Phase Angle Is a Stronger Predictor of Hospital Outcome than Subjective Global Assessment—Results from the Prospective Dessau Hospital Malnutrition Study
Abstract
1. Introduction
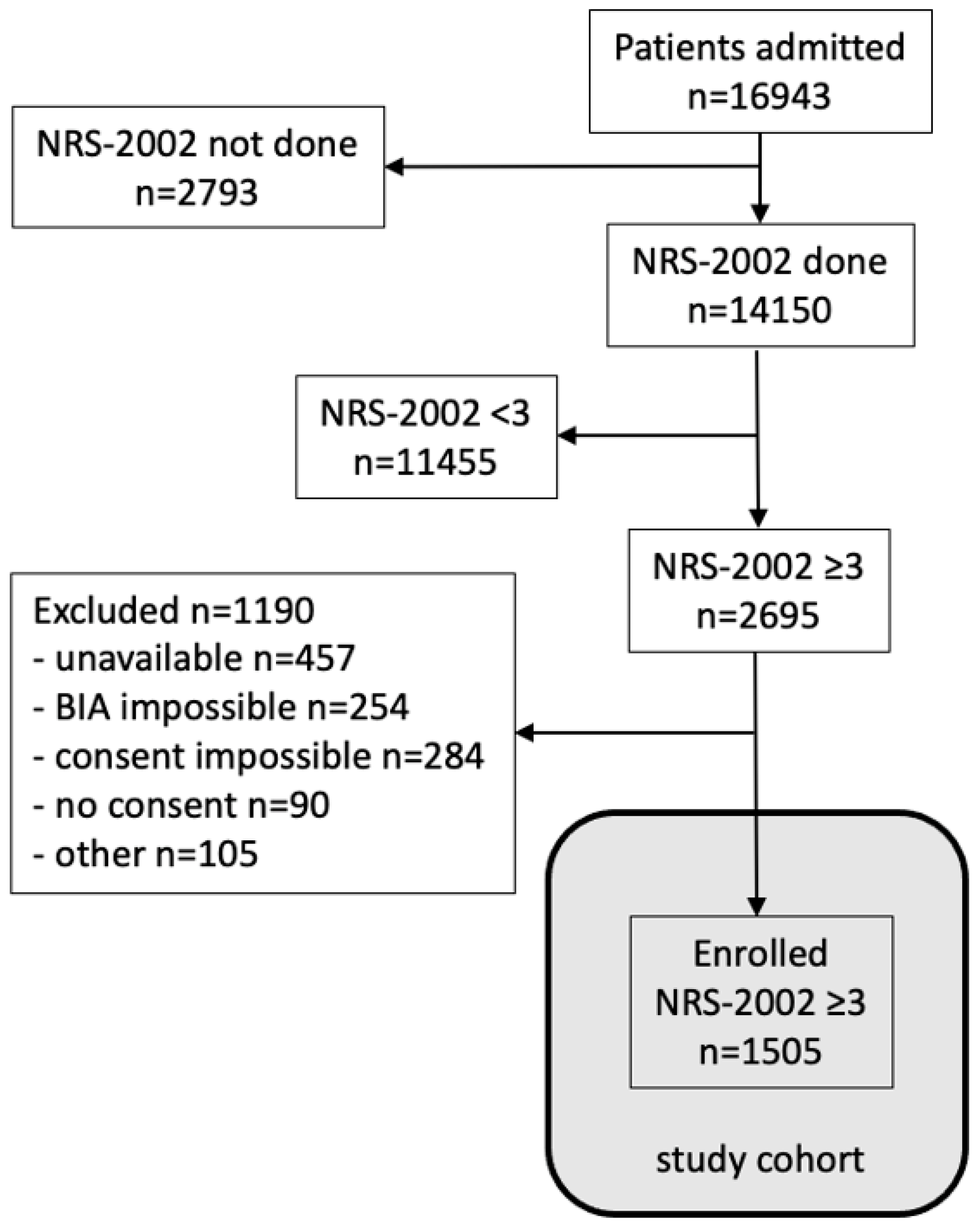
2. Patients and Methods
2.1. Patients
2.2. Estimation of Sample Size
2.3. Data Collection
2.4. Malnutrition Risk Screening
2.5. Subjective Global Assessment (SGA)
2.6. Phase Angle (PhA)
2.7. PANDORA-Score
2.8. Inflammatory Status
2.9. Statistical Analysis
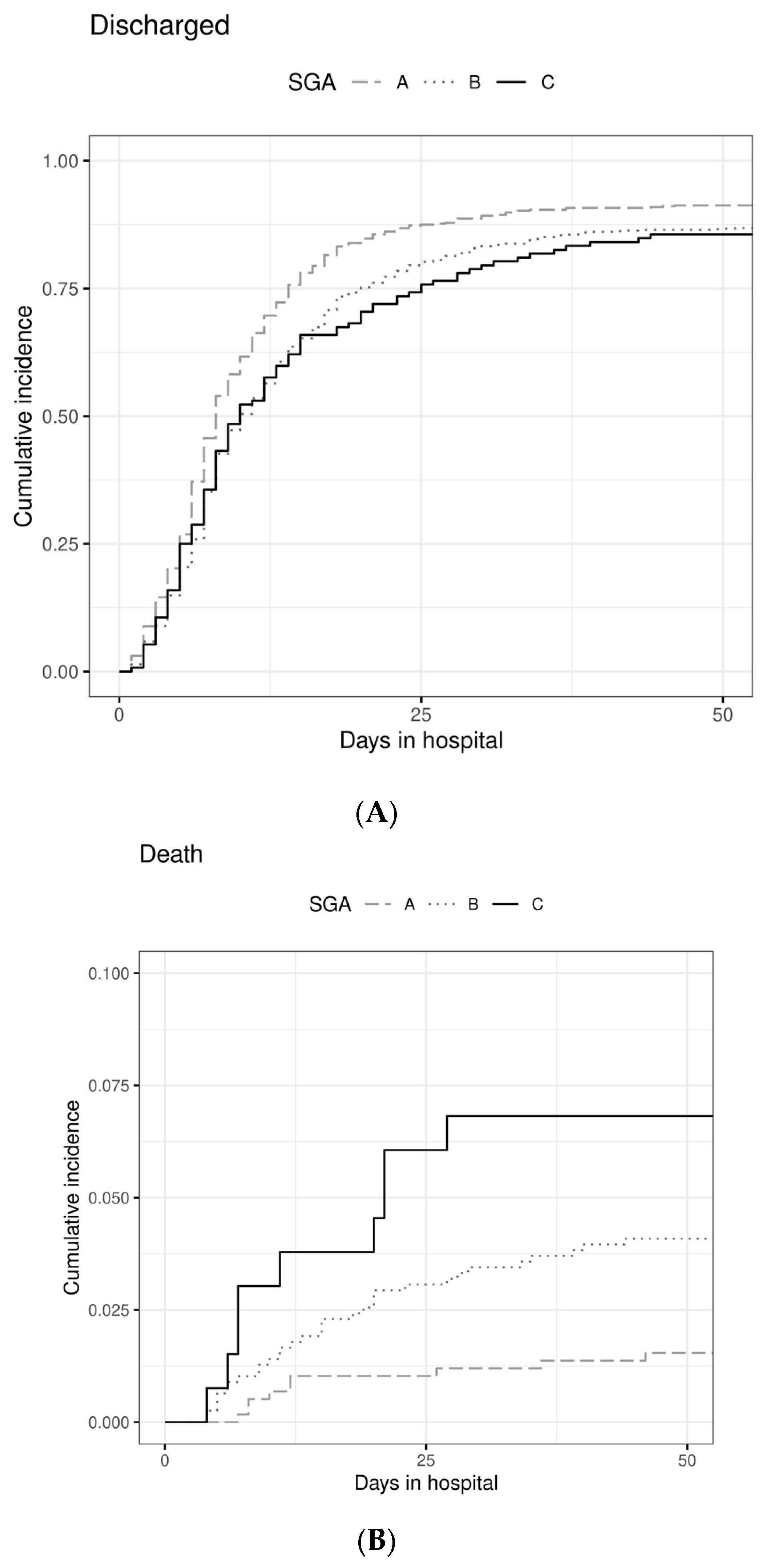
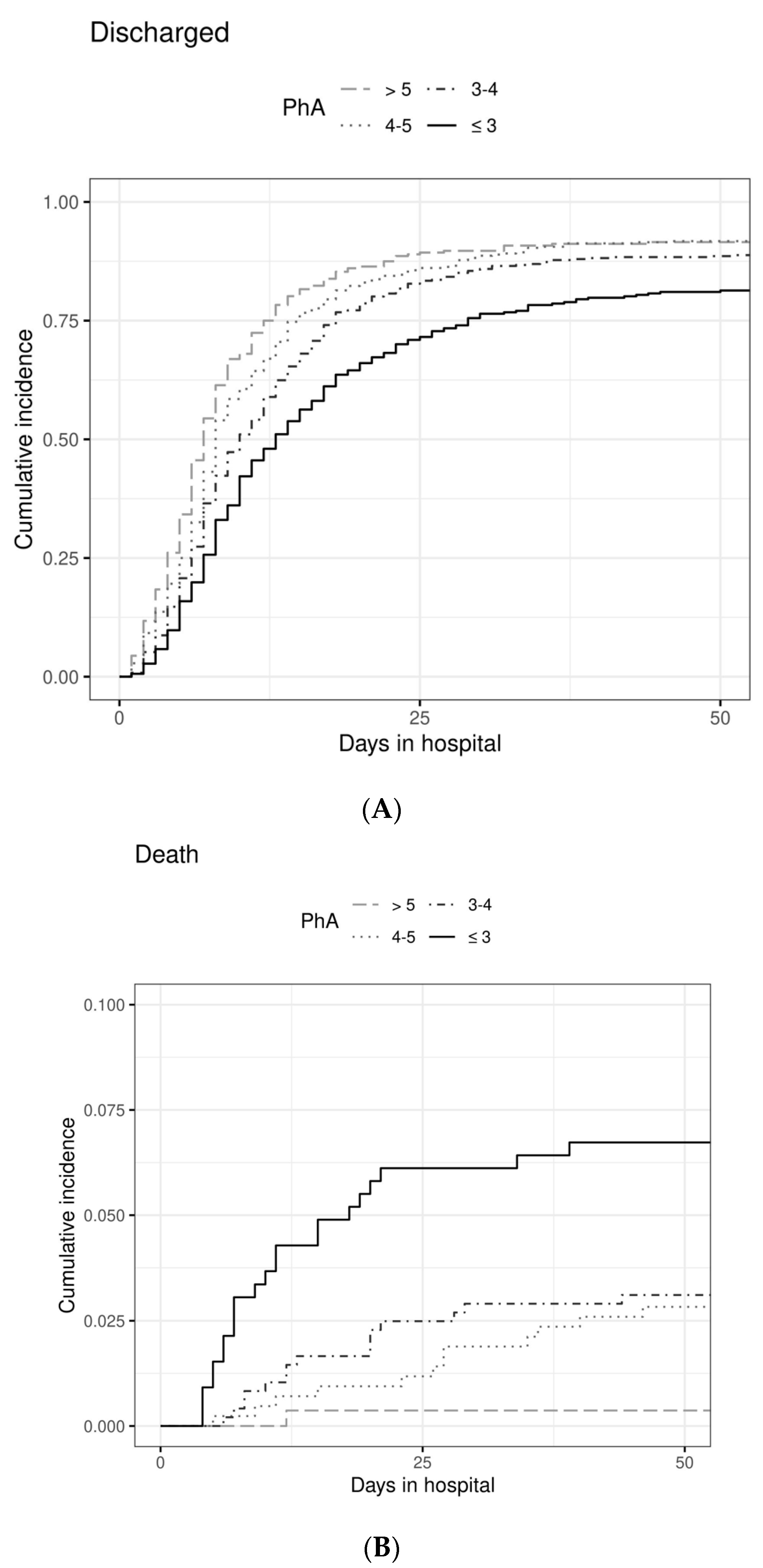
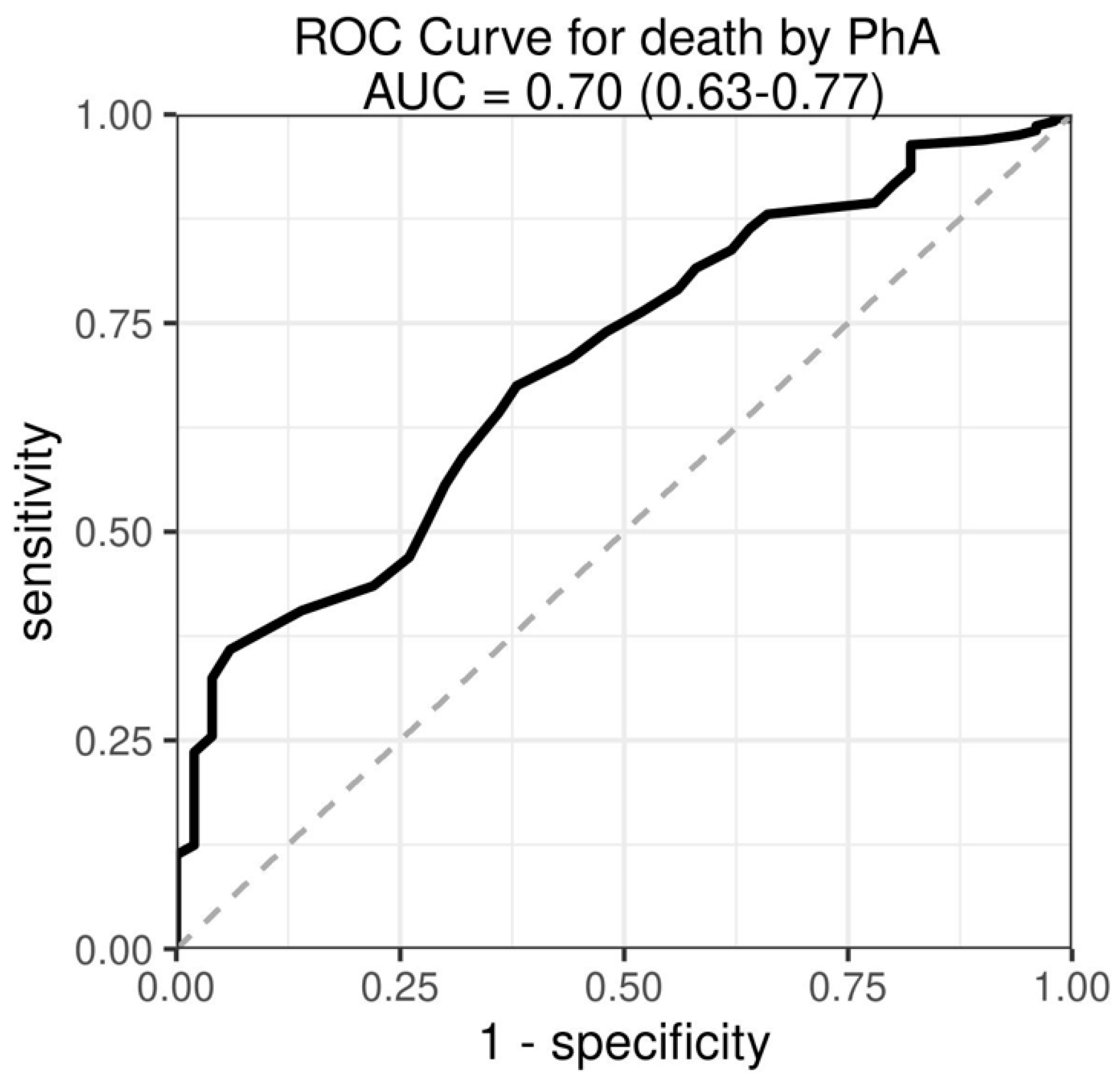
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Correia, M.I.; Waitzberg, D.L. The impact of malnutrition in morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin. Nutr. 2003, 22, 235–239. [Google Scholar] [CrossRef]
- Pirlich, M.; Schütz, T.; Norman, K.; Gastell, S.; Lübke, H.J.; Bischoff, S.C.; Bolder, U.; Frieling, T.; Güldenzoph, H.; Hahn, K.; et al. The German hospital malnutrition study. Clin. Nutr. 2006, 25, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Correia, M.I.T.D.; Perman, M.I.; Waitzberg, D.L. Hospital malnutrition in Latin America: A systematic review. Clin. Nutr. 2017, 36, 958–967. [Google Scholar] [CrossRef]
- Curtis, L.J.; Bernier, P.; Jeejeebhoy, K.; Allard, J.; Duerksen, D.; Gramlich, L.; Laporte, M.; Keller, H.H. Costs of hospital mal-nutrition. Clin. Nutr. 2017, 36, 1391–1396. [Google Scholar] [CrossRef]
- Sauer, A.C.; Goates, S.; Malone, A.; Mogensen, K.M.; Gewirtz, G.; Sulz, I.; Moick, S.; Laviano, A.; Hiesmayr, M. Prevalence of Malnutrition Risk and the Impact of Nutrition Risk on Hospital Outcomes: Results From nutritionDay in the U.S. J. Parenter. Enteral Nutr. 2019, 43, 918–926. [Google Scholar] [CrossRef]
- Inciong, J.F.B.; Chaudhary, A.; Hsu, H.-S.; Joshi, R.; Seo, J.-M.; Trung, L.V.; Ungpinitpong, W.; Usman, N. Hospital malnu-trition in northeast and southeast Asia: A systematic literature review. Clin. Nutr. ESPEN 2020, 39, 30–45. [Google Scholar] [CrossRef]
- Hiesmayr, M.; Schindler, K.; Pernicka, E.; Schuh, C.; Schoeniger-Hekele, A.; Bauer, P.; Laviano, A.; Lovell, A.D.; Mouhieddine, M.; Schuetz, M.; et al. Decreased food intake is a risk factor for mortality in hospitalised patients: The NutritionDay survey 2006. Clin. Nutr. 2009, 28, 484–492. [Google Scholar] [CrossRef]
- Blackburn, G.L.; Bistrian, B.R.; Maini, B.S.; Schlamm, H.T.; Smith, M.F. Nutritional and metabolic assessment of the hospitalized patient. J. Parenter. Enteral Nutr. 1977, 1, 11–22. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; McManus, C.; Smith, J.; Stevens, V.; Nixon, D.W. Anthropometric measurement of muscle mass: Revised equations for calculating bone-free arm muscle area. Am. J. Clin. Nutr. 1982, 36, 680–690. [Google Scholar] [CrossRef]
- Church, J.M.; Hill, G.L. Assessing the efficacy of intravenous nutrition in general surgical patients: Dynamic nutritional as-sessment with plasma proteins. J. Parenter. Enteral Nutr. 1987, 11, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Klidjian, A.M.; Foster, K.J.; Kammerling, R.M.; Cooper, A.; Karran, S.J. Relation of anthropometric and dynamometric variables to serious postoperative complications. Br. Med. J. 1980, 281, 899–901. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Detsky, A.S.; Baker, J.P.; Mendelson, R.A.; Wolman, S.L.; Wesson, D.A.; Jeejeebhoy, K.N. Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: Methodology and comparisons. J. Parenter. Enteral Nutr. 1984, 8, 153–159. [Google Scholar] [CrossRef]
- Waitzberg, D.L.; Caiaffa, W.T.; Correia, M.I. Hospital malnutrition: The Brazilian national survey (IBRANUTRI): A study of 4000 patients. Nutrition 2001, 17, 573–580. [Google Scholar] [CrossRef]
- Jeejeebhoy, K.N.; Keller, H.; Gramlich, L.; Allard, J.P.; Laporte, M.; Duerksen, D.R.; Payette, H.; Bernier, P.; Vesnaver, E.; Davidson, B.; et al. Nutritional assessment: Comparison of clinical assessment and objective variables for the prediction of length of hospital stay and readmission. Am. J. Clin. Nutr. 2015, 101, 956–965. [Google Scholar] [CrossRef]
- Buzby, G.P.; Mullen, J.L.; Matthews, D.C.; Hobbs, C.L.; Rosato, E.F. Prognostic nutritional index in gastrointestinal surgery. Am. J. Surg. 1980, 139, 160–167. [Google Scholar] [CrossRef]
- Wolinsky, F.D.; Coe, R.M.; McIntosh, W.A.; Kubena, K.S.; Prendergast, J.M.; Chavez, M.N.; Miller, D.K.; Romeis, J.C.; Landmann, W.A. Progress in the development of a nutritional risk index. J. Nutr. 1990, 120 (Suppl. S11), 1549–1553. [Google Scholar] [CrossRef]
- Mendenhall, C.L.; Moritz, T.E.; Roselle, G.A.; Morgan, T.R.; Nemchausky, B.A.; Tamburro, C.H.; Schiff, E.R.; McClain, C.J.; Marsano, L.S.; Allen, J.I.; et al. A study of oral nutritional support with oxandrolone in malnourished patients with alcoholic hepatitis: Results of a Department of Veterans Affairs cooperative study. Hepatology 1993, 17, 564–576. [Google Scholar] [CrossRef]
- Guigoz, Y.; Vellas, B.J.; Garry, P.J. Mini nutritional assessment: A practical tool for grading the nutritional state of elderly patients. Facts. Res. Gerontol. 1994, 4 (Suppl. S2), 15–59. [Google Scholar]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.; et al. Diagnostic criteria for malnutrition—An ESPEN Consensus Statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Soeters, P.B.; Reijven, P.L.M.; van Bokhorst-de van der Schueren, M.A.E.; Schols, J.M.G.A.; Halfens, R.J.G.; Meijers, J.M.M.; van Gemert, W.G. A rational approach to nutritional assessment. Clin. Nutr. 2008, 27, 706–716. [Google Scholar] [CrossRef] [PubMed]
- Lukaski, H.C.; Kyle, U.G.; Kondrup, J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: Phase angle and impedance ratio. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, M.C.G.; Barros, A.J.D. Bioelectrical impedance analysis in clinical practice: A new perspective on its use beyond body composition equations. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Zocher, D.; Bosy-Westphal, A.; Szramek, A.; Scheufele, R.; Smoliner, C.; Pirlich, M. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am. J. Clin. Nutr. 2010, 92, 612–619. [Google Scholar] [CrossRef]
- Bosy-Westphal, A.; Danielzik, S.; Dörhöfer, R.-P.; Later, W.; Wiese, S.; Müller, M.J. Phase angle from bioelectrical impedance analysis: Population reference values by age, sex, and body mass index. J. Parenter. Enteral Nutr. 2006, 30, 309–316. [Google Scholar] [CrossRef]
- Norman, K.; Stobäus, N.; Pirlich, M.; Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis--clinical relevance and applicability of impedance parameters. Clin. Nutr. 2012, 31, 854–861. [Google Scholar] [CrossRef]
- Campa, F.; Toselli, S.; Mazzilli, M.; Gobbo, L.A.; Coratella, G. Assessment of Body Composition in Athletes: A Narrative Review of Available Methods with Special Reference to Quantitative and Qualitative Bioimpedance Analysis. Nutrients 2021, 13, 1620. [Google Scholar] [CrossRef]
- Barrea, L.; Muscogiuri, G.; Pugliese, G.; Laudisio, D.; de Alteriis, G.; Graziadio, C.; Colao, A.; Savastano, S. Phase Angle as an Easy Diagnostic Tool of Meta-Inflammation for the Nutritionist. Nutrients 2021, 13, 1446. [Google Scholar] [CrossRef]
- Lukaski, H.C.; Vega Diaz, N.; Talluri, A.; Nescolarde, L. Classification of Hydration in Clinical Conditions: Indirect and Direct Approaches Using Bioimpedance. Nutrients 2019, 11, 809. [Google Scholar] [CrossRef]
- Di Vincenzo, O.; Marra, M.; Di Gregorio, A.; Pasanisi, F.; Scalfi, L. Bioelectrical impedance analysis (BIA) -derived phase angle in sarcopenia: A systematic review. Clin. Nutr. 2021, 40, 3052–3061. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Ando, K.; Kobayashi, K.; Seki, T.; Hamada, T.; Machino, M.; Ota, K.; Morozumi, M.; Kanbara, S.; Ito, S.; et al. Low Bioelectrical Impedance Phase Angle Is a Significant Risk Factor for Frailty. Biomed. Res. Int. 2019, 2019, 6283153. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Genton, L.; Pichard, C. Low phase angle determined by bioelectrical impedance analysis is associated with mal-nutrition and nutritional risk at hospital admission. Clin. Nutr. 2013, 32, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Jansen, A.K.; Gattermann, T.; da Silva Fink, J.; Saldanha, M.F.; Dias Nascimento Rocha, C.; de Souza Moreira, T.H.; Silva, F.M. Low standardized phase angle predicts prolonged hospitalization in critically ill patients. Clin. Nutr. ESPEN. 2019, 34, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Del Giorno, R.; Quarenghi, M.; Stefanelli, K.; Capelli, S.; Giagulli, A.; Quarleri, L.; Stehrenberger, D.; Ossola, N.; Monotti, R.; Gabutti, L. Nutritional Risk Screening and Body Composition in COVID-19 Patients Hospitalized in an Internal Medicine Ward. Int. J. Gen. Med. 2020, 13, 1643–1651. [Google Scholar] [CrossRef] [PubMed]
- Del Giorno, R.; Quarenghi, M.; Stefanelli, K.; Rigamonti, A.; Stanglini, C.; De Vecchi, V.; Gabutti, L. Phase angle is associated with length of hospital stay, readmissions, mortality, and falls in patients hospitalized in internal-medicine wards: A retro-spective cohort study. Nutrition 2021, 85, 111068. [Google Scholar] [CrossRef]
- Cornejo-Pareja, I.; Vegas-Aguilar, I.M.; García-Almeida, J.M.; Bellido-Guerrero, D.; Talluri, A.; Lukaski, H.; Tinahones, F.J. Phase angle and standardized phase angle from bioelectrical impedance measurements as a prognostic factor for mortality at 90 days in patients with COVID-19: A longitudinal cohort study. Clin. Nutr. 2021; in press. [Google Scholar] [CrossRef]
- Genton, L.; Herrmann, F.R.; Spörri, A.; Graf, C.E. Association of mortality and phase angle measured by different bioelectrical impedance analysis (BIA) devices. Clin. Nutr. 2018, 37, 1066–1069. [Google Scholar] [CrossRef]
- Viertel, M.; Bock, C.; Reich, M.; Löser, S.; Plauth, M. Performance of CT-based low skeletal muscle index, low mean muscle attenuation, and bioelectric impedance derived low phase angle in the detection of an increased risk of nutrition related mortality. Clin. Nutr. 2019, 38, 2375–2380. [Google Scholar] [CrossRef]
- Garlini, L.M.; Alves, F.D.; Ceretta, L.B.; Perry, I.S.; Souza, G.C.; Clausell, N.O. Phase angle and mortality: A systematic review. Eur. J. Clin. Nutr. 2019, 73, 495–508. [Google Scholar] [CrossRef]
- Kondrup, J.; Allison, S.P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN Guidelines for nutrition screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Hiesmayr, M.; Frantal, S.; Schindler, K.; Themessl-Huber, M.; Mouhieddine, M.; Schuh, C.; Pernicka, E.; Schneider, S.; Singer, P.; Ljunqvist, O.; et al. The Patient—And Nutrition-Derived Outcome Risk Assessment Score (PANDORA): Development of a Simple Predictive Risk Score for 30-Day In-Hospital Mortality Based on Demographics, Clinical Observation, and Nutrition. PLoS ONE 2015, 10, e0127316. [Google Scholar] [CrossRef] [PubMed]
- Merker, M.; Felder, M.; Gueissaz, L.; Bolliger, R.; Tribolet, P.; Kaegi-Braun, N.; Gomes, F.; Hoess, C.; Pavlicek, V.; Bilz, S.; et al. Association of Baseline Inflammation With Effectiveness of Nutritional Support Among Patients With Disease-Related Mal-nutrition: A Secondary Analysis of a Randomized Clinical Trial. JAMA. Netw. Open 2020, 3, e200663. [Google Scholar] [CrossRef] [PubMed]
- Pichard, C.; Kyle, U.G.; Morabia, A.; Perrier, A.; Vermeulen, B.; Unger, P. Nutritional assessment: Lean body mass depletion at hospital admission is associated with an increased length of stay. Am. J. Clin. Nutr. 2004, 79, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Elwyn, D.H.; Bryan-Brown, C.W.; Shoemaker, W.C. Nutritional aspects of water dislocation in postoperative and depleted patients. Ann. Surg. 1975, 182, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Shizgal, H.M.; Spanier, A.H.; Kurtz, R.S. Effect of parenteral nutrition on body composition in the critically ill patient. Am. J. Surg. 1976, 131, 156–161. [Google Scholar] [CrossRef]
- Starker, P.M.; La Sala, P.A.; Askanazi, J.; Todd, G.; Hensle, T.W.; Kinney, J.M. The influence of preoperative total parenteral nutrition upon morbidity and mortality. Surg. Gynecol. Obstet. 1986, 162, 569–574. [Google Scholar]
- Cereda, E.; Caraccia, M.; Klersy, C.; Cappello, S.; Turri, A.; Borioli, V.; Stobäus, N.; Giannoni, A.; Arcaini, L.; Benazzo, M.; et al. Validation of a new prognostic body composition parameter in cancer patients. Clin. Nutr. 2021, 40, 615–623. [Google Scholar] [CrossRef]
- Norman, K.; Wirth, R.; Neubauer, M.; Eckardt, R.; Stobäus, N. The bioimpedance phase angle predicts low muscle strength, impaired quality of life, and increased mortality in old patients with cancer. J. Am. Med. Dir. Assoc. 2015, 16, 173.e17–173.e22. [Google Scholar] [CrossRef]
- Kyle, U.G.; Soundar, E.P.; Genton, L.; Pichard, C. Can phase angle determined by bioelectrical impedance analysis assess nutritional risk? A comparison between healthy and hospitalized subjects. Clin. Nutr. 2012, 31, 875–881. [Google Scholar] [CrossRef]
- Stobäus, N.; Pirlich, M.; Valentini, L.; Schulzke, J.D.; Norman, K. Determinants of bioelectrical phase angle in disease. Br. J. Nut. 2012, 107, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Player, E.L.; Morris, P.; Thomas, T.; Chan, W.Y.; Vyas, R.; Dutton, J.; Tang, J.; Alexandre, L.; Forbes, A. Bioelectrical impedance analysis (BIA)-derived phase angle (PA) is a practical aid to nutritional assessment in hospital in-patients. Clin. Nutr. 2019, 38, 1700–1706. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, S.; Gilliland, J.; O’Connor, C.; Chesworth, B.; Madill, J. Is phase angle an appropriate indicator of malnutrition in different disease states? A systematic review. Clin. Nutr. ESPEN 2019, 29, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, M.C.; Barros, A.J.; Wang, J.; Heymsfield, S.B.; Pierson, R.N., Jr. Bioelectrical impedance analysis: Population reference values for phase angle by age and sex. Am. J. Clin. Nutr. 2005, 82, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Kaegi-Braun, N.; Tribolet, P.; Baumgartner, A.; Fehr, R.; Baechli, V.; Geiser, M.; Deiss, M.; Gomes, F.; Kutz, A.; Hoess, C.; et al. Value of handgrip strength to predict clinical outcomes and therapeutic response in malnourished medical inpatients: Sec-ondary analysis of a randomized controlled trial. Am. J. Clin. Nutr. 2021, 114, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Akamatsu, Y.; Kusakabe, T.; Arai, H.; Yamamoto, Y.; Nakao, K.; Ikeue, K.; Ishihara, Y.; Tagami, T.; Yasoda, A.; Ishii, K.; et al. Phase angle from bioelectrical impedance analysis is a useful indicator of muscle quality. J. Cachexia. Sar-copenia. Muscle. 2022, 13, 180–189. [Google Scholar] [CrossRef]
- Felder, S.; Lechtenboehmer, C.; Bally, M.; Fehr, R.; Deiss, M.; Faessler, L.; Kutz, A.; Steiner, D.; Rast, A.C.; Laukemann, S. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015, 31, 1385–1393. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nu-trition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar]

| n | 1.505 |
|---|---|
| age [years; median (IQR)] | 76 (66–81) |
| female [n (%)] | 782 (52%) |
| male [n (%)] | 723 (48%) |
| height [mean ± SD] | 167.8 ± 9.4 * |
| weight [mean ± SD] | 69.4 ± 17.1 * |
| BMI [mean ± SD] | 24.6 ± 5.5 * |
| weight gain [n (%)] | 208 (14%) |
| weight unchanged [n (%)] | 259 (18%) |
| weight loss (0–5%] [n (%)] | 312 (22%) |
| weight loss (5–10%] [n (%)] | 309 (21%) |
| weight loss > 10% [n (%)] | 352 (24%) |
| weight loss missing | 65 (4%) |
| SGA A [n (%)] | 584 (39%) |
| SGA B [n (%)] | 783 (52%) |
| SGA C [n (%)] | 131 (9%) |
| SGA missing | 6 (4%) |
| n | 1.505 |
|---|---|
| phase angle percentile not defined due to BMI < 18.5 | 163 (11%) |
| phase angle [°; median (IQR)] | 4.0 (3.2–4.7) |
| phase angle ≥ 5th perc [n (%)] | 565 (38%) |
| phase angle < 5th perc [n (%)] | 777 (52%) |
| n | 1.505 | |
|---|---|---|
| ICD-10 | n (%) | |
| A–B | infections | 78 (5%) |
| C–D50 | neoplasms | 356 (24%) |
| D50–D89 | blood, blood-forming organs | 72 (5%) |
| E | endocrine | 35 (2%) |
| F | mental | 5 (0%) |
| G | nervous system | 39 (3%) |
| H00–59 | eye | 3 (0%) |
| H60–95 | ear | 8 (1%) |
| I | circulatory | 176 (12%) |
| J | respiratory | 110 (7%) |
| K | digestive | 286 (19%) |
| L | skin | 15 (1%) |
| M | musculoskeletal | 60 (4%) |
| N | genitourinary | 62 (4%) |
| P | pregnancy | 2 (0%) |
| Q | malformations | 1 (0%) |
| R | abnormal findings | 65 (4%) |
| S-T | injury, poison | 103 (7%) |
| Z | factors from health services | 3 (0%) |
| missing | 25 (2%) |
| Model I | Model II (Including PhA) | Model III (Including PhA and CRP) | ||
|---|---|---|---|---|
| Variable | n (%) | HR [95%CI] | HR [95%CI] | HR [95%CI] |
| SGA–A | 584 (39%) | 1.00 | 1.00 | 1.00 |
| SGA–B/C | 915 (61%) | 0.74 [0.69,0.79] *** | 0.94 [0.85,1.05] | 0.98 [0.87,1.1] |
| Phase angle ≤ 3° | 327 (22%) | 0.47 [0.39,0.56] *** | 0.59 [0.48,0.72] *** | |
| Phase angle 3–4° | 482 (32%) | 0.66 [0.56,0.78] *** | 0.8 [0.67,0.95] # | |
| Phase angle 4–5° | 424 (28%) | 0.79 [0.69,0.9] ** | 0.83 [0.72,0.95] * | |
| Phase angle > 5° | 272 (18%) | 1.00 | 1.00 | |
| Age <65 | 375 (25%) | 0.85 [0.7,1.04] | 0.75 [0.63,0.89] * | 0.75 [0.63,0.89] * |
| Age 65–75 | 361 (24%) | 1.00 | 1.00 | 1.00 |
| Age 75–80 | 337 (22%) | 0.92 [0.78,1.09] | 0.9 [0.76,1.06] | 0.9 [0.78,1.04] |
| Age > 80 | 432 (29%) | 0.95 [0.84,1.07] | 1 [0.88,1.14] | 0.95 [0.83,1.08] |
| BMI < 18.5 | 162 (11%) | 0.99 [0.87,1.12] | 1.02 [0.91,1.14] | 0.97 [0.84,1.11] |
| BMI 18.5–25 | 715 (48%) | 1.00 | 1.00 | 1.00 |
| BMI 25–30 | 379 (25%) | 1.01 [0.87,1.17] | 1.02 [0.88,1.19] | 1.07 [0.92,1.25] |
| BMI > 30 | 241 (16%) | 0.83 [0.72,0.94] * | 0.85 [0.73,0.99] | 0.89 [0.79,1.01] |
| CRP ≤ 10 | 480 (32%) | 1.00 | ||
| CRP 10–100 | 673 (45%) | 0.75 [0.63,0.88] ** | ||
| CRP > 100 | 158 (10%) | 0.54 [0.44,0.65] *** | ||
| CRP—no value | 194 (13%) | 1.65 [1.27,2.16] ** | ||
| Sex—male | 723 (48%) | 1.00 | 1.00 | 1.00 |
| Sex—female | 782 (52%) | 1.05 [0.98,1.13] | 1.09 [1.02,1.17] | 0.99 [0.91,1.09] |
| ICD A–B: infections | 79 (5%) | 0.82 [0.67,0.99] | 0.85 [0.71,1.02] | 0.86 [0.69,1.07] |
| ICD C–D50: neoplasms | 356 (24%) | 0.62 [0.48,0.81] ** | 0.62 [0.47,0.82] ** | 0.61 [0.47,0.79] ** |
| ICD D50–89: blood and blood-forming organs | 72 (5%) | 1.08 [0.75,1.56] | 1.12 [0.77,1.62] | 0.98 [0.66,1.45] |
| ICD E: endocrine | 35 (2%) | 1.38 [0.81,2.38] | 1.31 [0.7,2.47] | 1.2 [0.66,2.2] |
| ICD G: nervous system | 39 (3%) | 1.08 [0.77,1.51] | 1.05 [0.75,1.47] | 0.81 [0.54,1.21] |
| ICD I: circulatory | 176 (12%) | 0.58 [0.47,0.71] *** | 0.57 [0.46,0.71] *** | 0.52 [0.4,0.67] *** |
| ICD J: respiratory | 110 (7%) | 0.64 [0.49,0.83] ** | 0.62 [0.48,0.81] ** | 0.61 [0.49,0.77] *** |
| ICD 1 K: digestive | 286 (19%) | 1.00 | 1.00 | 1.00 |
| ICD M: musculoskeletal | 60 (4%) | 0.61 [0.44,0.86] * | 0.61 [0.43,0.86] * | 0.56 [0.4,0.8] * |
| ICD N: genitourinary | 62 (4%) | 0.92 [0.61,1.39] | 0.96 [0.63,1.45] | 1.02 [0.76,1.35] |
| ICD: other | 37 (2%) | 0.69 [0.43,1.11] | 0.61 [0.37,1] | 0.52 [0.3,0.9] |
| ICD R: abnormal findings | 65 (4%) | 1.07 [0.65,1.78] | 1.06 [0.63,1.81] | 0.92 [0.54,1.57] |
| ICD S-T: injury, poison | 103 (7%) | 0.53 [0.43,0.64] *** | 0.54 [0.45,0.64] *** | 0.55 [0.47,0.64] *** |
| Model I without PhA | Model II with Numerical PhA | ||
|---|---|---|---|
| Variable | OR [95%CI] | OR [95%CI] | |
| SGA | A | 1.00 | 1.00 |
| B/C | 2.87 [1.38,5.94] * | 1.16 [0.49,2.75] | |
| PhA [°] | numerical | 0.44 [0.32,0.61] *** | |
| Age [years] | <65 | 2.12 [0.89,5.07] | 3.68 [1.52,8.92] * |
| 65–75 y | 1.00 | 1.00 | |
| 75–80 y | 2.71 [1.08,6.8] # | 2.79 [1.08,7.24] # | |
| >80 y | 2.82 [1.03,7.73] # | 2.27 [0.82,6.3] | |
| BMI [kg/m2] | <18.5 | 0.84 [0.38,1.87] | 0.64 [0.29,1.42] |
| 18.5–25 | 1.00 | 1.00 | |
| 25–30 | 0.92 [0.38,2.22] | 0.8 [0.33,1.95] | |
| >30 | 1.01 [0.42,2.47] | 0.82 [0.34,1.96] | |
| Sex | M | 1.00 | 1.00 |
| W | 0.3 [0.16,0.58] ** | 0.26 [0.13,0.52] ** | |
| ICD-10 | C-D50: neoplasms | 2.28 [0.9,5.77] | 2.49 [0.97,6.42] |
| I: circulatory | 1.03 [0.32,3.35] | 1.14 [0.35,3.74] | |
| J: respiratory | 1.41 [0.49,4.06] | 1.64 [0.52,5.14] | |
| K: digestive | 1.00 | 1.00 | |
| other | 0.37 [0.12,1.12] | 0.37 [0.12,1.17] | |
| S-T: injury, poison | 0.67 [0.15,3.03] | 0.7 [0.16,3.04] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plauth, M.; Sulz, I.; Viertel, M.; Höfer, V.; Witt, M.; Raddatz, F.; Reich, M.; Hiesmayr, M.; Bauer, P. Phase Angle Is a Stronger Predictor of Hospital Outcome than Subjective Global Assessment—Results from the Prospective Dessau Hospital Malnutrition Study. Nutrients 2022, 14, 1780. https://doi.org/10.3390/nu14091780
Plauth M, Sulz I, Viertel M, Höfer V, Witt M, Raddatz F, Reich M, Hiesmayr M, Bauer P. Phase Angle Is a Stronger Predictor of Hospital Outcome than Subjective Global Assessment—Results from the Prospective Dessau Hospital Malnutrition Study. Nutrients. 2022; 14(9):1780. https://doi.org/10.3390/nu14091780
Chicago/Turabian StylePlauth, Mathias, Isabella Sulz, Melanie Viertel, Veronika Höfer, Mila Witt, Frank Raddatz, Michael Reich, Michael Hiesmayr, and Peter Bauer. 2022. "Phase Angle Is a Stronger Predictor of Hospital Outcome than Subjective Global Assessment—Results from the Prospective Dessau Hospital Malnutrition Study" Nutrients 14, no. 9: 1780. https://doi.org/10.3390/nu14091780
APA StylePlauth, M., Sulz, I., Viertel, M., Höfer, V., Witt, M., Raddatz, F., Reich, M., Hiesmayr, M., & Bauer, P. (2022). Phase Angle Is a Stronger Predictor of Hospital Outcome than Subjective Global Assessment—Results from the Prospective Dessau Hospital Malnutrition Study. Nutrients, 14(9), 1780. https://doi.org/10.3390/nu14091780