Estimates of the Nutritional Impact of Non-Participation in the National School Lunch Program during COVID-19 School Closures
Abstract
:1. Introduction
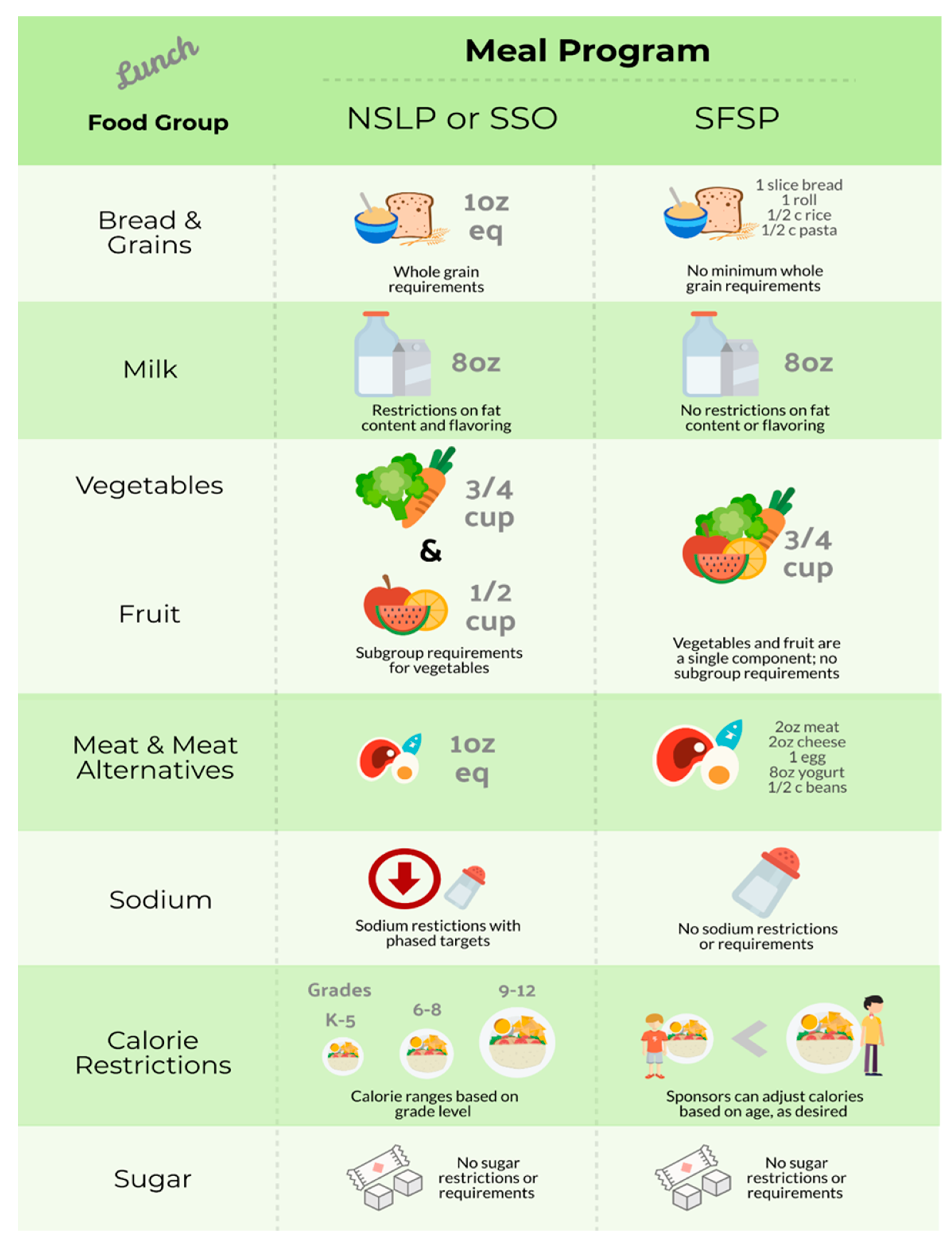
2. Materials and Methods
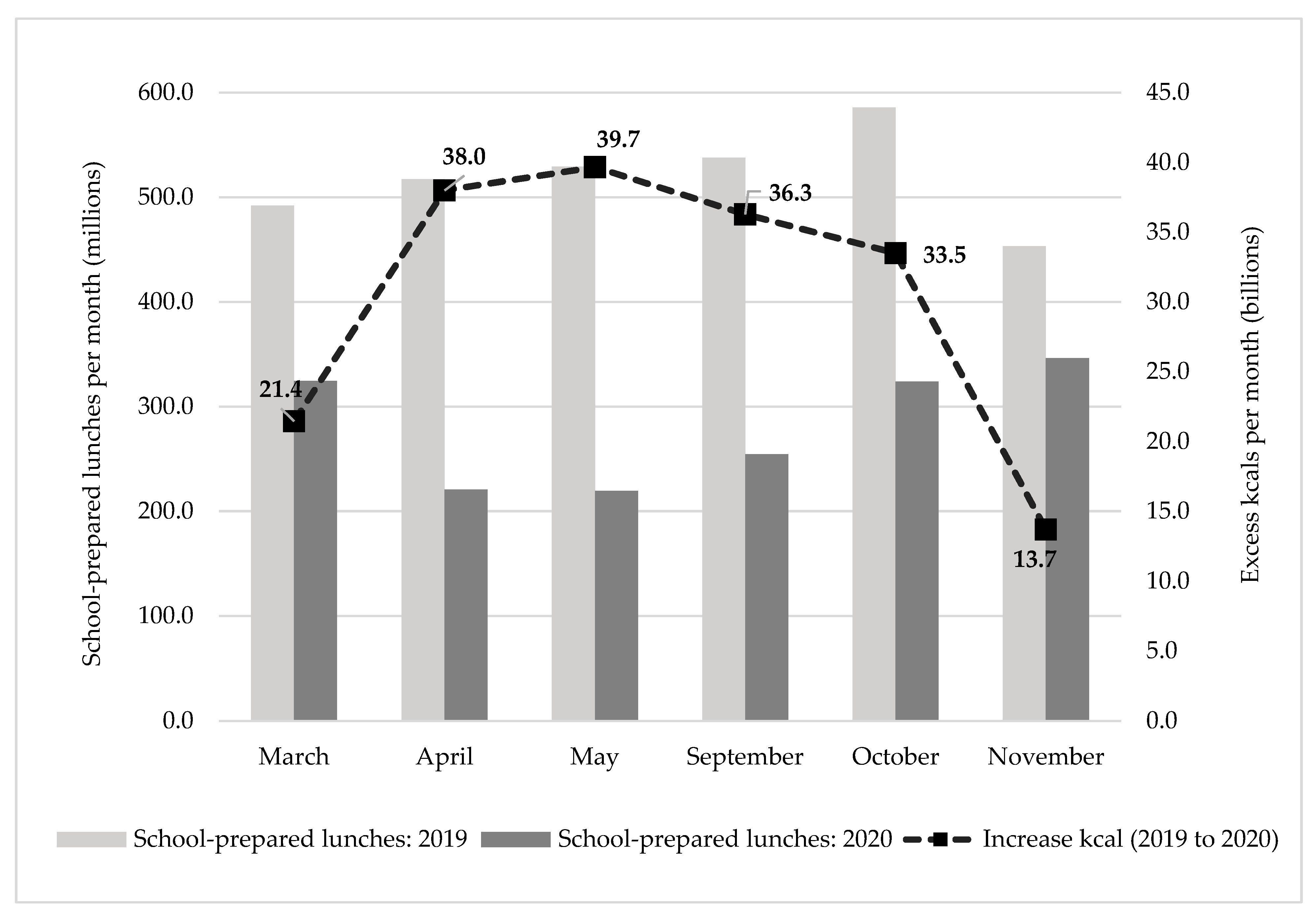
3. Results
4. Discussion
4.1. Limitations
4.2. Policy Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Elementary School | Middle School | High School | |||||||
|---|---|---|---|---|---|---|---|---|---|
| NSLP Participant | Nonparticipant | Daily Recommended | NSLP Participant | Nonparticipant | Daily Recommended | NSLP Participant | Nonparticipant | Daily Recommended | |
| kcal | 489 | 587 | 1200–1600 | 501 | 546 | 1600–1800 | 588 | 713 * | 1800–3200 |
| Nutrient | |||||||||
| Total fat (% kcal) a | 26.8 | 29.4 | 25–35 | 29.8 | 31.6 | 25–35 | 29.2 | 32.7 * | 25–35 |
| Saturated fat (% kcal) a | 8.6 | 9.4 | <10 | 8.9 | 9 | <10 | 9 | 10 | <10 |
| Carbohydrate (g) b | 69 | 82 | 130 | 66 | 75 | 130 | 78 | 93 * | 130 |
| Protein (g) b | 22 | 20 | 19 | 23 | 20 * | 34 | 27 | 27 | 46–52 |
| Vitamin D (mcg) b | 5.1 | 1.1 * | 15 | 4.3 | 2.1 * | 15 | 3 | 2.4 | 15 |
| Calcium (mg) b | 360 | 301 | 1000 | 322 | 268 * | 1300 | 394 | 358 | 1300 |
| Iron (mg) b | 3.1 | 3.8 | 10 | 3.1 | 3.4 | 8 | 3.7 | 4.4 * | 11–15 |
| Dietary fiber (g) c | 6 | 6 | 16.8–19.6 | 6 | 6 | 22.4–25.2 | 6 | 6 | 25.2–30.8 |
| Sodium (mg) d | 770 | 908 | 1900 | 794 | 902 | 2200 | 1015 | 1263 * | 2300 |
| Potassium (mg) e | 764 | 649 * | 3800 | 715 | 638 | 4500 | 837 | 846 | 4700 |
| NSLP Lunches Replaced Per Week by Emergency Meals | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Lunches Per Week Prepared at Home | 5 | 4 | 3 | 2 | 1 |
| Change in kcal | 18,944 | 15,155 | 11,366 | 7578 | 3789 |
| Change in nutrients | |||||
| Total fat (g) | 1036 | 829 | 622 | 414 | 207 |
| Saturated fat (g) | 296 | 237 | 178 | 118 | 59 |
| Carbohydrate (g) | 2368 | 1894 | 1421 | 947 | 474 |
| Protein (g) | 0 | 0 | 0 | 0 | 0 |
| Vitamin D (mcg) | −400 | −320 | −240 | −160 | −80 |
| Calcium (mg) | −5920 | −4736 | −3552 | −2368 | −1184 |
| Iron (mg) | 118 | 95 | 71 | 47 | 24 |
| Dietary fiber (g) | 0 | 0 | 0 | 0 | 0 |
| Sodium (mg) | 33,152 | 26,522 | 19,891 | 13,261 | 6630 |
| Potassium (mg) | −6216 | −4973 | −3730 | −2486 | −1243 |
References
- United States Department of Agriculture Economic Research Service National School Lunch Program. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/child-nutrition-programs/national-school-lunch-program.aspx (accessed on 19 August 2019).
- Ralston, K.; Treen, K.; Coleman-Jensen, A.; Guthrie, J. Children’s Food Security and USDA Child Nutrition Programs; United States Department of Agriculture Economic Research Service: Washington, DC, USA, 2017.
- Cullen, K.W.; Chen, T.-A. The contribution of the USDA school breakfast and lunch program meals to student daily dietary intake. Prev. Med. Rep. 2017, 5, 82–85. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Agriculture Food and Nutrition Service Child Nutrition Tables: National Level Annual Summary Tables: FY 1969–2019. Available online: https://www.fns.usda.gov/pd/child-nutrition-tables (accessed on 19 February 2020).
- Moore, Q.; Hulsey, L.; Ponza, M. Factors Associated with School Meal Participation and the Relationship Between Different Participation Measures; Final Report; Mathematica Policy Research: Princeton, NJ, USA, 2009; p. 173. [Google Scholar]
- Mansfield, J.L.; A Savaiano, D. Effect of school wellness policies and the Healthy, Hunger-Free Kids Act on food-consumption behaviors of students, 2006–2016: A systematic review. Nutr. Rev. 2017, 75, 533–552. [Google Scholar] [CrossRef] [PubMed]
- Fox, M.K. School Nutrition and Meal Cost Study Final Report Volume 4: Student Participation, Satisfaction, Plate Waste, and Dietary Intakes; Final Report; US Department of Agriculture: Washington, DC, USA; Food and Nutrition Service: Alexandria, VA, USA, 2019.
- Liu, J.; Micha, R.; Li, Y.; Mozaffarian, D. Trends in Food Sources and Diet Quality Among US Children and Adults, 2003–2018. JAMA Netw. Open 2021, 4, e215262. [Google Scholar] [CrossRef] [PubMed]
- Kinsey, E.W.; Hecht, A.A.; Dunn, C.G.; Levi, R.; Read, M.A.; Smith, C.; Niesen, P.; Seligman, H.K.; Hager, E.R. School Closures During COVID-19: Opportunities for Innovation in Meal Service. Am. J. Public Health 2020, 110, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Agriculture. November 2020 Keydata Report. Available online: https://www.fns.usda.gov/data/november-2020-keydata-report (accessed on 23 April 2021).
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.C.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Ferreira Peres, W.A.; Martorell, M.; Aires, M.T.; de Oliveira Cardoso, L.; et al. Covid-19 Confinement and Changes of Adolescent’s Dietary Trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Martín-Rodríguez, A.; Tornero-Aguilera, J.F.; López-Pérez, P.J.; Clemente-Suárez, V.J. Dietary patterns of adolescent students during the COVID-19 pandemic lockdown. Physiol. Behav. 2022, 249, 113764. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Mignogna, C.; Costanzo, S.; Ghulam, A.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Bonaccio, M. Impact of Nationwide Lockdowns Resulting from the First Wave of the COVID-19 Pandemic on Food Intake, Eating Behaviors, and Diet Quality: A Systematic Review. Adv. Nutr. Int. Rev. J. 2021, nmab130. [Google Scholar] [CrossRef]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown During the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 53. [Google Scholar] [CrossRef]
- Burkart, S.; Parker, H.; Weaver, R.G.; Beets, M.W.; Jones, A.; Adams, E.L.; Chaput, J.; Armstrong, B. Impact of the COVID-19 pandemic on elementary schoolers’ physical activity, sleep, screen time and diet: A quasi-experimental interrupted time series study. Pediatr. Obes. 2021, 17, e12846. [Google Scholar] [CrossRef]
- Wang, Y.C.; Gortmaker, S.L.; Sobol, A.M.; Kuntz, K.M. Estimating the Energy Gap Among US Children: A Counterfactual Approach. Pediatrics 2006, 118, e1721–e1733. [Google Scholar] [CrossRef] [PubMed]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.S.; Schmidt, L.; Beck, A.; Kepper, M.M.; Mazzucca, S.; Eyler, A. Associations of physical activity and sedentary behaviors with child mental well-being during the COVID-19 pandemic. BMC Public Health 2021, 21, 1770. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, A.P.; Kowalski, A.J.; Wang, Y.; Deitch, R.; Selam, H.; Rahmaty, Z.; Black, M.M.; Hager, E.R. On the Move or Barely Moving? Age-Related Changes in Physical Activity, Sedentary, and Sleep Behaviors by Weekday/Weekend Following Pandemic Control Policies. Int. J. Environ. Res. Public Health 2021, 19, 286. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Childhood Obesity Facts. Available online: https://www.cdc.gov/obesity/data/childhood.html (accessed on 20 November 2020).
- Centers for Disease Control and Prevention Causes and Consequences of Childhood Obesity. Available online: https://www.cdc.gov/obesity/childhood/causes.html (accessed on 20 November 2020).
- Guo, S.S.; Chumlea, W.C. Tracking of body mass index in children in relation to overweight in adulthood. Am. J. Clin. Nutr. 1999, 70, 145S–148S. [Google Scholar] [CrossRef] [Green Version]
- The, N.S.; Suchindran, C.; North, K.E.; Popkin, B.M.; Gordon-Larsen, P. Association of Adolescent Obesity With Risk of Severe Obesity in Adulthood. JAMA 2010, 304, 2042–2047. [Google Scholar] [CrossRef] [Green Version]
- Jenssen, B.P.; Kelly, M.K.; Powell, M.; Bouchelle, Z.; Mayne, S.L.; Fiks, A.G. COVID-19 and Changes in Child Obesity. Pediatrics 2021, 147, e2021050123. [Google Scholar] [CrossRef]
- US Department of Health and Human Services; US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans: Current Eating Patterns in the United States; US Department of Health and Human Services: Washington, DC, USA; US Department of Agriculture: Washington, DC, USA, 2015.
- Zhang, F.F.; Liu, J.; Rehm, C.D.; Wilde, P.; Mande, J.R.; Mozaffarian, D. Trends and Disparities in Diet Quality Among US Adults by Supplemental Nutrition Assistance Program Participation Status. JAMA Netw. Open 2018, 1, e180237. [Google Scholar] [CrossRef] [Green Version]
- Larson, N.I. Nutritional problems in childhood and adolescence: A narrative review of identified disparities. Nutr. Res. Rev. 2021, 34, 17–47. [Google Scholar] [CrossRef]
- McLoughlin, G.M.; McCarthy, J.A.; McGuirt, J.T.; Singleton, C.R.; Dunn, C.G.; Gadhoke, P. Addressing Food Insecurity through a Health Equity Lens: A Case Study of Large Urban School Districts during the COVID-19 Pandemic. J. Hered. 2020, 97, 759–775. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Pate, R.R.; Weaver, R.G. Children’s Obesogenic Behaviors During Summer Versus School: A Within-Person Comparison. J. Sch. Health 2018, 88, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, P.T.; Powell, B.; Downey, D.B.; Rowland, N.J. The Effect of School on Overweight in Childhood: Gain in Body Mass Index During the School Year and During Summer Vacation. Am. J. Public Health 2007, 97, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Franckle, R.; Adler, R.; Davison, K. Accelerated Weight Gain Among Children During Summer Versus School Year and Related Racial/Ethnic Disparities: A Systematic Review. Prev. Chronic Dis. 2014, 11, E101. [Google Scholar] [CrossRef] [Green Version]
- Moreno, J.P.; Johnston, C.A.; Woehler, D. Changes in Weight Over the School Year and Summer Vacation: Results of a 5-Year Longitudinal Study. J. Sch. Health 2013, 83, 473–477. [Google Scholar] [CrossRef]
- Nord, M.; Romig, K. Hunger in the Summer. J. Child. Poverty 2006, 12, 141–158. [Google Scholar] [CrossRef]
- Edwards, K.A. The Racial Disparity in Unemployment Benefits; RAND Corporation 2020. Available online: https://www.rand.org/blog/2020/07/the-racial-disparity-in-unemployment-benefits.html (accessed on 1 March 2022).
- Marte, J. Gap in U.S. Black and White Unemployment Rates Is Widest in Five Years. Reuters. 2020. Available online: https://www.reuters.com/article/us-usa-economy-unemployment-race/gap-in-u-s-black-and-white-unemployment-rates-is-widest-in-five-years-idUSKBN2431X7 (accessed on 1 March 2022).
- Center for Budget and Policy Priorities. Pandemic EBT Implementation Documentation Project; Center for Budget and Policy Priorities; Food Research & Action Center: Washington, DC, USA, 2020. [Google Scholar]
- Turner, L.; Calvert, H.G. The Academic, Behavioral, and Health Influence of Summer Child Nutrition Programs: A Narrative Review and Proposed Research and Policy Agenda. J. Acad. Nutr. Diet. 2019, 119, 972–983. [Google Scholar] [CrossRef]
- United States Department of Agriculture Child Nutrition COVID-19 Waivers. Available online: https://www.fns.usda.gov/programs/fns-disaster-assistance/fns-responds-covid-19/child-nutrition-covid-19-waivers (accessed on 20 November 2020).
- Hopkins, L.C.; Gunther, C. A Historical Review of Changes in Nutrition Standards of USDA Child Meal Programs Relative to Research Findings on the Nutritional Adequacy of Program Meals and the Diet and Nutritional Health of Participants: Implications for Future Research and the Summer Food Service Program. Nutrients 2015, 7, 10145–10167. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J.F.W.; Hecht, A.A.; McLoughlin, G.M.; Turner, L.; Schwartz, M.B. Universal School Meals and Associations with Student Participation, Attendance, Academic Performance, Diet Quality, Food Security, and Body Mass Index: A Systematic Review. Nutrients 2021, 13, 911. [Google Scholar] [CrossRef]
- Cohen, J.F.; Jahn, J.L.; Richardson, S.; Cluggish, S.A.; Parker, E.; Rimm, E.B. Amount of Time to Eat Lunch Is Associated with Children’s Selection and Consumption of School Meal Entrée, Fruits, Vegetables, and Milk. J. Acad. Nutr. Diet. 2016, 116, 123–128. [Google Scholar] [CrossRef] [Green Version]
- Chapman, L.E.; Cohen, J.; Canterberry, M.; Carton, T.W. Factors Associated with School Lunch Consumption: Reverse Recess and School “Brunch”. J. Acad. Nutr. Diet. 2017, 117, 1413–1418. [Google Scholar] [CrossRef]
- Saint Paul Public Schools COVID-19 Meal Access Plan. Available online: www.spps.org (accessed on 18 April 2020).
- United States Department of Agriculture Unpaid Meal Charges: Guidance and Q&As. Vol SP 23-20172017. Available online: https://www.fns.usda.gov/cn/unpaid-meal-charges-guidance-qas (accessed on 24 January 2021).
- Fleischhacker, S.; Campbell, E. Ensuring Equitable Access to School Meals. J. Acad. Nutr. Diet. 2020, 120, 893–897. [Google Scholar] [CrossRef]
- Soldavini, J.; Franckle, R.; Dunn, C.G.; Turner, L.; Fleischhacker, S. Strengthening the Impact of USDA’s Child Nutrition Summer Feeding Programs during and after the COVID-19 Pandemic; Healthy Eating Research: Durham, NC, USA, 2021. [Google Scholar]
- Kinsey, E.W.; Kinsey, D.; Rundle, A.G. COVID-19 and Food Insecurity: An Uneven Patchwork of Responses. J. Urban Health 2020, 97, 332–335. [Google Scholar] [CrossRef]
| NSLP Participants | NSLP Nonparticipants | Difference (Nonparticipants–Participants) | |
|---|---|---|---|
| kcal | 515 | 643 | +128 * |
| Nutrient | |||
| Total fat (g) | 17 | 24 | +7 * |
| Saturated fat (g) | 5 | 7 | +2 * |
| Carbohydrate (g) | 71 | 87 | +16 * |
| Protein (g) | 23 | 23 | 0.0 |
| Vitamin D (mcg) | 4.5 | 1.8 | −2.7 * |
| Calcium (mg) | 361 | 321 | −40 |
| Iron (mg) | 3.3 | 4.1 | +0.8 * |
| Dietary fiber (g) | 6 | 6 | 0.0 |
| Sodium (mg) | 833 | 1057 | +224 * |
| Potassium (mg) | 772 | 730 | −42 |
| NSLP Lunches Replaced Per Week by Emergency Meals | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Lunches Per Week Prepared at Home | 5 | 4 | 3 | 2 | 1 |
| Change in kcal | 640 | 512 | 384 | 256 | 128 |
| Change in nutrients | |||||
| Total fat (g) | 35 | 28 | 21 | 14 | 7 |
| Saturated fat (g) | 10 | 8 | 6 | 4 | 2 |
| Carbohydrate (g) | 80 | 64 | 48 | 32 | 16 |
| Protein (g) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Vitamin D (mcg) | −13.5 | −10.8 | −8.1 | −5.4 | −2.7 |
| Calcium (mg) | −200 | −160 | −120 | −80 | −40 |
| Iron (mg) | 4.0 | 3.2 | 2.4 | 1.6 | 0.8 |
| Dietary fiber (g) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Sodium (mg) | 1120 | 896 | 672 | 448 | 224 |
| Potassium (mg) | −210 | −168 | −126 | −84 | −42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hecht, A.A.; Dunn, C.G.; Kinsey, E.W.; Read, M.A.; Levi, R.; Richardson, A.S.; Hager, E.R.; Seligman, H.K. Estimates of the Nutritional Impact of Non-Participation in the National School Lunch Program during COVID-19 School Closures. Nutrients 2022, 14, 1387. https://doi.org/10.3390/nu14071387
Hecht AA, Dunn CG, Kinsey EW, Read MA, Levi R, Richardson AS, Hager ER, Seligman HK. Estimates of the Nutritional Impact of Non-Participation in the National School Lunch Program during COVID-19 School Closures. Nutrients. 2022; 14(7):1387. https://doi.org/10.3390/nu14071387
Chicago/Turabian StyleHecht, Amelie A., Caroline Glagola Dunn, Eliza W. Kinsey, Margaret A. Read, Ronli Levi, Andrea S. Richardson, Erin R. Hager, and Hilary K. Seligman. 2022. "Estimates of the Nutritional Impact of Non-Participation in the National School Lunch Program during COVID-19 School Closures" Nutrients 14, no. 7: 1387. https://doi.org/10.3390/nu14071387
APA StyleHecht, A. A., Dunn, C. G., Kinsey, E. W., Read, M. A., Levi, R., Richardson, A. S., Hager, E. R., & Seligman, H. K. (2022). Estimates of the Nutritional Impact of Non-Participation in the National School Lunch Program during COVID-19 School Closures. Nutrients, 14(7), 1387. https://doi.org/10.3390/nu14071387






