Abstract
Background: It is well established that older adults are at risk for malnutrition due to several social and non-social determinants, namely physiological, psychosocial, dietary and environmental determinants. The progression to malnutrition is often insidious and undetected. Thus, nutritional assessment should consider a complex web of factors that can impact nutritional status (NS). The primary objective of this study was to assess the NS of older adults attending senior centres (SCs) and to identify its predictors. Methods: This cross-sectional study enrolled a sample of community-dwelling older adults in Lisbon. NS was assessed using Mini Nutritional Assessment (MNA®). Malnutrition or malnutrition risk (recategorised into a single group) was predicted using binary logistic regression models, considering those participants classified as having a normal NS as the reference group. Data were collected through face-to-face interviews and anthropometric indices were measured according to Isak procedures. Results: A sample of 337 older adults, with an average age of 78.4 years old (range 66–99), mostly women (n = 210; 62.3%), were enrolled. Older adults at risk of malnutrition accounted for 40.7% of the sample. Being older (OR = 1.045, CI 95% [1.003–1.089], p = 0.037), having a worse perception of health status (OR = 3.395, CI 95% [1.182–9.746], p = 0.023), having or having had depression (OR = 5.138, CI 95% [2.869–9.201], p < 0.001), and not having or having had respiratory tract problems (OR = 0.477, CI 95% [0.246–0.925], p = 0.028) were independent predictors of malnutrition or malnutrition risk. An intermediate time of SC attendance was associated with a lower probability of malnutrition or risk (OR = 0.367, CI 95% [0.191–0.705], p = 0.003). Conclusions: NS among older adults has a multifactorial aetiology, with a strongly social component and is related to health circumstances. Further research is needed to timely identify and understand nutritional risk among this population.
1. Introduction
Population ageing is now a universal phenomenon [1] and women form the majority of older persons, as they currently outlive men by 4.8 years [2]. The population of older adults has been increasing rapidly worldwide as the proportion of people aged 60 and over has increased faster than any other population group due to greater average life expectancy and decreased fertility rates [3,4].
This phenomenon can be seen as a success in the history of public health policies and sociodemographic development, but it is also a societal challenge to adapt policies and programs more focused on identifying strategies to improve the quality of life (QoL), health status, and functional status of individuals in this age group, as well as their social participation and security [5,6]. Older adults present aspects that require a complex assessment with an analysis of risk factors. In addition to several age-related changes in the normal aging process which may affect NS, the literature has been consistent in pointing out multiple factors correlated with malnutrition in older adults such as social, environmental, and health-related factors. In the first instance, age-related changes include a decline in physiological function, sensory impairment such as diminished taste or olfactory dysfunction, delayed gastric emptying, and disturbed motility leading to the functional decline of the gastrointestinal tract. This is combined with a decrease in gastrointestinal hormones, and with adverse changes in anorectic signalling (e.g., leptin, cholecystokinin, neuropeptide Y, peptide YY, orexin A) can lead to a loss of appetite and anorexia of aging, and consequently predispose elders to having insufficient daily nutrient intake, with deleterious outcomes in NS and functionality: weight loss, loss of muscle mass and strength (i.e., sarcopenia), and the frailty syndrome [7,8]. Additionally, NS is affected by multiple interdependent factors, such as lifestyle, loneliness, isolation, marital status, educational level, socioeconomic level, and place of residence [7,9,10,11]. Moreover, sex can impact the risk of malnutrition. Alzahrani et al. recognized that female sex was a significant predictor for malnutrition, since elderly women seem to suffer more often from a lack of appetite and consequent weight loss when compared to their male counterparts [12].
Imbalanced NS presents a huge clinical significance as it adversely affects the health and QoL of older adults, as well as overall healthcare costs. In fact, the consequences of malnutrition have serious implications for clinical and social outcomes, for recovery from disease, and are associated with increased morbidity and mortality both in acute and chronic disease [13].
NS also impairs wound healing and resistance to infection, as it predisposes older adults to wound healing disorders and consequently to chronic wounds which are a great burden as they are associated with decreased QoL, and furthermore result in higher expenditure in the healthcare setting [5,7,11].
The literature highlights that the impact of poor NS is greater in older than in younger adults and occurs to a greater extent, but also that recovery is slower. Malnourished older adults are clearly at higher risk, which in turn greatly compromises their health status, cognitive function, and functionality. In line with this, the assessment of NS should consider several factors, such as the physiological changes of aging and its multifactorial causes, namely social isolation, loneliness, and chronicity of diseases [14].
Despite the growing research interest on NS in older adults, less is known about the elderly living in the community, as they are the group that need health care and social support services the most [11], namely SC. In fact, older adults have poverty rates that are clearly higher than those of the overall population [15], so it is not surprising that elderly people with low incomes are usually the attendees of SCs [16]. SCs are committed to serving poor elderly and minority individuals [16], and are, by definition, places that promote the physical and mental health of community-dwelling elders by providing several services, such as serving lunches, providing a critical community need to seniors who are still active but have limited financial means to make their own lunches, and prefer companionship while eating. Moreover, this setting provides services that satisfy basic needs and psychosocial support, and it promotes socialisation and the occupation of free time, interpersonal relationships, and socio-cultural entertainment in order to avoid isolation. An SC provides a set of services that contribute to the maintenance of the elderly in their social and family environment. In addition, services involve hygiene care, the treatment of clothes, and the service of adapted transport or accompanying services. It is intended, therefore, to have a diversified range of proximity services, allowing the citizen to remain there as long as possible living their usual way of life, thus delaying institutionalization. The motivations to request support from the SC are varied. According to Benet [17], reasons related to health come first when deciding to whether to attend this social facility. Therefore, we conducted this study to evaluate the NS of older adults attending SCs, and to identify its predictors.
2. Materials and Methods
2.1. Participants and Study Design
Data were collected from September 2015 to February 2016. This is a cross-sectional and observational study conducted in a sample of older adults (aged 65 years or higher) attending SCs in Lisbon.
In order to select the sample, Carta Social, an online tool describing social equipment in Portugal with financial support from the Ministry of Social Affairs, was used. The inclusion criteria applied for SCs were those belonging to the municipality of Lisbon, and having the capacity for 50 or more attendees. A total of 241 SCs were identified in Lisbon and 54 SCs met the criteria (Figure 1). These SCs were invited to participate by telephone and/or by e-mail, and from those 7 SCs accepted to participate in this study, with a total of 491 attendees. From these, 400 met the criteria and 63 refused to participate. The sample encompassed 337 participants (Figure 1).
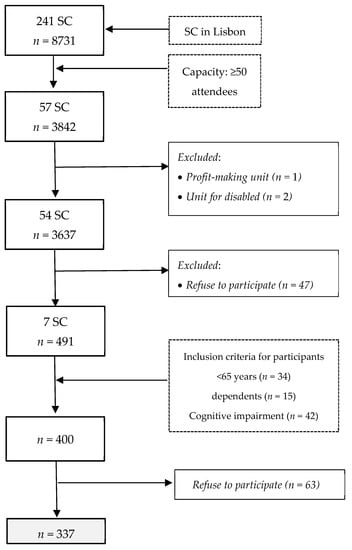
Figure 1.
Study design and participants.
The study included participants who met the following criteria: living in the community, being an SC attendee, being 65 years or older, being autonomous in daily living activities, and agreeing to participate in the study through written informed consent. Exclusion criteria were older adults with cognitive impairment that prevented them from understanding and/or answering the questionnaires, or who did not agree to participate in the study. Potential participants were contacted at the SC they were attending, and data were collected through face-to-face interviews in SC facilities by one trained nutritionist.
This investigation was conducted in accordance with the Declaration of Helsinki (World Medical Association, 1983) and approved by the ICBAS-UP Ethics Committee. All ethical issues inherent to the investigative process were safeguarded, and the informed consent of all was obtained.
Participants were asked sociodemographic and contextual questions, which included sex, age, marital status, education level (number of years spent in school), and number of children. It was also intended to contextualize the institution’s support scheme, duration of the support, and the services they enjoyed, as well as the main reason for attending SCs.
Health-related data were self-reported: self-reported chronic health problems and multimorbidity, defined as the coexistence of at least two self-reported chronic diseases and alcohol and tobacco consumption; daily medication and the consumption of nutritional/dietary supplements, and restrictions on their use due to economic constraints in the last 12 months at the time of the questionnaire. Finally, participants were asked to classify their health status, with the aim to know their perception about their particular health situation. The scale used (Likert type) presented five possibilities of response: very good, good, fair, poor, and very poor.
2.2. Assessment Instruments
To evaluate the social context of the sample, the Gijon Socio-Family Situation Assessment Scale was applied, due to its pertinence and adequacy in order to verify the family situation of the participants and identify the profile of social vulnerability [18].
Mini Nutritional Assessment, commonly referred to as MNA®, is a validated tool for assessing the NS of the older adult population [19]. Although there is an abbreviated version, the full form was chosen, as it was considered the most appropriate. It is a questionnaire with a total of 18 items, which include anthropometric assessment, food questionnaire, global assessment, and self-assessment.
All anthropometric measurements were performed following the standard methods (ISAK) [20]. Body weight, height, the calculation and classification of BMI, middle upper arm (MUAC), waist (WC), and calf circumferences (CC) were included.
Based on the experience of the phenomenon of Food Insecurity (FI), the Food Insecurity Scale (FIES) is already used in several countries to provide reliable information about the ability of individuals and families to access food. The FIES scale contains 8 closed questions, with the possibility of answering yes, no, does not know, and prefers not to answer/refuse, referring to the last 12 months [21].
2.3. Cognitive Status
General cognitive function was assessed by Mini-Mental State Examination (MMSE). The most often used screening tool for providing an overall measure of cognitive impairment in clinical, research, and community settings [22], it includes tests of orientation, concentration, attention, verbal memory, naming, and visuospatial skills. The cut-off was set according to the educational level of the participant.
2.4. Statistical Analysis
The statistical analysis was performed using SPSS® Statistical Package for Social Sciences (IMB®, version 25.0 for Windows).
Basic descriptive data were used to characterize the participants in the study and all variables were assessed for normality. For qualitative variables, absolute frequencies (n) and relative frequencies (%) were calculated, while for quantitative variables, the minimum value, maximum value, mean, and standard deviation (SD) were determined as descriptive measures.
Binary logistic regression models (uni- and multivariate) were used to predict malnutrition or risk of malnutrition (assessed using the MNA® and recategorised into a single group), considering participants classified as having a normal NS as the reference group. The independent variables included in the models were sex, age, Gijon’s Socio-Family Situation Assessment score, tobacco or alcohol use, self-perception of health, NCDs, time of SC attendance, reasons for attending the SC, and FI. Self-perception of health was included using good and very good as the reference category, and also combining poor and very poor in one single category. As for FI, food security was defined as the reference category, and moderate and severe FI were also combined into one category. The multivariate regression was adjusted for all variables in the model.
All inferential analyses were performed with 95% confidence.
3. Results
3.1. Sample Characterization
This study included a total of 337 older adults, with an average age of 78.4 (SD = 7.1 years), between 66 and 99 years, mostly female (62.3%). Females were presented in the majority in all age groups (Table 1). The prevalence of multimorbidity in the total sample was high (96.4%). The average number of self-reported noncommunicable diseases (NCDs) was 4.6 (SD = 1.8). Both sexes presented a high average number of diseases (Table 2). Arterial hypertension (HTN) represented the most predominant pathology (73.9%), and almost the whole sample took daily medication (99.4%) and more than three different medications per day (96.1%).

Table 1.
Distribution of age groups by sex, marital status, and education.

Table 2.
Multimorbidity and NCDs.
Most of the participants attended the SC due to a lack of money, loneliness, and conviviality. Almost half of the sample (45.4%) benefited from this support for between 1 and 4 years, and one in ten (10.4%) had been SC attendees for more than 10 years. More than one third of the participants (34.7%) presented high social risk and 70% of the sample presented some level of FI.
Regarding NS, participants at risk of malnutrition represented 40.7% of the sample (Table 3).

Table 3.
Nutritional Status (MNA), by sex.
According to Table 4, there are some variables that have a statistically significant relationship (p < 0.05) with NS.

Table 4.
Predictors of malnutrition and nutritional risk.
3.2. Clinical Factors
When considered separately, the following are predictors of malnutrition or the risk of malnutrition: a worse self-perception of health status (OR = 3.044, CI 95% [1.152–8.048]; p = 0.025), having or having had urinary incontinence (OR = 1.646, CI 95% [1.009–2.684]; p = 0.046) or depression (OR = 3.594, CI 95% [2.144–6.027], p < 0.001).
According to the adjusted logistic regression model, being older (OR = 1.045, CI 95% [1.003–1.089], having a worse self-perception of health status (OR = 3.395, CI 95% [1.182–9.746], p = 0.023), having or having had depression (OR = 5.138, CI 95% [2.869–9.201], p < 0.001), and not having or having had respiratory tract problems (OR = 0.477, CI 95% [0.246–0.925], p = 0.028) were independent predictors of malnutrition or risk of malnutrition.
3.3. Social Factors
In turn, a time of SC attendance equal to or greater than one year but less than five years is associated with lower odds of malnutrition, or risk of malnutrition (OR = 0.506, CI 95% [0.291–0.881], p = 0.016).
According to the adjusted model, intermediate attendance times of SC were associated with lower odds of malnutrition or risk (OR = 0.367, CI 95% [0.191–0.705], p = 0.003).
4. Discussion
It is universal that women have a higher average life expectancy compared to men [23]. Although the mean age between men and women in this study was similar, there was a predominance of female participants. The literature highlights remarkable sex differences in life expectancy and mortality, indicating that human longevity seems to be strongly influenced by sex [23,24].
In fact, the aging process is qualitatively different between men and women, since they differ not only biologically (including sex hormones and genetics), but also regarding lifestyles, where nutrition is, along with smoking, physical activity, type of work and education, one of the factors underpinning the sex difference in longevity and aging. Moreover, coping capacity with stressful events (e.g., serving as caregivers or spousal bereavement) also plays a role in this complex lifelong interaction between biological and non-biological factors, which impacts health, the propensity to diseases, and also disabilities later in life [24].
The marital status with the highest representation in the sample was the married state, in which women predominate. Additionally, the majority of widowed participants were women, in line with studies conducted by other authors [25,26], since women live longer as widows than men [26]. It is said that aging in the feminine is more solitary and less conjugal [27]. In terms of education level, we found a considerable prevalence of illiteracy and an average number of years of low education, which would be expected given the low level of education that characterizes this age group in Portugal [25].
This sample seems to be a group of older adults with a deterioration of their state of health, as is observed regarding the presence of numerous chronic diseases, reflected in their multimorbidity (96.4%), as well as in polypharmacy, since almost all participants took more than three different medications per day. Other authors also reported that more than 90% of the participants took medications daily [28]. The treatment of NCDs often includes long-term pharmacotherapeutic use [29]. The literature indicates that these elders present a higher risk of nutritional changes, either due to the underlying disease and comorbidities, or due to the therapeutic intervention that the clinical condition requires. In fact, the NS of the elderly interferes with the pharmacokinetics and pharmacodynamics, potentiating side effects. Additionally, the taking of drugs can also conditionate NS [30,31]. Prescribing drugs from different pharmaceutical groups also increases the risk of drug interactions that may result in negative outcomes.
More than half of the sample had normal NS, while 40.7% were at risk of malnutrition and approximately 5% were malnourished. The latter value is in accordance with the literature, which estimates that, in the community, malnutrition values in the elderly are between 0.7% and 5.8% [29].
Older adults present different aspects, which require a broader assessment with the analysis of risk factors, such as the physiological changes of aging and the multifactorial causes of poor NS, which include social isolation, loneliness, chronicity of diseases, changes in psychological disorders, depression, and disabilities [14,32]. Thus, these results reinforce the importance of nutritional assessment in the comprehensive assessment of the elderly (also known as Comprehensive Geriatric Assessment—CGA) [33], and intensify the need for nutritionists in the multidisciplinary teams that accompany the elderly, mainly for a rigorous and precise assessment of NS and an individualized nutritional prescription.
The predictors of NS are varied, and include clinical status and socioeconomic parameters [11,34]. It is well stablished that older adults are more vulnerable to malnutrition than the young, due to the presence of several chronic diseases [35,36], for which age is the greatest risk factor [37]. In fact, malnutrition is widespread among older adults. Due the rapid increase in this age group and their high risk of dependence, identifying factors that allow them to maintain a healthier and more independent life is of prime interest [37]. Age is recognized as one of the main risk factors for NS in the elderly [36,38], and, in this research, age constitutes an independent predictor of malnutrition or risk. The odds of having malnutrition or risk increased by 1.045 per year in the sample.
In addition to the numerous age-related changes during the normal aging process that can affect NS [39], the susceptibility of the elderly is related to their vulnerability and various disabilities [40], presence of chronic diseases [41], low income, and need for assistance with DLAs [36]. The set of these factors is often intertwined with the presence of FI, which negatively affects health, QoL and NS [35], as well as mental health [42,43], as it leads to depression and contributes to a more rapid decline in cognitive function [27,44,45]. Thus, older adults are at increased risk of malnutrition due to a variety of psychological, physiological and social factors [46]. The existence of at least one non-communicable chronic disease (NCD) increases from the age of 65 [47]. In fact, the literature highlights the high prevalence of multiple chronic diseases among the elderly [15,48,49]. With regard to self-reported chronic diseases and lifestyles, it was found that the most representative diseases in the sample were arterial hypertension (AHT), degenerative joint diseases, and hypercholesterolemia. These data are corroborated in national studies: since 1998, AHT and back pain have been presented as the most frequent chronic diseases among the elderly population surveyed [46]. Additionally, the National Health Survey 2005/2006 [48] highlighted that the elderly were the population group with the highest prevalence of chronic diseases, in particular HTN, and with situations of temporary or permanent disability, such as rheumatic disease, chronic pain, and diabetes, which registered a higher prevalence among the elderly, as observed among the participants of this study. In 2014, the most prevalent chronic diseases among the Portuguese elderly remained unchanged. Likewise, recent data from the national study Epidoc, with elderly people, corroborate the results of the present investigation [48].
Self-reported health status is a predictor of morbidity and mortality in older adults [50]. The association between poorer self-perceived health status and higher risk of malnutrition has been reported [51]. In the present investigation, a better self-perceived state of health decreased nutritional risk and malnutrition. The same was corroborated by Simsek et al. [11].
Regarding health variables, not having respiratory tract diseases decreases the probability of these older adults having a risk of malnutrition, in line with other studies; respiratory diseases, namely pulmonary emphysema, are predictors for malnutrition in the elderly population [52]. Urinary incontinence proved to be a predictor of malnutrition or risk when considered alone, but loses statistical significance in the adjusted models, contrary to other studies [53].
Nutrition may play a protective role against several health conditions, including cognitive decline [54]. In fact, depression, very prevalent in elders [55], has been reported as a major determinant for malnutrition in the elderly [56]. In agreement with the results of the present investigation, the elderly who reported depression were more likely to have malnutrition or to be at risk. Thus, depression is strongly associated with poor NS [57]. Additionally, depression is a predictor for FI [58], which in turn is an important risk factor in the elderly [59]. The loss of an active social life, and the deprivation of affection, so common in situations of loneliness, can induce a state of depression that can arise clinically as anorexia [34]. The elderly can perceive reality with a sense of futility and live with a passive attitude and disinterest. It should be noted that the first manifestation of depression is the lack of interest in food [50]. In the sample, depression is related to NS, being an independent predictor for malnutrition and the risk of malnutrition.
Participants who had been attending an SC for less than 5 years were 3.7 times less likely to have malnutrition or nutritional risk, being an independent factor. We can hypothesize that the SC contributes not only to guaranteeing the basic right to food—since the elderly may not be able to prepare balanced meals due to disabilities or lack of money—but also contributes to promoting social relationships with other attendees, thus reducing social isolation. Loneliness, social isolation, and other social aspects are important among elders.
Its impact on health and particularly on NS and the risk of this population is multifactorial [54,60]. Ramic and colleagues also explored the effect of loneliness on malnutrition in the elderly, concluding that loneliness was a strong predictor for the risk of malnutrition [61]. This condition can be explained by the negative effects on appetite and decreased nutrient intake due to mood and functional and cognitive decline [54], promoting an inability to buy, prepare, and make food, or even leading to the person forgetting to eat [34,54]. This disability creates a vicious cycle where malnutrition and functional and mental deterioration sustain and reinforce each other [34,50]. Thus, these elderly people should not eat their meals alone [54]. Active social participation is an important indicator of QoL in adulthood and overlaps with age-related losses and physical, mental, and social changes, serving as a protective factor against depression [62]. Having little social and material support can discourage the individual from spending time on buying healthier and also less expensive food options, which require preparation and some knowledge; so, social support positively influences healthy behaviours [63], as well as provides a “safety net” to which the elderly can turn whenever necessary. In the same vein, Sahyoun and Zhang (2005) reported that social interaction and food are positively associated with each other [62].
The reason “loneliness” for attending an SC was not shown to be a predictor in this sample. However, some literature on the association between social isolation and subjective loneliness and malnutrition in the elderly has shown a relationship between them, suggesting that social isolation and subjective loneliness are two independent risk factors for malnutrition in the elderly population [60]. Nevertheless, it seems pertinent to conclude that the SC can be a protective entity of the elderly who attend this social response. Another aspect that deserves discussion is the fact that the deterioration of the NS is closely related to lack of food intake, weight loss, disease, functional status, and stress [64], which is pointed out in the literature as a biopsychosocial factor for NS [52,65,66]. Both psychological stress and acute illness are threats to homeostasis [67], particularly acute disease is very catabolic and may promote unintentional weight loss and energy-protein malnutrition. Contrary to the literature revisited, in the present study, the insecure elderly were not more likely to be malnourished. These results do not reinforce the results found in other investigations [35,68]. Still, FI and malnutrition in the elderly should be analysed together, as economic deprivation is related to FI and also to malnutrition. Social factors such as poverty, loneliness, and low education level can also affect food availability and consequently the NS [21,60]. This binomial is complex, bidirectional, and self-perpetuating, as FI leads to a worse state of health and worse NS, which in turn leads to an increase in the severity of the FI, and thus the cycle continues [68,69,70,71]. The problem of FI is distinct in this age group and is assumed to be a risk factor for malnutrition in the elderly [36]. The fact that the whole sample includes users of SCs who eat in these institutions may explain this result, meaning that properly oriented SCs may have a crucial and protective role in the NS of these elders. Limited access to food contributes to a further deterioration in health status [46], and puts the elderly at nutritional risk [42].
5. Limitations and Strengths
Some limitations should be considered. The cross-sectional design of the study does not allow causality inference. The clinical data (namely NCDs) were self-reported and may therefore be biased, as there might be an underestimation of some health conditions due to a lack of memory, highly prevalent in older adults. Additionally, the sample encompassed older adults living in the community in a specific Portuguese region. Thereby, more studies with similar methos should be performed among other populations to verify the possibility of their generalization. Another limitation concerns the exclusion criteria of participants with cognitive impairment that may have biased some results, since many studies reported a relationship between cognitive impairment and a higher prevalence of malnutrition or risk of malnutrition.
However, the present study was strengthened using appropriate methodology and validated tools. There was only one interviewer for the entire sample, which prevented the existence of interindividual variations.
To search for malnutrition-related features (as assessed by the MNA items) and identify predictors based on sociodemographic, clinical data, and anthropometric measurements can provide crucial information for the development of direct and precise interventions, leading to overcoming nutritional risk, and this may contribute to early assessment and intervention in this specific population.
6. Conclusions
In conclusion, this study indicates that older age, worse self-perception of health status, depression, and the absence of respiratory tract problems were independent factors of malnutrition or risk. An SC attendance time of up to 5 years was shown to be an independent predictor of the lower odds of having malnutrition or nutritional risk. Therefore, keeping the elderly integrated into society, participatory and active, satisfied with their health status and perceiving it as positive can be protective behaviours for maintaining NS, in which the SC seems to be a mediator. Due to the above, the results support the fact that NS in older adults has a multifactorial aetiology, with a strongly social component, and is related to health circumstances. From this point of view, the evaluation of the elderly should integrate a comprehensive approach and consider all the dimensions of the concept of health. Further studies are needed to explore and understand nutritional risk among this population. Early screening to identify nutritional risk factors may allow for timely multimodal intervention and thus better clinical outcomes.
Author Contributions
S.G.-A.: conceptualization, investigation, methodology and writing—original draft. R.P.: conceptualization, formal analysis, methodology and writing—review and editing. S.P.: conceptualization, methodology and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
This study was performed in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) and was approved by the ICBAS-UP Ethics Committee (approval number 167/2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All raw data will be available upon reasonable request to the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dalgaard, C.J.; Hansen, C.W.; Strulik, H. Physiological Aging around the World. PLoS ONE 2022, 17, e0268276. [Google Scholar] [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights; United Nations: New York, NY, USA, 2020.
- Bloom, D.E.; Chatterji, S.; Kowal, P.; Lloyd-sherlock, P.; Mckee, M.; Rechel, B.; Rosenberg, L.; Smith, J.P. Macroeconomic Implications of Population Ageing and Selected Policy Responses. Lancet 2015, 385, 649–657. [Google Scholar] [CrossRef]
- Kuczmarski, M.F.; Kuczmarski, R.J.; Najjar, M. Descriptive Anthropometric Reference Data for Older Americans. J. Am. Diet. Assoc. 2000, 100, 59–66. [Google Scholar] [CrossRef]
- Hong, S.A.; Kim, K. Factors Contributing to Participation in Food Assistance Programs in the Elderly Population. Nutr. Res. Pract. 2014, 8, 425–431. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015.
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef] [PubMed]
- Cereda, E.; Pedrolli, C.; Klersy, C.; Bonardi, C.; Quarleri, L.; Cappello, S.; Turri, A.; Rondanelli, M.; Caccialanza, R. Nutritional Status in Older Persons According to Healthcare Setting: A Systematic Review and Meta-Analysis of Prevalence Data Using MNA®. Clin. Nutr. 2016, 35, 1282–1290. [Google Scholar] [CrossRef] [PubMed]
- Besora-Moreno, M.; Llauradó, E.; Tarro, L.; Solà, R. Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2020, 12, 737. [Google Scholar] [CrossRef]
- Wellman, N.S.; Weddle, D.O.; Kranz, S.; Brain, C.T. Elder Insecurities: Poverty, Hunger, and Malnutrition. J. Am. Diet. Assoc. 1997, 97, S120–S122. [Google Scholar] [CrossRef]
- Simsek, H.; Meseri, R.; Sahin, S.; Ucku, R. Prevalence of Food Insecurity and Malnutrition, Factors Related to Malnutrition in the Elderly: A Community-Based, Cross-Sectional Study from Turkey. Eur. Geriatr. Med. 2013, 4, 226–230. [Google Scholar] [CrossRef]
- Alzahrani, S.H.; Abdelmoneim, I.; Sayed, E.; Alshamrani, S.M. Prevalence and Factors Associated with Geriatric Malnutrition in an Outpatient Clinic of a Teaching Hospital in Jeddah, Saudi Arabia. Ann. Saudi Med. 2016, 36, 346–351. [Google Scholar] [CrossRef]
- Blössner, M.; De Onis, M. Malnutrition: Quantifying the Health Impact at National and Local Levels; World Health Organization: Geneva, Switzerland, 2005; Volume 12.
- Virtuoso-Júnior, J.S.; Tribess, S.; Romo-Pérez, V.; Oliveira-Guerra, R. Factors Associated to Risk of Malnutrition amongst Elderly Women in Low-Income Communities. Colomb. Med. 2012, 43, 54–62. [Google Scholar] [CrossRef]
- INE. O Envelhecimento Portugal Situação Demográfica e Socio-Económica Pessoas Idosas. In Revista de Estudos Demográficos; Instituto Nacional de Estatística (INE): Lisboa, Portugal, 2002; pp. 186–208. [Google Scholar]
- Schneider, A.E.; Ralph, N.; Olson, C.; Flatley, A.-M.; Thorpe, L. Predictors of Senior Center Use among Older Adults in New York City Public Housing. J. Urban Health 2014, 91, 1033–1047. [Google Scholar] [CrossRef]
- Benet, A.S. Los Centros de Día Para Personas Mayores; Universitat de Lleida: Lleida, Spain, 2003. [Google Scholar]
- Cabrera González, D.; Menéndez Caicoya, A.; Fernández Sánchez, A.; Acebal García, V.; García González, J.; Díaz Palacios, E.; Salamea García, A. Evaluación de la fiabilidad y validez de una escala de valoración social en el anciano. Aten. Primaria 1999, 23, 434–440. [Google Scholar]
- Guigoz, Y. The Mini Nutritional Assessment (MNA(Registered Trademark)) Review of the Literature-What Does It Tell Us? J. Nutr. Health Aging 2006, 10, 466–485. [Google Scholar] [CrossRef]
- Olds, T.; Ridder, H.; de Arthur, D.S.; Marfell-Jones, M. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: London, UK, 2011; ISBN 0620362073. [Google Scholar]
- Ballard, T.J.; Kepple, A.W.; Cafiero, C. The Food Insecurity Experience Scale: Development of a Global Standard\rfor Monitoring Hunger Worldwide. In Technical Paper; FAO: Rome, Italy, 2013. [Google Scholar]
- Figuls, R.M.; Cosp, B.X.; Arevalo-Rodriguez, I.C.S. Mini-Mental State Examination (MMSE) for the Detection of Alzheimer’s Disease and Other Dementias in People with Mild Cognitive Impairment (MCI) (Review). Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Amarya, S.; Singh, K.; Sabharwal, M. Changes during Aging and Their Association with Malnutrition. J. Clin. Gerontol. Geriatr. 2015, 6, 78–84. [Google Scholar] [CrossRef]
- Ostan, R.; Monti, D.; Gueresi, P.; Bussolotto, M.; Franceschi, C.; Baggio, G. Gender, Aging and Longevity in Humans: An Update of an Intriguing/Neglected Scenario Paving the Way to a Gender-Specific Medicine. Clin. Sci. 2016, 130, 1711–1725. [Google Scholar] [CrossRef]
- Mota-Pinto, A.; Rodrigues, V.; Botelho, A.; Veríssimo, M.T.; Morais, A.; Alves, C.; Rosa, M.S.; Resende de Oliveira, C. A Socio-Demographic Study of Aging in the Portuguese Population: The EPEPP Study. Arch. Gerontoloy Geriatr. 2010, 52, 304–308. [Google Scholar] [CrossRef]
- Gualtieri, M.C.; Donley, A.M. Senior Hunger: The Importance of Quality Assessment Tools in Determining Need. J. Appl. Soc. Sci. 2016, 10, 8–21. [Google Scholar] [CrossRef]
- Villaverde Cabral, M.; Ferreira, P.M.; da Silva, P.A.; Jerónimo, P.; Marques, T. Processos de Envelhecimento Em Portugal. Usos Do Tempo, Redes Sociais e Condições de Vida; Fundação Francisco Manuel dos Santos: Lisboa, Portugal, 2013; ISBN 9789898662002. [Google Scholar]
- Zhou, J.; Wang, M.; Wang, H.; Chi, Q. Comparison of Two Nutrition Assessment Tools in Surgical Elderly Inpatients in Northern China. Nutr. J. 2015, 14, 68. [Google Scholar] [CrossRef]
- Morley, J.E. Assessment of Malnutrition in Older Persons: A Focus on the Mini Nutritional Assessment. J. Nutr. Health Aging 2011, 15, 87–90. [Google Scholar] [CrossRef]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-Based Recommendations for Optimal Dietary Protein Intake in Older People: A Position Paper from the Prot-Age Study Group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Paddon-Jones, D.; Rasmussen, B.B. Dietary Protein Recommendations and the Prevention of Sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 2009, 12, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Secher, M.; Soto, M.E.; Villars, H.; van Kan, G.A.; Vellas, B.; Secher, M.; Soto, M.E. The Mini Nutritional Assessment (MNA) after 20 Years of Research and Clinical Practice. Rev. Clin. Gerontol. 2007, 17, 293–310. [Google Scholar] [CrossRef]
- Lee, J.S.; Frongillo, E.A. Nutritional and Health Consequences Are Associated with Food Insecurity. J. Nutr. 2001, 131, 1503–1509. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Scardella, P.; Piombo, L.; Neri, B.; Asprino, R.; Proietti, A.R.; Carcaterra, S.; Cava, E.; Cataldi, S.; Cucinotta, D.; et al. Malnutrition in Elderly: Social and Economic Determinants. J. Nutr. Health Aging 2013, 17, 9–15. [Google Scholar] [CrossRef]
- Collerton, J.; Barrass, K.; Bond, J.; Eccles, M.; Jagger, C.; James, O.; Martin-Ruiz, C.; Robinson, L.; Von Zglinicki, T.; Kirkwood, T. The Newcastle 85+ Study: Biological, Clinical and Psychosocial Factors Associated with Healthy Ageing: Study Protocol. BMC Geriatr. 2007, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Meng, H.; Dong, B. Factors Associated with Poor Nutritional Status among the Oldest-Old. Clin. Nutr. 2012, 31, 922–926. [Google Scholar] [CrossRef]
- Forster, S.; Gariballa, S. Age as a Determinant of Nutritional Status: A Cross Sectional Study. Nutr. J. 2005, 4, 28. [Google Scholar] [CrossRef]
- Ahmed, T.; Haboubi, N. Assessment and Management of Nutrition in Older People and Its Importance to Health. Clin. Interv. Aging 2010, 5, 207–216. [Google Scholar]
- Druml, C.; Ballmer, P.E.; Druml, W.; Oehmichen, F.; Shenkin, A.; Singer, P.; Soeters, P.; Weimann, A.; Bischoff, S.C. ESPEN Guideline on Ethical Aspects of Artificial Nutrition and Hydration. Clin. Nutr. 2016, 35, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.T.; Gallo, W.T.; Giunta, N.; Canavan, M.E.; Parikh, N.S.; Fahs, M.C. Linking Neighborhood Characteristics to Food Insecurity in Older Adults: The Role of Perceived Safety, Social Cohesion, and Walkability. J. Urban Health 2012, 89, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Scott, T.; Falcon, L.M.; Wilde, P.E.; Tucker, K.L. Food Insecurity and Cognitive Function in Puerto Rican Adults. Am. J. Clin. Nutr. 2009, 89, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Barrubés, L.; Babio, N.; Becerra-Tomás, N.; Rosique-Esteban, N.; Salas-Salvadó, J. Association Between Dairy Product Consumption and Colorectal Cancer Risk in Adults: A Systematic Review and Meta-Analysis of Epidemiologic Studies. Adv. Nutr. 2019, 10 (Suppl. S2), S190–S211. [Google Scholar] [CrossRef]
- Frith, E.; Loprinzi, P.D. Food Insecurity and Cognitive Function in Older Adults: Brief Report. Clin. Nutr. 2017, 37, 1765–1768. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.C.; Scott, T.; Wilde, P.; Li, Y.-G.; Tucker, K.L.; Gao, X. Food Insecurity Is Associated with Subsequent Cognitive Decline in the Boston Puerto Rican Health Study. J. Nutr. 2016, 146, 1740–1745. [Google Scholar] [CrossRef]
- Clegg, M.E.; Williams, E.A. Optimizing Nutrition in Older People. Maturitas 2018, 112, 34–38. [Google Scholar] [CrossRef]
- Wolff, J.L.; Starfield, B.; Anderson, G. Prevalence, Expenditures, and Complications of Multiple Chronic Conditions in the Elderly. Arch. Intern. Med. 2002, 162, 2269. [Google Scholar] [CrossRef] [PubMed]
- Arli, S.K.; Bakan, A.B.; Varol, E.; Aslan, G. Investigation of Pain and Life Satisfaction in Older Adults. Geriatr. Gerontol. Int. 2018, 18, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, A.M.; Gregório, M.J.; Sousa, R.D.; Dias, S.S. Challenges of Ageing in Portugal: Data from the EpiDoC Cohort Os Desafios Do Envelhecimento Em Portugal: Dados Da Coorte EpiDoC. Rev. Científica Da Ordem Dos Médicos 2018, 31, 80–93. [Google Scholar]
- Instituto Nacional, Saúde Doutor Ricardo Jorge. Inquérito Nacional de Saúde 2005/2006; Instituto Nacional de Estatística: Lisbon, Portugal, 2009; Volume 330. [CrossRef]
- Van Bokhorst-de van der Schueren, M.A.E.; Lonterman-Monasch, S.; de Vries, O.J.; Danner, S.A.; Kramer, M.H.H.; Muller, M. Prevalence and Determinants for Malnutrition in Geriatric Outpatients. Clin. Nutr. 2013, 32, 1007–1011. [Google Scholar] [CrossRef]
- Kokui, R.; Turkson, D.; Ngounda, J.; Nel, R.; Walsh, C.M. The Nutritional Status of Community-Dwelling Elderly in Lesotho and Factors Associated with Malnutrition. Nutr. Health 2022. [Google Scholar] [CrossRef]
- Eskelinen, K.; Hartikainen, S.; Nykänen, I. Is Loneliness Associated with Malnutrition in Older People? Int. J. Gerontol. 2015, 10, 43–45. [Google Scholar] [CrossRef]
- Wilkins, V.M.; Kiosses, D.; Ravdin, L.D. Late-Life Depression with Comorbid Cognitive Impairment and Disability: Nonpharmacological Interventions. Clin. Interv. Aging 2010, 5, 323–331. [Google Scholar] [PubMed]
- Feldblum, I.; German, L.; Castel, H.; Harman-Boehm, I.; Bilenko, N.; Eisinger, M.; Fraser, D.; Shahar, D.R. Characteristics of Undernourished Older Medical Patients and the Identification of Predictors for Undernutrition Status. Nutr. J. 2007, 6, 37. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, I.; Charlton, K.E.; Esterhuizen, T.M.; Cassim, B. High Risk of Malnutrition Associated with Depressive Symptoms in Older South Africans Living in KwaZulu-Natal, South Africa: A Cross-Sectional Survey. J. Health Popul. Nutr. 2015, 33, 19. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.L.; Mawn, B.E. Predictors of Food Insecurity among Older Adults in the United States. Public Health Nurs. 2015, 32, 397–407. [Google Scholar] [CrossRef]
- Russell, J.C.; Flood, V.M.; Yeatman, H.; Wang, J.J.; Mitchell, P. Food Insecurity and Poor Diet Quality Are Associated with Reduced Quality of Life in Older Adults. Nutr. Diet. 2016, 73, 50–58. [Google Scholar] [CrossRef]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Social Isolation and Risk for Malnutrition among Older People. Geriatr. Gerontol. Int. 2017, 17, 286–294. [Google Scholar] [CrossRef]
- del Díaz-López, M.P.; Aguilar-Parra, J.M.; López-Liria, R.; Rocamora-Pérez, P.; Vargas-Muñoz, M.E.; Padilla-Góngora, D. Skills for Successful Ageing in the Elderly. Education, Well-Being and Health. Procedia Soc. Behav. Sci. 2017, 237, 986–991. [Google Scholar] [CrossRef]
- Ashe, K.M.; Lapane, K.L. Food Insecurity and Obesity: Exploring the Role of Social Support. J. Womens Health 2017, 27, 651–658. [Google Scholar] [CrossRef]
- Ramic, E.; Pranjic, N.; Batic-Mujanovic, O.; Karic, E.; Alibasic, E.; Alic, A. The Effect of Loneliness on Malnutrition in Elderly Population. Med. Arch. 2011, 65, 92–95. [Google Scholar]
- Sahyoun, N.R.; Zhang, X.L. Dietary Quality and Social Contact among a Nationally Representative Sample of the Older Adult Population in the United States. J. Nutr. Health Aging 2005, 9, 177–183. [Google Scholar]
- Oliveira, M.R.; Fogaça, K.C.; Leandro-Merhi, V.A. Nutritional Status and Functional Capacity of Hospitalized Elderly. Nutr. J. 2009, 8, 54. [Google Scholar] [CrossRef]
- Laraia, B.A.; Leak, T.M.; Tester, J.M.; Leung, C.W. Biobehavioral Factors That Shape Nutrition in Low-Income Populations: A Narrative Review. Am. J. Prev. Med. 2017, 52, S118–S126. [Google Scholar] [CrossRef] [PubMed]
- Stajkovic, S.; Aitken, E.; Holroyd-Leduc, J. Unintentional Weight Loss in Older Adults Review. Can. Med. Assoc. J. 2011, 183, 1159–1165. [Google Scholar] [CrossRef]
- Junne, F.; Ziser, K.; Giel, K.E.; Schag, K.; Skoda, E.; Mack, I.; Niess, A.; Zipfel, S.; Teufel, M. Determinants of Perceived Stress in Individuals with Obesity: Exploring the Relationship of Potentially Obesity-Related Factors and Perceived Stress. Eur. J. Obes. 2017, 10, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.R.; Berthelot, E.R. Community Covariates of Malnutrition Based Mortality Among Older Adults. Ann. Epidemiol. 2017, 20, 371–379. [Google Scholar] [CrossRef]
- Althoff, R.R.; Ametti, M.; Bertmann, F. The Role of Food Insecurity in Developmental Psychopathology. Prev. Med. 2016, 92, 106–109. [Google Scholar] [CrossRef]
- Berkowitz, S.A.; Fabreau, G.E. Association between Household Food Insecurity and Annual Health Care Costs. CMAJ 2015, 187, 1031–1032. [Google Scholar] [CrossRef]
- Schroeder, K.; Smaldone, A. Food Insecurity: A Concept Analysis. Nurs. Forum 2016, 1848, 3047–3054. [Google Scholar] [CrossRef] [PubMed]
- Seligman, H.K.; Schillinger, D. Hunger and Socioeconomic Disparities in Chronic Disease. N. Engl. J. Med. 2010, 363, 6–9. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).