5 (50.0–55.0) | 51.6 (49.8–53.3) | 51.2 (49.4–52.9) | 50.6 (48.6–52.5) | 50.6 (48.8–52.4) |
| Girls | 47.1 (44.6–49.7) | 47.5 (45.0–50.0) | 48.4 (46.7–50.2) | 48.8 (47.1–50.6) | 49.4 (47.5–51.4) | 49.4 (47.6–51.2) | |
| Residence | Urban | 24.9 (21.7–28.4) | 25.7 (22.5–29.1) | 23.6 (20.7–26.8) | 25.1 (22.1–28.2) | 25.2 (22.1–28.6) | 25.7 (22.6–29.0) |
| Rural | 75.1 (71.6–78.3) | 74.3 (70.9–77.5) | 76.4 (73.2–79.3) | 74.9 (71.8–77.9) | 74.8 (71.4–77.9) | 74.3 (71.0–77.4) | |
| Wealth Index | Poorest | 15.9 (13.8–18.3) | 15.8 (13.7–18.1) | 18.1 (16.2–20.3) | 18.0 (15.8–20.4) | 17.8 (15.5–20.4) | 18.3 (16.0–20.8) |
| Poor | 21.2 (18.5–24.1) | 20.5 (17.9–23.4) | 21.3 (19.4–23.3) | 20.2 (18.5–21.9) | 20.5 (18.8–22.3) | 20.6 (18.9–22.3) | |
| Middle | 22.3 (20.4–24.3) | 21.7 (19.9–23.5) | 21.5 (19.9–23.3) | 21.0 (19.4–22.5) | 21.4 (19.8–23.1) | 20.3 (18.8–21.9) | |
| Rich | 20.8 (18.9–22.9) | 21.7 (19.7–23.9) | 21.0 (19.4–22.7) | 21.6 (19.9–23.3) | 20.9 (19.3–22.7) | 21.0 (19.4–22.8) | |
| Richest | 19.8 (17.7–22.0) | 20.3 (18.3–22.5) | 18.0 (16.4–19.8) | 19.3 (17.6–21.1) | 19.3 (17.5–21.2) | 19.8 (17.9–21.8) | |
| Mother’s Schooling | Primary | 34.3 (31.7–36.9) | 34.6 (31.9–37.3) | 47.8 (45.4–50.3) | 47.9 (45.6–50.3) | 16.3 (14.3–18.4) | 15.9 (14.1–18.0) |
| Secondary | 44.3 (41.8–46.8) | 43.6 (41.3–46.0) | 40.1 (38.0–42.3) | 39.8 (37.8–41.8) | 68.7 (66.2–71.1) | 69.3 (67.0–71.5) | |
| Higher secondary | 10.8 (9.3–12.5) | 11.4 (9.9–13.1) | 6.7 (6.0–7.6) | 6.9 (6.2–7.8) | 9.7 (7.7–12.1) | 9.5 (7.7–11.6) | |
| Graduation and above | 10.7 (9.2–12.4) | 10.4 (9.0–12.0) | 5.3 (4.7–6.1) | 5.4 (4.8–6.1) | 5.3 (4.4–6.3) | 5.3 (4.5–6.3) | |
| Father’s Occupation | Professional | 7.9 (6.8–9.2) | 8.5 (7.4–9.9) | 9.4 (8.1–10.8) | 9.5 (8.3–10.8) | 10.0 (8.5–11.7) | 9.4 (8.0–10.9) |
| Sales and services | 26.8 (24.6–29.1) | 28.0 (25.7–30.4) | 23.1 (21.4–25.0) | 24.2 (22.3–26.1) | 24.4 (22.7–26.2) | 24.1 (22.5–25.8) | |
| Manual, agriculture | 51.5 (48.8–54.1) | 50.4 (47.6–53.2) | 54.8 (52.2–57.4) | 53.8 (51.4–56.2) | 51.3 (48.8–53.7) | 52.4 (50.0–54.7) | |
| Others | 13.8 (11.8–16.0) | 13.1 (11.3–15.1) | 12.7 (11.1–14.5) | 12.5 (11.0–14.2) | 14.3 (12.5–16.4) | 14.2 (12.4–16.1) | |
| Child schooling | Yes | - | - | 92.2 (91.1–93.2) | 92.1 (91.1–93.0) | 80.7 (78.9–82.4) | 80.9 (79.2–82.5) |
| No | - | - | 7.8 (6.8–8.9) | 7.9 (7.0–8.9) | 19.3 (17.6–21.1) | 19.1 (17.5–20.8) | |
| Stunting | No stunting (HAZ < −2SD) | 64.4 (62.1–66.7) | 64.5 (62.3–66.7) | 79.3 (77.7–80.8) | 78.6 (76.9–80.3) | 73.0 (71.0–74.9) | 73.4 (71.6–75.2) |
| Moderate (HAZ: −3 to −2SD) | 24.0 (22.2–26.0) | 23.3 (21.6–25.0) | 15.5 (14.3–16.8) | 16.4 (15.1–17.8) | 21.3 (19.6–23.1) | 20.7 (19.2–22.3) | |
| Severe (HAZ < −3SD) | 11.5 (10.1–13.2) | 12.2 (10.7–13.9) | 5.1 (4.3–6.1) | 5.0 (4.2–5.8) | 5.7 (4.9–6.6) | 5.9 (5.1–6.7) | |
| Underweight | Not present (WAZ < −2SD) | 64.8 (62.0–67.6) | 65.1 (62.5–67.6) | - | - | - | - |
| Moderate (WAZ: −3 to −2SD) | 26.2 (23.7–28.8) | 26.7 (24.3–29.2) | - | - | - | - | |
| Severe (WAZ < −3SD) | 9.0 (7.8–10.3) | 8.2 (7.2–9.4) | - | - | - | - | |
| Wasting/ Thinness | Not present (WHZ < −2SD) | 84.0 (82.1–85.6) | 85.0 (83.5–86.5) | 76.4 (74.8–78.0) | 76.6 (75.2–78.0) | 75.5 (73.7–77.2) | 75.7 (74.0–77.2) |
| Moderate (WHZ:−3 to −2SD) | 12.2 (10.8–13.8) | 11.6 (10.4–12.9) | 18.5 (17.1–19.9) | 18.4 (17.1–19.8) | 18.1 (16.6–19.7) | 17.9 (16.6–19.4) | |
| Severe (WHZ < −3SD) | 3.8 (3.0–4.8) | 3.4 (2.8–4.1) | 5.1 (4.3–6.0) | 5.0 (4.3–5.8) | 6.4 (5.7–7.3) | 6.4 (5.6–7.3) | |
| Drinking water source | Piped and improved | 85.0 (82.4–87.3) | 85.2 (82.6–87.5) | 84.9 (82.5–87.0) | 85.2 (82.9–87.2) | 85.6 (83.5–87.5) | 86.2 (84.2–87.9) |
| Non-piped and improved | 8.9 (7.0–11.2) | 9.2 (7.4–11.3) | 8.2 (6.6–10.2) | 8.1 (6.7–9.9) | 8.1 (6.8–9.6) | 7.7 (6.5–9.1) | |
| Unimproved | 6.1 (4.8–7.6) | 5.6 (4.3–7.4) | 7.0 (5.7–8.4) | 6.7 (5.3–8.4) | 6.3 (5.1–7.9) | 6.1 (5.0–7.6) | |
| Handwashing | Basic | 50.3 (47.5–53.1) | 52.4 (49.7–55.2) | 46.8 (44.1–49.5) | 49.3 (46.7–51.9) | 47.8 (45.3–50.3) | 48.7 (46.2–51.3) |
| Limited | 36.1 (33.4–38.8) | 33.8 (31.3–36.5) | 39.4 (36.6–42.3) | 37.2 (34.6–39.8) | 35.5 (33.1–38.0) | 34.7 (32.5–37.1) | |
| No facility | 13.6 (11.7–15.9) | 13.7 (11.8–15.9) | 13.8 (12.1–15.8) | 13.5 (11.8–15.4) | 16.7 (14.7–19.0) | 16.5 (14.4–18.8) | |
| Sanitation | Improved and not shared | 43.8 (40.5–47.2) | 44.1 (41.0–47.1) | 39.7 (37.2–42.3) | 40.5 (38.0–43.0) | 47.8 (45.3–50.4) | 47.1 (44.5–49.7) |
| Improved and shared | 12.2 (10.8–13.7) | 13.0 (11.6–14.6) | 12.3 (11.0–13.8) | 12.3 (11.0–13.8) | 8.7 (7.7–9.8) | 9.0 (8.0–10.1) | |
| Unimproved | 44.0 (40.1–48.0) | 43.0 (39.3–46.7) | 48.0 (44.8–51.2) | 47.2 (44.1–50.4) | 43.5 (40.6–46.4) | 43.9 (41.1–46.8) | |
| History of diarrhea in the two weeks prior to survey | Yes | 15.0 (12.9–17.5) | 15.3 (13.3–17.6) | 9.4 (8.2–10.7) | 9.0 (8.0–10.2) | - | - |
| No | 85.0 (82.5–87.1) | 84.7 (82.4–86.7) | 90.6 (89.3–91.8) | 91.0 (89.8–92.0) | - | - | |
| History of fever in the two weeks prior to survey | Yes | 30.7 (28.3–33.2) | 31.5 (29.2–33.9) | 21.8 (19.8–24.0) | 22.2 (20.5–24.0) | - | - |
| No | 69.3 (66.8–71.7) | 68.5 (66.1–70.8) | 78.2 (76.0–80.2) | 77.8 (76.0–79.5) | - | - | |
| (A) | ||||||
| Sex | 1–4 Years (n = 9976) | 5–9 Years (n = 12,156) | 10–19 Years (n = 11,748) | |||
| Vitamin B12 (pg/mL) Geometric Mean (95% CI) | Vitamin B12 Deficiency % (95% CI) | Vitamin B12 (pg/mL) Geometric Mean (95% CI) | Vitamin B12 Deficiency % (95% CI) | Vitamin B12 (pg/mL) Geometric Mean (95% CI) | Vitamin B12 Deficiency % (95% CI) | |
| Boys | 310.3 a (301.4–319.3) | 14.3 a (11.4–17.7) | 297.3 a (290.0–304.7) | 16.7 a (14.7–18.9) | 241.6 a (235.2–248.2) | 35.0 a (31.8–38.3) |
| Girls | 313.3 a (304.1–322.8) | 13.3 a (10.9–16.2) | 291.7 a (283.5–300.2) | 17.9 a (15.3–20.8) | 257.1 b (250.6–263.8) | 27.0 b (24.4–29.7) |
| Total | 311.7 * (305.0–318.5) | 13.8 † (11.7–16.2) | 294.6 # (288.2–301.0) | 17.3 † (15.4–19.3) | 249.2 $ (243.9–254.6) | 31.0 ‡ (28.7–33.5) |
| (B) | ||||||
| Sex | 1–4 Years (n = 11,004) | 5–9 Years (n = 14,125) | 10–19 Years (n = 13,621) | |||
| Folate (ng/mL) Geometric Mean (95% CI) | Folate Deficiency % (95% CI) | Folate (ng/mL) Geometric Mean (95% CI) | Folate Deficiency % (95% CI) | Folate (ng/mL) Geometric Mean (95% CI) | Folate Deficiency % (95% CI) | |
| Boys | 245.8 a (233.4–258.9) | 22.6 a (19.7–25.8) | 217.7 a (208.0–228.0) | 27.7 a (25.1–30.4) | 173.3 a (164.4–182.6) | 38.3 a (35.3–41.4) |
| Girls | 237.8 a (225.1–251.1) | 22.9 a (20.2–25.9) | 212.2 a (201.8–223.2) | 27.6 a (25.1–30.3) | 196.7 b (186.6–207.3) | 32.9 a (30.2–35.7) |
| Total | 241.9 * (231.4–252.9) | 22.8 † (20.5–25.2) | 215.0 # (206.4–224.1) | 27.6 ‡ (25.5–29.9) | 184.5 $ (176.3–193.0) | 35.6 § (33.1–38.2) |
| Characteristics | 1–4 Years | 5–9 Years | 10–19 Years | ||||
|---|---|---|---|---|---|---|---|
| Vitamin B12 Deficiency % (95% CI) | Folate Deficiency % (95% CI) | Vitamin B12 Deficiency % (95% CI) | Folate Deficiency % (95% CI) | Vitamin B12 Deficiency % (95% CI) | Folate Deficiency % (95% CI) | ||
| Stunting | No Stunting (HAZ < −2 SD) | 12.7 a (10.2–15.8) | 22.9 a (20.5–25.5) | 17.8 a (15.8–20.0) | 28.1 a (25.9–30.4) | 31.2 a (28.8–33.7) | 37.2 a (34.4–40.1) |
| Moderate (HAZ: −3 to −2 SD) | 15.1 a (12.2–18.5) | 23.5 a (19.9–27.5) | 18.9 a (15.2–23.2) | 27.2 a (23.4–31.4) | 31.5 a (26.3–37.3) | 31.8 a (27.9–35.9) | |
| Severe (HAZ < −3 SD) | 18.9 a (12.7–27.3) | 21.6 a (16.8–27.4) | 8.2 b (5.2–12.8) | 22.2 a (16.7–28.8) | 27.6 a (20.3–36.3) | 29.1 a (23.5–35.5) | |
| Wasting/Thinness | Not present (WAZ < −2 SD) | 14.8 a (12.3–17.6) | 22.8 a (20.3–25.5) | 18.0 a (15.9–20.3) | 27.4 a (25.1–29.9) | 32.9 a (30.0–35.9) | 35.8 a (32.9–38.7) |
| Moderate (WAZ: −3 to −2 SD) | 11.1 a (8.2–14.8) | 21.5 a (17.5–26.2) | 17.0 a (13.7–20.8) | 29.1 a (25.6–32.9) | 26.8 ac (23.0–30.8) | 35.0 a (31.1–39.1) | |
| Severe (WAZ < −3 SD) | 7.8 a (4.7–12.7) | 24.0 a (17.1–32.7) | 12.1 a (8.0–18.0) | 26.4 a (20.5–33.4) | 21.6 bc (16.6–27.5) | 34.0 a (28.4–40.1) | |
| Underweight | Not present (WHZ < −2 SD) | 13.6 a (11.1–16.5) | 23.1 a (20.5–25.9) | - | - | - | - |
| Moderate (WHZ: −3 to −2 SD) | 15.8 a (12.2–20.2) | 22.6 a (18.9–26.8) | - | - | - | - | |
| Severe (WHZ < −3 SD) | 11.8 a (8.1–16.9) | 20.4 a (16.5–24.9) | - | - | - | - | |
| History of diarrhea in the two weeks prior to survey | Yes | 19.1 a (12.1–28.8) | 14.9 a (11.5–19.1) | 23.8 a (18.1–30.5) | 20.2 a (15.8–25.5) | - | - |
| No | 12.9 a (11.1–15.0) | 24.2 b (21.8–26.7) | 16.6 a (14.8–18.6) | 28.4 b (26.1–30.7) | - | - | |
| History of fever in the two weeks prior to survey | Yes | 16.9 a (11.6–23.9) | 19.6 a (16.4–23.3) | 15.8 a (12.5–19.8) | 22.8 a (19.6–26.4) | - | - |
| No | 12.5 a (10.7–14.4) | 24.2 a (21.5–27.1) | 17.7 a (15.9–19.7) | 29.0 b (26.7–31.4) | - | - | |
| IFA | 1–4 Years | 5–9 Years | 10–19 Years | |||
|---|---|---|---|---|---|---|
| Vitamin B12 Deficiency % (95% CI) | Folate Deficiency % (95% CI) | Vitamin B12 Deficiency % (95% CI) | Folate Deficiency % (95% CI) | Vitamin B12 Deficiency % (95% CI) | Folate Deficiency % (95% CI) | |
| Yes | 11.2 a (7.2–16.9) | 14.6 a (9.9–21.0) | 18.1 a (13.8–23.2) | 28.9 a (23.4–35.1) | 28.5 a (23.6–34.0) | 38.9 a (33.2–45.0) |
| No | 14.0 a (11.7–16.7) | 23.3 b (21.0–25.7) | 17.2 a (15.4–19.2) | 27.5 a (25.3–29.9) | 31.2 a (28.7–33.7) | 35.5 a (32.9–38.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shalini, T.; Pullakhandam, R.; Ghosh, S.; Kulkarni, B.; Rajkumar, H.; Sachdev, H.S.; Kurpad, A.V.; Reddy, G.B. Prevalence of Vitamin B12 and Folate Deficiencies in Indian Children and Adolescents. Nutrients 2023, 15, 3026. https://doi.org/10.3390/nu15133026
Shalini T, Pullakhandam R, Ghosh S, Kulkarni B, Rajkumar H, Sachdev HS, Kurpad AV, Reddy GB. Prevalence of Vitamin B12 and Folate Deficiencies in Indian Children and Adolescents. Nutrients. 2023; 15(13):3026. https://doi.org/10.3390/nu15133026
Chicago/Turabian StyleShalini, Tattari, Raghu Pullakhandam, Santu Ghosh, Bharati Kulkarni, Hemalatha Rajkumar, Harshpal S. Sachdev, Anura V. Kurpad, and Geereddy Bhanuprakash Reddy. 2023. "Prevalence of Vitamin B12 and Folate Deficiencies in Indian Children and Adolescents" Nutrients 15, no. 13: 3026. https://doi.org/10.3390/nu15133026
APA StyleShalini, T., Pullakhandam, R., Ghosh, S., Kulkarni, B., Rajkumar, H., Sachdev, H. S., Kurpad, A. V., & Reddy, G. B. (2023). Prevalence of Vitamin B12 and Folate Deficiencies in Indian Children and Adolescents. Nutrients, 15(13), 3026. https://doi.org/10.3390/nu15133026







