Weight Bias Internalization and Eating Disorder Psychopathology in Treatment-Seeking Patients with Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
- Weight (baseline), measured on medical weighing scales (Seca Digital Wheelchair Scale Model 664);
- Height, measured with a stadiometer (Wall-Mounted Mechanical Height Rod Model 00051A; Wunder);
- BMI, calculated using the standard formula (i.e., body weight (kg) divided by height (m) squared);
- Eating disorder features, assessing responses to the Eating Disorder Examination interview (EDE), Italian version [17]. This semi-structured questionnaire is designed to evaluate eating disorder psychopathology and behaviours in the 28 days before the interview is conducted. Specifically, scores of 0–6 are assigned to the behavioural symptoms (binge eating, self-induced vomiting, laxative misuse, diuretics misuse, excessive exercising, and food restriction) exhibited by individuals with eating disorders. EDE scores can be expressed on a global scale, but also four specific subscales (Restraint, Eating Concern, Weight Concern, and Shape Concern) reflecting the respective cognitive features. Excellent criterion validity and high test–retest reliability (r = 0.80) have been reported for the Italian version of the EDE, whose global score has very good inter-rater reliability (rho = 0.97) [17]. In our sample, Cronbach’s α for the global EDE score was 0.85. For the purposes of this study, the 22 items used to generate the four subscales and the global score were considered. The EDE was administered by assessors trained and supervised by RDG, an expert on the instrument;
- Weight bias internalization, assessed using the Italian version of the Weight Bias Internalization Scale (WBIS) [18]; this relies on a total of 11 items, rated on a seven-point Likert scale, to measure self-directed, weight-related stigma. The Cronbach’s α for the global WBIS score was 0.80 in our sample.
2.3. Statistical Analysis
2.3.1. Network Estimation
2.3.2. Bridge Nodes
2.3.3. Centrality Indices
2.3.4. Network Robustness, Stability, and Accuracy
3. Results
3.1. Patient Characteristics
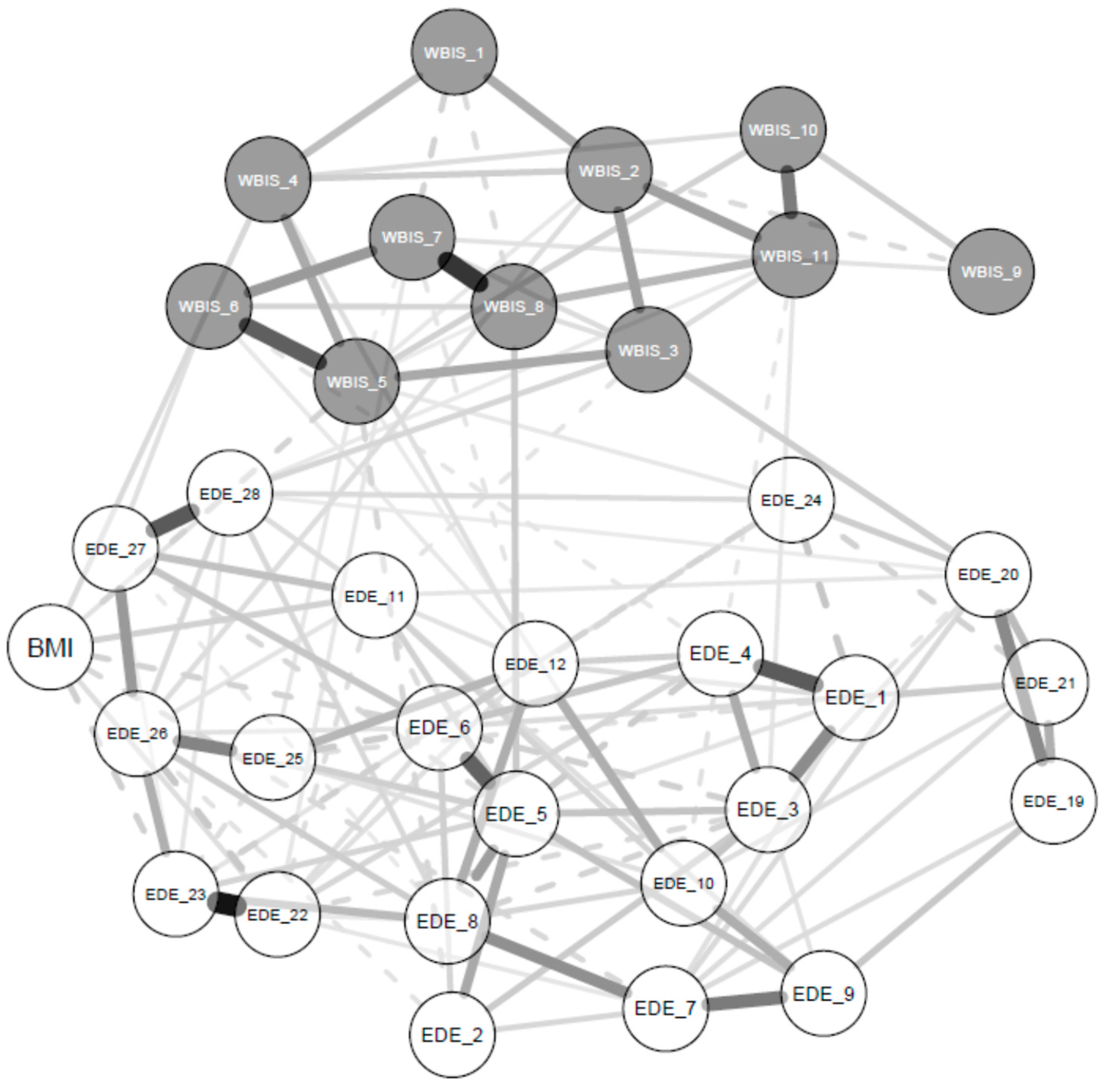
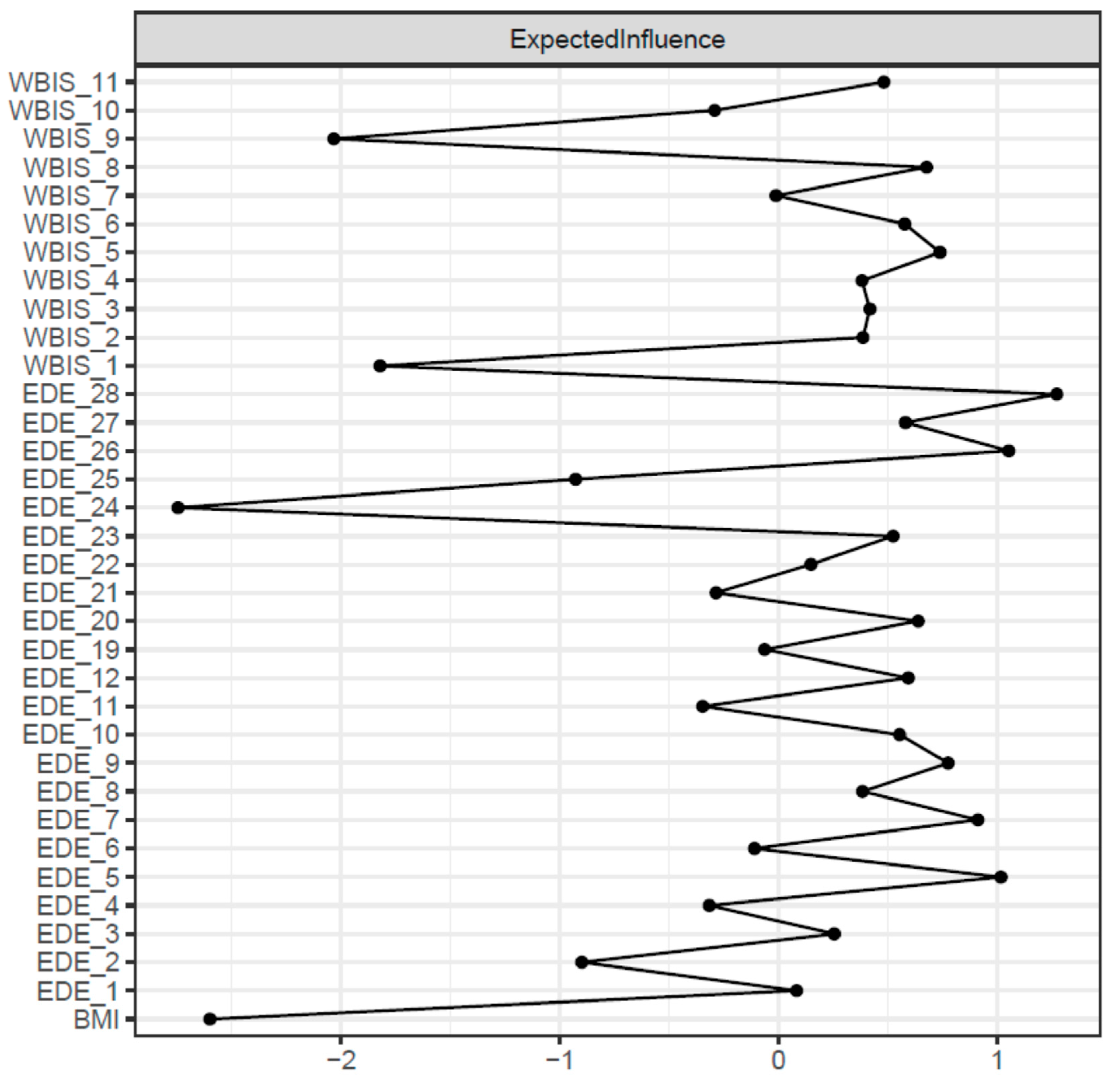
3.2. Network Structure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Puhl, R.; Brownell, K.D. Bias, discrimination, and obesity. Obes. Res. 2001, 9, 788–805. [Google Scholar] [CrossRef] [PubMed]
- Durso, L.E.; Latner, J.D. Understanding self-directed stigma: Development of the weight bias internalization scale. Obesity 2008, 16 (Suppl. S2), S80–S86. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Puhl, R.M.; Cummings, D.E.; Eckel, R.H.; Ryan, D.H.; Mechanick, J.I.; Nadglowski, J.; Ramos Salas, X.; Schauer, P.R.; Twenefour, D.; et al. Joint international consensus statement for ending stigma of obesity. Nat. Med. 2020, 26, 485–497. [Google Scholar] [CrossRef]
- Pearl, R.L.; Puhl, R.M. Weight bias internalization and health: A systematic review. Obes. Rev. 2018, 19, 1141–1163. [Google Scholar] [CrossRef] [PubMed]
- Himmelstein, M.S.; Puhl, R.M.; Pearl, R.L.; Pinto, A.M.; Foster, G.D. Coping with Weight Stigma among Adults in a Commercial Weight Management Sample. Int. J. Behav. Med. 2020, 27, 576–590. [Google Scholar] [CrossRef] [PubMed]
- Allegato B alla DGR n. 94, Scheda di Appropriatezza della Regione Veneto per il Ricovero Riabilitativo Intensivo dei Disturbi del Comportamento Alimentare; Regione Veneto: Venezia, Italy, 2012.
- Lawson, J.L.; LeCates, A.; Ivezaj, V.; Lydecker, J.; Grilo, C.M. Internalized weight bias and loss-of-control eating following bariatric surgery. Eat. Disord. 2021, 29, 630–643. [Google Scholar] [CrossRef]
- Tomiyama, A.J.; Epel, E.S.; McClatchey, T.M.; Poelke, G.; Kemeny, M.E.; McCoy, S.K.; Daubenmier, J. Associations of weight stigma with cortisol and oxidative stress independent of adiposity. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2014, 33, 862–867. [Google Scholar] [CrossRef]
- Durso, L.E.; Latner, J.D.; Hayashi, K. Perceived discrimination is associated with binge eating in a community sample of non-overweight, overweight, and obese adults. Obes. Facts 2012, 5, 869–880. [Google Scholar] [CrossRef]
- Romano, K.A.; Heron, K.E.; Henson, J.M. Examining associations among weight stigma, weight bias internalization, body dissatisfaction, and eating disorder symptoms: Does weight status matter? Body Image 2021, 37, 38–49. [Google Scholar] [CrossRef]
- Pearl, R.L.; White, M.A.; Grilo, C.M. Overvaluation of shape and weight as a mediator between self-esteem and weight bias internalization among patients with binge eating disorder. Eat. Behav. 2014, 15, 259–261. [Google Scholar] [CrossRef]
- Wang, S.B.; Lydecker, J.A.; Grilo, C.M. Rumination in patients with binge-eating disorder and obesity: Associations with eating-disorder psychopathology and weight-bias internalization. Eur. Eat. Disord. Rev. 2017, 25, 98–103. [Google Scholar] [CrossRef]
- McNally, R.J. Can network analysis transform psychopathology? Behav. Res. Ther. 2016, 86, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Personal. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Donini, L.M.; Dalle Grave, R.; Di Flaviano, E.; Gentile, M.G.; Mezzani, B.; Pandolfo Mayme, M.; Brunani, A.; Rovera, G.; Santini, F.; Lenzi, A.; et al. Assessing the appropriateness of the level of care for morbidly obese subjects: Validation of the CASCO-R scale. Ann. Ig. Med. Prev. Comunita 2014, 26, 195–204. [Google Scholar]
- Calugi, S.; Ricca, V.; Castellini, G.; Lo Sauro, C.; Ruocco, A.; Chignola, E.; El Ghoch, M.; Dalle Grave, R. The Eating Disorder Examination: Reliability and validity of the Italian version. Eat. Weight. Disord. 2015, 20, 505–511. [Google Scholar] [CrossRef]
- Innamorati, M.; Imperatori, C.; Lamis, D.A.; Contardi, A.; Castelnuovo, G.; Tamburello, S.; Manzoni, G.M.; Fabbricatore, M. Weight Bias Internalization scale discriminates obese and overweight patients with different severity levels of depression: The Italian version of the WBIS. Curr. Psychol. 2017, 36, 242–251. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Zhao, T.; Liu, H.; Roeder, K.; Lafferty, J.; Wasserman, L. The huge package for high-dimensional undirected graph estimation in R. J. Mach. Learn. Res. 2012, 13, 1059–1062. [Google Scholar] [PubMed]
- Epskamp, S.; Cramer, A.O.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network visualizations of relationships in psychometric data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Epskamp, S.; Fried, E.I. A tutorial on regularized partial correlation networks. Psychol. Methods 2018, 23, 617–634. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Kruis, J.; Marsman, M. Estimating psychopathological networks: Be careful what you wish for. PLoS ONE 2017, 12, e0179891. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef]
- Barber, R.F.; Drton, M. High-dimensional Ising model selection with Bayesian information criteria. Electron. J. Stat. 2015, 9, 567–607. [Google Scholar] [CrossRef]
- Foygel, R.; Drton, M. Extended Bayesian Information Criteria for Gaussian Graphical Models. In Advances in Neural Information Processing Systems 23; Lafferty, J.D., Williams, C.K.I., Shawe-Taylor, J., Zemel, R.S., Culotta, A., Eds.; Curran Associates, Inc.: Red Hook, NY, USA, 2010; pp. 604–612. [Google Scholar]
- Levinson, C.A.; Brosof, L.C.; Vanzhula, I.; Christian, C.; Jones, P.; Rodebaugh, T.L.; Langer, J.K.; White, E.K.; Warren, C.; Weeks, J.W.; et al. Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. Int. J. Eat. Disord. 2018, 51, 693–709. [Google Scholar] [CrossRef]
- Robinaugh, D.J.; Millner, A.J.; McNally, R.J. Identifying highly influential nodes in the complicated grief network. J. Abnorm. Psychol. 2016, 125, 747–757. [Google Scholar] [CrossRef]
- Yokoyama, H.; Nozaki, T.; Nishihara, T.; Sawamoto, R.; Komaki, G.; Sudo, N. Factors associated with the improvement of body image dissatisfaction of female patients with overweight and obesity during cognitive behavioral therapy. Front. Psychiatry 2022, 13, 1025946. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Czepczor-Bernat, K.; Modrzejewska, A. The relationship between eating patterns, body image and emotional dysregulation: Similarities between an excessive and normal body weight sample. Psychiatr. Pol. 2021, 55, 1065–1078. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Cuzzolaro, M.; Calugi, S.; Tomasi, F.; Temperilli, F.; Marchesini, G.; Group, Q.S. The effect of obesity management on body image in patients seeking treatment at medical centers. Obesity 2007, 15, 2320–2327. [Google Scholar] [CrossRef]
- Weinberger, N.A.; Kersting, A.; Riedel-Heller, S.G.; Luck-Sikorski, C. Body dissatisfaction in individuals with obesity compared to normal-weight individuals: A systematic review and meta-analysis. Obes. Facts 2016, 9, 424–441. [Google Scholar] [CrossRef]
- Shafran, R.; Fairburn, C.G.; Nelson, L.; Robinson, P.H. The interpretation of symptoms of severe dietary restraint. Behav. Res. Ther. 2003, 41, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R.; Di Pauli, D.; Sartirana, M.; Calugi, S.; Shafran, R. The interpretation of symptoms of starvation/severe dietary restraint in eating disorder patients. Eat. Weight. Disord. 2007, 12, 108–113. [Google Scholar] [CrossRef]
| BMI | Body Mass Index |
|---|---|
| EDE_1 | Restraint over eating |
| EDE_2 | Avoidance of eating |
| EDE_3 | Food avoidance |
| EDE_4 | Dietary rules |
| EDE_5 | Wanting an empty stomach |
| EDE_6 | Flat stomach |
| EDE_7 | Preoccupation with food, eating or calories |
| EDE_8 | Preoccupation with shape or weight |
| EDE_9 | Fear of losing control over eating |
| EDE_10 | Fear of weight gain |
| EDE_11 | Feelings of fatness |
| EDE_12 | Desire to lose weight |
| EDE_19 | Eating in secret |
| EDE_20 | Social eating |
| EDE_21 | Guilt about eating |
| EDE_22 | Importance of weight |
| EDE_23 | Importance of shape |
| EDE_24 | Reaction to prescribed weighing |
| EDE_25 | Dissatisfaction with weight |
| EDE_26 | Dissatisfaction with shape |
| EDE_27 | Discomfort seeing body |
| EDE_28 | Avoidance of exposure |
| WBIS_1 | As an overweight person, I feel that I am just as competent as anyone |
| WBIS_2 | I am less attractive than most other people because of my weight |
| WBIS_3 | I feel anxious about being overweight because of what people might think of me |
| WBIS_4 | I wish I could drastically change my weight |
| WBIS_5 | Whenever I think a lot about being overweight, I feel depressed |
| WBIS_6 | I hate myself for being overweight |
| WBIS_7 | My weight is a major way that I judge my value as a person |
| WBIS_8 | I don’t feel that I deserve to have a really fulfilling social life, as long as I’m overweight |
| WBIS_9 | I am OK being the weight that I am |
| WBIS_10 | Because I’m overweight, I don’t feel like my true self |
| WBIS_11 | Because of my weight, I don’t understand how anyone attractive would want to date me |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calugi, S.; Segattini, B.; Cattaneo, G.; Chimini, M.; Dalle Grave, A.; Dametti, L.; Molgora, M.; Dalle Grave, R. Weight Bias Internalization and Eating Disorder Psychopathology in Treatment-Seeking Patients with Obesity. Nutrients 2023, 15, 2932. https://doi.org/10.3390/nu15132932
Calugi S, Segattini B, Cattaneo G, Chimini M, Dalle Grave A, Dametti L, Molgora M, Dalle Grave R. Weight Bias Internalization and Eating Disorder Psychopathology in Treatment-Seeking Patients with Obesity. Nutrients. 2023; 15(13):2932. https://doi.org/10.3390/nu15132932
Chicago/Turabian StyleCalugi, Simona, Barbara Segattini, Gianmatteo Cattaneo, Mirko Chimini, Anna Dalle Grave, Laura Dametti, Manuela Molgora, and Riccardo Dalle Grave. 2023. "Weight Bias Internalization and Eating Disorder Psychopathology in Treatment-Seeking Patients with Obesity" Nutrients 15, no. 13: 2932. https://doi.org/10.3390/nu15132932
APA StyleCalugi, S., Segattini, B., Cattaneo, G., Chimini, M., Dalle Grave, A., Dametti, L., Molgora, M., & Dalle Grave, R. (2023). Weight Bias Internalization and Eating Disorder Psychopathology in Treatment-Seeking Patients with Obesity. Nutrients, 15(13), 2932. https://doi.org/10.3390/nu15132932







