Sarcopenia Prevalence and Risk Factors among Residents in Aged Care †
Abstract
1. Introduction
2. Materials and Methods
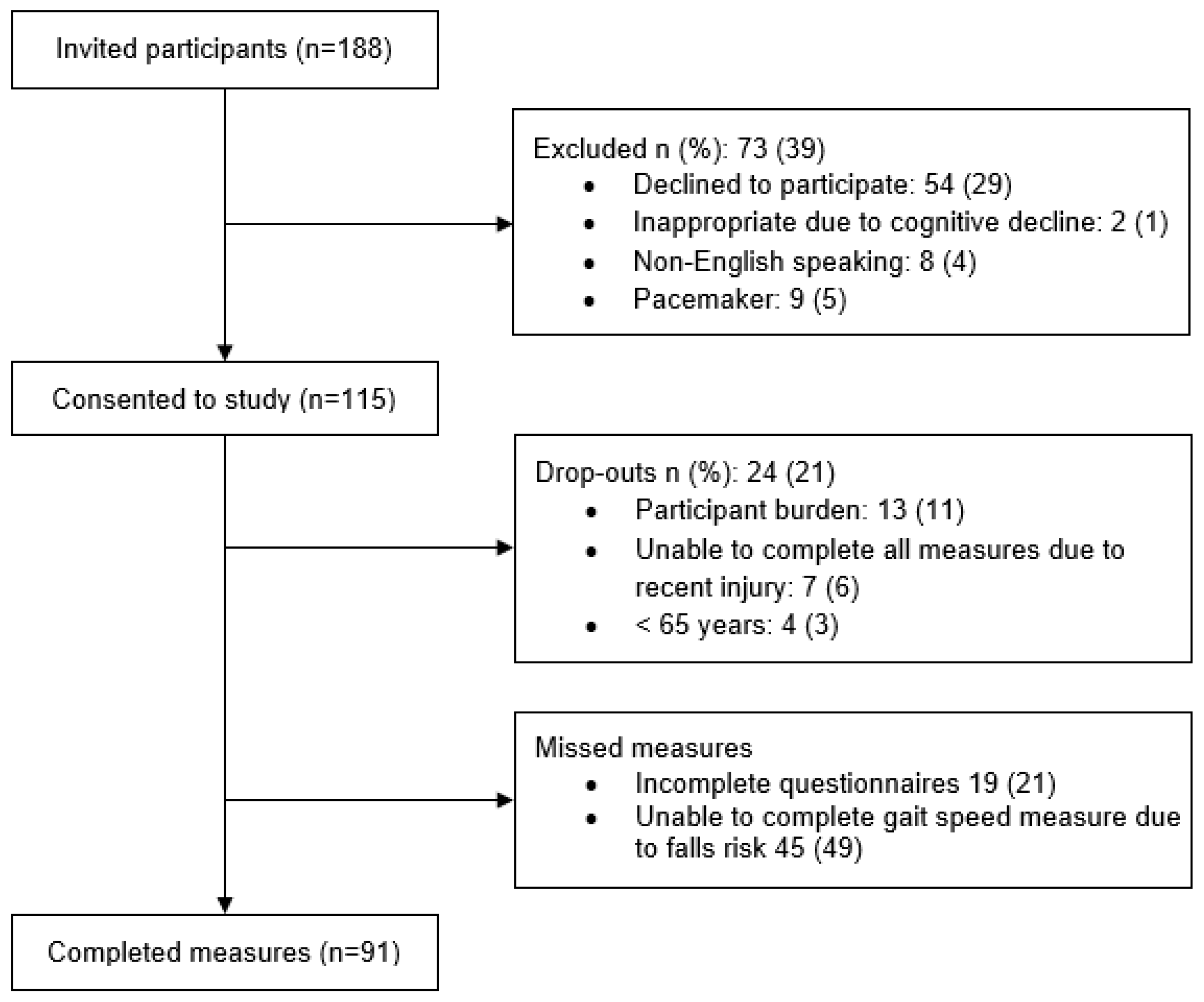
2.1. Study Design and Recruitment
2.2. Data Collection
2.2.1. Questionnaires
SARC-F
Malnutrition
Dysphagia
Depression
Quality of Life
2.2.2. Physical Measures
Height and Weight
Grip Strength
Gait Speed
Body Composition
Sarcopenia
2.3. Statistical Analysis
3. Results
3.1. Sarcopenia Prevalence and Participant Characteristics
3.2. Body Composition
3.3. Participants’ Nutritional Status and Mental/Physical Well-Being
3.4. Factors Predicting Sarcopenia
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dos Santos, L.; Cyrino, E.S.; Antunes, M.; Santos, D.A.; Sardinha, L.B. Sarcopenia and physical independence in older adults: The independent and synergic role of muscle mass and muscle function. J. Cachexia Sarcopenia Muscle 2017, 8, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Stolz, E.; Mayerl, H.; Rásky, É.; Freidl, W. Individual and country-level determinants of nursing home admission in the last year of life in Europe. PLoS ONE 2019, 14, e0213787. [Google Scholar] [CrossRef] [PubMed]
- Tsekoura, M.; Kastrinis, A.; Katsoulaki, M.; Billis, E.; Gliatis, J. Sarcopenia and its impact on quality of life. Adv. Exp. Med. Biol. 2017, 987, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Yeung, S.S.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, Y.; Hao, Q.; Ge, M.; Dong, B. Sarcopenia and hospital-related outcomes in the old people: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2019, 31, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Altuna-Venegas, S.; Aliaga-Vega, R.; Maguiña, J.L.; Parodi, J.F.; Runzer-Colmenares, F.M. Risk of community-acquired pneumonia in older adults with sarcopenia of a hospital from Callao, Peru 2010–2015. Arch. Gerontol. Geriatr. 2019, 82, 100–105. [Google Scholar] [CrossRef]
- Bone, A.E.; Hepgul, N.; Kon, S.; Maddocks, M. Sarcopenia and frailty in chronic respiratory disease: Lessons from gerontology. Chron. Respir. Dis. 2017, 14, 85–99. [Google Scholar] [CrossRef]
- Liu, P.; Hao, Q.; Hai, S.; Wang, H.; Cao, L.; Dong, B. Sarcopenia as a predictor of all-cause mortality among community-dwelling older people: A systematic review and meta-analysis. Maturitas 2017, 103, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-García, J.D.; Martínez-Amat, A.; Hita-Contreras, F.; Fábrega-Cuadros, R.; Álvarez-Salvago, F.; Aibar-Almazán, A. Muscle Strength and Physical Performance Are Associated with Reaction Time Performance in Older People. Int. J. Environ. Res. Public Health 2021, 18, 5893. [Google Scholar] [CrossRef]
- Zanker, J.; Scott, D.; Reijnierse, E.; Brennan-Olsen, S.; Daly, R.; Girgis, C.; Grossmann, M.; Hayes, A.; Henwood, T.; Hirani, V. Establishing an operational definition of sarcopenia in Australia and New Zealand: Delphi method based consensus statement. J. Nutr. Health Aging 2019, 23, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.M.; Cruz-Jentoft, A.J.; Fielding, R.A.; Kanis, J.A.; Reginster, J.-Y.; Bruyère, O.; Cesari, M.; Chapurlat, R.; Al-Daghri, N.; Dennison, E.; et al. Is There Enough Evidence for Osteosarcopenic Obesity as a Distinct Entity? A Critical Literature Review. Calcif. Tissue Int. 2019, 105, 109–124. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Liperoti, R.; Fusco, D.; Mastropaolo, S.; Quattrociocchi, D.; Proia, A.; Russo, A.; Bernabei, R.; Onder, G. Prevalence and risk factors of sarcopenia among nursing home older residents. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2012, 67, 48–55. [Google Scholar] [CrossRef]
- Senior, H.E.; Henwood, T.R.; Beller, E.M.; Mitchell, G.K.; Keogh, J.W. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas 2015, 82, 418–423. [Google Scholar] [CrossRef]
- Urzi, F.; Šimunič, B.; Buzan, E. Basis for sarcopenia screening with the SARC-CalF in nursing homes. J. Am. Med. Dir. Assoc. 2017, 18, 991.e5–991.e10. [Google Scholar] [CrossRef]
- Rahman, T.T.A.; Elkholy, N.M.; Mortagy, A.K. Prevalence of sarcopenia among nursing home older residents in Cairo, Egypt. Adv. Aging Res. 2014, 3, 118. [Google Scholar] [CrossRef][Green Version]
- Yang, M.; Lu, J.; Jiang, J.; Zeng, Y.; Tang, H. Comparison of four sarcopenia screening tools in nursing home residents. Aging Clin. Exp. Res. 2019, 31, 1481–1489. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M. Validation of the Mini Nutritional Assessment Short-Form (MNA®-SF): A practical tool for identification of nutritional status. JNHA-J. Nutr. Health Aging 2009, 13, 782. [Google Scholar] [CrossRef]
- Ranhoff, A.H.; Gjoen, A.; Mowe, M. Screening for malnutrition in elderly acute medical patients: The usefulness of MNA-SF. J. Nutr. Health Aging 2005, 9, 221–225. [Google Scholar]
- Belafsky, P.C.; Mouadeb, D.A.; Rees, C.J.; Pryor, J.C.; Postma, G.N.; Allen, J.; Leonard, R.J. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann. Otol. Rhinol. Laryngol. 2008, 117, 919–924. [Google Scholar] [CrossRef]
- Brink, T.L.; Yesavage, J.A.; Lum, O.; Heersema, P.H.; Adey, M.; Rose, T.L. Screening tests for geriatric depression. Clin. Gerontol. 1982, 1, 37–43. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Greenberg, S.A. The geriatric depression scale (GDS). Best Pract. Nurs. Care Older Adults 2012, 4, 1–2. [Google Scholar]
- Jakobsson, U.; Westergren, A.; Lindskov, S.; Hagell, P. Construct validity of the SF-12 in three different samples. J. Eval. Clin. Pract. 2012, 18, 560–566. [Google Scholar] [CrossRef]
- Resnick, B.; Nahm, E.S. Reliability and validity testing of the revised 12-item Short-Form Health Survey in older adults. J. Nurs. Meas. 2001, 9, 151–161. [Google Scholar] [CrossRef]
- Barbosa, V.; Stratton, R.; Lafuente, E.; Elia, M. Ulna length to predict height in English and Portuguese patient populations. Eur. J. Clin. Nutr. 2012, 66, 209–215. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower extremity function and subsequent disability: Consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M221–M231. [Google Scholar] [CrossRef]
- Ling, C.H.; de Craen, A.J.; Slagboom, P.E.; Gunn, D.A.; Stokkel, M.P.; Westendorp, R.G.; Maier, A.B. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin. Nutr. 2011, 30, 610–615. [Google Scholar] [CrossRef]
- Voelker, S.N.; Michalopoulos, N.; Maier, A.B.; Reijnierse, E.M. Reliability and Concurrent Validity of the SARC-F and Its Modified Versions: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2021, 22, 1864–1876. [Google Scholar] [CrossRef]
- Juby, A.G.; Mager, D.R. A review of nutrition screening tools used to assess the malnutrition-sarcopenia syndrome (MSS) in the older adult. Clin. Nutr. 2019, 32, 8–15. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Mithal, A.; Bonjour, J.-P.; Boonen, S.; Burckhardt, P.; Degens, H.; Fuleihan, G.E.H.; Josse, R.; Lips, P.; Torres, J.M.; Rizzoli, R. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos. Int. 2013, 24, 1555–1566. [Google Scholar] [CrossRef]
- Poortmans, J.; Carpentier, A.; Pereira-Lancha, L.; Lancha, A., Jr. Protein turnover, amino acid requirements and recommendations for athletes and active populations. Braz. J. Med. Biol. Res. 2012, 45, 875–890. [Google Scholar] [CrossRef] [PubMed]
- Chatindiara, I.; Allen, J.; Hettige, D.; Senior, S.; Richter, M.; Kruger, M.; Wham, C. High prevalence of malnutrition and frailty among older adults at admission to residential aged care. J. Prim. Health Care 2020, 12, 305–317. [Google Scholar] [CrossRef]
- Visvanathan, R. Australia and New Zealand Society for Geriatric Medicine Position Statement No. 6: Undernutrition and the Older Person. Aust. N. Z. Soc. Geriatr. Med. 2009, 28, 99–105. [Google Scholar]
- Beaudart, C.; Sanchez-Rodriguez, D.; Locquet, M.; Reginster, J.-Y.; Lengelé, L.; Bruyère, O. Malnutrition as a strong predictor of the onset of sarcopenia. Nutrients 2019, 11, 2883. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Baumgartner, R.N. Body composition in healthy aging. Ann. N. Y. Acad. Sci. 2000, 904, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Davison, K.K.; Ford, E.S.; Cogswell, M.E.; Dietz, W.H. Percentage of body fat and body mass index are associated with mobility limitations in people aged 70 and older from NHANES III. J. Am. Geriatr. Soc. 2002, 50, 1802–1809. [Google Scholar] [CrossRef]
- Zoico, E.; Di Francesco, V.; Guralnik, J.; Mazzali, G.; Bortolani, A.; Guariento, S.; Sergi, G.; Bosello, O.; Zamboni, M. Physical disability and muscular strength in relation to obesity and different body composition indexes in a sample of healthy elderly women. Int. J. Obes. 2004, 28, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Perna, S.; Peroni, G.; Faliva, M.A.; Bartolo, A.; Naso, M.; Miccono, A.; Rondanelli, M. Sarcopenia and sarcopenic obesity in comparison: Prevalence, metabolic profile, and key differences. A cross-sectional study in Italian hospitalized elderly. Aging Clin. Exp. Res. 2017, 29, 1249–1258. [Google Scholar] [CrossRef]
- Stenholm, S.; Harris, T.B.; Rantanen, T.; Visser, M.; Kritchevsky, S.B.; Ferrucci, L. Sarcopenic obesity-definition, etiology and consequences. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 693. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Atkins, J.L. Muscle loss and obesity: The health implications of sarcopenia and sarcopenic obesity. Proc. Nutr. Soc. 2015, 74, 405–412. [Google Scholar] [CrossRef]
- Sun, A.; Heshka, S.; Heymsfield, S.; Wang, J.; Pierson, R.; Gallagher, D. Is there an association between skeletal muscle mass and bone mineral density among African-American, Asian-American, and European-American women? Acta Diabetol. 2003, 40, s309–s313. [Google Scholar] [CrossRef]
- Zhong, K.; Lei, S.; Yang, F.; Chen, X.; Tan, L.; Zhu, X.; Tian, Q.; Deng, H.-W. The differences of sarcopenia-related phenotypes: Effects of gender and population. Eur. Rev. Aging Phys. Act. 2012, 9, 63–69. [Google Scholar] [CrossRef]
- Visser, M.; Deeg, D.J.H.; Lips, P.; Harris, T.B.; Bouter, L.M. Skeletal Muscle Mass and Muscle Strength in Relation to Lower-Extremity Performance in Older Men and Women. J. Am. Geriatr. Soc. 2000, 48, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Schonnop, R.; Yang, Y.; Feldman, F.; Robinson, E.; Loughin, M.; Robinovitch, S.N. Prevalence of and factors associated with head impact during falls in older adults in long-term care. Can. Med. Assoc. J. 2013, 185, E803. [Google Scholar] [CrossRef]
- Park, S.W.; Goodpaster, B.H.; Strotmeyer, E.S.; Kuller, L.H.; Broudeau, R.; Kammerer, C.; De Rekeneire, N.; Harris, T.B.; Schwartz, A.V.; Tylavsky, F.A. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: The health, aging, and body composition study. Diabetes Care 2007, 30, 1507–1512. [Google Scholar] [CrossRef]
- Mesinovic, J.; Zengin, A.; De Courten, B.; Ebeling, P.R.; Scott, D. Sarcopenia and type 2 diabetes mellitus: A bidirectional relationship. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 1057. [Google Scholar] [CrossRef]
- Nomura, T.; Ishiguro, T.; Ohira, M.; Ikeda, Y. Diabetic polyneuropathy is a risk factor for decline of lower extremity strength in patients with type 2 diabetes. J. Diabetes Investig. 2018, 9, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Shachar, S.S.; Williams, G.R.; Muss, H.B.; Nishijima, T.F. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. Eur. J. Cancer 2016, 57, 58–67. [Google Scholar] [CrossRef]
- Baracos, V.E.; Martin, L.; Korc, M.; Guttridge, D.C.; Fearon, K.C. Cancer-associated cachexia. Nat. Rev. Dis. Primers 2018, 4, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.R.; Rier, H.N.; McDonald, A.; Shachar, S.S. Sarcopenia & aging in cancer. J. Geriatr. Oncol. 2019, 10, 374–377. [Google Scholar] [PubMed]
- Li, Z.; Jeon, Y.-H.; Low, L.-F.; Chenoweth, L.; O’Connor, D.W.; Beattie, E.; Brodaty, H. Validity of the geriatric depression scale and the collateral source version of the geriatric depression scale in nursing homes. Int. Psychogeriatr. 2015, 27, 1495. [Google Scholar] [CrossRef]
| Total (n = 91) | Sarcopenic n (%): 37 (41) | Non-Sarcopenic n (%): 54 (59) | p-Value * | |
|---|---|---|---|---|
| Age, years, mean ± SD | 86.0 ± 8.3 | 88.6 ± 7.6 | 84.2 ± 8.4 | 0.01 * |
| Age, years, n (%) | 0.14 | |||
| <85 | 38 (42) | 12 (32) | 26 (68) | |
| ≥85 | 53 (58) | 25 (47) | 28 (53) | |
| Gender, n (%) | 0.80 | |||
| Women | 58 (64) | 23 (40) | 35 (60) | |
| Men | 33 (36) | 14 (42) | 19 (58) | |
| Ethnicity (n = 88) 1, n (%) | 0.84 | |||
| New Zealand European | 59 (67) | 23 (39) | 36 (61) | |
| Other 2 | 29 (33) | 13 (45) | 16 (55) | |
| Marital status (n = 76) 1, n (%) | 0.79 | |||
| Partnered | 29 (38) | 12 (41) | 17 (59 | |
| No partner | 47 (62) | 18 (38) | 29 (62) | |
| Level of education (n = 72) 1, n (%) | 0.48 | |||
| Less than tertiary | 25 (35) | 8 (32) | 17 (68) | |
| Tertiary and higher | 47 (65) | 19 (40) | 28 (60) | |
| Length of stay (n = 76) 1, n (%) | 0.15 | |||
| ≤30 months | 48 (63) | 16 (33) | 32 (67) | |
| >30 months | 28 (37) | 14 (50) | 14 (50) | |
| Level of care (n = 91), n (%) | 0.005 * | |||
| Rest home level | 53 (58) | 15 (28) | 38 (72) | |
| Hospital level | 38 (42) | 22 (58) | 16 (42) | |
| Oral nutritional supplement use (n = 85) 1, n (%) | 0.52 | |||
| Yes | 18 (21) | 6 (33) | 12 (67) | |
| No | 67 (79) | 28 (42) | 39 (58) |
| Total (n = 91) | Sarcopenic n (%): 37 (41) | Non-Sarcopenic n (%): 54 (59) | p-Value * | |
|---|---|---|---|---|
| Number of regular medications (n = 81), n (%) 1 | 0.004 * | |||
| ≤7 | 41 (51) | 23 (56) | 18 (44) | |
| >7 | 40 (49) | 10 (25) | 30 (75) | |
| Comorbidities (n = 86), n (%) 1 | ||||
| Number of comorbidities | 0.90 | |||
| ≤5 | 41 (48) | 17 (42) | 24 (58) | |
| >5 | 45 (52) | 18 (40) | 27 (60) | |
| Hypertension | 0.22 | |||
| No | 45 (54) | 16 (36) | 29 (64) | |
| Yes | 39 (46) | 19 (49) | 20 (51) | |
| Cardiovascular diseases | 0.94 | |||
| No | 26 (31) | 11 (42) | 15 (58) | |
| Yes | 59 (69) | 24 (41) | 34 (59) | |
| Diabetes | 0.03 * | |||
| No | 71 (79) | 26 (37) | 45 (63) | |
| Yes | 13 (21) | 9 (69) | 4 (31) | |
| Cognitive impairment | 0.66 | |||
| No | 48 (57) | 19 (40) | 29 (60) | |
| Yes | 36 (43) | 16 (44) | 20 (56) | |
| Renal diseases | 0.35 | |||
| No | 68 (81) | 30 (44) | 38 (56) | |
| Yes | 16 (19) | 5 (31) | 11 (69) | |
| Cancer | 0.05 * | |||
| No | 74 (88) | 28 (38) | 46 (62) | |
| Yes | 10 (12) | 7 (70) | 3 (30) | |
| Chronic respiratory diseases | 0.72 | |||
| No | 71 (85) | 29 (41) | 42 (59) | |
| Yes | 13 (15) | 6 (46) | 7 (54) | |
| Arthritis | 0.23 | |||
| No | 64 (76) | 29 (45) | 35 (55) | |
| Yes | 20 (24) | 6 (30) | 14 (70) | |
| Fracture | 0.91 | |||
| No | 74 (88) | 31 (42) | 43 (58) | |
| Yes | 10 (12) | 4 (40) | 6 (60) | |
| SARC-F Score (n = 76) 1 | ||||
| <4 | 35 (46) | 10 (29) | 25 (71) | 0.34 |
| ≥4 | 41 (54) | 16 (39) | 25 (61) | |
| Dysphagia (n = 76) 1 | 0.19 | |||
| Not at risk | 53 (70) | 17 (32) | 36 (68) | |
| At-risk | 23 (30) | 11 (48) | 12 (52) | |
| Depression (n = 72) 1 | 0.006 * | |||
| Low risk | 47 (65) | 11 (23) | 36 (77) | |
| At-risk/high risk | 25 (35) | 14 (56) | 11 (44) | |
| Malnutrition (n = 87) 1 | 0.004 | |||
| Not at risk | 15 (17) | 1 (7) | 14 (93) | |
| At-risk/malnourished | 72 (83) | 34 (47) | 38 (53) | |
| SF-12 Physical Component Score (n = 61) 1 | 0.73 | |||
| ≥50 | 48 (80) | 19 (86) | 29 (76) | |
| <50 | 12 (20) | 3 (14) | 9 (24) | |
| SF-12 Mental Component Score(n = 61) 1 | 0.36 | |||
| ≥42 | 10 (17) | 5 (23) | 5 (13) | |
| <42 | 50 (83) | 17 (77) | 33 (87) | |
| Total (n = 91) | Sarcopenic n (%): 37 (41) | Non-Sarcopenic n (%): 54 (59) | p-Value * | |
|---|---|---|---|---|
| BMI (kg/m2) | 24.9 ± 6.1 | 21.6 ± 3.7 | 27.7 ± 5.9 | <0.001 * |
| Fat mass, mean ± SD (kg) | 25 ± 12 | 19 ± 8 | 30 ± 12 | <0.001 * |
| BF%, mean ± SD (kg) | 37 ± 11 | 33 ± 9.7 | 39 ± 11 | 0.01 * |
| Fat free mass (kg) | 40 (34, 47) | 34 (31, 40) | 42 (37, 51) | <0.001 * |
| Skeletal mass index (kg/h2) | 6.1 (5.3, 7.1) | 5.1 (4.7, 5.8) | 6.8 (6.0, 7.7) | <0.001 * |
| Skeletal muscle mass (kg) | 20 (17, 25) | 17 (15, 21) | 22 (20, 27) | <0.001 * |
| Appendicular lean mass (kg) | 15 (13, 20) | 13 (11, 15) | 17 (15, 22) | <0.001 * |
| Bone mineral content (kg) | 2.4 (2.1, 2.8) | 2.3 (2.0, 2.6) | 2.5 (2.3, 2.9) | 0.003 * |
| Grip strength, mean ± SD (kg) (n = 82) 1 | 13.9 ± 7.8 | 9.5 ± 5.9 | 16.7 ± 7.6 | <0.001 * |
| Gait speed, mean ± SD (m/s) (n = 46) 1 | 0.55 ± 1.42 | 0.49 ± 1.30 | 0.57 ± 1.45 | 0.175 |
| Total | With Sarcopenia | Without Sarcopenia | OR (95% CI) | ||
|---|---|---|---|---|---|
| Univariate | Multivariate | ||||
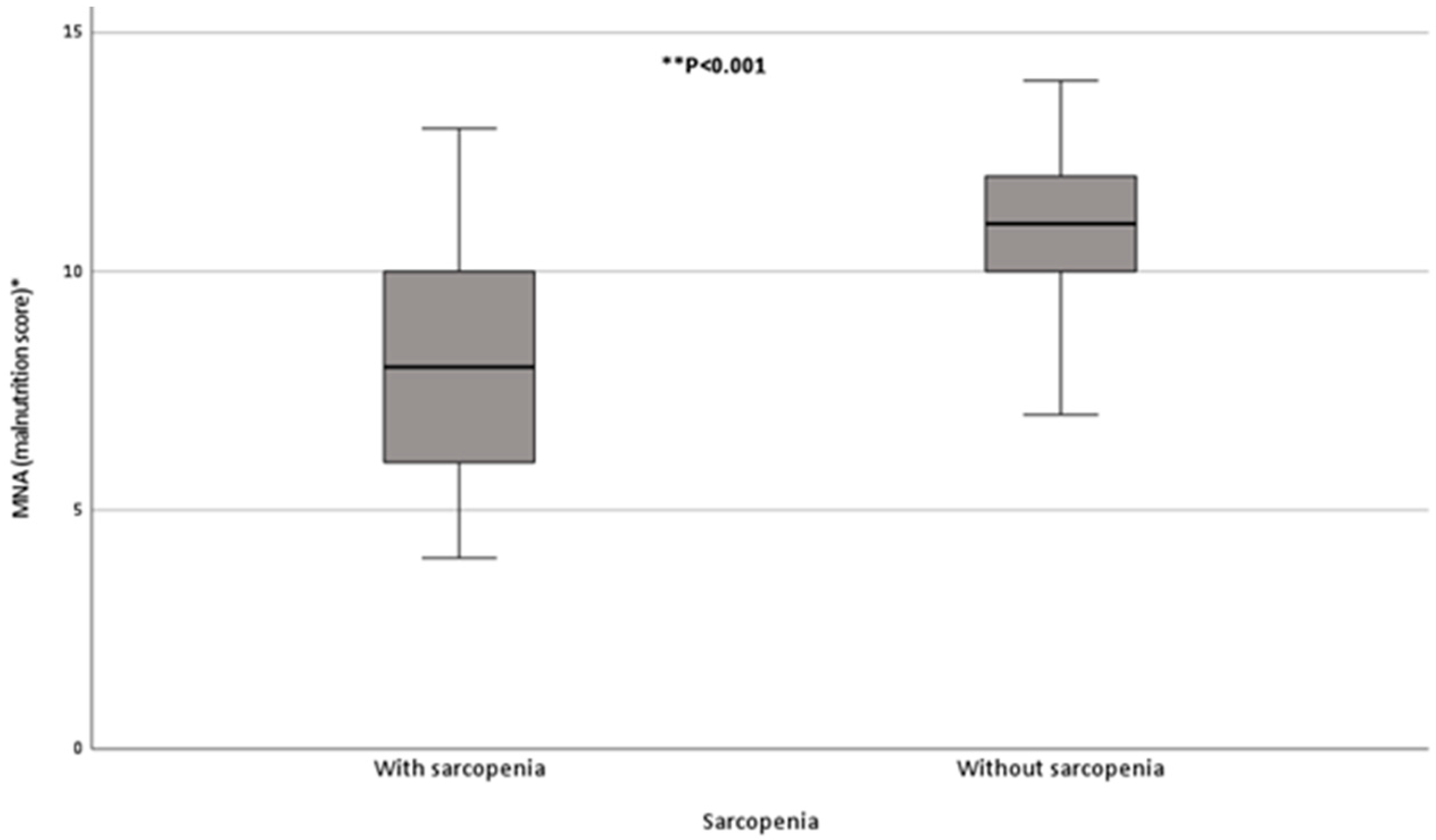
| Malnutrition score 1 | 9.5 ± 2.3 | 8.2 ± 2.1 | 10.0 ± 1.9 | 1.7 (1.3, 2.2) | 1.6 (1.0, 2.4) |
| Depression score 2 | 4.4 ± 3.3 | 5.4 ± 3.8 | 3.7 ± 2.9 | 0.9 (0.7, 1.0) | 0.8 (0.6, 1.1) |
| BMI (kg/m2) | 24.9 ± 6.1 | 21.6 ± 3.7 | 27.7 ± 5.9 | 1.4 (1.2, 1.6) | 1.4 (1.1, 1.7) |
| Age (years) | 86.0 ± 8.3 | 88.6 ± 7.6 | 84.2 ± 8.8 | 0.9 (0.9, 1.0) | 0.9 (0.8, 1.0) |
| Number of regular medications | 7.7 ± 3.4 | 6.4 ± 3.0 | 8.7 ± 3.4 | 1.3 (1.0, 1.5) | 1.1 (0.8, 1.4) |
| Level of care, n (%) | |||||
| Rest home care | 53 (58) | 15 (28) | 38 (72) | Reference category | |
| Hospital care | 38 (42) | 22 (58) | 16 (42) | 3.5 (1.4, 8.4) | 1.0 (0.2, 5.6) |
| Total | With Sarcopenia | Without Sarcopenia | OR (95% CI) | ||
|---|---|---|---|---|---|
| Univariate | Multivariate | ||||
| Malnutrition score 1 | 9.5 ± 2.3 | 8.2 ± 2.1 | 10 ± 1.9 | 1.7 (1.3, 2.2) | 1.6 (1.1, 2.4) |
| Depression score 2 | 4.4 ± 3.3 | 5.4 ± 3.8 | 3.7 ± 2.9 | 0.9 (0.7, 1.0) | 0.8 (0.6, 1.0) |
| BF% | 37 ± 11 | 33 ± 10 | 39 ± 11 | 1.1 (1.0, 1.1) | 1.1 (1.0, 1.1) |
| Age (years) | 86.0 ± 8.3 | 88.6 ± 7.6 | 84.2 ± 8.8 | 0.9 (0.9, 1.0) | 0.9 (0.8, 1.0) |
| Number of regular medications | 7.7 ± 3.4 | 6.4 ± 3.0 | 8.7 ± 3.4 | 1.3 (1.0, 1.5) | 1.2 (0.9, 1.5) |
| Level of care, n (%) | |||||
| Rest home care | 53 (58) | 15 (28) | 38 (72) | Reference category | |
| Hospital care | 38 (42) | 22 (58) | 16 (42) | 3.5 (1.4, 8.4) | 1.0 (0.2, 4.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Darroch, P.; O’Brien, W.J.; Mazahery, H.; Wham, C. Sarcopenia Prevalence and Risk Factors among Residents in Aged Care. Nutrients 2022, 14, 1837. https://doi.org/10.3390/nu14091837
Darroch P, O’Brien WJ, Mazahery H, Wham C. Sarcopenia Prevalence and Risk Factors among Residents in Aged Care. Nutrients. 2022; 14(9):1837. https://doi.org/10.3390/nu14091837
Chicago/Turabian StyleDarroch, Phillipa, Wendy J. O’Brien, Hajar Mazahery, and Carol Wham. 2022. "Sarcopenia Prevalence and Risk Factors among Residents in Aged Care" Nutrients 14, no. 9: 1837. https://doi.org/10.3390/nu14091837
APA StyleDarroch, P., O’Brien, W. J., Mazahery, H., & Wham, C. (2022). Sarcopenia Prevalence and Risk Factors among Residents in Aged Care. Nutrients, 14(9), 1837. https://doi.org/10.3390/nu14091837







