The Role of Multiply-Fortified Table Salt and Bouillon in Food Systems Transformation
Abstract
:1. Introduction
2. Current and Emerging Dietary Trends
3. The Role of Salt and Bouillon in Food Systems Transformation
4. Salt and Bouillon Fortification within the Global Effort to Reduce Dietary Sodium Intake
5. Areas of Further Research Needed
5.1. Sodium Substitutes
5.2. Micronutrient Innovation
5.3. Dietary Surveillance
6. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The World Health Report: 2000: Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Picchioni, F.; Goulao, L.F.; Roberfroid, D. The impact of COVID-19 on diet quality, food security and nutrition in low and middle income countries: A systematic review of the evidence. Clin. Nutr. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, K.; Bai, Y.; Headey, D.; Masters, W.A. Affordability of the EAT–Lancet reference diet: A global analysis. Lancet Glob. Health 2020, 8, e59–e66. [Google Scholar] [CrossRef] [Green Version]
- Welch, R.M. Micronutrients, Agriculture and Nutrition; Linkages for Improved Health and Well Being. In Perspectives on the Micronutrient Nutrition of Crops; Scientific Publishers: Jodhpur, India, 2001; pp. 247–289. [Google Scholar]
- Beal, T.; Massiot, E.; Arsenault, J.E.; Smith, M.R.; Hijmans, R.J. Global trends in dietary micronutrient supplies and estimated prevalence of inadequate intakes. PLoS ONE 2017, 12, e0175554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azam, M.M.; Padmavathi, S.; Abdul Fiyaz, R.; Waris, A.; Ramya, K.T.; Neeraja, C.N. Effect of different cooking methods on loss of iron and zinc micronutrients in fortified and non-fortified rice. Saudi J. Biol. Sci. 2021, 28, 2886–2894. [Google Scholar] [CrossRef]
- Garg, M.; Sharma, A.; Vats, S.; Tiwari, V.; Kumari, A.; Mishra, V.; Krishania, M. Vitamins in Cereals: A Critical Review of Content, Health Effects, Processing Losses, Bioaccessibility, Fortification, and Biofortification Strategies for Their Improvement. Front. Nutr. 2021, 8, 254. [Google Scholar] [CrossRef]
- Guerrant, R.L.; Lima, A.A.M.; Davidson, F. Micronutrients and Infection: Interactions and Implications with Enteric and Other Infections and Future Priorities. J. Infect. Dis. 2000, 182, S134–S138. [Google Scholar] [CrossRef] [Green Version]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Gupta, S.; Brazier, A.K.M.; Lowe, N.M. Zinc deficiency in low- and middle-income countries: Prevalence and approaches for mitigation. J. Hum. Nutr. Diet. 2020, 33, 624–643. [Google Scholar] [CrossRef]
- Horton, S.; Ross, J. The economics of iron deficiency. Food Policy 2003, 28, 51–75. [Google Scholar] [CrossRef]
- Horton, S.; Mannar, V.; Wesley, A. Best Practices Paper: Food Fortification with Iron and Iodine; Copenhagen Consensus Center: Lowell, MA, USA, 2008; Working Paper October 2008. [Google Scholar]
- Global Panel on Agriculture and Food Systems for Nutrition. Future Food Systems: For People, Our Planet, and Prosperity; Global Panel on Agriculture and Food Systems for Nutrition: London, UK, 2020; Available online: https://www.glopan.org/foresight2/ (accessed on 21 January 2022).
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D.; Global Burden of Diseases, N.; Chronic Diseases Expert, G. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142. [Google Scholar] [CrossRef] [Green Version]
- Ronto, R.; Wu, J.H.; Singh, G.M. The global nutrition transition: Trends, disease burdens and policy interventions. Public Health Nutr. 2018, 21, 2267–2270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunford, E.; Farrand, C.; Huffman, M.; Thout, S.R.; Shahid, M.; Mhurchu, C.N.; Neal, B.; Johnson, C. Availability, healthiness, and price of packaged and unpackaged foods in India: A cross-sectional study. Nutr. Health 2021. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Dietary Reference Intakes for Sodium and Potassium; The National Academies Press: Washington, DC, USA, 2019; p. 594. [Google Scholar]
- Collaborators, G.B.D.R.F. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef] [Green Version]
- Mozaffarian, D.; Fahimi, S.; Singh, G.M.; Micha, R.; Khatibzadeh, S.; Engell, R.E.; Lim, S.; Danaei, G.; Ezzati, M.; Powles, J.; et al. Global sodium consumption and death from cardiovascular causes. N. Engl. J. Med. 2014, 371, 624–634. [Google Scholar] [CrossRef] [Green Version]
- Powles, J.; Fahimi, S.; Micha, R.; Khatibzadeh, S.; Shi, P.; Ezzati, M.; Engell, R.E.; Lim, S.S.; Danaei, G.; Mozaffarian, D.; et al. Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013, 3, e003733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Development Initiatives. 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition; Development Initiatives: Bristol, UK, 2018. [Google Scholar]
- Hawkes, C.; Ruel, M.T.; Salm, L.; Sinclair, B.; Branca, F. Double-duty actions: Seizing programme and policy opportunities to address malnutrition in all its forms. Lancet 2020, 395, 142–155. [Google Scholar] [CrossRef]
- Houston, R.; Tsang, B.L.; Gorstein, J. The Double-Fortified Salt (Iodized Salt with Iron) Consultation: A Process for Developing Evidence-Based Considerations for Countries. J. Nutr. 2021, 151, 1s–2s. [Google Scholar] [CrossRef]
- Wadman, M. Beset by neural tube defects, Ethiopia may fortify salt. Science 2019, 366, 1177–1178. [Google Scholar] [CrossRef]
- Garcia-Casal, M.N.; Peña-Rosas, J.P.; McLean, M.; De-Regil, L.M.; Zamora, G. Fortification of condiments with micronutrients in public health: From proof of concept to scaling up. Ann. N. Y. Acad. Sci. 2016, 1379, 38–47. [Google Scholar] [CrossRef]
- World Health Organization and Food and Agriculture Organization of the United Nations. Guidelines on Food Fortification with Micronutrients; Allen, L., de Benoist, B., Dary, O., Hurrell, R., Eds.; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Diosady, L.L.; Mannar, M.G.V.; Krishnaswamy, K. Improving the lives of millions through new double fortification of salt technology. Matern. Child Nutr. 2019, 15, e12773. [Google Scholar] [CrossRef] [PubMed]
- Dold, S.; Zimmermann, M.B.; Jeroense, F.; Zeder, C.; Habeych, E.; Galaffu, N.; Grathwohl, D.; Tajeri Foman, J.; Merinat, S.; Rey, B.; et al. Iron bioavailability from bouillon fortified with a novel ferric phytate compound: A stable iron isotope study in healthy women (part II). Sci. Rep. 2020, 10, 5339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cercamondi, C.I.; Duchateau, G.S.M.J.E.; Harika, R.K.; van den Berg, R.; Murray, P.; Koppenol, W.P.; Zeder, C.; Zimmermann, M.B.; Moretti, D. Sodium pyrophosphate enhances iron bioavailability from bouillon cubes fortified with ferric pyrophosphate. Br. J. Nutr. 2016, 116, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Engle-Stone, R.; Ndjebayi, A.O.; Nankap, M.; Brown, K.H. Consumption of potentially fortifiable foods by women and young children varies by ecological zone and socio-economic status in Cameroon. J. Nutr. 2012, 142, 555–565. [Google Scholar] [CrossRef] [Green Version]
- Friesen, V.M.; Mbuya, M.N.N.; Aaron, G.J.; Pachón, H.; Adegoke, O.; Noor, R.A.; Swart, R.; Kaaya, A.; Wieringa, F.T.; Neufeld, L.M. Fortified Foods Are Major Contributors to Apparent Intakes of Vitamin A and Iodine, but Not Iron, in Diets of Women of Reproductive Age in 4 African Countries. J. Nutr. 2020, 150, 2183–2190. [Google Scholar] [CrossRef]
- Hess, S.Y.; Brown, K.H.; Sablah, M.; Engle-Stone, R.; Aaron, G.J.; Baker, S.K. Results of Fortification Rapid Assessment Tool (FRAT) surveys in sub-Saharan Africa and suggestions for future modifications of the survey instrument. Food Nutr. Bull. 2013, 34, 21–38. [Google Scholar] [CrossRef] [Green Version]
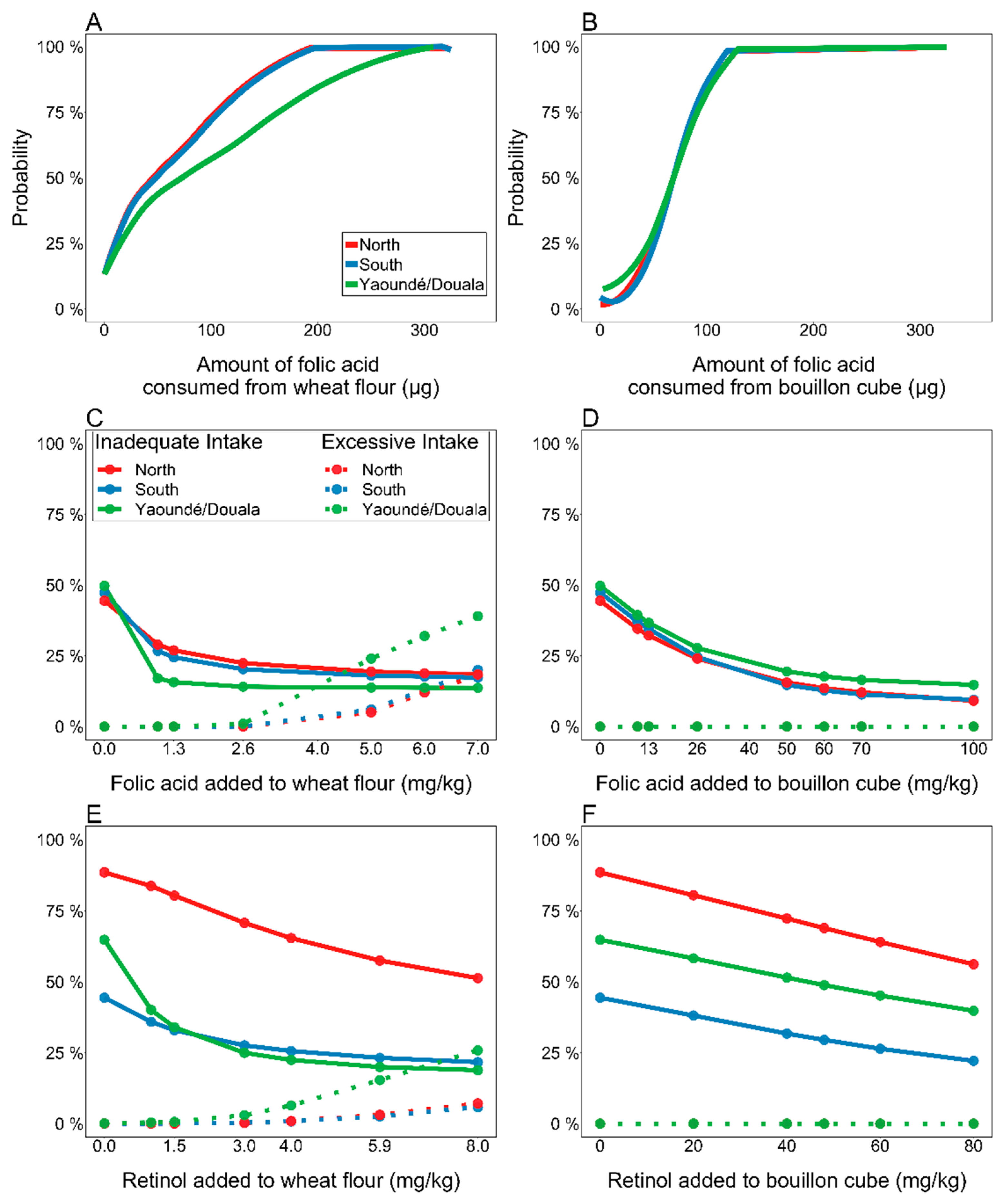
- Engle-Stone, R.; Vosti, S.A.; Luo, H.; Kagin, J.; Tarini, A.; Adams, K.P.; French, C.; Brown, K.H. Weighing the risks of high intakes of selected micronutrients compared with the risks of deficiencies. Ann. N. Y. Acad. Sci. 2019, 1446, 81–101. [Google Scholar] [CrossRef]
- Engle-Stone, R.; Nankap, M.; Ndjebayi, A.O.; Brown, K.H. Simulations based on representative 24-h recall data predict region-specific differences in adequacy of vitamin A intake among Cameroonian women and young children following large-scale fortification of vegetable oil and other potential food vehicles. J. Nutr. 2014, 144, 1826–1834. [Google Scholar] [CrossRef] [Green Version]
- Engle-Stone, R.; Adams, K.; Kumordzie, S.; Luo, H.; Wessells, K.R.; Adu-Afarwuah, S.; Ndjebayi, A.; Teta, I.; Régis, Y.-L.; Haskell, M.; et al. Analyses Using National Survey Data from Cameroon, Haiti, and Ghana Indicate the Potential for Bouillon Fortification to Help Fill Dietary Gaps for 5 Nutrients. Curr. Dev. Nutr. 2021, 5, 640. [Google Scholar] [CrossRef]
- Feyrer, J.; Politi, D.; Weil, D.N. The Cognitive Effects of Micronutrient Deficiency: Evidence from Salt Iodization in the United States. J. Eur. Econ. Assoc. 2017, 15, 355–387. [Google Scholar] [CrossRef]
- Gorstein, J.L.; Bagriansky, J.; Pearce, E.N.; Kupka, R.; Zimmermann, M.B. Estimating the Health and Economic Benefits of Universal Salt Iodization Programs to Correct Iodine Deficiency Disorders. Thyroid 2020, 30, 1802–1809. [Google Scholar] [CrossRef] [PubMed]
- Larson, L.M.; Cyriac, S.; Djimeu, E.W.; Mbuya, M.N.N.; Neufeld, L.M. Can Double Fortification of Salt with Iron and Iodine Reduce Anemia, Iron Deficiency Anemia, Iron Deficiency, Iodine Deficiency, and Functional Outcomes? Evidence of Efficacy, Effectiveness, and Safety. J. Nutr. 2021, 151, 15S–28S. [Google Scholar] [CrossRef] [PubMed]
- Vosti, S.A.; Kagin, J.; Engle-Stone, R.; Luo, H.; Tarini, A.; Clermont, A.; Assiene, J.G.; Nankap, M.; Brown, K.H. Strategies to achieve adequate vitamin A intake for young children: Options for Cameroon. Ann. N. Y. Acad. Sci. 2020, 1465, 161–180. [Google Scholar] [CrossRef] [PubMed]
- Horton, S.; Levin, C. Cost-effectiveness of interventions for reproductive, maternal, neonatal, and child health. In Reproductive, Maternal, Newborn, and Child Health. Disease Control Priorities, 3rd ed.; Black, R.E., Laxminarayan, R., Temmerman, M., Walker, N., Eds.; World Bank: Washington, DC, USA, 2016; Volume 2. [Google Scholar]
- Bhat, S.; Marklund, M.; Henry, M.E.; Appel, L.J.; Croft, K.D.; Neal, B.; Wu, J.H.Y. A Systematic Review of the Sources of Dietary Salt around the World. Adv. Nutr. 2020, 11, 677–686. [Google Scholar] [CrossRef]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- World Health Organization. A Global Brief on Hypertension. Silent Killer, Global Public Health Crisis; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Zhou, B.; Bentham, J.; Di Cesare, M.; Bixby, H.; Danaei, G.; Cowan, M.J.; Paciorek, C.J.; Singh, G.; Hajifathalian, K.; Bennett, J.E.; et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef] [Green Version]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Rural and Urban Communities in High-, Middle-, and Low-Income Countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef] [Green Version]
- Webb, M.; Fahimi, S.; Singh, G.M.; Khatibzadeh, S.; Micha, R.; Powles, J.; Mozaffarian, D. Cost effectiveness of a government supported policy strategy to decrease sodium intake: Global analysis across 183 nations. BMJ 2017, 356, i6699. [Google Scholar] [CrossRef] [Green Version]
- Archer, N.; Cochet-Broch, M.; Mihnea, M.; Garrido-Banuelos, G.; Lopez-Sanchez, P.; Lundin, L.; Frank, D. Sodium reduction in bouillon: Targeting a food staple to reduce hypertension in Sub-Saharan Africa. Front. Nutr. 2022; in press. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013–2020; Global Action Plan for the Prevention and Control of NCDs 2013–2020; WHO Press: Geneva, Switzerland, 2013. [Google Scholar]
- Santos, J.A.; Tekle, D.; Rosewarne, E.; Flexner, N.; Cobb, L.; Al-Jawaldeh, A.; Kim, W.J.; Breda, J.; Whiting, S.; Campbell, N.; et al. A Systematic Review of Salt Reduction Initiatives around the World: A Midterm Evaluation of Progress towards the 2025 Global Non-Communicable Diseases Salt Reduction Target. Adv. Nutr. 2021, 12, 1768–1780. [Google Scholar] [CrossRef]
- Webster, J.; Trieu, K.; Dunford, E.; Hawkes, C. Target Salt 2025: A Global Overview of National Programs to Encourage the Food Industry to Reduce Salt in Foods. Nutrients 2014, 6, 3274–3287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adeyemo, A.A.; Prewitt, T.E.; Luke, A.; Omotade, O.O.; Rotimi, C.N.; Brieger, W.R.; Cooper, R.S. The feasibility of implementing a dietary sodium reduction intervention among free-living normotensive individuals in south west Nigeria. Ethn. Dis. 2002, 12, 207–212. [Google Scholar] [PubMed]
- Neal, B.; Wu, Y.; Feng, X.; Zhang, R.; Zhang, Y.; Shi, J.; Zhang, J.; Tian, M.; Huang, L.; Li, Z.; et al. Effect of Salt Substitution on Cardiovascular Events and Death. N. Engl. J. Med. 2021, 385, 1067–1077. [Google Scholar] [CrossRef] [PubMed]
- Vandevijvere, S. Sodium reduction and the correction of iodine intake in Belgium: Policy options. Arch. Public Health 2012, 70, 10. [Google Scholar] [CrossRef] [Green Version]
- Menyanu, E.; Corso, B.; Minicuci, N.; Rocco, I.; Zandberg, L.; Baumgartner, J.; Russell, J.; Naidoo, N.; Biritwum, R.; Schutte, A.E.; et al. Salt-reduction strategies may compromise salt iodization programs: Learnings from South Africa and Ghana. Nutrition 2021, 84, 111065. [Google Scholar] [CrossRef]
- Drewnowski, A.; Garrett, G.S.; Kansagra, R.; Khan, N.; Kupka, R.; Kurpad, A.V.; Mannar, V.; Martorell, R.; Zimmermann, M.B.; for the Double Fortified Salt Consultation Steering Group. Key Considerations for Policymakers—Iodized Salt as a Vehicle for Iron Fortification: Current Evidence, Challenges, and Knowledge Gaps. J. Nutr. 2021, 151, 64S–73S. [Google Scholar] [CrossRef]
- Benson, T.; Lavelle, F.; McCloat, A.; Mooney, E.; Bucher, T.; Egan, B.; Dean, M. Are the Claims to Blame? A Qualitative Study to Understand the Effects of Nutrition and Health Claims on Perceptions and Consumption of Food. Nutrients 2019, 11, 2058. [Google Scholar] [CrossRef] [Green Version]
- Olivieri, A.; Giorgino, F.; Maffeis, C.; Bagnasco, M. Salt reduction and iodine intake in Italy. J. Endocrinol. Investig. 2021. [Google Scholar] [CrossRef]
- World Health Organization. Salt Reduction and Iodine Fortification Strategies in Public Health: Report of a Joint Technical Meeting Convened by the World Health Organization and the George Institute for Global Health in Collaboration with the International Council for the Control of Iodine Deficiency Disorders Global Network, Sydney, Australia, March 2013; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Charlton, K.; Ware, L.J.; Baumgartner, J.; Cockeran, M.; Schutte, A.E.; Naidoo, N.; Kowal, P. How will South Africa’s mandatory salt reduction policy affect its salt iodisation programme? A cross-sectional analysis from the WHO-SAGE Wave 2 Salt & Tobacco study. BMJ Open 2018, 8, e020404. [Google Scholar] [CrossRef] [Green Version]
- Campbell, N.; Dary, O.; Cappuccio, F.P.; Neufeld, L.M.; Harding, K.B.; Zimmermann, M.B. Collaboration to optimize dietary intakes of salt and iodine: A critical but overlooked public health issue. Bull. World Health Organ. 2012, 90, 73–74. [Google Scholar] [CrossRef]
- Campbell, N.R.C.; Dary, O.; Cappuccio, F.P.; NeufeldI, L.M.; Harding, K.B.; Zimmermann, M.B. Need for coordinated programs to improve global health by optimizing salt and iodine intake. Rev. Panam. Salud Publica 2012, 32, 281–286. [Google Scholar] [CrossRef] [Green Version]
- Andersson, M.; Hunziker, S.; Fingerhut, R.; Zimmermann, M.B.; Herter-Aeberli, I. Effectiveness of increased salt iodine concentration on iodine status: Trend analysis of cross-sectional national studies in Switzerland. Eur. J. Nutr. 2020, 59, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Watutantrige-Fernando, S.; Barollo, S.; Bertazza, L.; Cavedon, E.; Censi, S.; Manso, J.; Vianello, F. Food Hygiene, Nutrition Services SIAN, Mian, C. Efficacy of educational intervention to improve awareness of the importance of iodine, use of iodized salt, and dietary iodine intake in northeastern Italian schoolchildren. Nutrition 2018, 53, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Shields, A.; Ansari, M.A. Review of Experience of the Production of Salt Fortified with Iron and Iodine. J. Nutr. 2021, 151, 29S–37S. [Google Scholar] [CrossRef] [PubMed]
- Cyriac, S.; Haardörfer, R.; Neufeld, L.M.; Girard, A.W.; Ramakrishnan, U.; Martorell, R.; Mbuya, M.N.N. High Coverage and Low Utilization of the Double Fortified Salt Program in Uttar Pradesh, India: Implications for Program Implementation and Evaluation. Curr. Dev. Nutr. 2020, 4, nzaa133. [Google Scholar] [CrossRef]
- Wegmüller, R.; Zimmermann, M.B.; Hurrell, R.F. Dual Fortification of Salt with Iodine and Encapsulated Iron Compounds: Stability and Acceptability Testing in Morocco and Côte d’Ivoire. J. Food Sci. 2003, 68, 2129–2135. [Google Scholar] [CrossRef]
- Hackl, L.; Cercamondi, C.I.; Zeder, C.; Wild, D.; Adelmann, H.; Zimmermann, M.B.; Moretti, D. Cofortification of ferric pyrophosphate and citric acid/trisodium citrate into extruded rice grains doubles iron bioavailability through in situ generation of soluble ferric pyrophosphate citrate complexes. Am. J. Clin. Nutr. 2016, 103, 1252–1259. [Google Scholar] [CrossRef] [Green Version]
- Anselmo, A.C.; Xu, X.; Buerkli, S.; Zeng, Y.; Tang, W.; McHugh, K.J.; Behrens, A.M.; Rosenberg, E.; Duan, A.R.; Sugarman, J.L.; et al. A heat-stable microparticle platform for oral micronutrient delivery. Sci. Transl. Med. 2019, 11, eaaw3680. [Google Scholar] [CrossRef]
- Rogers, B.L.; Somé, J.W.; Bakun, P.; Adams, K.P.; Bell, W.; Wafa, S.; Coates, J. Validation of the INDDEX24 mobile app vs. a pen-and-paper 24-hour dietary recall using the weighed food record as a benchmark in Burkina Faso. Br. J. Nutr. 2021, 1–41. [Google Scholar] [CrossRef]
- Luo, H.; Dodd, K.W.; Arnold, C.D.; Engle-Stone, R. Introduction to the SIMPLE Macro, a Tool to Increase the Accessibility of 24-Hour Dietary Recall Analysis and Modeling. J. Nutr. 2021, 151, 1329–1340. [Google Scholar] [CrossRef]
- Friesen, V.M.; Jungjohann, S.; Mbuya, M.N.N.; Harb, J.; Visram, A.; Hug, J.; Garrett, G.S.; Neufeld, L.M. Fortification Assessment Coverage Toolkit (FACT) Manual. Global Alliance for Improved Nutrition (Geneva) and Oxford Policy Management (Oxford). 2019. Available online: https://www.gainhealth.org/resources/reports-and-publications/fortification-assessment-coverage-toolkit-fact (accessed on 21 January 2022).
- Coates, J.; Colaiezzi, B.; Fiedler, J.L.; Wirth, J.; Lividini, K.; Rogers, B. A Program Needs-Driven Approach to Selecting Dietary Assessment Methods for Decision-Making in Food Fortification Programs. Food Nutr. Bull. 2012, 33, S146–S156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matthias, D.; McDonald, C.M.; Archer, N.; Engle-Stone, R. The Role of Multiply-Fortified Table Salt and Bouillon in Food Systems Transformation. Nutrients 2022, 14, 989. https://doi.org/10.3390/nu14050989
Matthias D, McDonald CM, Archer N, Engle-Stone R. The Role of Multiply-Fortified Table Salt and Bouillon in Food Systems Transformation. Nutrients. 2022; 14(5):989. https://doi.org/10.3390/nu14050989
Chicago/Turabian StyleMatthias, Dipika, Christine M. McDonald, Nicholas Archer, and Reina Engle-Stone. 2022. "The Role of Multiply-Fortified Table Salt and Bouillon in Food Systems Transformation" Nutrients 14, no. 5: 989. https://doi.org/10.3390/nu14050989
APA StyleMatthias, D., McDonald, C. M., Archer, N., & Engle-Stone, R. (2022). The Role of Multiply-Fortified Table Salt and Bouillon in Food Systems Transformation. Nutrients, 14(5), 989. https://doi.org/10.3390/nu14050989





