What Is a 2021 Reference Body?
Abstract
1. Introduction
1.1. A Historical View
1.2. Do We Need a 2021 Reference Body?
1.3. Purpose of This Study
2. Methods
2.1. Study Populations
2.2. Body Composition Analyses
2.3. Assessment of Resting Energy Expenditure (REE) and Analyses of Plasma Leptin Levels
2.4. Calculations
3. Results
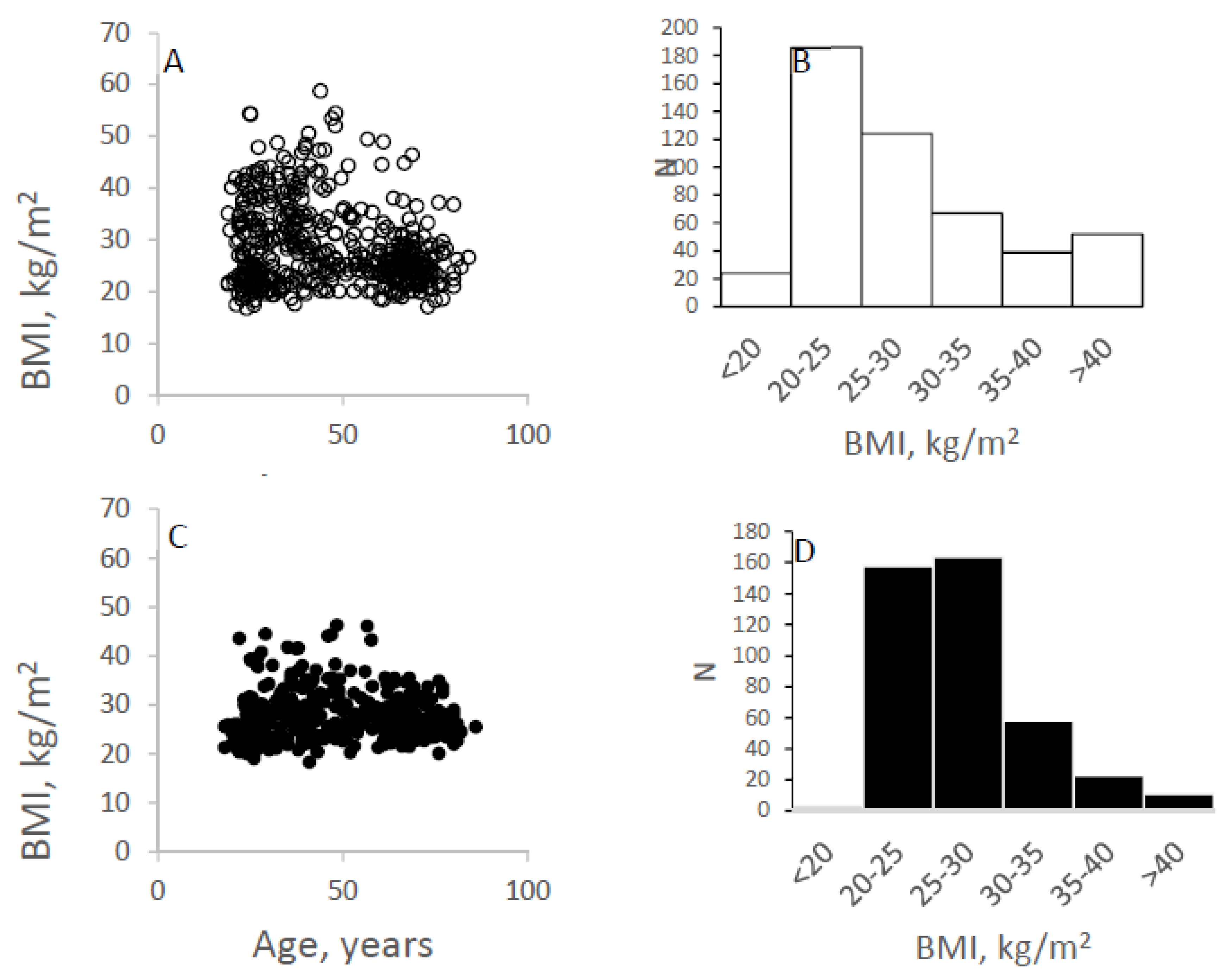
3.1. BMI vs. Age and BMI Distribution
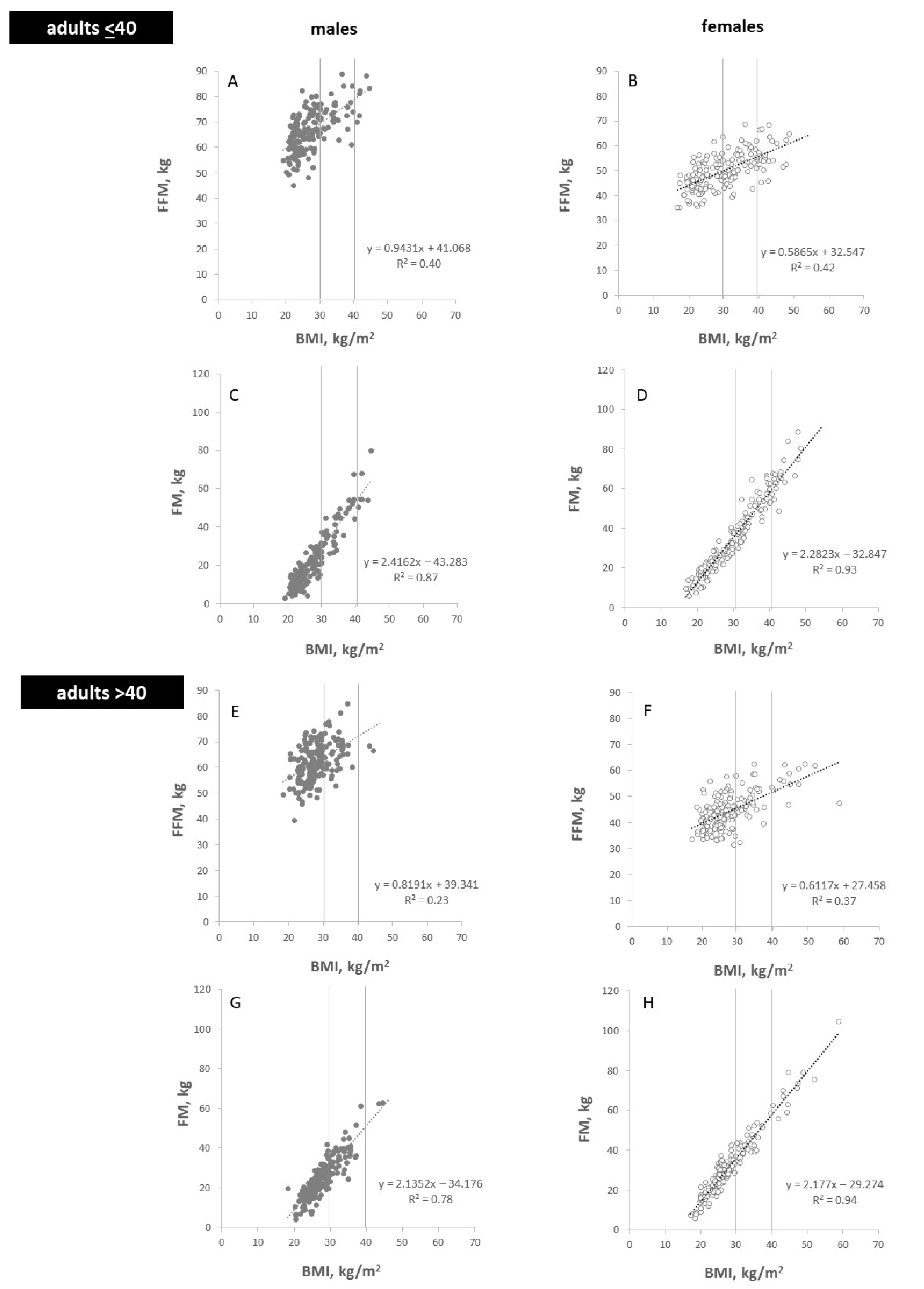
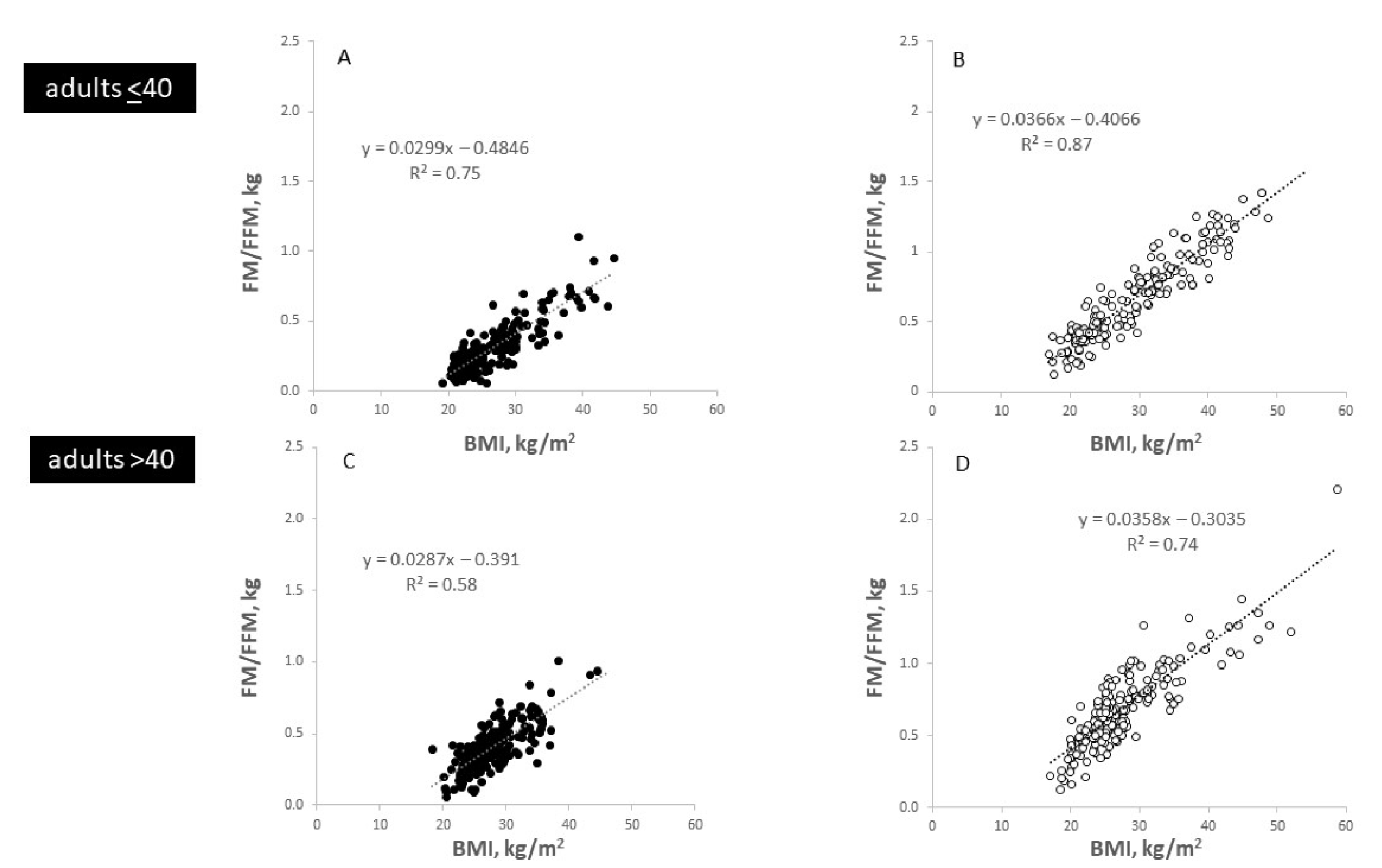
3.2. BMI vs. FM and FFM
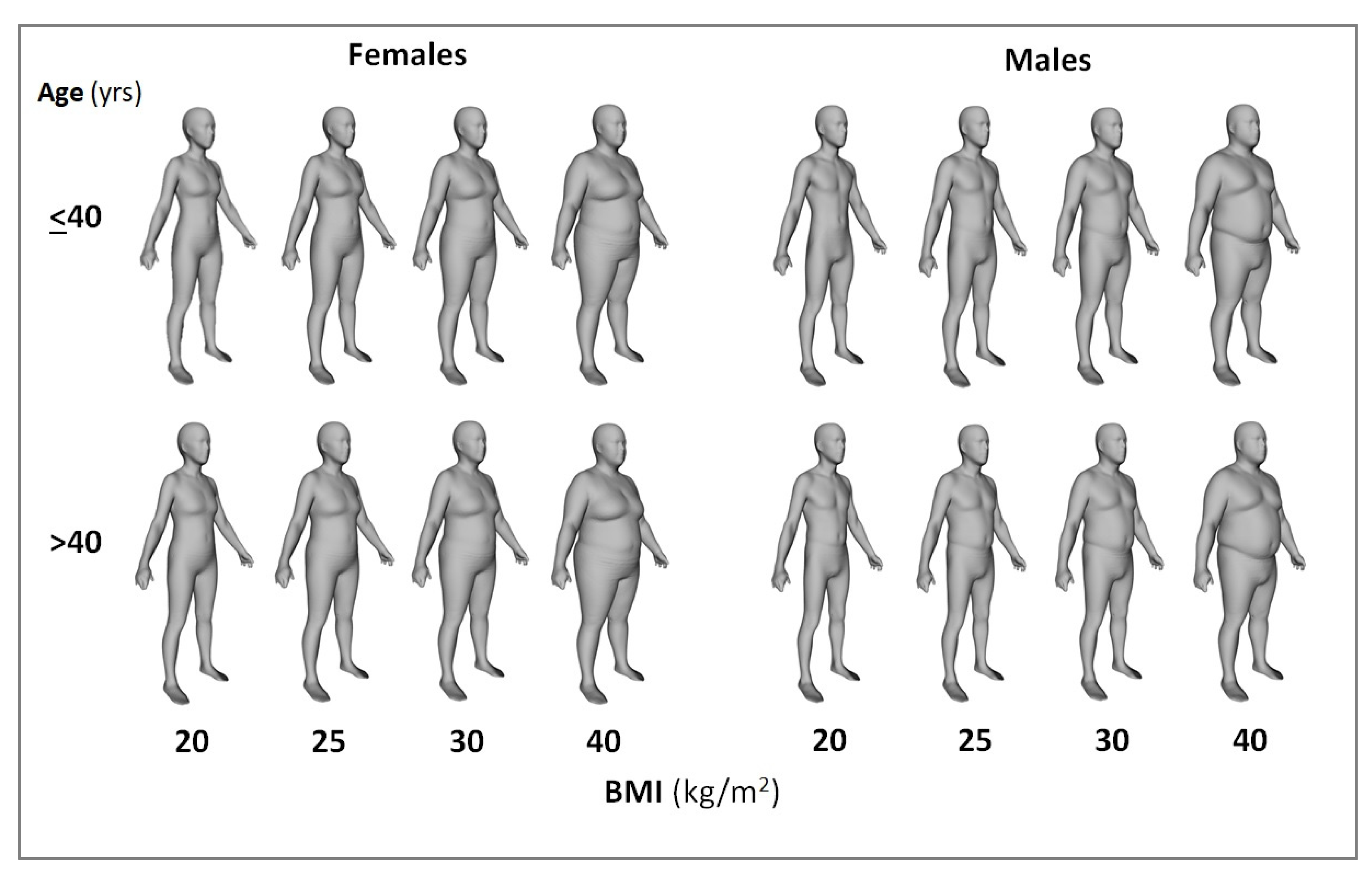
3.3. The 2021 Reference Body at BMI 20, 25, 30, 40 kg/m2 and Age <40 yrs and >40 yrs
3.4. Associations between Whole Body and Regional Body Composition
3.5. Body Shape and Body Circumferences
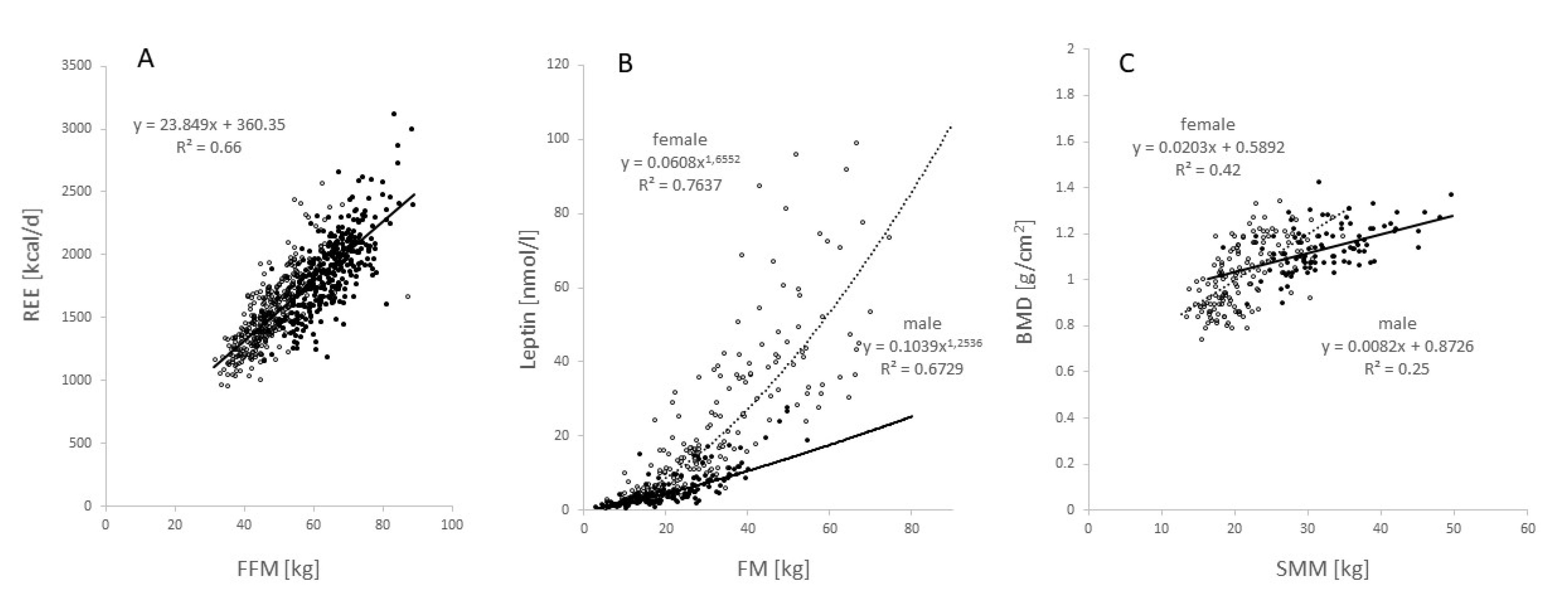
3.6. Functional Body Composition (FBC)
4. Discussion
4.1. Is the 2021 Reference Body a Step Forward?
4.2. Should the 2021 Reference Body Replace the 1975 Reference Man?
4.3. Suitable Applications of the 2021 Reference Body
4.4. Future Directions of the 2021 Reference Body
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Snyder, W.S.; Cook, M.J.; Karhausen, L.R.; Tipton, I.H. Report of the Task Group on Reference Man; ICPR Publication No. 23; Pergamon Press: Oxford, UK, 1975. [Google Scholar]
- ICPR. Annual Report of the International Commission on Radiological Protection 2002; ICPR Publication No. 89; Pergamon Press, Elsevier Sc. Ltd.: Oxford, UK, 2003. [Google Scholar]
- Makhijani, A. The Use of Reference Man in Radiation Protection Standards and Guidance with Recommendations for Change. Institute for Energy and Environmental Research (ieer), Maryland. 2009. Available online: https://ieer.org/wp/wp-content/uploads/2009/04/referenceman.pdf (accessed on 2 April 2022).
- Later, W.; Bosy-Westphal, A.; Kossel, E.; Gluer, C.-C.; Heller, M.; Muller, M.J. Is the 1975 Reference Man still a suitable reference? Eur. J. Clin. Nutr. 2010, 64, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- VanItallie, T.B.; Yang, M.U.; Heymsfield, S.B.; Funk, R.C.; Boileau, R.A. Height-normalized indices of the body’s fat-free mass and fat mass: Potentially useful indicators of nutritional status. Am. J. Clin. Nutr. 1990, 52, 953–959. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Langemann, D.; Gehrke, I.; Later, W.; Heller, M.; Glüer, C.C.; Heymsfield, S.B.; Bosy-Westphal, A. Effect of Constitution on Mass of Individual Organs and Their Association with Metabolic Rate in Humans—A Detailed View on Allometric Scaling. PLoS ONE 2011, 6, e22732. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Geisler, C.; Hübers, M.; Pourhassan, M.; Braun, W.; Bosy-Westphal, A. Normalizing resting energy expenditure across the life course in humans: Challenges and hopes. Eur. J. Clin. Nutr. 2018, 72, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Geisler, C.; Braun, W.; Pourhassan, M.; Schweitzer, L.; Glüer, C.-C.; Bosy-Westphal, A.; Müller, M.J. Gender-Specific Associations in Age-Related Changes in Resting Energy Expenditure (REE) and MRI Measured Body Composition in Healthy Caucasians. J. Gerontol. Ser. A 2016, 71, 941–946. [Google Scholar] [CrossRef]
- Tian, I.Y.; Ng, B.K.; Wong, M.C.; Kennedy, S.; Hwaung, P.; Kelly, N.; Liu, E.; Garber, A.K.; Curless, B.; Heymsfield, S.B.; et al. Predicting 3D body shape and body composition from conventional 2D photography. Med. Phys. 2020, 47, 6232–6245. [Google Scholar] [CrossRef]
- Morse, S.; Talty, K.; Kuiper, P.; Scioletti, M.; Heymsfield, S.B.; Atkinson, R.L.; Thomas, D.M. Machine learning prediction of combat basic training injury from 3D body shape images. PLoS ONE 2020, 15, e0235017. [Google Scholar] [CrossRef]
- Ng, B.K.; Sommer, M.J.; Wong, M.C.; Pagano, I.; Nie, Y.; Fan, B.; Kennedy, S.; Bourgeois, B.; Kelly, N.; Liu, Y.E.; et al. Detailed 3-dimensional body shape features predict body composition, blood metabolites, and functional strength: The Shape Up! studies. Am. J. Clin. Nutr. 2019, 110, 1316–1326. [Google Scholar] [CrossRef]
- Müller, M.J.; Braun, W.; Pourhassan, M.; Geisler, C.; Bosy-Westphal, A. Application of standards and models in body composition analysis. Proc. Nutr. Soc. 2015, 75, 181–187. [Google Scholar] [CrossRef]
- Müller, M.J.; Enderle, J.; Pourhassan, M.; Braun, W.; Eggeling, B.; Lagerpusch, M.; Glüer, C.-C.; Kehayias, J.J.; Kiosz, D.; Bosy-Westphal, A. Metabolic adaptation to caloric restriction and subsequent refeeding: The Minnesota Starvation Experiment revisited. Am. J. Clin. Nutr. 2015, 102, 807–819. [Google Scholar] [CrossRef]
- Müller, M.J.; Bosy-Westphal, A.; Kutzner, D.; Heller, M. Metabolically active components of fat-free mass and resting energy expenditure in humans: Recent lessons from imaging technologies. Obes. Rev. 2002, 3, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Marín, D.; Luque, V.; Ferré, N.; Fewtrell, M.S.; Williams, J.E.; Wells, J.C.K. Associations of age and body mass index with hydration and density of fat-free mass from 4 to 22 years. Eur. J. Clin. Nutr. 2019, 73, 1422–1430. [Google Scholar] [CrossRef] [PubMed]
- Allen, B.; Curless, B.; Popovic, Z. The space of human body shapes: Reconstruction and parameterization from range scans. ACM Trans. Graph. 2003, 22, 587–594. [Google Scholar] [CrossRef]
- Wong, M.C.; McCarthy, C.; Fernbach, N.; Yang, S.; Shephard, J.; Heymsfield, S.B. Emergence of the obesity epidemic: Six decade visualization with humanoid avatars. Am. J. Clin. Nutr. 2022, 115, 1189–1193. [Google Scholar] [CrossRef] [PubMed]
- Sobhiyeh, S.; Dunkel, A.; Dechenaud, M.; Mehrnezhad, A.; Kennedy, S.; Shepherd, J.; Wolenski, P.; Heymsfield, S.B. Digital anthropometric volumes: Toward the development and validation of a universal software. Med. Phys. 2021, 48, 3654–3664. [Google Scholar] [CrossRef]
- Müller, M.J.; Baracos, V.; Bosy-Westphal, A.; Dulloo, A.; Eckel, J.; Fearon, K.C.H.; Hall, K.D.; Pietrobelli, A.; Sørensen, T.I.A.; Speakman, J.; et al. Functional body composition and related aspects in research on obesity and cachexia: Report on the 12th Stock Conference held on 6 and 7 September 2013 in Hamburg, Germany. Obes. Rev. 2014, 15, 640–656. [Google Scholar] [CrossRef]
- Müller, M.J.; Braun, W.; Enderle, J.; Bosy-Westphal, A. Beyond BMI: Conceptual Issues Related to Overweight and Obese Patients. Obes. Facts 2016, 9, 193–205. [Google Scholar] [CrossRef]
- Müller, M.J.; Heymsfield, S.B.; Bosy-Westphal, A. Are metabolic adaptations to weight changes an artefact? Am. J. Clin. Nutr. 2021, 114, 1386–1395. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Lohman, T.G.; Wang, Z.; Going, S.B. (Eds.) Human Body Composition, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2005. [Google Scholar]
- Hall, K.D. Predicting metabolic adaptation, body weight change, and energy intake in humans. Am. J. Physiol. Endocrinol. Metab. 2010, 298, E449–E466. [Google Scholar] [CrossRef]
- Thomas, D.M.; Schoeller, D.A.; Redman, L.A.; Martin, C.K.; Levine, J.A.; Heymsfield, S.B. A computational model to determine energy intake during weight loss. Am. J. Clin. Nutr. 2010, 92, 1326–1331. [Google Scholar] [CrossRef]
- Hall, K.D.; Sacks, G.; Chandramohan, D.; Chow, C.C.; Wang, Y.C.; Gortmaker, S.L.; Swinburn, B.A. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011, 378, 826–837. [Google Scholar] [CrossRef]
- Hall, K.D. Modeling Metabolic Adaptations and Energy Regulation in Humans. Annu. Rev. Nutr. 2012, 32, 35–54. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.A.; Hall, K.D.; Thomas, D.M.; Hardin, J.W.; Allison, D.; Heymsfield, S.B. Novel Mathematical Models for Investigating Topics in Obesity. Adv. Nutr. Int. Rev. J. 2014, 5, 561–562. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heymsfield, S.B.; Peterson, C.M.; Bourgeois, B.; Thomas, D.M.; Gallagher, D.; Strauss, B.; Müller, M.J.; Bosy-Westphal, A. Human energy expenditure: Advances in organ-tissue prediction models. Obes. Rev. 2018, 19, 1177–1188. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.M.; Scioletti, M.; Heymsfield, S.B. Predictive Mathematical Models of Weight Loss. Curr. Diabetes Rep. 2019, 19, 93. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.J.; Bosy-Westphal, A. Effect of Over- and Underfeeding on Body Composition and Related Metabolic Functions in Humans. Curr. Diabetes Rep. 2019, 19, 108. [Google Scholar] [CrossRef]
- Müller, M.J.; Geisler, C.; Hübers, M.; Pourhassan, M.; Bosy-Westphal, A. Body composition-related functions: A problem-oriented approach to phenotyping. Eur. J. Clin. Nutr. 2018, 73, 179–186. [Google Scholar] [CrossRef]
- Rowland, M.; Peck, C.; Tucker, G. Physiologically-Based Pharmacokinetics in Drug Development and Regulatory Science. Annu. Rev. Pharmacol. Toxicol. 2011, 51, 45–73. [Google Scholar] [CrossRef]
- Peters, S.A. Physiologically-Based Pharmacokinetic (PBPK) Modeling and Simulations: Principles, Methods, and Applications in the Pharmaceutical Industry. Physiol Pharmacokinetic Model Simulations Princ Methods. Appl. Pharm. Ind. 2012. [Google Scholar]
- Quaye, E.; Chacko, S.; Chung, S.T.; Brychta, R.J.; Chen, K.Y.; Brown, R.J. Energy expenditure due to gluconeogenesis in pathological conditions of insulin resistance. Am. J. Physiol. Metab. 2021, 321, E795–E801. [Google Scholar] [CrossRef]
- Müller, M.J.; Paschen, U.; Müller, M.J. Starvation-induced ketone body production in the conscious un-restrained miniature pig. J. Nutr. 1982, 112, 1379–1386. [Google Scholar] [CrossRef] [PubMed]
- Lange, M.; Angelidou, G.; Ni, Z.; Criscuolo, A.; Schiller, J.; Blüher, M.; Fedorova, M. AdipoAtlas: A reference lipidome for human white adipose tissue. Cell Rep. Med. 2021, 2, 100407. [Google Scholar] [CrossRef] [PubMed]
- Metabolomicsworkbench.org. Available online: https://www.metabolomicsworkbench.org/data/show_metabolite_table.php?STUDY_ID=ST001738&ANALYSIS_ID=AN002831&TITLE=AdipoAtlas%3A+A+Reference+Lipidome+for+Human+White+Adipose+Tissue&COMMENTS=HILIC+POSITIVE+ION+MODE (accessed on 2 April 2022).
- Uhlén, M.; Fagerberg, L.; Hallström, B.M.; Lindskog, C.; Oksvold, P.; Mardinoglu, A.; Sivertsson, A.; Kampf, C.; Sjöstedt, E.; Asplund, A.; et al. Tissue-based map of the human proteome. Science 2015, 347, 1260419. [Google Scholar] [CrossRef] [PubMed]



| BMI, kg/m2 | Age | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 20 | 25 | 30 | 40 | 20 | 25 | 30 | 40 | ||
| FM, kg; % | >40 yrs | 8.47 | 19.44 | 30.40 | 52.33 | 14.69 | 25.47 | 36.24 | 57.79 |
| 15.48 | 24.49 | 31.85 | 43.47 | 29.21 | 37.30 | 43.90 | 54.33 | ||
| ≤40 yrs | 4.95 | 17.04 | 29.13 | 53.31 | 24.32 | 12.90 | 35.74 | 58.58 | |
| 10.38 | 20.36 | 28.51 | 41.37 | 24.80 | 33.30 | 40.25 | 51.21 | ||
| SAT, L | >40 yrs | 10.22 | 15.78 | 21.35 | 32.48 | 16.90 | 22.35 | 27.81 | 38.72 |
| ≤40 yrs | 7.26 | 14.76 | 22.27 | 37.28 | 14.94 | 22.80 | 30.66 | 46.38 | |
| VAT, L | >40 yrs | 1.68 | 3.27 | 4.86 | 8.04 | 1.08 | 1.96 | 2.85 | 4.62 |
| ≤40 yrs | 0.74 | 2.22 | 3.71 | 6.68 | 0.89 | 1.43 | 1.20 | 3.10 | |
| FFM, kg | >40 yrs | 55.38 | 59.63 | 63.87 | 72.36 | 38.62 | 41.76 | 44.91 | 51.20 |
| ≤40 yrs | 60.05 | 64.74 | 69.43 | 78.81 | 43.98 | 47.16 | 50.34 | 56.70 | |
| SM, kg | >40 yrs | 24.19 | 27.74 | 31.28 | 38.37 | 16.85 | 18.78 | 20.72 | 24.59 |
| ≤40 yrs | 28.10 | 31.51 | 34.91 | 41.72 | 19.64 | 21.30 | 22.96 | 26.28 | |
| Bone, kg | >40 yrs | 4.67 | 4.77 | 4.87 | 5.07 | 3.43 | 3.65 | 3.86 | 4.33 |
| ≤40 yrs | 5.21 | 5.32 | 5.43 | 5.65 | 4.20 | 4.33 | 4.46 | 4.72 | |
| Brain, kg | >40 yrs | 1.527 | 1.547 | 1.567 | 1.607 | 1.319 | 1.339 | 1.359 | 1.399 |
| ≤40 yrs | 1.385 | 1.395 | 1.405 | 1.425 | |||||
| Heart, kg | >40 yrs | 0.344 | 0.359 | 0.374 | 0.404 | 0.291 | 0.281 | 0.271 | 0.251 |
| ≤40 yrs | 0.261 | 0.271 | 0.281 | 0.301 | |||||
| Liver, kg | >40 yrs | 1.225 | 1.545 | 1.865 | 2.505 | 1.022 | 1.272 | 1.522 | 2.022 |
| ≤40 yrs | 1.439 | 1.714 | 1.989 | 2.539 | 1.286 | 1.451 | 1.616 | 1.946 | |
| Kidneys, kg | >40 yrs | 0.246 | 0.276 | 0.306 | 0.366 | 0.195 | 0.220 | 0.245 | 0.295 |
| ≤40 yrs | 0.234 | 0.274 | 0.314 | 0.394 | 0.218 | 0.243 | 0.268 | 0.318 | |
| TBW, L | >40 yrs | 40.29 | 44.86 | 49.43 | 58.57 | 29.80 | 33.20 | 36.60 | 43.41 |
| ≤40 yrs | 40.95 | 46.96 | 52.98 | 65.01 | 31.10 | 35.29 | 39.50 | 47.92 | |
| TBW/FFM, L/kg | >40 yrs | 0.72 | 0.74 | 0.76 | 0.80 | 0.74 | 0.76 | 0.78 | 0.82 |
| ≤40 yrs | 0.70 | 0.73 | 0.75 | 0.80 | 0.70 | 0.73 | 0.76 | 0.82 | |
| ECW, L | >40 yrs | 16.38 | 18.01 | 19.66 | 22.94 | 13.10 | 14.17 | 15.24 | 17.38 |
| ≤40 yrs | 16.77 | 17.97 | 19.17 | 21.57 | 13.10 | 14.37 | 15.68 | 18.30 | |
| Protein, kg | >40 yrs | 13.12 | 14.41 | 15.70 | 18.26 | 9.11 | 9.66 | 10.21 | 11.31 |
| ≤40 yrs | 13.23 | 14.83 | 16.42 | 19.61 | 9.81 | 10.78 | 11.75 | 13.69 | |
| FM, kg | SAT, L | VAT, kg | FFM, kg | SM, kg | Bone, kg | Brain, kg | Heart, kg | Liver, kg | Kidney, kg | TBW, L | ECW, L | Protein, kg | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FM, kg | 0.978 *** | 0.541 *** | 0.581 *** | 0.637 *** | 0.267 *** | 0.153 ** | 0.136 * | 0.665 *** | 0.506 *** | 0.730 *** | 0.640 *** | 0.357 ** | |
| SAT, L | 0.936 *** | 0.529 *** | 0.636 *** | 0.652 *** | 0.392 *** | 0.232 *** | 0.343 *** | 0.497 *** | 0.575 *** | 0.756 *** | 0.616 *** | 0.468 *** | |
| VAT, kg | 0.682 *** | 0.591 *** | 0.340 *** | 0.448 *** | 0.217 *** | 0.001 (NS) | 0.310 *** | 0.317 *** | 0.301 *** | 0.252 *** | 0.204 *** | 0.040 (NS) | |
| FFM, kg | 0.300 *** | 0.447 *** | 0.228 *** | 0.869 *** | 0.785 *** | 0.384 *** | 0.233 *** | 0.700 *** | 0.522 *** | 0.885 *** | 0.777 *** | 0.882 *** | |
| SM, kg | 0.442 *** | 0.506 *** | 0.313 *** | 0.874 *** | 0.684 *** | 0.292 *** | 0.311 *** | 0.796 *** | 0.611 *** | 0.882 *** | 0.782 *** | 0.779 *** | |
| Bone, kg | −0.041 (NS) | 0.066 (NS) | 0.057 (NS) | 0.764 *** | 0.534 *** | 0.273 *** | 0.233 *** | 0.452 *** | 0.120 * | 0.554 *** | 0.479 *** | 0.573 *** | |
| Brain, kg | 0.104 (NS) | 0.283 *** | 0.246 *** | 0.300 *** | 0.247 *** | 0.187 ** | -0.033 (NS) | 0.312 *** | 0.347 *** | 0.361 *** | 0.229 *** | 0.304 * | |
| Heart, kg | 0.133 * | 0.229 *** | 0.255 *** | 0.179 ** | 0.024 (NS) | 0.302 *** | 0.034 (NS) | -0.066 (NS) | 0.209 *** | 0.445 *** | 0.352 *** | 0.261 * | |
| Liver, kg | 0.554 *** | 0.556 ** | 0.410 *** | 0.678 *** | 0.685 *** | 0.349 *** | 0.308 *** | 0.071 (NS) | 0.381 *** | 0.760 *** | 0.719 *** | 0.604 *** | |
| Kidney, kg | 0.326 *** | 0.498 *** | 0.430 *** | 0.395 *** | 0.376 *** | 0.139 * | 0.420 *** | 0.152 * | 0.546 *** | 0.602 *** | 0.449 *** | 0.503 *** | |
| TBW, L | 0.496 *** | 0.571 *** | 0.258 *** | 0.857 *** | 0.898 *** | 0.555 *** | 0.278 *** | 0.079 (NS) | 0.691 *** | 0.374 *** | 0.806 *** | 0.775 *** | |
| ECW, L | 0.346 *** | 0.357 *** | 0.147 * | 0.685 *** | 0.702 *** | 0.506 *** | 0.026 (NS) | 0.282 *** | 0.584 *** | 0.281 *** | 0.758 *** | 0.786 *** | |
| Protein, kg | 0.232 * | 0.316* | 0.211 * | 0.774 *** | 0.676 *** | 0.545 *** | 0.228 * | 0.169 (NS) | 0.530 *** | 0.228 * | 0.658 *** | 0.601 *** |
| BMI, kg/m2 | Age | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 20 | 25 | 30 | 40 | 20 | 25 | 30 | 40 | ||
| Circumferences | |||||||||
| Rt Bicep, m | >40 yrs | 0.298 | 0.335 | 0.370 | 0.425 | 0.269 | 0.309 | 0.342 | 0.427 |
| ≤40 yrs | 0.287 | 0.319 | 0.355 | 0.425 | 0.267 | 0.302 | 0.337 | 0.446 | |
| Lt Bicep,m | >40 yrs | 0.309 | 0.345 | 0.378 | 0.439 | 0.277 | 0.316 | 0.351 | 0.421 |
| ≤40 yrs | 0.296 | 0.325 | 0.359 | 0.426 | 0.276 | 0.311 | 0.347 | 0.425 | |
| Chest, m | >40 yrs | 0.882 | 0.983 | 1.059 | 1.203 | 0.870 | 0.959 | 1.038 | 1.178 |
| ≤40 yrs | 0.921 | 1.005 | 1.083 | 1.246 | 0.885 | 0.970 | 1.053 | 1.163 | |
| Waist, m | >40 yrs | 0.742 | 0.885 | 1.008 | 1.213 | 0.756 | 0.864 | 0.968 | 1.217 |
| ≤40 yrs | 0.823 | 0.963 | 1.073 | 1.270 | 0.788 | 0.899 | 1.015 | 1.269 | |
| Hip, m | >40 yrs | 0.922 | 1.006 | 1.079 | 1.212 | 0.956 | 1.037 | 1.106 | 1.285 |
| ≤40 yrs | 0.919 | 0.997 | 1.078 | 1.224 | 0.935 | 1.019 | 1.119 | 1.279 | |
| Rt Thigh, m | >40 yrs | 0.508 | 0.579 | 0.631 | 0.698 | 0.500 | 0.569 | 0.622 | 0.724 |
| ≤40 yrs | 0.489 | 0.538 | 0.590 | 0.673 | 0.491 | 0.539 | 0.602 | 0.694 | |
| Lt Thigh, m | >40 yrs | 0.512 | 0.580 | 0.629 | 0.701 | 0.500 | 0.571 | 0.619 | 0.716 |
| ≤40 yrs | 0.491 | 0.537 | 0.588 | 0.674 | 0.492 | 0.539 | 0.601 | 0.689 | |
| Surface Areas | |||||||||
| Head, m2 | >40 yrs | 0.182 | 0.198 | 0.208 | 0.219 | 0.170 | 0.179 | 0.183 | 0.199 |
| ≤40 yrs | 0.182 | 0.190 | 0.202 | 0.223 | 0.170 | 0.176 | 0.184 | 0.198 | |
| Rt Arm, m2 | >40 yrs | 0.172 | 0.196 | 0.208 | 0.219 | 0.149 | 0.165 | 0.171 | 0.199 |
| ≤40 yrs | 0.177 | 0.188 | 0.202 | 0.224 | 0.145 | 0.153 | 0.167 | 0.204 | |
| Lt Arm, m2 | >40 yrs | 0.178 | 0.200 | 0.211 | 0.219 | 0.151 | 0.168 | 0.173 | 0.198 |
| ≤40 yrs | 0.179 | 0.190 | 0.201 | 0.223 | 0.148 | 0.155 | 0.169 | 0.198 | |
| Trunk, m2 | >40 yrs | 0.479 | 0.554 | 0.624 | 0.736 | 0.460 | 0.523 | 0.550 | 0.694 |
| ≤40rsy | 0.511 | 0.562 | 0.643 | 0.807 | 0.454 | 0.502 | 0.550 | 0.726 | |
| Legs, m2 | >40 yrs | 0.686 | 0.801 | 0.833 | 0.815 | 0.652 | 0.732 | 0.772 | 0.845 |
| ≤40 yrs | 0.701 | 0.762 | 0.785 | 0.812 | 0.637 | 0.675 | 0.748 | 0.791 | |
| Total, m2 | >40rsy | 1.680 | 1.928 | 2.062 | 2.182 | 1.566 | 1.748 | 1.829 | 2.109 |
| ≤40 yrs | 1.731 | 1.874 | 2.011 | 2.262 | 1.538 | 1.644 | 1.797 | 2.090 | |
| Males | Females | ||||
|---|---|---|---|---|---|
| Age | ≤40 yrs | >40 yrs | ≤40 yrs | >40 yrs | |
| BMI, kg/m2 | |||||
| 20 | 1828 kcal/d | 1622 kcal/d | 1458 kcal/d | 1236 kcal/d | |
| 25 | 1936 kcal/d | 1720 kcal/d | 1531 kcal/d | 1309 kcal/d | |
| 30 | 2044 kcal/d | 1818 kcal/d | 1605 kcal/d | 1381 kcal/d | |
| 40 | 2260 kcal/d | 2013 kcal/d | 1751 kcal/d | 1526 kcal/d | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller, M.J.; Bosy-Westphal, A.; Braun, W.; Wong, M.C.; Shepherd, J.A.; Heymsfield, S.B. What Is a 2021 Reference Body? Nutrients 2022, 14, 1526. https://doi.org/10.3390/nu14071526
Müller MJ, Bosy-Westphal A, Braun W, Wong MC, Shepherd JA, Heymsfield SB. What Is a 2021 Reference Body? Nutrients. 2022; 14(7):1526. https://doi.org/10.3390/nu14071526
Chicago/Turabian StyleMüller, Manfred J., Anja Bosy-Westphal, Wiebke Braun, Michael C. Wong, John A. Shepherd, and Steven B. Heymsfield. 2022. "What Is a 2021 Reference Body?" Nutrients 14, no. 7: 1526. https://doi.org/10.3390/nu14071526
APA StyleMüller, M. J., Bosy-Westphal, A., Braun, W., Wong, M. C., Shepherd, J. A., & Heymsfield, S. B. (2022). What Is a 2021 Reference Body? Nutrients, 14(7), 1526. https://doi.org/10.3390/nu14071526






