Vitamin D Deficiency and Its Associated Factors among Female Migrants in the United Arab Emirates
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Ethics
2.2. Selection of Study Participants
2.3. Inclusion Criteria
2.4. Measures
2.5. Statistical Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lips, P.; de Jongh, R.T.; Van Schoor, N.M. Trends in Vitamin D Status Around the World. JBMR Plus 2020, 12, e10585. [Google Scholar] [CrossRef] [PubMed]
- Saraf, R.; Morton, S.M.B.; Camargo, C.A.; Grant, C.C. Global summary of maternal and newborn vitamin D status—A systematic review. Matern. Child Nutr. 2016, 12, 647–668. [Google Scholar] [CrossRef] [PubMed]
- Bi, W.G.; Nuyt, A.M.; Weiler, H.; Leduc, L.; Santamaria, C.; Wei, S.Q. Association between vitamin D supplementation during pregnancy and offspring growth, morbidity, and mortality: A systematic review and meta-analysis. JAMA Pediatr. 2018, 7, 635–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oristrell, J.; Oliva, J.C.; Casad, E.; Subirana, I.; Dominguez, D.; Toloba, A.; Balado, A.; Grau, M.J. Vitamin D supplementation and COVID-19 risk: A population-based, cohort study. J. Endocrinol. Investig. 2021, 45, 167–179. [Google Scholar] [CrossRef]
- Dissanayake, H.A.; de Silva, N.L.; Sumanatilleke, M.; de Silva, S.D.N.; Gamage, K.K.K.; Dematapitiya, C.; Kuruppu, D.C.; Ranasimghe, P.; Sumanathan, S.; Katulanda, P.J. Prognostic and therapeutic role of vitamin D in COVID-19: Systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2021, 20, dgab892. [Google Scholar] [CrossRef] [PubMed]
- Rejnmark, L.; Bislev, L.S.; Cashman, K.D.; Eirlksdottir, G.; Gaksch, M.; Grubler, M.; Grimnes, G.; Gudnason, V.; Lips, P.; Pilz, S.; et al. Non-skeletal healtheffects of vitamin D supplementation: A systematic review on finding from meta-analyses summarizing trial data. PLoS ONE 2017, 12, e0180512. [Google Scholar] [CrossRef] [Green Version]
- Pludowski, P.; Holick, M.F.; Grant, W.B.; Konstantynowicz, J.; Mascarenhas, M.R.; Haq, A.; Povoroznyuk, V.; Balatska, N.; Barbosa, A.P.; Karonova, T.; et al. Vitamin D supplementation guidelines. J. Steroid Biochem. Mol. Biol. 2018, 175, 125–135. [Google Scholar] [CrossRef] [Green Version]
- Chakhtoura, M.; Rahme, M.; Chamoun, N.; Fuleihan, G.E. Vitamin D in the Middle East, and North Africa. Bone Rep. 2018, 8, 135–146. [Google Scholar] [CrossRef]
- Grant, W.B.; Fakhoury, H.M.A.; Karras, S.N.; Al Anouti, F.; Bhattoa, H.P. Variations in 25-Hydroxyvitamin D in countries from the Middle East and Europe: The Roles of UVB Exposure and Diet. Nutrients 2019, 11, 2065. [Google Scholar] [CrossRef] [Green Version]
- Welch, T.R.; Bergstrom, W.H.; Tsang, R.C. Vitamin D-deficient rickets: The re-emergence of a once conquered disease. J. Pediatr. 2000, 137, 143–145. [Google Scholar] [CrossRef] [PubMed]
- Yared, M.N.; Chemali, R.; Yaacoub, N.; Halaby, G. Hypovitaminosis D in a sunny country: Relation to lifestyle and bone markers. J. Bone Miner. Res. 2000, 15, 1856–1862. [Google Scholar] [CrossRef]
- Sedrani, K.M.; Elidrissy, A.W.T.H.; El-Arabi, K.M. Sunlight and vitamin D status in normal Saudi subjects. Am. J. Clin. Nutr. 1983, 38, 129–132. [Google Scholar] [CrossRef]
- Hobbs, R.D.; Habib, Z.; Alromaihi, D.; Ldi, L.; Parikh, N.; Blocki, F.; Rao, D.S. Severe vitamin D deficiency in Arab-American women living in Dearborn, Michigan. Endocr. Pract. 2009, 15, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Muhairi, S.J.; Mehairi, A.E.; Khouri, A.A.; Naqbi, M.; Maskari, F.; Al Kaabi, J.; Al Dhaheri, A.; Naglekerke, N.; Shah, S. Vitamin D deficiency among healthy adolescents in Al Ain, United Arab Emirates. BMC Public Health 2013, 13, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Arab Emirates Ministry of Economy. Preliminary Results of Population, Housing, and Establishment Census 2005, United Arab Emirates 2006. Available online: http://www.cscc.unc.edu/uaee/public/UNLICOMMUAE2005CensusResults07282008.pdf (accessed on 10 June 2020).
- Yousef, S.; Elliott, J.; Manuel, D.; Colman, I.; Papadimitropoulos, M.; Hossain, A.; Leclair, N.; Well, G.A. Study protocol: Worldwide comparison of vitamin D status of immigrants from different ethnic origins and native-born populations-a systematic review and meta-analysis. Syst. Rev. 2019, 8, 211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, S.M.; Ali, R.; Loney, T.; Aziz, F.; ElBarazi, I.; Al Dhaheri, S.; Farooqi, M.H.; Blair, I. Prevalence of diabetes among migrant women and duration of residence in the United Arab Emirates: A cross sectional study. PLoS ONE 2017, 12, e0169949. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The WHO STEPwise Approach to Noncommunicable Disease Risk Factor Surveillance. Available online: https://www.who.int/ncds/surveillance/steps/STEPS_Manual.pdf (accessed on 16 May 2020).
- Herrick, K.A.; Storandt, R.J.; Afful, J.; Pfeiffer, C.M.; Schleicher, R.L.; Gahche, J.J.; Potischman, N. Vitamin D status in the United States 2011–2014. Am. J. Clin. Nutr. 2019, 110, 150–157. [Google Scholar] [CrossRef] [Green Version]
- Pottie, K.; Greenaway, C.; Feightner, J.; Welch, V.; Swinkels, H.; Rashid, M.; Narasiah, L.; Kirmayer, L.J.; Ueffing, E.; MacDonald, N.E.; et al. Evidence-based clinical guidelines for immigrants and refugees. CMAJ 2011, 183, E824–E925. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J. Hypertens. 1999, 17, 151–183. [Google Scholar]
- International Physical Activity Questionnaire (IPAQ). Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. 2005. Available online: http://www.ipaq.ki.se/scoring.pdf (accessed on 16 May 2020).
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haq, A.; Svobodova, J.; Imran, S.; Stanford, C.; Razzaque, M.S. Vitamin D deficiency: A single center analysis of patients from 136 countries. J. Steroid Biochem. Mol. Biol. 2016, 164, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Schleicher, R.L.; Sternberg, M.R.; Looker, A.C.; Yetley, E.A.; Lacher, D.A.; Sempos, C.T.; Taylor, C.L.; Durazo-Arvizu, R.A.; Maw, K.L.; Chaudhary-Webb, M.; et al. National estimates of serum 25(OH)D and metabolite concentrations measured by liquid chromatography-Tandem, mass spectrometry in the US population during 2007–2010. J. Nutr. 2016, 146, 1051–1061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarafin, K.; Durazo-Arvizu, R.; Tian, L.; Phinney, K.W.; Tai, S.; Camara, J.E.; Merkel, J.; Green, E.; Sempos, C.T.; Brooks, S.P. Standardizing 25-hydoxyvitamin D values from the Canadian Health Measures Survey. Am. J. Clin. Nutr. 2015, 102, 1044–1050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horton-French, K.; Dunlop, E.; Lucas, R.M.; Pereira, G.; Black, L.J. Prevalence and predictors of vitamin D deficiency in a nationally representative sample of Australian adolescents and young adults. Eur. J. Clin. Nutr. 2021, 75, 1627–1636. [Google Scholar] [CrossRef]
- Lips, P.; Cashman, K.D.; Lamberg-Allardt, C.; Bischoff-Ferrari, H.A.; Obermayer-Pietsch, B.R.; Bianchi, M.; Stepan, J.; El-Hajj Fuleihan, G.; Bouillon, R. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: A position statement of the European Calcified Tissue Society. Eur. J. Endocrinol. 2019, 180, 23–54. [Google Scholar] [CrossRef] [Green Version]
- Mogire, R.M.; Mutua, A.; Kimita, W.; Kamau, A.; Bejon, P.; Pettifor, J.M.; Adeyemo, A.; Williams, T.N.; Atkinson, S.H. Prevalence of vitamin D deficiency in Africa: A systematic review and meta-analysis. Lancet Glob. Health 2020, 8, e134-42. [Google Scholar] [CrossRef] [Green Version]
- Clemens, T.L.; Henderson, S.L.; Adams, J.S.; Holick, M.F. Increased skin pigment reduces the capacity skin to synthesise vitamin D3. Lancet 1982, 319, 4–6. [Google Scholar] [CrossRef]
- Nesby-O’Dell, S.; Scanlon, K.S.; Cogswell, M.E.; Gillespie, C.; Hollis, B.W.; Looker, A.C.; Allen, C.; Doughertly, C.; Gunter, E.W.; Bowman, B.A. Hypovitaminosis D prevalence and determinants among White women of reproductive age: Third National and Nutrition Examination Survey 1988–1994. Am. J. Clin. Nutr. 2002, 76, 187–192. [Google Scholar] [CrossRef] [Green Version]
- Yetley, E.A. Assessing the Vitamin D status of the US population. Am. J. Clin. Nutr. 2008, 88, 558S–564S. [Google Scholar] [CrossRef]
- Jiang, Z.; Pu, R.; Li, N.; Chen, C.; Li, J.; Dai, W.; Wang, Y.; Hu, J.; Zhu, D.; Yu, Q.; et al. High prevalence of vitamin D deficiency in Asia: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2021, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kambo, P.; Dwivedi, S.; Toteja, G.S. Prevalence of hypovitaminosis D in India & wayfoward. Indian J. Med. Res. 2018, 148, 548–556. [Google Scholar] [CrossRef]
- Darling, A.L. Vitamin D deficiency in western dwelling South Asian populations: An unrecognized epidemic. Proc. Nutr. Soc. 2020, 79, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Brock, K.; Huang, W.Y.; Fraser, D.R.; Ke, L.; Tseng, M.; Stolzenberg-Solomon, R.; Peters, U.; Ahn, J.; Purdue, M.; Mason, R.S.; et al. Low vitamin D is associated with physical inactivity, obesity and low vitamin D intake in a large US sample of healthy middle-aged men and women. J. Steroid Biochem. Mol. Biol. 2010, 121, 462–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zumaraga, M.P.; Concepcion, M.A.; Duante, C.; Rodriguez, M. Next Generation Sequencing of Lifestyle and Nutrition related genetic polymorphisms reveals independent loci for low serum 25-hydroxyvitamin D levels among adult respondents of the 2013 Philippine National Nutrition Survey. J. Asean Fed. Endocr. Soc. 2021, 36, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Valentini, A.; Perrone, M.A.; Cianfarani, M.A.; Tarantino, U.; Massoud, R.; Merra, G.; Bernardini, S.; Morris, H.A.; Bertoli, A. Obesity, vitamin D status and physical activity: 1,25(OH)2D as a potential marker of vitamin D deficiency in obese subjects. Panminerva Med. 2020, 62, 83–92. [Google Scholar] [CrossRef]
- De Oliveira, L.F.; De Azevedo, L.G.; da Mota Santana, J.; de Sales, L.P.C.; Pereira Santos, M. Obesity and overweight decreases the effect of 25(OH) D supplementation in adults: Systematic review and meta-analysis of randomized controlled trials. Rev. Endocr. Metab. Disord. 2020, 21, 61. [Google Scholar] [CrossRef]
- Holick, M.F. Biological Effects of Sunlight, Ultraviolet Radiation, Visible Light, Infrared Radiation and Vitamin D for Health. Anticancer Res. 2016, 36, 1345–1356. [Google Scholar]
- Pietiläinen, K.H.; Kaprio, J.; Borg, P.; Plasqui, G.; Yki-Järvinen, H.; Kujala, U.M.; Rose, R.J.; Westerterp, K.R.; Rissanen, A. Physical inactivity and obesity: A vicious circle. Obesity 2008, 16, 409–414. [Google Scholar] [CrossRef]
- Scott, D.; Blizzard, L.; Fell, J.; Ding, C.; Winzenberg, T.; Jones, G. A prospective study of the associations between 25-hydroxy-vitamin D, sarcopenia progression and physical activity in older adults. Clin. Endocrinol. 2010, 73, 581–587. [Google Scholar] [CrossRef]
- Pang, Y.; Kim, O.; Choi, J.A.; Jung, H.; Kim, J.; Lee, H.; Lee, H. Vitamin D deficiency and associated factors in south Korean childbearing women: A cross-sectional study. BMC Nurs. 2021, 20, 218. [Google Scholar] [CrossRef] [PubMed]
- Al-Othman, A.; Al-Musharaf, S.; Al-Daghri, N.M.; Krishnaswamy, S.; Yusuf, D.S.; Alkharfy, K.M.; Al-Saleh, Y.; Al-Attas, O.S.; Alokail, M.S.; Moharram, O.; et al. Effect of physical activity and sun exposure on vitamin D status of Saudi children and adolescents. BMC Pediatr. 2012, 12, 92. [Google Scholar]
- Liu, X.; Baylin, A.; Levy, P.D. Vitamin D deficiency and insufficiency among US adults: Prevalence, predictors and clinical implications. Br. J. Nutr. 2018, 119, 928–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 June 2021).
- Haq, A.; Wimalawansa, S.J.; Pludowski, P.; Anouti, F.A. Clinical practice guidelines for vitamin D in the United Arab Emirates. J. Steroid Biochem. Mol. Biol. 2018, 175, 4–11. [Google Scholar] [CrossRef]
- Zemel, M.B.; Shi, H.; Greer, B.; Dirienzo, D.; Zemel, P.C. Regulation of adiposity by dietary calcium. FASEB J. 2000, 14, 1132–1138. [Google Scholar] [CrossRef]
- Chang, E.; Kim, Y. Vitamin D decreases adipocyte lipid storage and increases NAD-SIRT1 pathway in 3T3-L1 adipocytes. Nutrition 2016, 32, 702–708. [Google Scholar] [CrossRef] [Green Version]
- De Pergola, G.; Martino, T.; Zupo, R.; Caccavo, D.; Pecorella, C.; Paradiso, S.; Silvestris, F.; Triggiani, V. 25 Hydroxyvitamin D Levels are Negatively and Independently Associated with Fat Mass in a Cohort of Healthy Overweight and Obese Subjects. Endocr. Metab. Immune Disord. Drug Targets 2019, 19, 838–844. [Google Scholar] [CrossRef]
- Salant, T.; Lauderdale, D.S. Measuring culture: A critical review of acculturation and health in Asian immigrant populations. Soc. Sci. Med. 2003, 57, 71–90. [Google Scholar] [CrossRef]
- Yousef, S.; Manuel, D.; Colman, I.; Papadimitropoulos, M.; Hossain, A.; Faris, M.; Wells, G.A. Vitamin D Status among First-Generation Immigrants from Different Ethnic Groups and Origins: An Observational Study Using the Canadian Health Measures Survey. Nutrients 2021, 13, 2702. [Google Scholar] [CrossRef]
- Sanou, D.; O’Reilly, E.; Ngnie-Teta, I.; Batal, M.; Mondain, N.; Andrew, C.; Newbold, B.K.; Bourgeault, I.L. Acculturation and nutritional health of immigrants in Canada: A scoping review. J. Immigant Minority Health 2014, 16, 24–34. [Google Scholar] [CrossRef] [Green Version]
- Buyukuslu, N.; Esin, K.; Hizli, H.; Sunal, N.; Yigit, P.; Garipagaoglu, M. Clothing preference affects vitamin D status of young women. Nutr. Res. 2014, 34, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Chailurkit, L.O.; Aekplakorn, W.; Ongphiphadhanakul, B. Regional variation and determinants of vitamin D status in sunshine-abundant Thailand. BMC Public Health 2011, 11, 853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, C.A.; Gowda, U.; Renzaho, A.M. The prevalence of vitamin D deficiency among dark-skinned populations according to their stage of migration and region of birth: A meta-analysis. Nutrition 2016, 32, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Harris, S.S. Vitamin D and African Americans. J. Nutr. 2006, 136, 1126–1129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arabi, A. El Rassi, R.; El-Hajj, F.G. Hypovitaminosis D in developing countries-prevalence, risk factors and outcomes. Nat. Rev. Endocrinol. 2010, 6, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Durazo-Arvizu, R.A.; Camacho, P.; Bovet, P.; Forrester, T.; Lambert, E.V.; Plange-Rhule, J.; Hoofnagle, A.N.; Aloia, J.; Tayo, B.; Dugas, L.R.; et al. 25-Hydroxyvitamin D in African-origin populations at varying latitudes challenges the construct of a physiologic norm. Am. J. Clin. Nutr. 2014, 100, 908–914. [Google Scholar] [CrossRef] [PubMed]
- AlZarooni, A.A.R.; AlMarzouqi, F.I.; AlDramaki, S.H.; Prinsloo, E.A.M.; Nagelkerke, N. Prevalence of vitamin D deficiency and associated comorbidities among Abu Dhabi Emirates population. BMC Res. Notes 2019, 12, 503. [Google Scholar] [CrossRef] [Green Version]
- Alrayyes, S.F.; Alrayyes, S.F.; Farooq, U.D. Skin-lightening patterns among female students: A cross-sectional study in Saudi Arabia. Int. J. Women’s Dermatol. 2019, 5, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Janzi, S.; Padilla, E.C.; Najafi KRamne, S.; Ahlqvist, E.; Borne, Y.; Sonestedt, E. Single Nucleotide Polymorphisms in close proximity to the fibroblast growth factor 11 (FG21) Gene Found to be associated with sugar intake in a Swedish population. Nutrients 2021, 13, 3954. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, V.; Faerber, S.J.; Greeff, J.M.; Lefevre, C.E.; Re, D.E.; Perrett, D.I. African Perceptions of Female Attractiveness. PLoS ONE 2012, 7, e48116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shroff, H.; Diedrichs, P.C.; Craddock, N. Skin Color, Cultural Capital, and Beauty Products: An Investigation of the Use of Skin Fairness Products in Mumbai, India. Front. Public Health 2018, 5, 365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, E.P.H.; Min, H.J.; Belk, R.W.; Kimura, J.; Bahl, S. Skin Lightening and Beauty in Four Asian Cultures. Adv. Consum. Res. 2008, 35, 444–449. [Google Scholar]
- Carlberg, C. Nutrigenomics of vitamin D. Nutrients 2019, 11, 676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Filipinas | Arab | South Asian | ||||
|---|---|---|---|---|---|---|---|
| N | n | % | n | % | n | % | |
| All | 553 | 290 | 52.4 | 136 | 24.6 | 127 | 23.0 |
| Age, (years) | |||||||
| 18–30 | 186 | 123 | (43.0) | 43 | (31.6) | 55 | (43.7) |
| 31–40 | 171 | 119 | (41.6) | 45 | (33.3) | 39 | (39.9) |
| ≥41 | 191 | 44 | (15.4) | 47 | (34.8) | 32 | (25.4) |
| Education of the participant | |||||||
| No formal schooling | 39 | 15 | (5.2) | 15 | (11.2) | 9 | (7.3) |
| Up to secondary | 203 | 124 | (43.2) | 40 | (29.8) | 59 | (31.4) |
| College or higher | 303 | 148 | (51.6) | 79 | (59.0) | 76 | (61.3) |
| Marital status | |||||||
| Unmarried | 194 | 137 | (49.6) | 34 | (25.6) | 23 | (18.6) |
| Married | 306 | 118 | (42.8) | 89 | (66.9) | 99 | (79.8) |
| Divorced, or widowed | 33 | 21 | (7.6) | 10 | (7.5) | 2 | (1.6) |
| Occupation | |||||||
| Housemaid | 192 | 176 | 63.6 | 8 | 6.2 | 8 | 6.8 |
| Housewife | 122 | 4 | 1.4 | 64 | 49.6 | 54 | 45.8 |
| Driver | 10 | 10 | 3.6 | 0 | 0 | 0 | 0.0 |
| Cook | 10 | 10 | 3.6 | 0 | 0 | 0 | 0.0 |
| Administrator, supervisor | 35 | 21 | 7.6 | 7 | 5.4 | 7 | 5.9 |
| Teacher | 36 | 5 | 1.8 | 16 | 12.4 | 15 | 12.7 |
| Health care worker | 55 | 23 | 8.3 | 13 | 10.1 | 19 | 16.1 |
| Other | 64 | 28 | 10.1 | 21 | 16.3 | 15 | 12.7 |
| Monthly income, AED (1 USD = 3.6 AED) | |||||||
| Lowest (812.6) | 133 | 125 | (52.5) | 5 | (13.2) | 3 | (6.5) |
| Middle (1365.8) | 85 | 72 | (30.3) | 5 | (13.2) | 8 | (17.4) |
| Highest (7422.8) | 104 | 41 | (17.2) | 28 | (73.6) | 35 | (76.1) |
| Residence in home country, n (%) | |||||||
| Urban | 263 | 129 | (50.8) | 54 | (43.2) | 80 | (67.2) |
| Rural | 235 | 125 | (49.2) | 71 | (56.8) | 39 | (32.8) |
| Duration of residence in UAE | |||||||
| <1 year | 185 | 133 | (53.0) | 27 | (22.9) | 25 | (22.9) |
| 1 to 5 years | 208 | 106 | (42.2) | 43 | (36.4) | 59 | (54.1) |
| ≥5 years | 85 | 12 | (4.8) | 48 | (40.7) | 25 | (23.0) |
| Moderate or vigorous physical activity | |||||||
| Yes | 161 | 133 | (45.9) | 15 | (11.0) | 13 | (10.2) |
| No | 391 | 157 | (54.1) | 121 | 89.0) | 114 | (89.8) |
| Body mass index categories | |||||||
| <25.0 | 294 | 187 | (64.5) | 44 | (32.4) | 63 | (49.6) |
| 25–30 | 166 | 83 | (28.6) | 41 | (30.1 | 42 | (33.1) |
| ≥30.0 | 93 | 20 | (6.9) | 51 | (37.5) | 22 | (17.3) |
| Cigarette smoking, currently | |||||||
| No | 514 | 268 | (92.4) | 122 | (89.7) | 124 | (97.6) |
| Yes | 39 | 22 | (7.6) | 14 | (10.3) | 3 | (2.4) |
| Alcohol consumption | |||||||
| No | 448 | 193 | (66.6) | 135 | (99.3) | 120 | (94.5) |
| Yes | 105 | 97 | (33.4) | 1 | (0.7) | 7 | (5.5) |
| Hemoglobin A1c level | |||||||
| <5.7% | 151 | 52 | (91.2) | 64 | (71.1) | 35 | (53.9) |
| 5.7–6.4% | 38 | 4 | (7.0) | 15 | (16.7) | 19 | (29.2) |
| ≥6.5% | 23 | 1 | (1.8) | 11 | (12.2) | 11 | (16.9) |
| Blood pressure, mm Hg | 363 | 188 | (64.8) | 93 | (68.4) | 82 | (64.6) |
| <140/90 | 190 | 102 | (35.2) | 43 | (31.6) | 45 | (35.4) |
| ≥140/90 or on hypertension medication | |||||||
| Levels of the serum 25(OH)D concentrations (ng/mL) | |||||||
| Mean (ng/mL, (± SD) | 20 (±12) | 30 | (±11) | 14 | (±10) | 15 | (±9) |
| Serum 25(OH)D concentrations by category | |||||||
| >20 ng/mL (50 nmol/L), n (%) | 71 (33.3) | 48 | (84.2) | 12 | (13.3) | 11 | (16.7) |
| ≤20 ng/mL (50 nmol/L) | 142 (66.7) | 9 | (15.8) | 78 | (86.7) | 55 | (83.3) |
| Variable | 25(OH)D Levels (ng/mL) | ||||||
|---|---|---|---|---|---|---|---|
| <20 ng/mL) | |||||||
| N | Mean | (±SD) | p | % | (95% CI) | p | |
| All | 213 | 19 | (11) | 66.7 | (60.0–72.7) | ||
| Age, (years) | |||||||
| 18–34 | 113 | 18 | (12) | 0.37 | 68.1 | (58.9–76.1) | 0.38 |
| 35–44 | 57 | 20 | (14) | 59.6 | (47.1–72.2) | ||
| ≥45 | 43 | 18 | (11) | 72.1 | (55.8–83.2) | ||
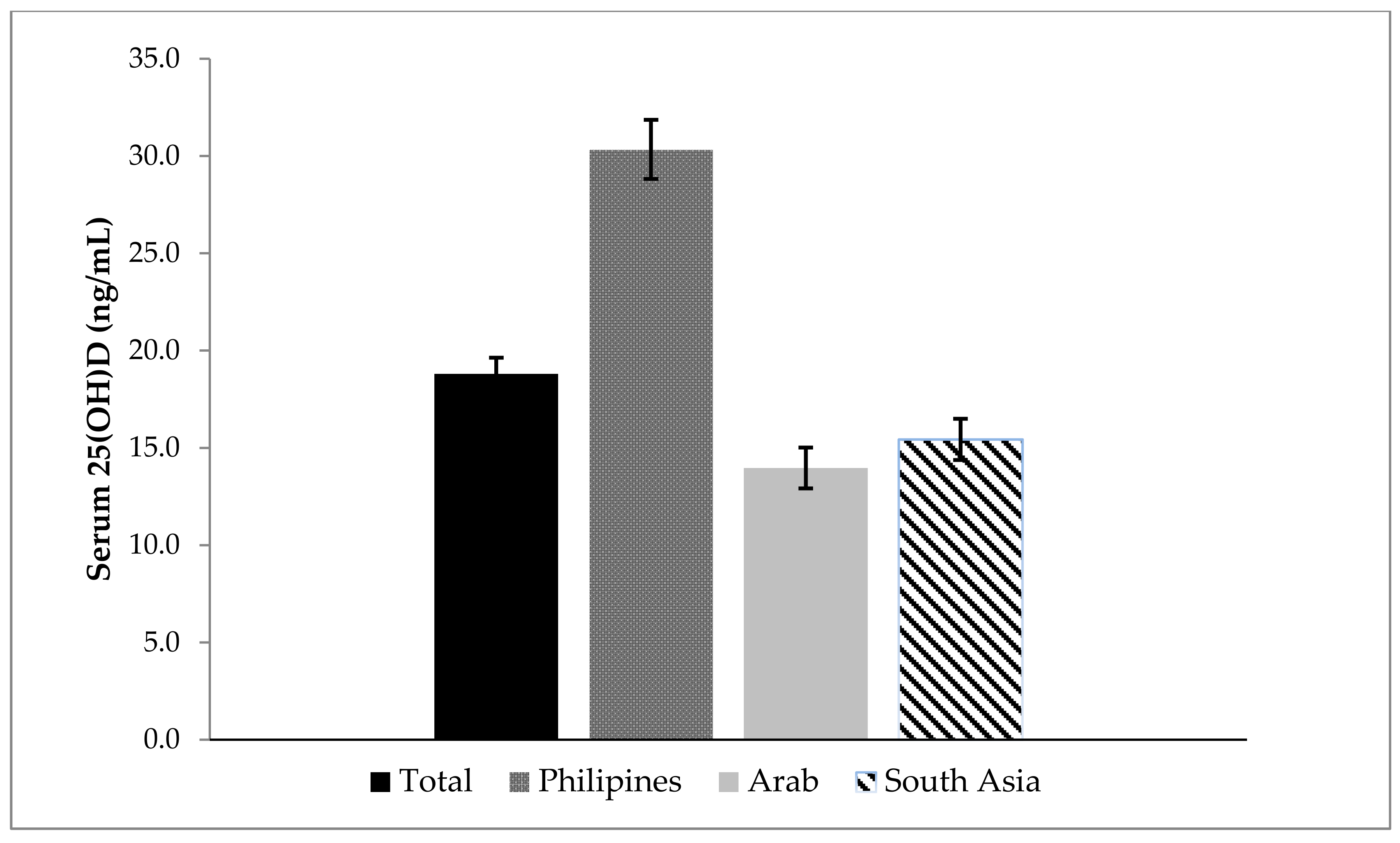
| Nationality | |||||||
| Filipinas | 57 | 30 | (12) | <0.001 | 15.8 | (8.3–27.8) | <0.001 |
| Arab | 90 | 14 | (10) | 86.7 | (77.8–92.3) | ||
| South Asian | 66 | 15 | (9) | 83.3 | (72.2–90.6) | ||
| Education of the participant | |||||||
| No formal schooling | 18 | 17 | (15) | 0.02 | 77.8 | (52.6–91.7) | <0.001 |
| Up to secondary | 91 | 22 | (13) | 49.4 | (39.2–59.7) | ||
| College or higher | 101 | 17 | (10) | 79.2 | (70.1–86.1) | ||
| Marital status | |||||||
| Unmarried | 69 | 21 | (13) | 0.26 | 56.5 | (44.5–67.58 | 0.06 |
| Married | 129 | 18 | (11) | 72.9 | (64.5–79.8) | ||
| Divorced, or widowed | 10 | 19 | (12) | 60.0 | (28.2–85.1) | ||
| Occupation | |||||||
| Housemaid | 64 | 29 | (12) | <0.001 | 21.9 | (13.3–33.8) | <0.001 |
| Housewife | 71 | 14 | (9) | 88.7 | (78.9–94.3) | ||
| Driver | 8 | 12 | (7) | 87.5 | (31.9–98.1) | ||
| Administrator, supervisor | 9 | 14 | (5) | 77.8 | (39.6–94.9) | ||
| Teacher | 21 | 15 | (10) | 80.9 | (58.0–92.9) | ||
| Health care worker | 18 | 18 | (8) | 77.8 | (52.6–91.7) | ||
| Other | 22 | 14 | (13) | 90.9 | (69.1–97.8) | ||
| Monthly income, Dirham (AED) | |||||||
| (US dollar = 3.7 AED) | |||||||
| Lowest (801.2) | 42 | 29 | 12 | <0.001 | 23.8 | (13.1–39.3) | <0.001 |
| Middle (1386.3) | 19 | 24 | 13 | 36.8 | (18.1–60.6) | ||
| Highest (8397.5) | 40 | 17 | 13 | 80.0 | (64.4–89.8) | ||
| Residence, n (%) | |||||||
| Urban | 84 | 19 | 13 | 0.74 | 65.5 | (54.6–74.9) | 0.57 |
| Rural | 114 | 19 | 12 | 69.3 | (60.1–77.1) | ||
| Duration of residence in UAE | |||||||
| <1 year | 62 | 22 | 14 | 0.005 | 56.4 | (43.8–68.2) | <0.001 |
| 1 to 5 years | 72 | 18 | 11 | 65.3 | (53.5–75.4) | ||
| ≥5 years | 49 | 14 | 14 | 91.8 | (79.69–96.9) | ||
| Physical activity (mod/vigorous.) | |||||||
| Yes | 52 | 25 | 13 | <0.001 | 42.3 | (29.5–56.2) | <0.001 |
| No | 161 | 17 | 11 | 75.5 | (67.2–80.7) | ||
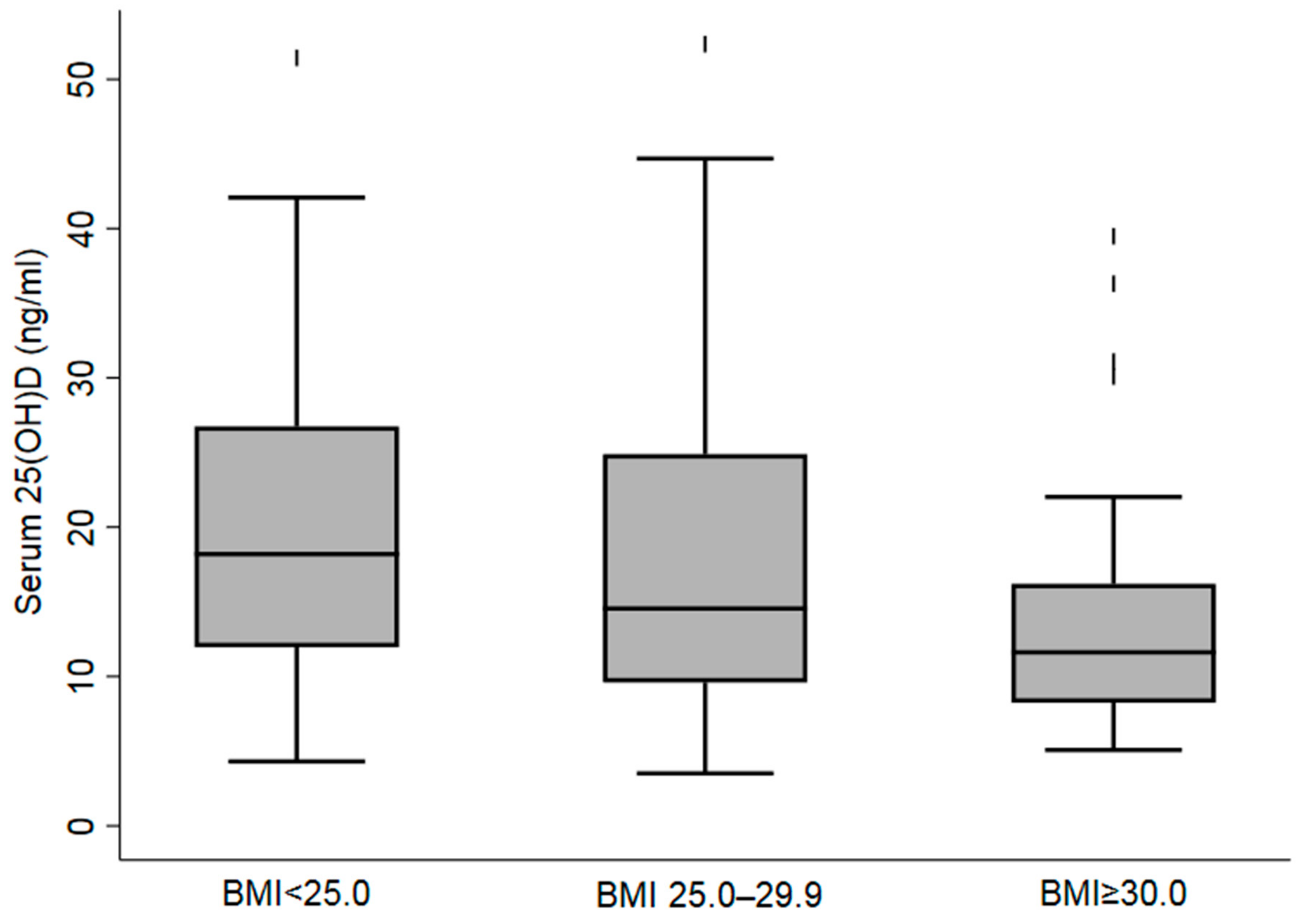
| Body mass index categories | 0.002 | ||||||
| <25.0 | 94 | 21 | 13 | 57.4 | (47.62–67.1) | 0.007 | |
| 25–30 | 74 | 19 | 12 | 67.6 | (55.9–77.3) | ||
| ≥30.0 | 45 | 14 | 8 | 84.4 | (70.5–92.4) | ||
| Cigarette smoking, currently | |||||||
| No | 199 | 19 | 12 | 0.99 | 65.3 | (17.1–20.5) | 0.12 |
| Yes | 14 | 19 | 16 | 85.7 | (9.5–28.0) | ||
| Alcohol use | |||||||
| No | 197 | 18 | 12 | <0.001 | 71.1 | (64.3–77.0) | <0.001 |
| Yes | 16 | 32 | 13 | 12.5 | (2.9–39.9) | ||
| Hemoglobin A1c level | |||||||
| <5.7% | 151 | 20 | 13 | 0.29 | 62.2 | (54.2–69.7) | 0.11 |
| 5.7–6.4% | 38 | 16 | 8 | 79.9 | (62.8–89.2) | ||
| ≥6.5% | 23 | 19 | 13 | 73.9 | (52.1.3–88.1) | ||
| Blood pressure, mm Hg | |||||||
| <140/90 | 139 | 18 | 13 | 0.45 | 70.5 | (62.3–77.5) | 0.10 |
| ≥140/90 or on hypertension medication | 74 | 20 | 11 | 59.5 | (47.8–70.1) | ||
| Determinants | Adjusted | ||
|---|---|---|---|
| OR | 95% CI | p | |
| Age in years | 0.97 | (0.92–1.01) | 0.18 |
| Nationality | |||
| Filipinas | 0.06 | (0.01–0.42) | 0.004 |
| Arab | Reference | ||
| South Asian | 0.79 | (0.32–1.98) | 0.62 |
| Education | |||
| No formal education | Reference | ||
| Up to secondary | 0.24 | (0.05–1.04) | 0.06 |
| College or higher | 0.66 | 0.15–2.89) | 0.59 |
| Duration of residence in UAE | |||
| ≤1 year | Reference | ||
| >1 to 5 years | 0.78 | (0.33–1.83) | 0.67 |
| >5 years | 4.65 | (1.31–16.53) | 0.02 |
| Body mass index categories | |||
| BMI | |||
| ≤24.99 | Reference | ||
| 25–29.99 | 2.21 | (0.92–5.30) | 0.08 |
| ≥30.0 | 3.56 | (1.04–12.20) | 0.04 |
| Low level of physical activity * | |||
| No | Reference | ||
| Yes | 4.59 | (1.98–10.63) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anouti, F.A.; Ahmed, L.A.; Riaz, A.; Grant, W.B.; Shah, N.; Ali, R.; Alkaabi, J.; Shah, S.M. Vitamin D Deficiency and Its Associated Factors among Female Migrants in the United Arab Emirates. Nutrients 2022, 14, 1074. https://doi.org/10.3390/nu14051074
Anouti FA, Ahmed LA, Riaz A, Grant WB, Shah N, Ali R, Alkaabi J, Shah SM. Vitamin D Deficiency and Its Associated Factors among Female Migrants in the United Arab Emirates. Nutrients. 2022; 14(5):1074. https://doi.org/10.3390/nu14051074
Chicago/Turabian StyleAnouti, Fatme Al, Luai A. Ahmed, Azmat Riaz, William B. Grant, Nadir Shah, Raghib Ali, Juma Alkaabi, and Syed M. Shah. 2022. "Vitamin D Deficiency and Its Associated Factors among Female Migrants in the United Arab Emirates" Nutrients 14, no. 5: 1074. https://doi.org/10.3390/nu14051074
APA StyleAnouti, F. A., Ahmed, L. A., Riaz, A., Grant, W. B., Shah, N., Ali, R., Alkaabi, J., & Shah, S. M. (2022). Vitamin D Deficiency and Its Associated Factors among Female Migrants in the United Arab Emirates. Nutrients, 14(5), 1074. https://doi.org/10.3390/nu14051074








