The Impact of Infant Feeding Regimen on Cow’s Milk Protein Allergy, Atopic Dermatitis and Growth in High-Risk Infants during the First 6 Months of Life: The Allergy Reduction Trial
Abstract
1. Introduction
2. Materials and Methods
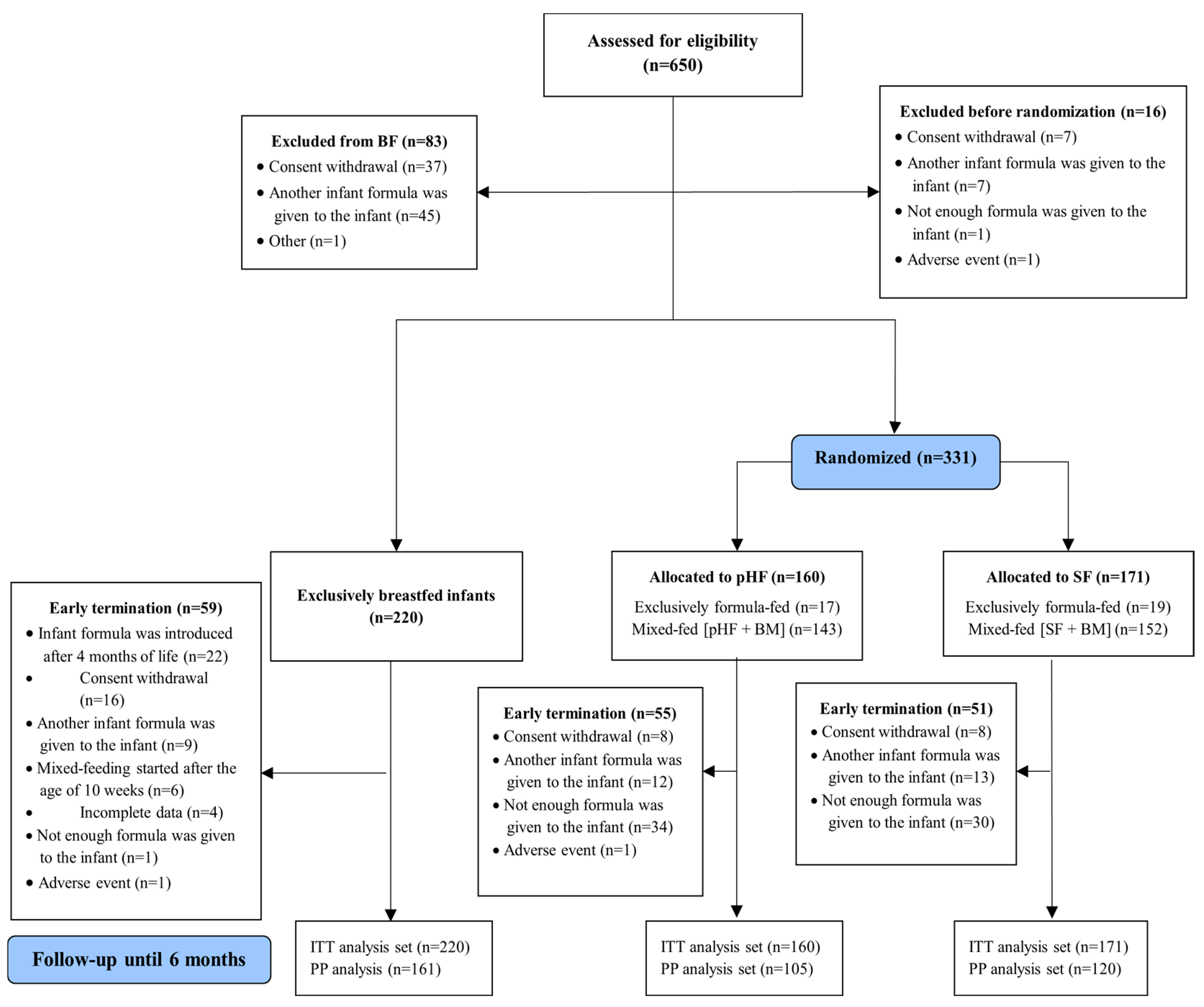
2.1. Study Design and Participants
2.2. Recruitment Procedures and Inclusion Criteria
2.3. Follow-Up Evaluation and Compliance
2.4. Definition of Study Outcomes
2.5. Statistical Analysis
3. Results
3.1. Study Populations at Baseline
3.1.1. ITT Population
3.1.2. PP Population
3.2. Effect of Intervention
3.2.1. ITT Population
3.2.2. PP Population
3.3. The Estimated Breastmilk Intake in Mixed-Fed Groups
3.4. Limitations and Strengths of This Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Allen, K.J.; Koplin, J.J. Prospects for prevention of food allergy. J. Allergy Clin. Immunol. Pract. 2016, 4, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Zepeda-Ortega, B.; Goh, A.; Xepapadaki, P.; Sprikkelman, A.; Nicolaou, N.; Hernandez, R.E.H.; Latiff, A.H.A.; Yat, M.T.; Diab, M.; Hussaini, B.A.; et al. Strategies and Future Opportunities for the Prevention, Diagnosis, and Management of Cow Milk Allergy. Front. Immunol. 2021, 12, 608372. [Google Scholar] [CrossRef] [PubMed]
- Flom, J.D.; Sicherer, S.H. Epidemiology of Cow’s Milk Allergy. Nutrients 2019, 11, 1051. [Google Scholar] [CrossRef] [PubMed]
- Bylund, S.; Kobyletzki, L.B.; Svalstedt, M.; Svensson, Å. Prevalence and Incidence of Atopic Dermatitis: A Systematic Review. Acta Derm. Venereol. 2020, 100, adv00160. [Google Scholar] [CrossRef]
- Papapostolou, N.; Xepapadaki, P.; Gregoriou, S.; Makris, M. Atopic Dermatitis and Food Allergy: A Complex Interplay What We Know and What We Would Like to Learn. J. Clin. Med. 2022, 11, 4232. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Dupont, C.; Eigenmann, P.; Host, A.; Kuitunen, M.; Ribes-Koninckx, C.; Shah, N.; Shamir, R.; Staiano, A.; Szajewska, H.; et al. A workshop report on the development of the Cow’s Milk-related Symptom Score awareness tool for young children. Acta Paediatr. 2015, 104, 334–349. [Google Scholar] [CrossRef] [PubMed]
- Severity scoring of atopic dermatitis: The SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology 1993, 186, 23–31. [CrossRef]
- Onizawa, Y.; Noguchi, E.; Okada, M.; Sumazaki, R.; Hayashi, D. The Association of the Delayed Introduction of Cow’s Milk with IgE-Mediated Cow’s Milk Allergies. J. Allergy Clin. Immunol. Pract. 2016, 4, 481–488.e2. [Google Scholar] [CrossRef]
- Bion, V.; Lockett, G.A.; Soto-Ramirez, N.; Zhang, H.; Venter, C.; Karmaus, W.; Holloway, J.W.; Arshad, S.H. Evaluating the efficacy of breastfeeding guidelines on long-term outcomes for allergic disease. Allergy 2016, 71, 661–670. [Google Scholar] [CrossRef]
- du Toit, G.; Tsakok, T.; Lack, S.; Lack, G. Prevention of Food Allergy. J. Allergy Clin. Immunol. 2016, 137, 998–1010. [Google Scholar] [CrossRef]
- Flohr, C.; Henderson, A.J.; Kramer, M.S.; Patel, R.; Thompson, J.; Rifas-Shiman, S.L.; Yang, S.; Vilchuck, K.; Bogdanovich, N.; Hameza, M.; et al. Effect of an Intervention to Promote Breastfeeding on Asthma, Lung Function, and Atopic Eczema at Age 16 Years: Follow-Up of the PROBIT Randomized Trial. JAMA Pediatr. 2018, 172, e174064. [Google Scholar] [CrossRef] [PubMed]
- Greer, F.R.; Sicherer, S.H.; Burks, A.W. The effects of early nutritional interventions on the development of atopic disease in infants and children: The role of maternal dietary restriction, breastfeeding, hydrolyzed formulas, and timing of introduction of allergenic complementary foods. Pediatrics 2019, 143, e20190281. [Google Scholar] [CrossRef] [PubMed]
- Osborn, D.A.; Sinn, J.K.; Jones, L.J. Infant Formulas Containing Hydrolyzed Protein for Prevention of Allergic Disease. Cochrane Database Syst. Rev. 2018, 10, CD003664. [Google Scholar] [CrossRef]
- von Berg, A.; Filipiak-Pittroff, B.; Schulz, H.; Hoffmann, U.; Link, E.; Sussmann, M.; Schnappinger, M.; Brüske, I.; Standl, M.; Krämer, U.; et al. Allergic Manifestation 15 Years After Early Intervention with Hydrolyzed Formulas–the GINI Study. Allergy 2016, 71, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Boyle, R.J.; Tang, M.L.; Chiang, W.C.; Chua, M.C.; Ismail, I.; Nauta, A.; Hourihane, J.O.B.; Smith, P.; Gold, M.; Ziegler, J.; et al. Prebiotic-Supplemented Partially Hydrolyzed Cow’s Milk Formula for the Prevention of Eczema in High-Risk Infants: A Randomized Controlled Trial. Allergy 2016, 71, 701–710. [Google Scholar] [CrossRef]
- Urashima, M.; Mezawa, H.; Okuyama, M.; Urashima, T.; Hirano, D.; Gocho, N.; Tachimoto, H. Primary Prevention of Cow’s Milk Sensitization and Food Allergy by Avoiding Supplementation with Cow’s Milk Formula at Birth: A Randomized Clinical Trial. JAMA Pediatr. 2019, 173, 1137–1145. [Google Scholar] [CrossRef]
- Kelly, E.; DunnGalvin, G.; Murphy, B.P.; O’B Hourihane, J. Formula supplementation remains a risk for cow’s milk allergy in breast-fed infants. Pediatr. Allergy Immunol. 2019, 30, 810–816. [Google Scholar] [CrossRef]
- Nicolaou, N.; Pancheva, R.; Karaglani, E.; Sekkidou, M.; Marinova-Achkar, M.; Popova, S.; Tzaki, M.; Kapetanaki, A.; Iacovidou, N.; Boutsikou, T.; et al. The Risk Reduction Effect of a Nutritional Intervention with a Partially Hydrolyzed Whey-Based Formula on Cow’s Milk Protein Allergy and Atopic Dermatitis in High-Risk Infants Within the First 6 Months of Life: The Allergy Reduction Trial (A.R.T.), a Multicenter Double-Blinded Randomized Controlled Study. Front. Nutr. 2022, 9, 863599. [Google Scholar] [CrossRef]
- Sauser, J.; Nutten, S.; de Groot, N.; Pecquet, S.; Simon, D.; Simon, H.U.; Spergel, J.M.; Koletzko, S.; Blanchard, C. Partially Hydrolyzed Whey Infant Formula: Literature Review on Effects on Growth and the Risk of Developing Atopic Dermatitis in Infants from the General Population. Int. Arch. Allergy Immunol. 2018, 177, 123–134. [Google Scholar] [CrossRef]
- Picaud, J.C.; Pajek, B.; Arciszewska, M.; Tarczón, I.; Escribano, J.; Porcel, R.; Adelt, T.; Hassink, E.; Rijnierse, A.; Abrahamse-Berkeveld, M.; et al. An Infant Formula with Partially Hydrolyzed Whey Protein Supports Adequate Growth and Is Safe and Well-Tolerated in Healthy, Term Infants: A Randomized, Double-Blind, Equivalence Trial. Nutrients 2020, 12, 2072. [Google Scholar] [CrossRef]
- Daniels, L.; Gibson, R.S.; Diana, A.; Haszard, J.J.; Rahmannia, S.; Luftimas, D.E.; Hampel, D.; Shahab-Ferdows, S.; Reid, M.; Melo, L.; et al. Micronutrient intakes of lactating mothers and their association with breast milk concentrations and micronutrient adequacy of exclusively breastfed Indonesian infants. Am. J. Clin. Nutr. 2019, 110, 391–400. [Google Scholar] [CrossRef] [PubMed]
- von Berg, A.; Koletzko, S.; Grübl, A.; Filipiak-Pittroff, B.; Wichmann, H.E.; Bauer, C.P.; Reinhardt, D.; Berdel, D.; German Infant Nutritional Intervention Study Group. The effect of hydrolyzed cow’s milk formula for allergy prevention in the first year of life: The German Infant Nutritional Intervention Study, a randomized double-blind trial. J. Allergy Clin. Immunol. 2003, 111, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Katz, Y.; Rajuan, N.; Goldberg, M.R.; Eisenberg, E.; Heyman, E.; Cohen, A.; Leshno, M. Early exposure to cow’s milk protein is protective against IgE-mediated cow’s milk protein allergy. J. Allergy Clin. Immunol. 2010, 126, P77–P82.e1. [Google Scholar] [CrossRef] [PubMed]
- Sakihara, T.; Otsuji, K.; Arakaki, Y.; Hamada, K.; Sugiura, S.; Ito, K. Randomized trial of early infant formula introduction to prevent cow’s milk allergy. J. Allergy Clin. Immunol. 2021, 147, 224–232.e8. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Latiff, A.H.A.; Fleischer, D.M.; Gutiérrez-Castrellón, P.; Miqdady, M.S.; Smith, P.K.; von Berg, A.; Greenhawt, M.J. Partially hydrolyzed formula in non-exclusively breastfed infants: A systematic review and expert consensus. Nutrition 2019, 57, 268–274. [Google Scholar] [CrossRef]
- Inuo, C.; Tanaka, K.; Nakajima, Y.; Yamawaki, K.; Matsubara, T.; Iwamoto, H.; Tsuge, I.; Urisu, A.; Kondo, Y. Tolerability of partially and extensively hydrolysed milk formulas in children with cow’s milk allergy. Asia Pac. J. Clin. Nutr. 2019, 28, 49–56. [Google Scholar]
- Kansen, H.M.; Lebbink, M.A.; Mul, J.; van Erp, F.C.; van Engelen, M.; de Vries, E.; Prevaes, S.M.P.J.; Le, T.M.; van der Ent, C.K.; Verhagen, L.M. Risk factors for atopic diseases and recurrent respiratory tract infections in children. Pediatr. Pulmonol. 2020, 55, 3168–3179. [Google Scholar] [CrossRef]
- Xepapadaki, P.; Fiocchi, A.; Grabenhenrich, L.; Roberts, G.; Grimshaw, K.E.; Fiandor, A.; Larco, J.I.; Sigurdardottir, S.; Clausen, M.; Papadopoulos, N.G.; et al. Incidence and natural history of hen’s egg allergy in the first 2 years of life-the EuroPrevall birth cohort study. Allergy 2016, 71, 350–357. [Google Scholar] [CrossRef]
- Schoemaker, A.A.; Sprikkelman, A.B.; Grimshaw, K.E.; Roberts, G.; Grabenhenrich, L.; Rosenfeld, L.; Siegert, S.; Dubakiene, R.; Rudzeviciene, O.; Reche, M.; et al. Incidence and natural history of challenge-proven cow’s milk allergy in European children--EuroPrevall birth cohort. Allergy 2015, 70, 963–972. [Google Scholar] [CrossRef]
- Picariello, G.; De Cicco, M.; Nocerino, R.; Paparo, L.; Mamone, G.; Addeo, F.; Berni Canani, R. Excretion of Dietary Cow’s Milk Derived Peptides into Breast Milk. Front. Nutr. 2019, 6, 25. [Google Scholar] [CrossRef]
- Karaglani, E.; Thijs-Verhoeven, I.; Gros, M.; Chairistanidou, C.; Zervas, G.; Filoilia, C.; Kampani, T.M.; Miligkos, V.; Matiatou, M.; Valaveri, S.; et al. A Partially Hydrolyzed Whey Infant Formula Supports Appropriate Growth: A Randomized Controlled Non-Inferiority Trial. Nutrients 2020, 12, 3056. [Google Scholar] [CrossRef] [PubMed]



| ITT Analysis Dataset | |||||
|---|---|---|---|---|---|
| EBF Group (N = 220) | pHF Group (N = 160) | SF Group (N = 171) | p-Value | Total Sample (N = 551) | |
| Infant’s characteristics | |||||
| Country of infant’s birth | |||||
| Bulgaria, n (%) | 48 (31.8) a,b | 76 (47.5) a | 82 (48.0) b | <0.001 | 206 (37.4) |
| Cyprus, n (%) | 58 (26.4) | 55 (34.4) | 61 (35.7) | 174 (31.6) | |
| Greece, n (%) | 114 (51.8) a,b | 29 (18.1) a | 28 (16.4) b | 171 (31.0) | |
| Normal conception, n (%) | 215 (98.2) a | 148 (93.1) a | 164 (95.9) | 0.045 | 527 (96.0) |
| Gestational age, weeks, mean (SD) | 38.9 (1.0) a | 38.6 (1.2) a | 38.7 (1.0) | 0.025 | 38.8 (1.1) |
| Cesarean delivery, n (%) | 101 (45.9) a,b | 106 (66.3) a | 106 (62.0) b | <0.001 | 313 (56.8) |
| Birth weight, g, mean (SD) | 3303.6 (392.3) | 3270.5 (433.6) | 3278.1 (453.7) | 0.722 | 3286.1 (423.6) |
| Head circumference, cm, mean (SD) | 34.4 (1.2) | 34.2 (1.2) | 34.1 (1.1) | 0.011 | 34.2 (1.2) |
| Gender, female, n (%) | 104 (47.3) | 67 (41.9) | 78 (45.6) | 0.575 | 249 (45.2) |
| Mother’s characteristics | |||||
| Age, years, mean (SD) | 32.5 (4.9) | 31.7 (5.1) | 31.3 (5.1) | 0.062 | 31.9 (5.1) |
| Educational level | |||||
| ≤14 years, n (%) | 60 (27.3) b | 60 (37.5) | 70 (40.9) b | 0.012 | 190 (34.5) |
| >14 years, n (%) | 160 (72.7) b | 100 (62.5) | 101 (59.1) b | 361 (65.5) | |
| Mother smoking during pregnancy, n (%) | 13 (5.9) | 15 (9.4) | 22 (12.9) | 0.059 | 50 (9.1) |
| Mother smoking at baseline, n (%) | 25 (11.4) b | 28 (17.5) | 41 (24.0) b | 0.004 | 94 (17.1) |
| Father’s characteristics | |||||
| Age, years, mean (SD) | 35.1 (5.6) | 34.5 (5.7) | 34.1 (5.6) | 0.210 | 34.6 (5.6) |
| Educational level | |||||
| ≤14 years | 92 (41.8) b | 76 (47.8) | 95 (55.6) b | 0.026 | 263 (47.8) |
| >14 years | 128 (58.2) b | 83 (52.2) | 76 (44.4) b | 287 (52.2) | |
| Father smoking at baseline, n (%) | 82 (37.3) b | 77 (48.1) | 83 (48.5) b | 0.037 | 242 (43.9) |
| Family characteristics | |||||
| Family members at home, median, IQR | 4.0 (1.0) | 3.0 (1.0) | 3.0 (1.0) | 0.329 | 3.0 (1.0) |
| Urban residence, n (%) | 203 (92.3) b | 146 (91.3) | 141 (82.9) b | 0.008 | 490 (89.1) |
| Presence of pets indoors at home, n (%) | 39 (17.7) | 32 (20.0) | 38 (22.2) | 0.207 | 109 (19.8) |
| Medical history | |||||
| Family history of: | |||||
| Allergic asthma, n (%) | 66 (30.0) | 42 (26.3) | 42 (24.6) | 0.462 | 150 (27.2) |
| Rhinitis, n (%) | 130 (59.1) | 81 (50.6) | 85 (49.7) | 0.118 | 296 (53.7) |
| Atopic dermatitis, n (%) | 75 (34.1) | 46 (28.7) | 44 (25.7) | 0.186 | 165 (29.9) |
| Urticaria, n (%) | 32 (14.6) | 22 (13.8) | 28 (16.4) | 0.789 | 82 (14.9) |
| Food allergy, n (%) | 70 (31.8) | 45 (28.1) | 52 (30.4) | 0.741 | 167 (30.3) |
| Occurrence of early life infections in infants | |||||
| No infections, n (%) | 176 (80.0) | 114 (71.3) | 127 (74.3) | 0.177 | 417 (75.7) |
| Before 1st month, n (%) | 7 (3.2) | 3 (1.9) | 6. (3.5) | 16 (2.9) | |
| After 1st month, n (%) | 37 (16.8) | 43 (26.9) | 38 (22.2) | 118 (21.4) | |
| Time-Point of Evaluation (ITT Analysis Dataset) | Time Effect (4-Month Change) | Time Effect (6-Month Change) | |||
|---|---|---|---|---|---|
| Baseline | Visit 2 (4 Months) | Visit 3 (6 Months) | |||
| Mean (SEM) | Mean (SEM) | Mean (SEM) | Mean Change (95% CI) | Mean Change (95% CI) | |
| Body weight (kg) | |||||
| EBF group (n = 219) | 3.25 (0.007) a,b | 6.62 (0.046) | 7.65 (0.060) | 3.37 (3.28; 3.46) | 4.41 (4.29; 4.53) |
| pHF group (n = 159) | 3.22 (0.008) a | 6.63 (0.052) | 7.68 (0.069) | 3.41 (3.31; 3.51) | 4.47 (4.33; 4.60) |
| SFgroup (n = 170) | 3.20 (0.008) b | 6.76 (0.052) | 7.82 (0.068) | 3.55 (3.45; 3.66) | 4.62 (4.49; 4.75) |
| Treatment effect (p-value) * | <0.001 | 0.085 | 0.148 | 0.025 | 0.017 |
| Length (cm) | |||||
| EBF group (n = 219) | 49.9 (0.09) | 63.4 (0.17) | 67.4 (0.19) | 13.4 (13.1; 13.7) | 17.5 (17.1; 17.8) |
| pHF group (n = 159) | 49.8 (0.11) | 63.6 (0.19) | 67.9 (0.21) | 13.8 (13.4; 14.1) | 18.1 (17.7; 18.5) |
| SFgroup (n = 170) | 50.0 (0.10) | 63.4 (0.19) | 67.9 (0.21) | 13.5 (13.1; 13.8) | 17.9 (17.6; 18.3) |
| Between-group effect (p-value) * | 0.412 | 0.770 | 0.127 | 0.305 | 0.056 |
| Body Mass Index (Kg/m2) | |||||
| EBF group (n = 219) | 13.0 (0.05) b | 16.5 (0.11) | 16.8 (0.12) | 3.5 (3.2; 3.7) | 3.8 (3.6; 4.1) |
| pHF group (n = 159) | 12.9 (0.06) | 16.4 (0.13) | 16.7 (0.14) | 3.5 (3.2; 3.7) | 3.7 (3.5; 4.0) |
| SFgroup (n = 170) | 12.8 (0.06) b | 16.8 (0.13) | 16.9 (0.14) | 4.0 (3.7; 4.3) | 4.2 (3.9; 4.4) |
| Between-group effect (p-value) * | 0.035 | 0.075 | 0.405 | 0.004 | 0.004 |
| Head Circumference (cm) | |||||
| EBF group (n = 219) | 34.4 (0.07) b | 41,3 (0.08) | 43.0 (0.10) | 6.9 (6.8; 7.1) | 8.6 (8.5; 8.8) |
| pHF group (n = 159) | 34.2 (0.07) | 41.3 (0.10) | 42.9 (0.11) | 7.1 (6.9; 7.3) | 8.7 (8.5; 8.9) |
| SFgroup (n = 170) | 34.1 (0.07) b | 41.3 (0.09) | 43.0 (0.11) | 7.2 (7.0; 7.4) | 8.9 (8.7; 9.1) |
| Between-group effect (p-value) * | 0.020 | 0.997 | 0.907 | 0.083 | 0.057 |
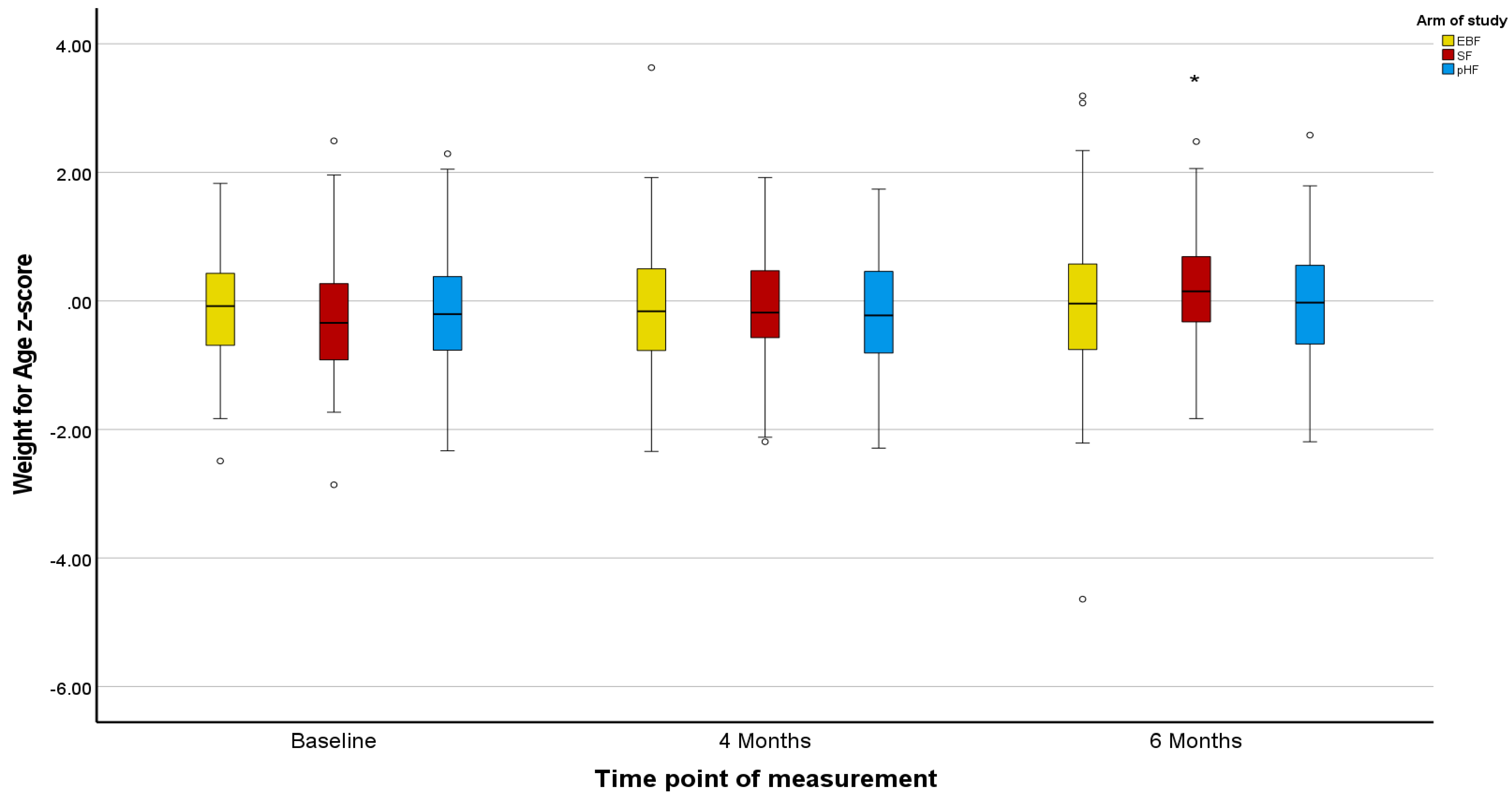
| Weight-for-age Z-score | |||||
| EBF group (n = 219) | −0.13 (0.02) a,b | −0.28 (0.06) | −0.13 (0.07) | −0.15 (−0.27; −0.03) | 0.00 (−0.14; 0.14) |
| pHF group (n = 159) | −0.19 (0.02) a | −0.25 (0.07) | −0.08 (0.08) | −0.06 (−0.19; 0.08) | 0.12 (−0.04; 0.27) |
| SFgroup (n = 170) | −0.22 (0.02) b | −0.08 (0.07) | 0.09 (0.08) | 0.14 (0.009; 0.27) | 0.31 (0.16; 0.46) |
| Treatment effect (p-value) * | <0.001 | 0.069 | 0.109 | 0.006 | 0.003 |
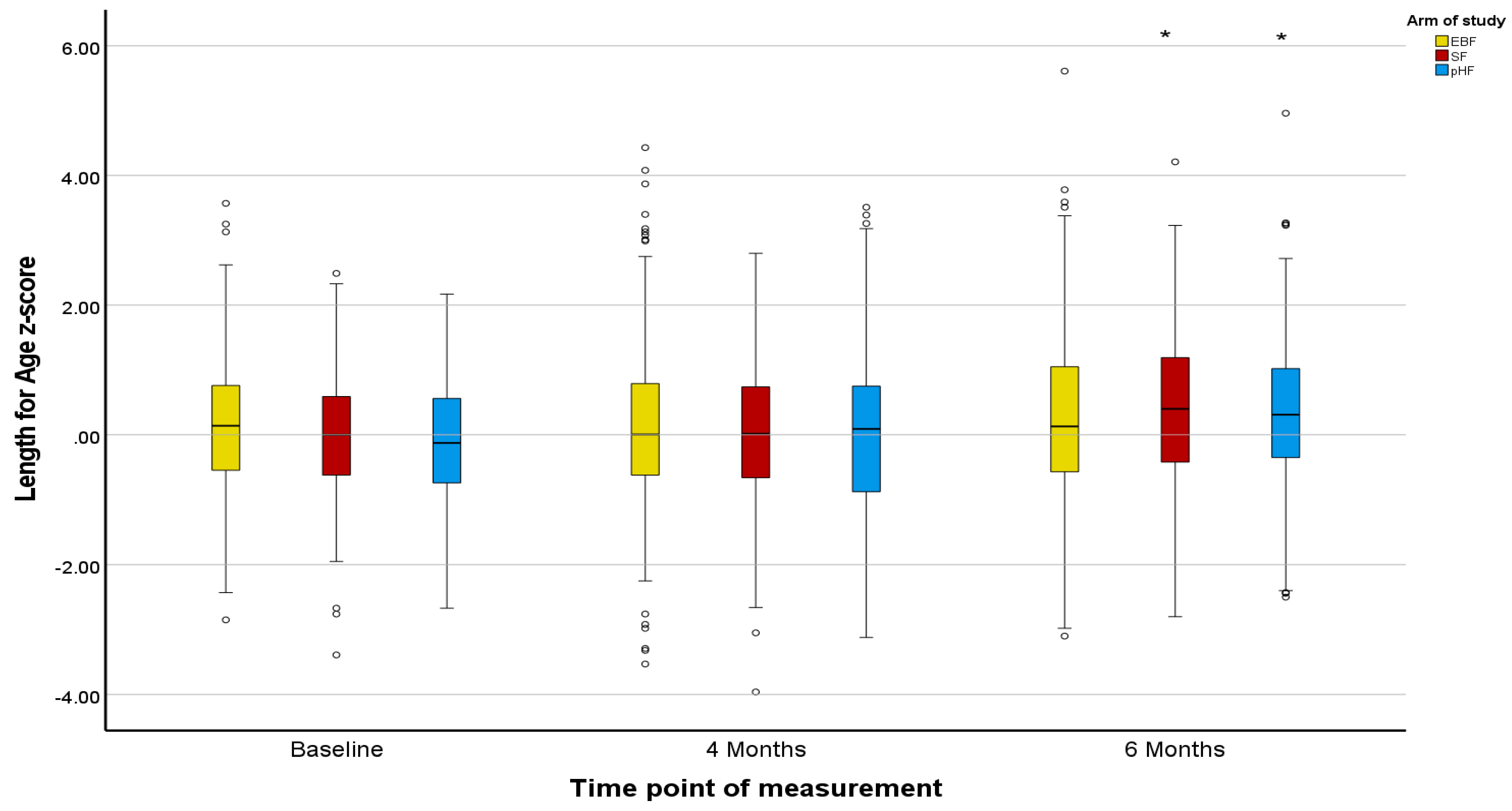
| Length-for-age-Z-score | |||||
| EBF group (n = 219) | 0.04 (0.05) | 0.04 (0.08) | 0.19 (0.08) | 0.002 (−0.14; 0.15) | 0.15 (−0.01; 0.31) |
| pHF group (n = 159) | −0.06 (0.06) | 0.14 (0.09) | 0.43 (0.10) | 0.19 (0.03; 0.36) | 0.48 (0.30; 0.67) |
| SFgroup (n = 170) | 0.03 (0.06) | 0.08 (0.09) | 0.44 (0.09) | 0.04 (−0.12; 0.21) | 0.41 (0.23; 0.59) |
| Between-group effect (p-value) * | 0.419 | 0.722 | 0.081 | 0.206 | 0.019 |
| Body Mass Index-for age Z-score | |||||
| EBF group (n = 219) | −0.34 (0.04) b | −0.40 (0.04) | −0.31 (0.09) | −0.06 (−0.23; 0.10) | 0.03 (−0.15; 0.21) |
| pHF group (n = 159) | −0.37 (0.05) | −0.43 (0.09) | −0.42 (0.10) c | −0.06 (−0.25; 0.13) | −0.05 (−0.26; 0.15) |
| SFgroup (n = 170) | −0.50 (0.05) b | −0.16 (0.09) | −0.22 (0.10) c | 0.34 (0.15; 0.52) | 0.29 (0.09; 0.49) |
| Between-group effect (p-value) * | 0.032 | 0.069 | 0.333 | 0.003 | 0.002 |
| EBF Group (N = 161) | pHF Group (N = 105) | SF Group (N = 120) | p-Value | Total Sample (N = 386) | |
|---|---|---|---|---|---|
| Infant’s characteristics | |||||
| Country of infant’s birth | |||||
| Bulgaria, n (%) | 35 (21.7) a,b | 45 (42.9) a | 58 (48.3) b | <0.001 | 138 (35.8) |
| Cyprus, n (%) | 33 (20.5) a,b | 45 (42.9) a | 43 (35.8) b | 121 (31.3) | |
| Greece, n (%) | 93 (57.8) a,b | 15 (14.3) a | 19 (15.8) b | 127 (32.9) | |
| Normal conception, n (%) | 157 (97.5) | 97 (92.4) | 113 (94.2) | 0.214 | 367 (95.3) |
| Gestational age, weeks, mean (SD) | 38.9 (1.0) a | 38.6 (1.2) a | 38.7 (1.0) | 0.023 | 38.8 (1.1) |
| Cesarean delivery, n (%) | 72 (44.7) a,b | 69 (65.7) a | 73 (60.8) b | 0.001 | 214 (55.4) |
| Birth weight, g, mean (SD) | 3290.1 (374.3) | 3257.1 (431.4) | 3246.7 (449.6) | 0.656 | 3267.6 (413.9) |
| Weight at baseline, g, mean (SD) | 3248.8 (378.3) | 3198.5 (409.8) | 3171.0 (430.9) | 0.263 | 3210.9 (404.2) |
| Length at baseline, cm, mean (SD) | 50.2 (2.0) a | 49.5 (1.8) a | 49.8 (2.0) | 0.029 | 49.9 (2.0) |
| Head circumference, cm, mean (SD) | 34.4 (1.2) | 34.1 (1.1) | 34.1 (1.1) | 0.103 | 34.2 (1.2) |
| Gender, female, n (%) | 77 (47.8) | 47 (44.8) | 55 (45.8) | 0.878 | 179 (46.4) |
| Mother’s characteristics | |||||
| Age, years, mean (SD) | 32.9 (4.7) a,b | 31.3 (4.8) a | 31.4 (5.4) b | 0.010 | 32.0 (5.0) |
| Educational level | |||||
| ≤14 years, n (%) | 44 (27.3) b | 43 (41.0) | 52 (43.3) b | 0.010 | 139 (36.0) |
| >14 years, n (%) | 117 (72.7) b | 62 (59.0) | 68 (56.7) b | 247 (64.0) | |
| Mother smoking during pregnancy, n (%) | 10 (6.2) b | 10 (9.5) | 18 (15.0) b | 0.050 | 38 (9.8) |
| Mother smoking at baseline, n (%) | 17 (10.6) b | 20 (19.0) | 29 (24.2) b | 0.009 | 66 (17.1) |
| Father’s characteristics | |||||
| Age, years, mean (SD) | 35.5 (5.5) | 34.4 (6.0) | 34.1 (5.7) | 0.099 | 34.8 (5.7) |
| Educational level | |||||
| ≤14 years, n (%) | 64 (39.8) b | 53 (51.0) | 67 (55.8) b | 0.021 | 184 (47.8) |
| >14 years, n (%) | 97 (60.2) b | 52 (49.0) | 53 (44.2) b | 201 (52.2) | |
| Father smoking at baseline, n (%) | 61 (37.9) | 55 (52.4) | 54 (45.0) | 0.065 | 170 (44.0) |
| Family characteristics | |||||
| Family members at home, median, IQR | 3.0 (1.0) | 3.0 (1.0) | 3.5 (1.0) | 0.821 | 3.0 (1.0) |
| Urban residence, n (%) | 150 (93.2) | 96 (91.4) | 102 (85.7) | 0.103 | 348 (90.4) |
| Presence of pets indoors at home, n (%) | 29 (18.0) | 25 (23.8) | 28 (23.3) | 0.699 | 82 (21.2) |
| Medical history | |||||
| Family history of: | |||||
| Allergic asthma, n (%) | 53 (32.9) | 25 (23.8) | 30 (25.0) | 0.184 | 108 (28.0) |
| Rhinitis, n (%) | 96 (59.6) | 52 (49.5) | 59 (49.2) | 0.135 | 207 (53.6) |
| Atopic dermatitis, n (%) | 59 (36.6) | 26 (24.8) | 34 (28.3) | 0.095 | 119 (30.8) |
| Urticaria, n (%) | 28 (17.4) | 15 (14.3) | 21 (17.5) | 0.760 | 64 (16.6) |
| Food allergy, n (%) | 47 (29.2) | 31 (29.5) | 33 (27.5) | 0.934 | 111 (28.8) |
| Occurrence of early life infections in infants | |||||
| No infections, n (%) | 126 (78.3) a | 63 (60.0) a | 79 (65.8) | 0.005 | 368 (69.4) |
| Before 1st month, n (%) | 6 (3.7) | 2 (1.9) | 6 (5.0) | 14 (3.6) | |
| After 1st month, n (%) | 29 (18.0) a | 40 (38.1) a | 35 (29.2) | 104 (26.9) |
| Time-Point of Evaluation (ITT Analysis Dataset) | Time Effect (4-Month Change) | Time Effect (6-Month Change) | |||
|---|---|---|---|---|---|
| Baseline | Visit 2 (4 Months) | Visit 3 (6 Months) | |||
| Mean (SEM) | Mean (SEM) | Mean (SEM) | Mean Change (95% CI) | Mean Change (95% CI) | |
| Body weight (kg) | |||||
| EBF group (n = 160) | 3.23 (0.008) a,b | 6.70 (0.054) | 7.67 (0.067) | 3.47 (3.36; 3.57) | 4.43 (4.30; 4.57) |
| pHF group (n = 104) | 3.20 (0.009) a | 6.68 (0.065) | 7.66 (0.081) | 3.48 (3.35; 3.60) | 4.46 (4.30; 4.62) |
| SF group (n = 119) | 3.18 (0.009) b | 6.77 (0.060) | 7.87 (0.075) | 3.59 (3.47; 3.71) | 4.69 (4.54; 4.84) |
| Treatment effect (p-value) * | <0.001 | 0.489 | 0.073 | 0.260 | 0.029 |
| Length (cm) | |||||
| EBF group (n = 160) | 49.9 (0.12) | 63.2 (0.19) | 67.3 (0.22) | 13.2 (12.9; 13.6) | 17.4 (16.9; 17.8) |
| pHF group (n = 104) | 49.7 (0.14) | 63.6 (0.23) | 68.0 (0.26) | 13.9 (13.5; 14.3) | 18.3 (17.8; 18.8) |
| SF group (n = 119) | 49.9 (0.13) | 63.4 (0.21) | 67.7 (0.25) | 13.5 (13.1; 13.9) | 17.8 (17.3; 18.2) |
| Between-group effect (p-value) * | 0.408 | 0.321 | 0.124 | 0.055 | 0.013 |
| Body Mass Index (Kg/m2) | |||||
| EBF group (n = 160) | 12.9 (0.07) | 16.8 (0.12) | 16.9 (0.14) | 3.8 (3.6; 4.1) | 4.0 (3.7; 4.3) |
| pHF group (n = 104) | 12.9 (0.08) | 16.5 (0.15) | 16.6 (0.17) c | 3.5 (3.2; 3.9) | 3.7 (3.3; 4.0) |
| SF group (n = 119) | 12.7 (0.07) | 16.8 (0.14) | 17.2 (0.16) c | 4.1 (3.8; 4.4) | 4.4 (4.1; 4.8) |
| Between-group effect (p-value) * | 0.053 | 0.136 | 0.039 | 0.029 | 0.004 |
| Head Circumference (cm) | |||||
| EBF group (n = 160) | 34.3 (0.08) | 41.3 (0.10) | 42.9 (0.11) | 7.0 (6.8; 7.2) | 8.7 (8.5; 8.9) |
| pHF group (n = 104) | 34.1 (0.09) | 41.1 (0.12) | 42.9 (0.13) | 7.0 (6.8; 7.2) | 8.8 (8.5; 9.0) |
| SF group (n = 119) | 34.1 (0.09) | 41.3 (0.11) | 43.0 (0.12) | 7.2 (7.0; 7.4) | 8.9 (8.7; 9.1) |
| Between-group effect (p-value) * | 0.316 | 0.384 | 0.845 | 0.249 | 0.247 |
| Weight-for-age z-score | |||||
| EBF group (n = 160) | −0.15 (0.02) a,b | −0.17 (0.09) | −0.09 (0.08) b | −0.02 (−0.16; 0.12) | 0.06 (−0.09; 0.22) |
| pHF group (n = 104) | −0.23 (0.02) a | −0.18 (0.08) | −0.08 (0.09) c | 0.05 (−0.12; 0.22) | 0.15 (−0.03; 0.33) |
| SF group (n = 119) | −0.26 (0.02) b | −0.05 (0.08) | 0.17 (0.08) b,c | 0.21 (0.06; 0.37) | 0.43 (0.26; 0.60) |
| Treatment effect (p-value) * | 0.001 | 0.409 | 0.048 | 0.094 | 0.006 |
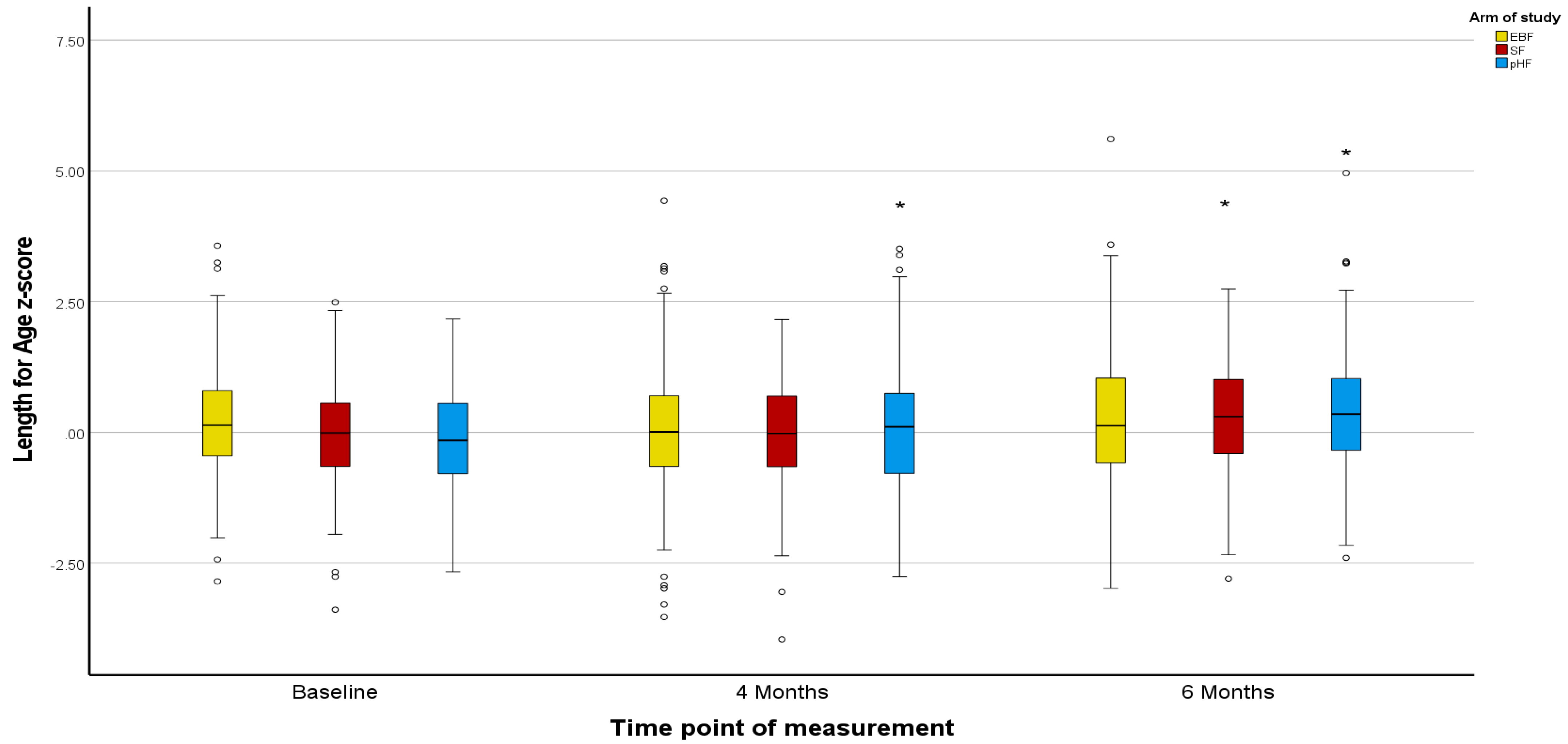
| Length-for-age-z-score | |||||
| EBF group (n = 160) | 0.04 (0.06) | −0.05 (0.09) | 0.15 (0.10) | −0.09 (−0.26; 0.08) | 0.11 (−0.08; 0.30) |
| pHF group (n = 104) | −0.08 (0.08) | 0.19 (0.11) | 0.49 (0.12) | 0.27 (0.07; 0.47) | 0.57 (0.34; 0.79) |
| SF group (n = 119) | 0.03 (0.07) | 0.08 (0.10) | 0.36 (0.11) | 0.06 (−0.13; 0.25) | 0.34 (0.12; 0.55) |
| Between-group effect (p-value) * | 0.448 | 0.256 | 0.099 | 0.033 | 0.007 |
| Body Mass Index-for age z-score | |||||
| EBF group (n = 160) | −0.37 (0.05) | −0.18 (0.08) | −0.23 (0.10) | 0.19 (0.002; 0.37) | 0.14 (−0.07; 0.35) |
| pHF group (n = 104) | −0.39 (0.06) | −0.37 (0.10) | −0.46 (0.12)c | 0.02 (−0.20; 0.24) | −0.07 (−0.32; 0.18) |
| SF group (n = 119) | −0.55 (0.06) | −0.13 (0.09) | −0.05 (0.11)c | 0.43 (0.22; 0.63) | 0.50 (0.26; 0.73) |
| Between-group effect (p-value) * | 0.052 | 0.171 | 0.041 | 0.026 | 0.003 |
| Treatment Arms | RR1 (95% CI) (PHF/ExcBF) | p-Value1 | RR2 (95% CI) (SF/ExcBF) | p-Value2 | p-Value3 | |||
|---|---|---|---|---|---|---|---|---|
| EBF | pHF | SF | ||||||
| Model 1 | (N = 220) | (N = 160) | (N = 171) | |||||
| AD, n (%) | 38 (17.3) | 17 (10.6) | 32 (18.7) | 0.62 (0.36, 1.05) | 0.064 | 1.08 (0.71, 1.66) | 0.709 | 0.069 |
| CMPA, n (%) | 21 (9.5) | 8 (5.0) | 16 (9.4) | 0.52 (0.24, 1.15) | 0.086 | 0.98 (0.53, 1.82) | 0.953 | 0.154 |
| Model 2 | ||||||||
| FHAD (+) | (N = 75) | (N = 46) | (N = 44) | |||||
| AD, n (%) | 17 (22.7) | 3 (6.5) | 12 (27.3) | 0.29 (0.09, 0.93) | 0.007 | 1.20 (0.63, 2.28) | 0.576 | 0.003 |
| CMPA, n (%) | 12 (16.0) | 3 (6.5) | 7 (15.9) | 0.41 (0.12, 1.37) | 0.088 | 0.99 (0.42, 2.34) | 0.990 | 0.166 |
| FHAD (−) | (N = 145) | (N = 114) | (N = 127) | |||||
| AD, n (%) | 21 (14.5) | 14 (12.3) | 20 (15.7) | 0.85 (0.45, 1.59) | 0.628 | 1.08 (0.62, 1.91) | 0.769 | 0.751 |
| CMPA, n (%) | 9 (6.2) | 5 (4.4) | 9 (7.1) | 0.71 (0.24, 2.05) | 0.525 | 1.14 (0.47, 2.79) | 0.770 | 0.651 |
| Model 3 | ||||||||
| Lower % BM intake | (N = 0) | (N = 126) | (N = 150) | |||||
| AD, n (%) | N/A | 13 (10.3) | 28 (18.7) | N/A | N/A | N/A | N/A | N/A |
| CMPA, n (%) | N/A | 8 (6.3) | 15 (10.0) | N/A | N/A | N/A | N/A | N/A |
| Higher % BM intake | (N = 220) | (N = 34) | (N = 21) | |||||
| AD, n (%) | 38 (17.3) | 4 (11.8) | 4 (19.0) | 0.68 (0.26, 1.79) | 0.367 | 1.10 (0.44, 2.79) | 0.849 | 0.636 |
| CMPA, n (%) | 21 (9.5) | 0 (0.0) | 1 (4.8) | N/A | <0.001 | 0.50 (0.07, 3.53) | 0.347 | <0.001 |
| Treatment Arms | RR1 (95% CI) (PHF/ExcBF) | p-Value1 | RR2 (95% CI) (SF/ExcBF) | p-Value2 | p-Value3 | |||
|---|---|---|---|---|---|---|---|---|
| EBF | pHF | SF | ||||||
| Model 1 | (N = 161) | (N = 105) | (N = 120) | |||||
| AD, n (%) | 33 (19.9) | 12 (11.4) | 29 (24.2) | 0.58 (0.31, 1.07) | 0.066 | 1.22 (0.78, 1.89) | 0.371 | 0.031 |
| CMPA, n (%) | 21 (13.0) | 7 (6.7) | 14 (11.7) | 0.51 (0.23, 1.16) | 0.085 | 0.89 (0.48, 1.69) | 0.748 | 0.195 |
| Model 2 | ||||||||
| FHAD (+) | (N = 59) | (N = 26) | (N = 34) | |||||
| AD, n (%) | 14 (23.7) | 2 (7.7) | 10 (29.4) | 0.32 (0.08, 1.33) | 0.035 | 1.24 (0.62, 2.48) | 0.550 | 0.031 |
| CMPA, n (%) | 12 (20.3) | 3 (11.5) | 5 (14.7) | 0.57 (0.18, 1.84) | 0.285 | 0.72 (0.28, 1.88) | 0.484 | 0.539 |
| FHAD (−) | (N = 102) | (N = 79) | (N = 86) | |||||
| AD, n (%) | 18 (17.6) | 10 (12.7) | 19 (22.1) | 0.72 (0.35, 1.47) | 0.387 | 1.25 (0.70, 2.23) | 0.423 | 0.282 |
| CMPA, n (%) | 9 (8.8) | 4 (5.1) | 9 (10.5) | 0.57 (0.18, 1.80) | 0.336 | 1.19 (0.49, 2.85) | 0.685 | 0.390 |
| Model 3 | ||||||||
| Lower % BM intake | (N = 0) | (N = 74) | (N = 101) | |||||
| AD, n (%) | N/A | 9 (12.2) | 25 (24.8) | N/A | N/A | N/A | N/A | 0.032 |
| CMPA, n (%) | N/A | 7 (9.5) | 13 (12.9) | N/A | N/A | N/A | N/A | 0.499 |
| Higher % BM intake | (N = 161) | (N = 31) | (N = 19) | |||||
| AD, n (%) | 32 (19.9) | 3 (9.7) | 4 (21.1) | 0.49 (0.16, 1.49) | 0.106 | 1.06 (0.42, 2.67) | 0.905 | 0.253 |
| CMPA, n (%) | 21 (13.0) | 0 (0.0) | 1 (5.3) | N/A | <0.001 | 0.40 (0.06, 2.83) | 0.187 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boutsikou, T.; Sekkidou, M.; Karaglani, E.; Krepi, A.; Moschonis, G.; Nicolaou, N.; Iacovidou, N.; Pancheva, R.; Marinova-Achkar, M.; Popova, S.; et al. The Impact of Infant Feeding Regimen on Cow’s Milk Protein Allergy, Atopic Dermatitis and Growth in High-Risk Infants during the First 6 Months of Life: The Allergy Reduction Trial. Nutrients 2023, 15, 2622. https://doi.org/10.3390/nu15112622
Boutsikou T, Sekkidou M, Karaglani E, Krepi A, Moschonis G, Nicolaou N, Iacovidou N, Pancheva R, Marinova-Achkar M, Popova S, et al. The Impact of Infant Feeding Regimen on Cow’s Milk Protein Allergy, Atopic Dermatitis and Growth in High-Risk Infants during the First 6 Months of Life: The Allergy Reduction Trial. Nutrients. 2023; 15(11):2622. https://doi.org/10.3390/nu15112622
Chicago/Turabian StyleBoutsikou, Theodora, Mikaela Sekkidou, Eva Karaglani, Adamantia Krepi, George Moschonis, Nicolaos Nicolaou, Nicoletta Iacovidou, Rouzha Pancheva, Miglena Marinova-Achkar, Simoneta Popova, and et al. 2023. "The Impact of Infant Feeding Regimen on Cow’s Milk Protein Allergy, Atopic Dermatitis and Growth in High-Risk Infants during the First 6 Months of Life: The Allergy Reduction Trial" Nutrients 15, no. 11: 2622. https://doi.org/10.3390/nu15112622
APA StyleBoutsikou, T., Sekkidou, M., Karaglani, E., Krepi, A., Moschonis, G., Nicolaou, N., Iacovidou, N., Pancheva, R., Marinova-Achkar, M., Popova, S., Kapetanaki, A., Iliodromiti, Z., Papaevangelou, V., Sardeli, O., Papathoma, E., Schaafsma, A., Bos, R., Manios, Y., & Xepapadaki, P. (2023). The Impact of Infant Feeding Regimen on Cow’s Milk Protein Allergy, Atopic Dermatitis and Growth in High-Risk Infants during the First 6 Months of Life: The Allergy Reduction Trial. Nutrients, 15(11), 2622. https://doi.org/10.3390/nu15112622









