Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT)
Abstract
1. Introduction
2. Methods and Materials
2.1. Translation and Cultural Adaptation
2.2. Sample Size Determination
2.3. Procedure
2.4. Participants
2.5. Measures
2.5.1. The Addiction-Like Eating Behavioral Scale—Italian Version (AEBS-IT)
2.5.2. The Modified Yale Food Addiction Scale 2.0 (mYFAS2.0)
2.5.3. The Binge Eating Scale (BES)
2.5.4. The Measure of Eating Compulsivity—Italian Version (MEC10-IT)
2.5.5. The Dutch Eating Behavior Questionnaire (DEBQ)
2.5.6. Statistical Analyses
3. Results
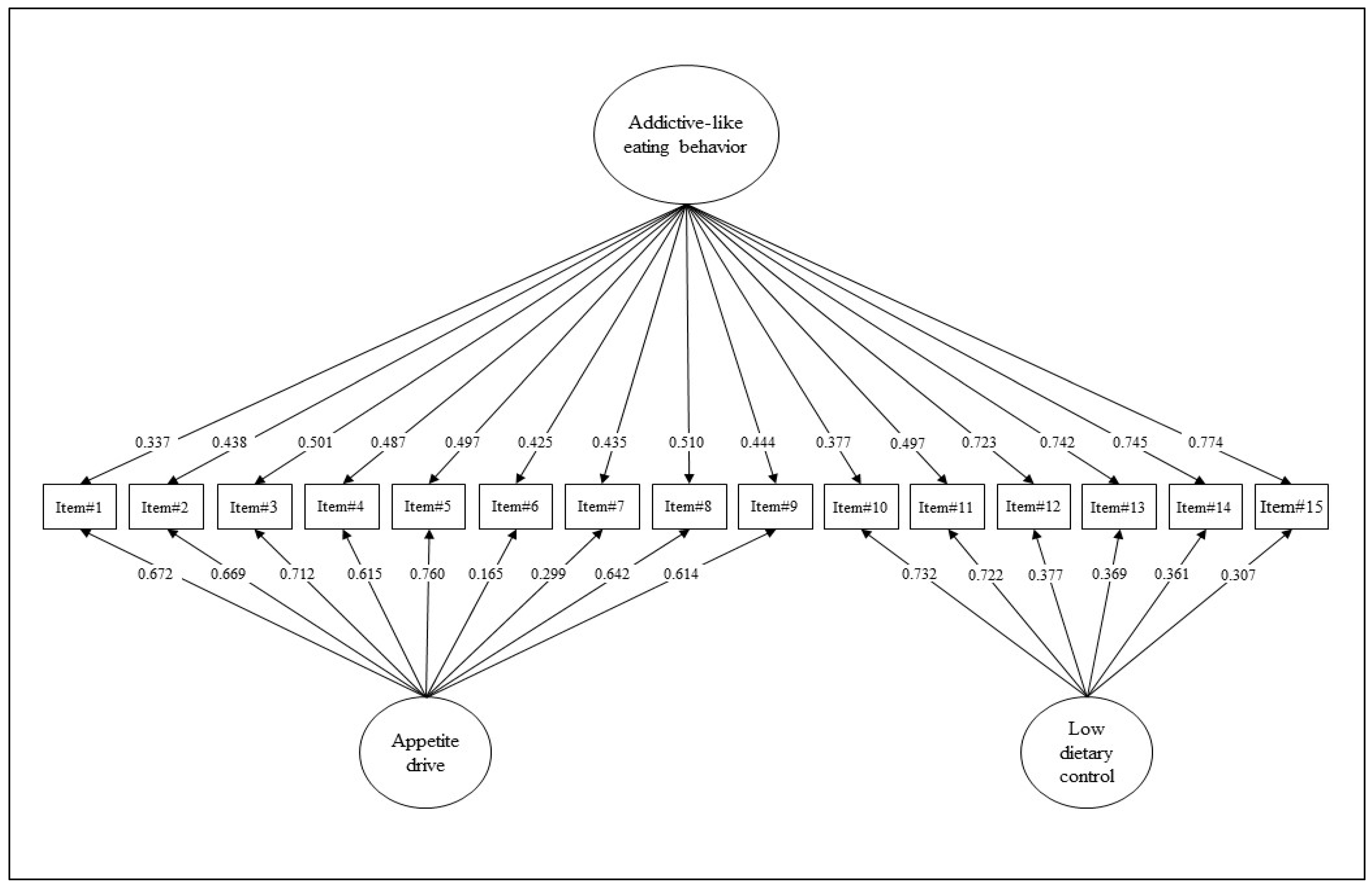
3.1. Structural Validity and Model Comparisons
3.2. Measurement Invariance across Samples
3.3. Psychometrics Properties
3.4. Convergent Validity
3.5. Accuracy of the ‘Addiction-Like Eating Behavior’ Scale as a Screening/Diagnostic Tool
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1 | 2 | 3 | 4 | 5 |
| MAI/QUASI MAI | QUALCHE VOLTA | METÀ DELLE VOLTE | IL PIÙ DELLE VOLTE | QUASI SEMPRE/ SEMPRE |
| 1 | Continuo a mangiare nonostante mi senta pieno | 1 | 2 | 3 | 4 | 5 |
| 2 | Mi servo porzioni eccessivamente grandi | 1 | 2 | 3 | 4 | 5 |
| 3 | Trovo difficile limitare cosa e/o quanto mangio | 1 | 2 | 3 | 4 | 5 |
| 4 | Una volta che comincio a mangiare certi cibi, non posso fermarmi finché non rimane niente | 1 | 2 | 3 | 4 | 5 |
| 5 | Quando si tratta di cibo, tendo a esagerare | 1 | 2 | 3 | 4 | 5 |
| 6 | Tendo a non mangiare troppo | 1 | 2 | 3 | 4 | 5 |
| 7 | Mi sento incapace di controllare il mio peso | 1 | 2 | 3 | 4 | 5 |
| 8 | Faccio abbuffate (grandi quantità di cibo in poco tempo) | 1 | 2 | 3 | 4 | 5 |
| 9 | Mangio fino a quando mi sento male | 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| FORTEMENTE IN DISACCORDO | IN DISACCORDO | NÉ IN ACCORDO, NÉ IN DISACCORDO | IN ACCORDO | FORTEMENTE IN ACCORDO |
| 10 | Tendo a non comprare alimenti lavorati ad alto contenuto di grassi e/o zuccheri | 1 | 2 | 3 | 4 | 5 |
| 11 | Non mangio molti cibi ad alto contenuto di grassi e/o zuccheri | 1 | 2 | 3 | 4 | 5 |
| 12 | Credo di avere una dieta sana | 1 | 2 | 3 | 4 | 5 |
| 13 | Riesco facilmente a fare scelte alimentari sane | 1 | 2 | 3 | 4 | 5 |
| 14 | Nonostante provi a mangiare in modo sano, finisco per mangiare cibi “cattivi” | 1 | 2 | 3 | 4 | 5 |
| 15 | Nonostante sia consapevole dell’effetto sulla mia salute, continuo a mangiare certi cibi non salutari | 1 | 2 | 3 | 4 | 5 |
References
- World Health Organisation. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 November 2022).
- Avila, C.; Holloway, A.C.; Hahn, M.K.; Morrison, K.M.; Restivo, M.; Anglin, R.; Taylor, V.H. An overview of links between obesity and mental health. Curr. Obes. Rep. 2015, 4, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Rajan, T.M.; Menon, V. Psychiatric disorders and obesity: A review of association studies. J. Postgrad. Med. 2017, 63, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.K. Biological, environmental, and social influences on childhood obesity. Pediatr. Res. 2016, 79, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, G. Group Motivation-Focused Interventions for Patients with Obesity and Binge Eating Disorder. Front. Psychol. 2018, 9, 1104. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Romano, L.; Di Renzo, L.; Di Lorenzo, N.; Cenname, G.; Gualtieri, P. Obesity: A preventable, treatable, but relapsing disease. Nutrition 2020, 71, 110615. [Google Scholar] [CrossRef] [PubMed]
- Hebebrand, J.; Albayrak, O.; Adan, R.; Antel, J.; Dieguez, C.; de Jong, J.; Leng, G.; Menzies, J.; Mercer, J.G.; Murphy, M.; et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 2014, 47, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Meule, A.; Heckel, D.; Jurowich, C.F.; Vogele, C.; Kubler, A. Correlates of food addiction in obese individuals seeking bariatric surgery. Clin. Obes. 2014, 4, 228–236. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Varallo, G.; Molinari, E.; Poggiogalle, E.; Donini, L.M.; Tarrini, G.; Melchionda, N.; Piccione, C.; et al. Validation of the Italian Yale Food Addiction Scale in postgraduate university students. Eat. Weight Disord. 2018, 23, 167–176. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Pursey, K.M.; Gearhardt, A.N.; Burrows, T.L. The relationship between "food addiction" and visceral adiposity in young females. Physiol. Behav. 2016, 157, 9–12. [Google Scholar] [CrossRef]
- Meule, A.; Gearhardt, A.N. Ten Years of the Yale Food Addiction Scale: A Review of Version 2.0. Curr. Addict. Rep. 2019, 6, 218–228. [Google Scholar] [CrossRef]
- Aloi, M.; Rania, M.; Rodriguez Munoz, R.C.; Jimenez Murcia, S.; Fernandez-Aranda, F.; De Fazio, P.; Segura-Garcia, C. Validation of the Italian version of the Yale Food Addiction Scale 2.0 (I-YFAS 2.0) in a sample of undergraduate students. Eat. Weight. Disord. 2017, 22, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Mannarini, S.; Fabbricatore, M.; Imperatori, C.; Innamorati, M.; Gearhardt, A.N.; Castelnuovo, G. Structural validity, measurement invariance, reliability and diagnostic accuracy of the Italian version of the Yale Food Addiction Scale 2.0 in patients with severe obesity and the general population. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2021, 26, 345–366. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Burrows, T.; Kay-Lambkin, F.; Pursey, K.; Skinner, J.; Dayas, C. Food addiction and associations with mental health symptoms: A systematic review with meta-analysis. J. Hum. Nutr. Diet 2018, 31, 544–572. [Google Scholar] [CrossRef] [PubMed]
- Ivezaj, V.; Wiedemann, A.A.; Grilo, C.M. Food addiction and bariatric surgery: A systematic review of the literature. Obes. Rev. 2017, 18, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Pursey, K.M.; Stanwell, P.; Gearhardt, A.N.; Collins, C.E.; Burrows, T.L. The Prevalence of Food Addiction as Assessed by the Yale Food Addiction Scale: A Systematic Review. Nutrients 2014, 6, 4552–4590. [Google Scholar] [CrossRef]
- Ziauddeen, H.; Fletcher, P.C. Is food addiction a valid and useful concept? Obes. Rev. Off. J. Int. Assoc. Study Obes. 2013, 14, 19–28. [Google Scholar] [CrossRef]
- Ruddock, H.K.; Christiansen, P.; Halford, J.C.G.; Hardman, C.A. The development and validation of the Addiction-like Eating Behaviour Scale. Int. J. Obes. 2017, 41, 1710–1717. [Google Scholar] [CrossRef]
- Markus, C.R.; Rogers, P.J.; Brouns, F.; Schepers, R. Eating dependence and weight gain; no human evidence for a ’sugar-addiction’ model of overweight. Appetite 2017, 114, 64–72. [Google Scholar] [CrossRef][Green Version]
- Ziauddeen, H.; Farooqi, I.S.; Fletcher, P.C. Obesity and the brain: How convincing is the addiction model? Nat. Rev. Neurosci. 2012, 13, 279–286. [Google Scholar] [CrossRef]
- Bechara, A. Decision making, impulse control and loss of willpower to resist drugs: A neurocognitive perspective. Nat. Neurosci. 2005, 8, 1458–1463. [Google Scholar] [CrossRef] [PubMed]
- Wiers, R.W.; Bartholow, B.D.; van den Wildenberg, E.; Thush, C.; Engels, R.C.; Sher, K.J.; Grenard, J.; Ames, S.L.; Stacy, A.W. Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacol. Biochem. Behav. 2007, 86, 263–283. [Google Scholar] [CrossRef]
- Legendre, M.; Begin, C. French validation of the addiction-like eating behavior scale and its clinical implication. Eat. Weight Disord. 2021, 26, 1893–1902. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, T.Q.; Pereira, C.W.; de Souza Costa, T.; da CostaLima, M.D. Translation and validation of the addiction-like Eating Behavior Scale from English to Portuguese in Brazil. J. Addict. Dis. 2020, 38, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed]
- Guillemin, F.; Bombardier, C.; Beaton, D.E. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Muthén, B.; Asparouhov, T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. Mplus Web Notes 2002, 9, 1–22. [Google Scholar]
- Yu, C.Y. Evaluating Cutoff Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes. Ph.D. Thesis, University of California, Los Angeles, CA, USA, 2002. [Google Scholar]
- Tomarken, A.J.; Waller, N.G. Structural Equation Modeling: Strengths, Limitations, and Misconceptions. Annu. Rev. Clin. Psychol. 2005, 1, 31–65. [Google Scholar] [CrossRef]
- Flora, D.B.; Curran, P.J. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychol. Methods 2004, 9, 466–491. [Google Scholar] [CrossRef]
- Bentler, P.M.; Chou, C.H. Practical issues in structural modeling. Soc. Methods Res. 1987, 16, 78–117. [Google Scholar] [CrossRef]
- Boomsma, A.; Hoogland, J.J. The robustness of LISREL modeling revisited. A Festschrift in honor of Karl Jöreskog. In Structural Equation Models: Present and Future; Cudeck, R., du Toit, S., Sorbom, D., Eds.; Scientific Software International: Lincolnwood, IL, USA, 2001; pp. 139–168. [Google Scholar]
- Marsh, H.W.; Balla, J.R.; McDonald, R.P. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychol. Bull. 1988, 103, 391–410. [Google Scholar] [CrossRef]
- Consoli, S.; Rossi, A.; Thompson, L.Y.; Volpi, C.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Assessing Psychometric Properties of the Italian Version of the Heartland Forgiveness Scale. Front. Psychol. 2020, 11, 596501. [Google Scholar] [CrossRef] [PubMed]
- Imperatori, C.; Fabbricatore, M.; Lester, D.; Manzoni, G.M.; Castelnuovo, G.; Raimondi, G.; Innamorati, M. Psychometric properties of the modified Yale Food Addiction Scale Version 2.0 in an Italian non-clinical sample. Eat. Weight. Disord. 2019, 24, 37–45. [Google Scholar] [CrossRef]
- Schulte, E.M.; Gearhardt, A.N. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2017, 25, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Gormally, J.; Black, S.; Daston, S.; Rardin, D. The assessment of binge eating severity among obese persons. Addict. Behav. 1982, 7, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Ricca, V.; Mannucci, E.; Moretti, S.; Di Bernardo, M.; Zucchi, T.; Cabras, P.L.; Rotella, C.M. Screening for binge eating disorder in obese outpatients. Compr. Psychiatry 2000, 41, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Imperatori, C.; Innamorati, M.; Lamis, D.A.; Contardi, A.; Continisio, M.; Castelnuovo, G.; Manzoni, G.M.; Fabbricatore, M. Factor Structure of the Binge Eating Scale in a Large Sample of Obese and Overweight Patients Attending Low Energy Diet Therapy. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2016, 24, 174–178. [Google Scholar] [CrossRef]
- Marcus, M.D.; Wing, R.R.; Hopkins, J. Obese binge eaters: Affect, cognitions, and response to behavioural weight control. J. Consult. Clin. Psychol. 1988, 56, 433–439. [Google Scholar] [CrossRef]
- Freitas, S.R.; Lopes, C.S.; Appolinario, J.C.; Coutinho, W. The assessment of binge eating disorder in obese women: A comparison of the binge eating scale with the structured clinical interview for the DSM-IV. Eat. Behav. 2006, 7, 282–289. [Google Scholar] [CrossRef]
- Grupski, A.E.; Hood, M.M.; Hall, B.J.; Azarbad, L.; Fitzpatrick, S.L.; Corsica, J.A. Examining the Binge Eating Scale in screening for binge eating disorder in bariatric surgery candidates. Obes. Surg. 2013, 23, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Duarte, C.; Pinto-Gouveia, J.; Ferreira, C. Expanding binge eating assessment: Validity and screening value of the Binge Eating Scale in women from the general population. Eat. Behav. 2015, 18, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Hood, M.M.; Grupski, A.E.; Hall, B.J.; Ivan, I.; Corsica, J. Factor structure and predictive utility of the Binge Eating Scale in bariatric surgery candidates. Surg. Obes. Relat. Dis. 2013, 9, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Schroder, R.; Sellman, J.D.; Adamson, S. Development and Validation of a Brief Measure of Eating Compulsivity (MEC). Subst. Use Misuse 2017, 52, 1918–1924. [Google Scholar] [CrossRef]
- Rossi, A.A.; Mannarini, S.; Schroder, R.; Castelnuovo, G.; Pietrabissa, G. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Measure of Eating Compulsivity (MEC10-IT). Appetite 2022. submitted. [Google Scholar]
- Van Strien, T.; Frijters, J.E.R.; Bergers, G.P.A.; Defares, P.B. The Dutch Eating Behaviour Questionnaire (DEBQ) for assessment of restrained, emotional and external eating behaviour. Int. J. Eat. Disord. 1986, 5, 747–755. [Google Scholar] [CrossRef]
- Dakanalis, A.; Zanetti, M.A.; Clerici, M.; Madeddu, F.; Riva, G.; Caccialanza, R. Italian version of the Dutch Eating Behavior Questionnaire. Psychometric proprieties and measurement invariance across sex, BMI-status and age. Appetite 2013, 71, 187–195. [Google Scholar] [CrossRef]
- Van Strien, T.; Herman, C.P.; Verheijden, M.W. Eating style, overeating and weight gain. A prospective 2-year follow-up study in a representative Dutch sample. Appetite 2013, 59, 782–789. [Google Scholar] [CrossRef]
- Riva, G.; Molinari, E. Clinical Psychology of Obesity; Boringhieri, B., Ed.; Bollati Boringhieri: Turin, Italy, 2004. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- R Core Team. The R Project for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014. [Google Scholar]
- Wei, T.; Simko, V. R Package “Corrplot”: Visualization of a Correlation Matrix, 0.84; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Rosseel, Y.; Oberski, D.; Byrnes, J.; Vanbrabant, L.; Savalei, V.; Merkle, E.; Hallquist, M.; Rhemtulla, M.; Katsikatsou, M.; Barendse, M. Package ‘lavaan’; R Foundation for Statistical Computing: Vienna, Austria, 2015. [Google Scholar]
- Sachs, M.C. plotROC: A Tool for Plotting ROC Curves. J. Stat. Softw. 2017, 79, 1–19. [Google Scholar] [CrossRef]
- Robin, X.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.; Müller, M. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Revelle, W. psych: Procedures for Personality and Psychological Research; Northwestern University: Evanston, IL, USA, 2018. [Google Scholar]
- Revelle, W. psychTools: Tools to Accompany the ’Psych’ Package for Psychological Research, 2.0.6; Northwestern University: Evanston, IL, USA, 2020. [Google Scholar]
- semTools Contributors. semTools: Useful Tools for Structural Equation Modeling, R package version 0.4-14; R Foundation for Statistical Computing: Vienna, Austria, 2016. [Google Scholar]
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Hoyle, R.H. Handbook of Strucural Equation Modeling; The Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Lionetti, F.; Keijsers, L.; Dellagiulia, A.; Pastore, M. Evidence of factorial validity of parental knowledge, control and solicitation, and adolescent disclosure scales: When the ordered nature of Likert scales matters. Front. Psychol. 2016, 7, 941. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Van de Schoot, R.; Lugtig, P.; Hox, J. A checklist for testing measurement invariance. Eur. J. Dev. Psychol. 2012, 9, 486–492. [Google Scholar] [CrossRef]
- Cheung, G.W.; Rensvold, R.B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Millsap, R.E. Statistical Approaches to Measurement Invariance; Routledge: New York, NY, USA, 2012; 368p. [Google Scholar] [CrossRef]
- Millsap, R.E.; Yun-Tein, J. Assessing Factorial Invariance in Ordered-Categorical Measures. Multivar. Behav. Res. 2004, 39, 479–515. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Lance, C.E. A Review and Synthesis of the Measurement Invariance Literature: Suggestions, Practices, and Recommendations for Organizational Research. Organ. Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Meredith, W. Measurement invariance, factor analysis and factorial invariance. Psychometrika 1993, 58, 525–543. [Google Scholar] [CrossRef]
- McDonald, R.P. Test Theory: A Unified Treatment; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1999. [Google Scholar]
- McDonald, R.P.; Ho, M.-H.R. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64–82. [Google Scholar] [CrossRef]
- McDonald, R.P.; Mulaik, S.A. Determinacy of common factors. Psychol. Bull. 1979, 86, 297–306. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson Ed.: Harlow, UK, 2014. [Google Scholar]
- Pallant, J. SPSS Survival Manual; McGraw-Hill Education: New York, NY, USA, 2013. [Google Scholar]
- Howell, D.C. Statistical Methods for Psychology; Wadsworth, Cengage Learning: Belmont, CA, USA, 2013. [Google Scholar]
- Chiorri, C. Teoria e Tecnica Psicometrica. Costruire un Test Psicologico; McGraw-Hill Companies: New York, NY, USA, 2011. [Google Scholar]
- Ebel, R.L. Measuring Educational Achievement; Prentice-Hall: Englewood Cliffs, NJ, USA, 1965. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Pepe, M.S. The Statistical Evaluation of Medical Tests for Classification and Prediction; Oxford Universtiy Press: New York, NY, USA, 2003. [Google Scholar]
- Zhou, X.H.; Obuchowski, N.A.; McClish, D. Statistical Methods in Diagnostic Medicine; Wiley: New York, NY, USA, 2002. [Google Scholar]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1998, 240, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- Steiger, J.H. Structural Model Evaluation and Modification: An Interval Estimation Approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Marazzi, N.; Agosti, F.; De Col, A.; Pietrabissa, G.; Castelnuovo, G.; Molinari, E.; Sartorio, A. Feasibility, Validity, and Reliability of the Italian Pediatric Quality of Life Inventory Multidimensional Fatigue Scale for Adults in Inpatients with Severe Obesity. Obes. Facts 2018, 11, 25–36. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Rossi, A.; Borrello, M.; Manzoni, G.M.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Development and Validation of a Self-Determination Theory-Based Measure of Motivation to Exercise and Diet in Children. Front. Psychol. 2020, 11, 1299. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; White, M.A.; Masheb, R.M.; Morgan, P.T.; Crosby, R.D.; Grilo, C.M. An examination of the food addiction construct in obese patients with binge eating disorder. Int. J. Eat. Disord. 2012, 45, 657–663. [Google Scholar] [CrossRef]
- Di Giacomo, E.; Aliberti, F.; Pescatore, F.; Santorelli, M.; Pessina, R.; Placenti, V.; Colmegna, F.; Clerici, M. Disentangling binge eating disorder and food addiction: A systematic review and meta-analysis. Eat. Weight Disord. 2022, 27, 1963–1970. [Google Scholar] [CrossRef]
- Piccinni, A.; Bucchi, R.; Fini, C.; Vanelli, F.; Mauri, M.; Stallone, T.; Cavallo, E.D.; Claudio, C. Food addiction and psychiatric comorbidities: A review of current evidence. Eat. Weight Disord. 2021, 26, 1049–1056. [Google Scholar] [CrossRef]
- Maxwell, A.L.; Gardiner, E.; Loxton, N.J. Investigating the relationship between reward sensitivity, impulsivity, and food addiction: A systematic review. Eur. Eat Disord. Rev. 2020, 28, 368–384. [Google Scholar] [CrossRef] [PubMed]
- Carr, M.M.; Wiedemann, A.A.; Macdonald-Gagnon, G.; Potenza, M.N. Impulsivity and compulsivity in binge eating disorder: A systematic review of behavioral studies. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 110, 110318. [Google Scholar] [CrossRef] [PubMed]
- Adamson, S. Measuring Eating Compulsivity in the Wider Clinical Context. Subst. Use Misuse 2017, 52, 1925–1926. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; White, M.A.; Masheb, R.M.; Grilo, C.M. An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr. Psychiatry 2013, 54, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Castelnuovo, G.; Pietrabissa, G.; Cattivelli, R.; Manzoni, G.M.; Molinari, E. Not Only Clinical Efficacy in Psychological Treatments: Clinical Psychology Must Promote Cost-Benefit, Cost-Effectiveness, and Cost-Utility Analysis. Front. Psychol. 2016, 7, 563. [Google Scholar] [CrossRef] [PubMed]


| Overall Sample (N = 953) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Descriptive Statistics | IDP—Specific Factor | IDP—General Factor | CFA | ||||||||||
| Mean | SD | SK | K | tsf | dsf | r(it−tot) sf | tgf | dgf | r(it−tot) gf | |λsf| | |λgf| | R2 | |
| Item#1 | 1.905 | 0.995 | 1.250 | 1.227 | −20.79 | 1.93 | 0.640 | −17.58 | 1.57 | 0.546 | 0.672 | 0.337 | 0.565 |
| Item#2 | 2.065 | 1.073 | 1.021 | 0.401 | −26.87 | 2.49 | 0.692 | −22.03 | 1.97 | 0.624 | 0.669 | 0.438 | 0.639 |
| Item#3 | 2.114 | 1.100 | 0.963 | 0.194 | −32.64 | 3.02 | 0.781 | −26.58 | 2.38 | 0.704 | 0.712 | 0.501 | 0.758 |
| Item#4 | 2.142 | 1.255 | 0.906 | −0.336 | −33.41 | 3.10 | 0.710 | −26.11 | 2.34 | 0.646 | 0.615 | 0.487 | 0.615 |
| Item#5 | 2.151 | 1.100 | 0.875 | −0.023 | −36.76 | 3.40 | 0.793 | −28.69 | 2.57 | 0.713 | 0.760 | 0.497 | 0.824 |
| Item#6 * | 3.329 | 1.261 | −0.368 | −0.991 | −15.89 | 1.43 | 0.304 | −16.35 | 1.46 | 0.401 | 0.165 | 0.425 | 0.208 |
| Item#7 | 2.610 | 1.340 | 0.389 | −1.084 | −19.30 | 1.77 | 0.414 | −17.77 | 1.59 | 0.440 | 0.299 | 0.435 | 0.279 |
| Item#8 | 1.751 | 1.052 | 1.561 | 1.824 | −24.38 | 2.27 | 0.729 | −21.85 | 1.96 | 0.654 | 0.642 | 0.510 | 0.672 |
| Item#9 | 1.363 | 0.797 | 2.714 | 7.653 | −13.42 | 1.25 | 0.565 | −13.05 | 1.17 | 0.499 | 0.614 | 0.444 | 0.574 |
| Item#10 * | 2.768 | 1.245 | 0.295 | −0.892 | −25.40 | 2.28 | 0.483 | −14.28 | 1.28 | 0.323 | 0.732 | 0.377 | 0.678 |
| Item#11 * | 2.898 | 1.182 | 0.133 | −0.870 | −30.45 | 2.74 | 0.581 | −20.05 | 1.79 | 0.450 | 0.722 | 0.497 | 0.768 |
| Item#12 * | 2.919 | 1.223 | 0.203 | −0.920 | −34.58 | 3.12 | 0.637 | −24.10 | 2.15 | 0.554 | 0.377 | 0.723 | 0.665 |
| Item#13 * | 2.803 | 1.151 | 0.299 | −0.710 | −31.09 | 2.78 | 0.642 | −23.45 | 2.10 | 0.582 | 0.369 | 0.742 | 0.687 |
| Item#14 | 2.910 | 1.155 | −0.065 | −0.933 | −22.13 | 1.99 | 0.418 | −18.19 | 1.63 | 0.474 | 0.361 | 0.745 | 0.686 |
| Item#15 | 2.965 | 1.220 | −0.128 | −1.049 | −24.42 | 2.21 | 0.466 | −21.47 | 1.92 | 0.513 | 0.307 | 0.774 | 0.693 |
| Inpatients with SEVERE obesity (n = 502) | |||||||||||||
| Descriptive Statistics | IDP—Specific Factor | IDP—General Factor | CFA | ||||||||||
| Mean | SD | SK | K | tsf | dsf | r(it−tot) sf | tgf | dgf | r(it−tot) gf | |λsf| | |λgf| | R2 | |
| Item#1 | 1.793 | 1.009 | 1.441 | 1.638 | −15.65 | 1.98 | 0.668 | −14.44 | 1.85 | 0.604 | 0.595 | 0.492 | 0.596 |
| Item#2 | 2.203 | 1.149 | 0.881 | −0.069 | −21.60 | 2.72 | 0.710 | −18.76 | 2.41 | 0.648 | 0.660 | 0.484 | 0.670 |
| Item#3 | 2.203 | 1.108 | 0.829 | −0.059 | −24.36 | 3.06 | 0.780 | −20.34 | 2.61 | 0.719 | 0.705 | 0.528 | 0.775 |
| Item#4 | 2.380 | 1.333 | 0.603 | −0.919 | −29.77 | 3.74 | 0.734 | −24.07 | 3.09 | 0.675 | 0.635 | 0.519 | 0.673 |
| Item#5 | 2.231 | 1.163 | 0.743 | −0.436 | −31.37 | 3.93 | 0.796 | −23.78 | 3.05 | 0.727 | 0.722 | 0.552 | 0.826 |
| Item#6 * | 3.424 | 1.286 | −0.535 | −0.847 | −8.83 | 1.06 | 0.301 | −10.69 | 1.38 | 0.405 | 0.104 | 0.448 | 0.211 |
| Item#7 | 3.084 | 1.288 | −0.027 | −1.180 | −16.08 | 1.96 | 0.428 | −11.63 | 1.50 | 0.451 | 0.328 | 0.426 | 0.289 |
| Item#8 | 1.922 | 1.156 | 1.248 | 0.642 | −20.90 | 2.65 | 0.734 | −19.17 | 2.46 | 0.669 | 0.585 | 0.565 | 0.662 |
| Item#9 | 1.408 | 0.868 | 2.565 | 6.468 | −10.50 | 1.34 | 0.559 | −10.25 | 1.31 | 0.499 | 0.562 | 0.496 | 0.562 |
| Item#10* | 2.743 | 1.309 | 0.280 | −1.029 | −18.48 | 2.32 | 0.462 | −12.05 | 1.55 | 0.356 | 0.639 | 0.448 | 0.609 |
| Item#11 * | 2.875 | 1.228 | 0.039 | −0.925 | −21.96 | 2.78 | 0.591 | −16.71 | 2.15 | 0.482 | 0.668 | 0.557 | 0.756 |
| Item#12 * | 3.223 | 1.303 | −0.191 | −1.023 | −23.19 | 2.94 | 0.587 | −16.76 | 2.16 | 0.514 | 0.424 | 0.659 | 0.614 |
| Item#13 * | 2.994 | 1.228 | 0.076 | −0.915 | −24.67 | 3.11 | 0.598 | −17.22 | 2.22 | 0.549 | 0.410 | 0.681 | 0.632 |
| Item#14 | 3.129 | 1.204 | −0.333 | −0.878 | −12.17 | 1.55 | 0.340 | −11.43 | 1.47 | 0.418 | 0.454 | 0.656 | 0.636 |
| Item#15 | 3.124 | 1.272 | −0.321 | −0.975 | −13.28 | 1.70 | 0.391 | −14.18 | 1.83 | 0.495 | 0.495 | 0.777 | 0.848 |
| General Population (n = 451) | |||||||||||||
| Descriptive Statistics | IDP—Specific Factor | IDP—General Factor | CFA | ||||||||||
| Mean | SD | SK | K | tsf | dsf | r(it−tot) sf | tgf | dgf | r(it−tot) gf | |λsf| | |λgf| | R2 | |
| Item#1 | 2.029 | 0.965 | 1.107 | 1.054 | −16.11 | 2.18 | 0.718 | −12.97 | 1.73 | 0.582 | 0.770 | 0.299 | 0.683 |
| Item#2 | 1.911 | 0.960 | 1.133 | 0.977 | −17.18 | 2.33 | 0.648 | −14.01 | 1.87 | 0.562 | 0.681 | 0.348 | 0.584 |
| Item#3 | 2.016 | 1.084 | 1.136 | 0.612 | −21.97 | 2.97 | 0.788 | −17.04 | 2.28 | 0.691 | 0.717 | 0.482 | 0.746 |
| Item#4 | 1.876 | 1.105 | 1.311 | 0.935 | −16.00 | 2.17 | 0.648 | −13.32 | 1.78 | 0.562 | 0.620 | 0.384 | 0.531 |
| Item#5 | 2.062 | 1.020 | 1.023 | 0.604 | −23.64 | 3.20 | 0.797 | −18.10 | 2.42 | 0.698 | 0.783 | 0.444 | 0.810 |
| Item#6 * | 3.224 | 1.226 | −0.187 | −1.074 | −12.76 | 1.72 | 0.289 | −12.92 | 1.72 | 0.383 | 0.203 | 0.391 | 0.194 |
| Item#7 | 2.082 | 1.193 | 1.002 | 0.075 | −10.11 | 1.37 | 0.362 | −9.02 | 1.20 | 0.360 | 0.325 | 0.329 | 0.213 |
| Item#8 | 1.561 | 0.886 | 2.002 | 4.243 | −12.60 | 1.71 | 0.703 | −11.32 | 1.51 | 0.597 | 0.720 | 0.407 | 0.683 |
| Item#9 | 1.313 | 0.707 | 2.844 | 9.003 | −8.40 | 1.14 | 0.576 | −7.99 | 1.07 | 0.497 | 0.662 | 0.392 | 0.592 |
| Item#10 * | 2.796 | 1.171 | 0.336 | −0.714 | −18.09 | 2.40 | 0.547 | −9.74 | 1.30 | 0.306 | 0.904 | 0.271 | 0.891 |
| Item#11 * | 2.925 | 1.129 | 0.279 | −0.842 | −20.65 | 2.73 | 0.610 | −12.93 | 1.72 | 0.443 | 0.738 | 0.420 | 0.721 |
| Item#12 * | 2.581 | 1.026 | 0.562 | −0.209 | −20.44 | 2.70 | 0.698 | −15.25 | 2.04 | 0.564 | 0.386 | 0.758 | 0.724 |
| Item#13 * | 2.590 | 1.019 | 0.483 | −0.307 | −20.55 | 2.71 | 0.683 | −15.66 | 2.09 | 0.595 | 0.356 | 0.796 | 0.760 |
| Item#14 | 2.665 | 1.046 | 0.153 | −0.742 | −16.29 | 2.14 | 0.487 | −12.43 | 1.66 | 0.505 | 0.118 | 0.787 | 0.634 |
| Item#15 | 2.789 | 1.136 | 0.046 | −1.038 | −19.94 | 2.64 | 0.541 | −15.45 | 2.06 | 0.508 | 0.000 | 0.744 | 0.554 |
| Model | χ2 (df) | CFI | RMSEA | Comparison | Δχ2(Δdf) | p-Value | |ΔCFI| | |ΔRMSEA| |
|---|---|---|---|---|---|---|---|---|
| 1. Bi-factor model | 506.245 (75) | 0.989 | 0.078 | |||||
| 2. Two first-order factors model | 2284.543 (89) | 0.945 | 0.161 | 1 vs. 2 | 1178.3 (14) | < 0.001 | 0.045 | 0.083 |
| 3. Single factor model | 4505.043 (90) | 0.891 | 0.227 | 1 vs. 3 | 3998.8 (15) | < 0.001 | 0.099 | 0.149 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, A.A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients 2023, 15, 104. https://doi.org/10.3390/nu15010104
Rossi AA, Mannarini S, Castelnuovo G, Pietrabissa G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients. 2023; 15(1):104. https://doi.org/10.3390/nu15010104
Chicago/Turabian StyleRossi, Alessandro Alberto, Stefania Mannarini, Gianluca Castelnuovo, and Giada Pietrabissa. 2023. "Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT)" Nutrients 15, no. 1: 104. https://doi.org/10.3390/nu15010104
APA StyleRossi, A. A., Mannarini, S., Castelnuovo, G., & Pietrabissa, G. (2023). Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients, 15(1), 104. https://doi.org/10.3390/nu15010104








