Complementary Feeding and Malnutrition among Infants and Young Children Aged 6–23 Months in Rural Areas of China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.2.1. Anthropometry
2.2.2. Questionnaires
2.3. Grouping Criterion
2.4. Outcome Measures
2.5. Data Handling and Analysis
3. Results
3.1. Demographic Characteristics
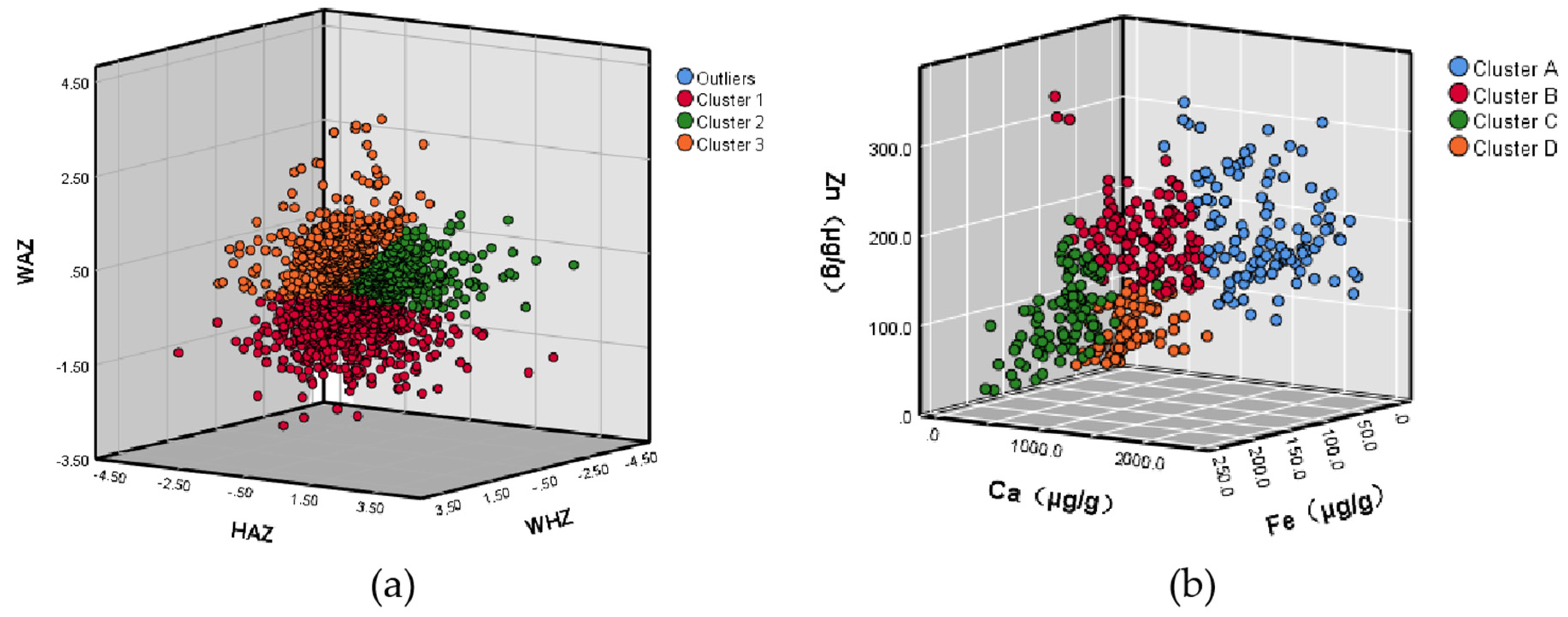
3.2. Grouping Results
3.3. Complementary Feeding Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Spearman Correlation | p | |
|---|---|---|
| Ca vs. Zn | 0.517 | <0.01 |
| Ca vs. Fe | −0.742 | <0.01 |
| Zn vs. Fe | −0.461 | <0.01 |
References
- Li, Z.; Kim, R.; Vollmer, S.; Subramanian, S.V. Factors Associated with Child Stunting, Wasting, and Underweight in 35 Low- and Middle-Income Countries. JAMA Netw. Open 2020, 3, e203386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 19 January 2022).
- United Nations Children’s Fund (UNICEF); World Health Organization; International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2021 Edition of the Joint Child Malnutrition Estimates. Available online: https://data.unicef.org/resources/jme-report-2021 (accessed on 19 January 2022).
- Prado, E.L.; Dewey, K.G. Nutrition and Brain Development in Early Life. Nutr. Rev. 2014, 72, 267–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Health Commission of the People’s Republic of China. Assessment for Growth Status of Children under 5 Years of Age. Available online: http://www.nhc.gov.cn/wjw/yingyang/201308/5d64ff7a2a044f34b4564963a20857c9.shtml (accessed on 19 March 2022).
- Shi, Y.; Li, L.; Yin, S. Malnutrition Prevalence in Children Aged 0–5 Years and Complementary Feeding Status for Infants and Young Children in China. Chin. J. Woman Child Health Res. 2021, 32, 1817–1821. [Google Scholar]
- Bhutta, Z.A.; Berkley, J.A.; Bandsma, R.H.J.; Kerac, M.; Trehan, I.; Briend, A. Severe Childhood Malnutrition. Nat. Rev. Dis. Primers 2017, 3, 17067. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the Double Burden of Malnutrition and the Changing Nutrition Reality. Lancet 2020, 395, 65–74. [Google Scholar]
- Zhang, Y.; Huang, X.; Yang, Y.; Liu, X.; Yang, C.; Wang, A.; Wang, Y.; Zhou, H. Double Burden of Malnutrition among Children under 5 in Poor Areas of China. PLoS ONE 2018, 13, e0204142. [Google Scholar] [CrossRef]
- Okubo, T.; Janmohamed, A.; Topothai, C.; Blankenship, J.L. Risk Factors Modifying the Double Burden of Malnutrition of Young Children in Thailand. Matern. Child Nutr. 2020, 16 (Suppl. 2), e12910. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Agosti, M.; The MeNu Group. Nutrition in the First 1000 Days: Ten Practices to Minimize Obesity Emerging from Published Science. Int. J. Environ. Res. Public Health 2017, 14, 1491. [Google Scholar] [CrossRef] [Green Version]
- Mameli, C.; Mazzantini, S.; Zuccotti, G.V. Nutrition in the First 1000 Days: The Origin of Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 838. [Google Scholar] [CrossRef] [Green Version]
- National Health Commission of the People’s Republic of China. Health Management Technological Protocol under 6-Year-Old Children. Available online: http://www.nhc.gov.cn/wjw/pqt/201507/001fb92117774491aa62de9cf161ac29.shtml (accessed on 19 March 2022).
- United Nations Children’s Fund (UNICEF). Diets. Available online: https://data.unicef.org/topic/nutrition/diets (accessed on 19 January 2022).
- The State of the World’s Children 2019. Children, Food and Nutrition: Growing Well in a Changing World; Unicef: New York, NY, USA, 2019; Available online: https://www.unicef.org/reports/state-of-worlds-children-2019 (accessed on 21 April 2022).
- Ramírez-Luzuriaga, M.J.; Hoddinott, J.F.; Martorell, R.; Ramírez-Zea, M.; Stein, A.D. Early-Life Nutrition and Subsequent International Migration: A Prospective Study in Rural Guatemala. J. Nutr. 2021, 151, 716–721. [Google Scholar] [CrossRef]
- Bailey, R.L.; West, K.P., Jr.; Black, R.E. The Epidemiology of Global Micronutrient Deficiencies. Ann. Nutr. Metab. 2015, 66 (Suppl. 2), 22–23. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Arif, M.; Shah, A.A. Complementary Feeding Practices and Associated Factors among Children Aged 6–23 Months in Pakistan. PLoS ONE 2021, 16, e0247602. [Google Scholar] [CrossRef] [PubMed]
- United Nations Sustainable Development Goals. Goal 2: Zero Hunger. Available online: https://www.un.org/sustainabledevelopment/hunger (accessed on 19 January 2022).
- Liu, J.; Huo, J.; Sun, J.; Huang, J.; Gong, W.; Wang, O. Prevalence of Complementary Feeding Indicators and Associated Factors among 6- to 23-Month Breastfed Infants and Young Children in Poor Rural Areas of China. Front. Public Health 2021, 9, 691894. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Huo, J.; Liu, Z.; Sun, J.; Huang, J. Prevalence and Temporal Trend (2016–2018) of Anaemia among 6–23-Month-Old Infants and Young Children in China. Int. J. Environ. Res. Public Health 2021, 18, 2041. [Google Scholar] [CrossRef]
- Yu, I.-C.; Fang, J.-T.; Tsai, Y.-F. Exploring Demands of Hemodialysis Patients in Taiwan: A Two-Step Cluster Analysis. PLoS ONE 2020, 15, e0228259. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Who Child Growth Standards: Methods and Development. Available online: https://www.who.int/childgrowth/standards/technical_report/en/ (accessed on 19 January 2022).
- World Health Organization (WHO). Indicators for Assessing Infant and Young Child Feeding Practices. Part 1: Definitions; World Health Organization (WHO): Geneva, Switzerland, 2008; Available online: https://www.who.int/publications/i/item/9789241596664 (accessed on 21 April 2022).
- de Onis, M.; Blössner, M.; Borghi, E.; Morris, R.; Frongillo, E.A. Methodology for Estimating Regional and Global Trends of Child Malnutrition. Int. J. Epidemiol. 2004, 33, 1260–1270. [Google Scholar] [CrossRef] [Green Version]
- Melse-Boonstra, A. Bioavailability of Micronutrients from Nutrient-Dense Whole Foods: Zooming in on Dairy, Vegetables, and Fruits. Front. Nutr. 2020, 7, 101. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Nutrition Guidelines of Complementary Feeding for Infants and Toddlers. Available online: http://www.nhc.gov.cn/wjw/yingyang/202005/69faa104fdda4df18e51b5c117830488.shtml (accessed on 19 March 2022).
- Roager, H.M.; Vogt, J.K.; Kristensen, M.; Hansen, L.B.S.; Ibrügger, S. Whole Grain-Rich Diet Reduces Body Weight and Systemic Low-Grade Inflammation without Inducing Major Changes of the Gut Microbiome: A Randomised Cross-over Tria. Gut 2019, 68, 83–93. [Google Scholar] [CrossRef] [Green Version]
- Kirwan, J.P.; Malin, S.K.; Scelsi, A.R.; Kullman, E.L.; Navaneethan, S.D.; Pagadala, M.R. A Whole-Grain Diet Reduces Cardiovascular Risk Factors in Overweight and Obese Adults: A Randomized Controlled Trial. J. Nutr. 2016, 146, 2244–2251. [Google Scholar] [CrossRef]
- Malin, S.K.; Kullman, E.L.; Scelsi, A.R.; Haus, J.M.; Filion, J.; Pagadala, M.R. A Whole-Grain Diet Reduces Peripheral Insulin Resistance and Improves Glucose Kinetics in Obese Adults: A Randomized-Controlled Trial. Metabolism 2018, 82, 111–117. [Google Scholar] [CrossRef]
- Petrikova, I. The Role of Complementary Feeding in India’s High Child Malnutrition Rates: Findings from a Comprehensive Analysis of Nfhs Iv (2015–2016) Data. Food Secur. 2021, 28, 1–28. [Google Scholar] [CrossRef] [PubMed]
- van der Crabben, S.N.; Heymans, H.S.; van Kempen, A.A.; Holman, R.; Sauerwein, H.P. Qualitative Malnutrition Due to Incorrect Complementary Feeding in Bush Negro Children in Suriname. Ned. Tijdschrift Voor Geneeskd. 2004, 148, 1093–1097. [Google Scholar] [PubMed]
- Nai, H.M.E.; Renyoet, B.S. Poor Dietary Diversity Is Associated with Stunting among Children 6–23 Months in Area of Mergangsan Public Health Center, Yogyakarta. J. Nutr. Sci. Vitaminol. 2020, 66, S398–S405. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.; Hendricks, A.E.; Krebs, N.F. A Meat- or Dairy-Based Complementary Diet Leads to Distinct Growth Patterns in Formula-Fed Infants: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2018, 107, 734–742. [Google Scholar] [CrossRef]
- Wang, J.; Wang, H.; Chang, S. The Influence of Malnutrition and Micronutrient Status on Anemic Risk in Children under 3 Years Old in Poor Areas in China. PLoS ONE 2015, 10, e0140840. [Google Scholar] [CrossRef]
- Gammoh, N.Z.; Rink, L. Zinc in Infection and Inflammation. Nutrients 2017, 9, 624. [Google Scholar] [CrossRef] [Green Version]
- Wessels, I.; Maywald, M.; Rink, L. Zinc as a Gatekeeper of Immune Function. Nutrients 2017, 9, 1286. [Google Scholar] [CrossRef] [Green Version]
- Knez, M.; Pantovic, A.; Zekovic, M.; Pavlovic, Z.; Glibetic, M.; Zec, M. Is There a Link between Zinc Intake and Status with Plasma Fatty Acid Profile and Desaturase Activities in Dyslipidemic Subjects? Nutrients 2019, 12, 93. [Google Scholar] [CrossRef] [Green Version]
- Maggini, S.; Pierre, A.; Calder, P.C. Immune Function and Micronutrient Requirements Change over the Life Course. Nutrients 2018, 10, 1531. [Google Scholar] [CrossRef] [Green Version]
- Society, C.N. The Dietary Guidelines for Chinese Residents (2016); People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- World Health Organization. Guideline: Use of Multiple Micronutrient Powders for Home Fortification of Foods Consumed by Infants and Children 6–23 Months of Age. 2011. Available online: https://apps.who.int/iris/handle/10665/44651 (accessed on 19 January 2022).
- Tam, E.; Keats, E.C.; Rind, F.; Das, J.K.; Bhutta, A.Z.A. Micronutrient Supplementation and Fortification Interventions on Health and Development Outcomes among Children under-Five in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 289. [Google Scholar] [CrossRef] [Green Version]
- Gernand, A.D.; Schulze, K.J.; Stewart, C.P.; West, K.P., Jr.; Christian, P. Micronutrient Deficiencies in Pregnancy Worldwide: Health Effects and Prevention. Nat. Rev. Endocrinol. 2016, 12, 274–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massari, M.; Novielli, C.; Mandò, C.; Francesco, S.D.; Porta, M.D.; Cazzola, R.; Panteghini, M. Multiple Micronutrients and Docosahexaenoic Acid Supplementation During Pregnancy: A Randomized Controlled Study. Nutrients 2020, 12, 2432. [Google Scholar] [CrossRef] [PubMed]
- Keats, E.C.; Haider, B.A.; Tam, E.; Bhutta, Z.A. Multiple-Micronutrient Supplementation for Women During Pregnancy. Cochrane Database Syst. Rev. 2019, 3, CD004905. [Google Scholar] [CrossRef] [PubMed]
- Dewey, K.G.; Wessells, K.R.; Arnold, C.D.; Prado, E.L.; Abbeddou, S.; Adu-Afarwuah, S.; Ali, H.; Arnold, B.F.; Ashorn, P. Characteristics That Modify the Effect of Small-Quantity Lipid-Based Nutrient Supplementation on Child Growth: An Individual Participant Data Meta-Analysis of Randomized Controlled Trials. Am. J. Clin. Nutr. 2021, 114 (Suppl. 1), 15S–42S. [Google Scholar] [CrossRef]
- Verhoef, H.; Teshome, E.; Prentice, A.M. Micronutrient Powders to Combat Anaemia in Young Children: Do They Work? BMC Med. 2018, 16, 7. [Google Scholar] [CrossRef] [Green Version]
- De-Regil, L.M.; Jefferds, M.E.D.; Peña-Rosas, J.P. Point-of-Use Fortification of Foods with Micronutrient Powders Containing Iron in Children of Preschool and School-Age. Cochrane Database Syst. Rev. 2017, 11, CD009666. [Google Scholar] [CrossRef]
- Li, Z.; Li, X.; Sudfeld, C.R.; Liu, Y.; Tang, K.; Huang, Y.; Fawzi, W. The Effect of the Yingyangbao Complementary Food Supplement on the Nutritional Status of Infants and Children: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2404. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Chang, S.; Zhao, L.; Yu, W.; Zhang, J.; Man, Q.; He, L. Effectiveness of Community-Based Complementary Food Supplement (Yingyangbao) Distribution in Children Aged 6–23 Months in Poor Areas in China. PLoS ONE 2017, 10, 1371. [Google Scholar] [CrossRef] [Green Version]
- Ballesteros, M.T.L.; Serrano, I.N.; Álvarez, S.I. Reference Levels of Trace Elements in Hair Samples from Children and Adolescents in Madrid, Spain. J. Trace Elem. Med. Biol. 2017, 43, 113–120. [Google Scholar] [CrossRef]
| Characteristics | Mean or Frequency (SD or Rate) |
|---|---|
| IYC | |
| Age, month | 15.6 (5.4) |
| Male, n (%) | 795 (52.1) |
| Birth Length, cm | 50.2 (1.7) |
| Birth Weight, g | 3290.4 (501.2) |
| Mother | |
| Age, year | 28.9 (5.2) |
| Han, n (%) | 907 (59.4) |
| Education | |
| Primary School or Below, n (%) | 171 (11.2) |
| Middle School, n (%) | 992 (65.1) |
| High School or Above, n (%) | 361 (20.1) |
| Domestically Unemployed, n (%) | 722 (47.4) |
| Father | |
| Age, year | 31.3 (5.5) |
| Han, n (%) | 948 (62.1) |
| Education | |
| Primary School or Below, n (%) | 133 (8.7) |
| Middle School, n (%) | 1009 (66.2) |
| High School or Above, n (%) | 382 (25.1) |
| Domestically Unemployed, n (%) | 40 (2.6) |
| Caregiver | |
| Parents as main caregivers, n (%) | 1151 (75.4) |
| Education | |
| Primary School or Below, n (%) | 422 (28.0) |
| Middle School, n (%) | 847 (55.6) |
| High School or Above, n (%) | 167 (16.4) |
| Domestically Unemployed, n (%) | 898 (59.0) |
| Clusters | Distribution n(%) | Z-Score x ± SD | The Prevalence of Malnutrition n (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LAZ | WAZ | WLZ | Stunting | Underweight | Wasting | Overweight | ||
| 1 | 680 (44.9) | −1.06 ± 0.89 | −1.00 ± 0.59 | −0.63 ± 0.81 | 98 (14.4) | 44 (6.5) | 44 (6.5) | 0 (0.0) |
| 2 | 377 (24.9) | 0.99 ± 0.82 | 0.33 ± 0.46 | −0.17 ± 0.56 | 0 (0.0) | 0 (0.0) | 2 (0.5) | 0 (0.0) |
| 3 | 458 (30.2) | −0.01 ± 1.01 | 0.92 ± 0.80 | 1.25 ± 0.68 | 13 (2.8) | 0 (0.0) | 0 (0.0) | 56 (12.2) |
| Total | 1515 (100.0) | −0.23 ± 1.23 | −0.09 ± 1.06 | 0.05 ± 1.08 | 111 (7.3) | 44 (2.9) | 46 (3.0) | 56 (3.7) |
| Clusters | Distribution n(%) | Micronutrient in Hair M(Q) | ||
|---|---|---|---|---|
| Ca (µg/g) | Fe (µg/g) | Zn (µg/g) | ||
| A | 114 (26.6) | 1462.35 (598.82) | 24.47 (20.50) | 173.47 (78.92) |
| B | 125 (29.2) | 607.50 (385.88) | 61.50 (35.79) | 164.48 (48.88) |
| C | 103 (24.1) | 248.94 (166.60) | 115.26 (35.60) | 92.33 (49.68) |
| D | 86 (20.1) | 445.70 (219.79) | 66.58 (32.72) | 59.78 (43.65) |
| Total | 428 (100.0) | 550.10 (748.38) | 62.94 (57.55) | 132.86 (93.01) |
| Clusters | Total | p | |||
|---|---|---|---|---|---|
| 1 (Undernutrition) | 2 (Fine) | 3 (Overweight) | |||
| Groups of CF | |||||
| Grains, roots, and tubers | 651 (96.9) | 355 (95.9) | 410 (92.6) | 1416 (95.4) | <0.01 |
| Vitamin-A-rich fruits and vegetables | 429 (63.9) | 248 (67.0) | 262 (59.1) | 939 (63.3) | 0.06 |
| Other fruits and vegetables | 448 (66.8) | 248 (67.0) | 281 (63.4) | 977 (65.8) | 0.44 |
| Fresh foods | 392 (58.3) | 197 (53.2) | 229 (51.7) | 818 (55.1) | 0.06 |
| Eggs | 322 (47.9) | 185 (50.0) | 216 (48.8) | 723 (48.7) | 0.81 |
| Dairy products | 397 (58.4) | 257 (68.2) | 261 (57.0) | 915 (60.4) | <0.01 |
| Legumes and nuts | 288 (42.9) | 145 (39.2) | 176 (39.7) | 609 (41.0) | 0.42 |
| Structure of CF | |||||
| ISSF (6–8 months) | 56 (86.2) | 39 (86.7) | 60 (83.3) | 155 (85.2) | 0.85 |
| MDD | 484 (71.2) | 274 (72.9) | 285 (62.2) | 1043 (68.9) | <0.01 |
| MMF | 469 (78.3) | 274 (81.5) | 297 (74.3) | 1040 (77.9) | 0.05 |
| MAD | 251 (49.5) | 157 (49.7) | 145 (39.4) | 553 (46.4) | <0.01 |
| Clusters | Total | p | ||||
|---|---|---|---|---|---|---|
| A (High Ca and Low Fe) | B (Fine) | C (Low Ca, Low Zn, and High Fe) | D (Low Ca and Low Zn) | |||
| Groups of CF | ||||||
| Grains, roots, and tubers | 101 (93.5) | 115 (95.0) | 97 (98.0) | 78 (94.0) | 391 (95.1) | 0.43 |
| Vitamin-A-rich fruits and vegetables | 58 (53.7) | 65 (53.7) | 58 (59.2) | 52 (62.7) | 233 (56.8) | 0.52 |
| Other fruits and vegetables | 67 (62.0) | 92 (76.0) | 67 (68.4) | 54 (65.1) | 280 (68.3) | 0.13 |
| Fresh foods | 64 (59.3) | 63 (52.1) | 51 (51.5) | 41 (49.4) | 219 (53.3) | 0.52 |
| Eggs | 52 (48.1) | 61 (50.4) | 44 (44.4) | 38 (45.8) | 195 (47.4) | 0.84 |
| Dairy products | 73 (64.0) | 82 (65.6) | 63 (61.2) | 51 (59.3) | 269 (62.9) | 0.79 |
| Legumes and nuts | 43 (39.8) | 55 (45.5) | 48 (48.5) | 44 (53.0) | 190 (46.2) | 0.31 |
| Structure of CF | ||||||
| ISSF (6–8 months) | 14 (70.0) | 10 (83.3) | 4 (66.7) | 8 (72.7) | 36 (73.5) | 0.83 |
| MDD | 72 (63.2) | 87 (69.6) | 66 (64.1) | 60 (69.8) | 285 (66.6) | 0.62 |
| MMF | 75 (75.8) | 98 (84.5) | 74 (77.9) | 53 (73.6) | 300 (78.5) | 0.27 |
| MAD | 40 (46.0) | 56 (52.8) | 28 (37.8) | 30 (44.8) | 154 (46.1) | 0.26 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, J.; Gong, Z.; Wang, Y.; Huo, J.; Zhuo, Q. Complementary Feeding and Malnutrition among Infants and Young Children Aged 6–23 Months in Rural Areas of China. Nutrients 2022, 14, 1807. https://doi.org/10.3390/nu14091807
Feng J, Gong Z, Wang Y, Huo J, Zhuo Q. Complementary Feeding and Malnutrition among Infants and Young Children Aged 6–23 Months in Rural Areas of China. Nutrients. 2022; 14(9):1807. https://doi.org/10.3390/nu14091807
Chicago/Turabian StyleFeng, Jing, Zhaolong Gong, Yongjun Wang, Junsheng Huo, and Qin Zhuo. 2022. "Complementary Feeding and Malnutrition among Infants and Young Children Aged 6–23 Months in Rural Areas of China" Nutrients 14, no. 9: 1807. https://doi.org/10.3390/nu14091807
APA StyleFeng, J., Gong, Z., Wang, Y., Huo, J., & Zhuo, Q. (2022). Complementary Feeding and Malnutrition among Infants and Young Children Aged 6–23 Months in Rural Areas of China. Nutrients, 14(9), 1807. https://doi.org/10.3390/nu14091807







