A Study of United States Registered Dietitian Nutritionists during COVID-19: From Impact to Adaptation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Group
2.2. Ethical Approval
2.3. Measures
2.3.1. Demographic, Weight, Eating Patterns, Physical Activity, and Psychological Factors
2.3.2. Qualitative Questions
2.4. Data Coding and Analysis
3. Results
3.1. Demographic Characteristics
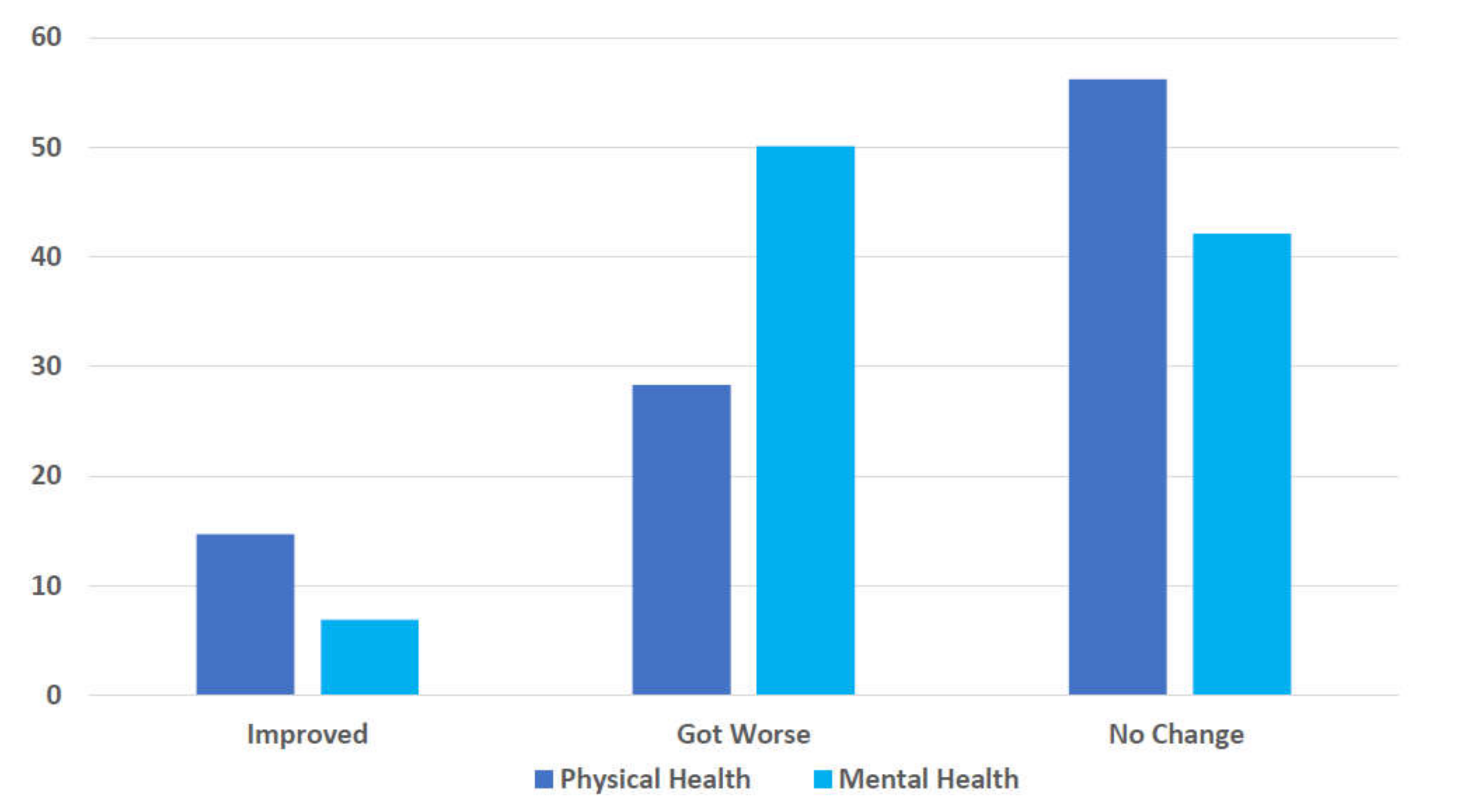
3.2. Health Changes
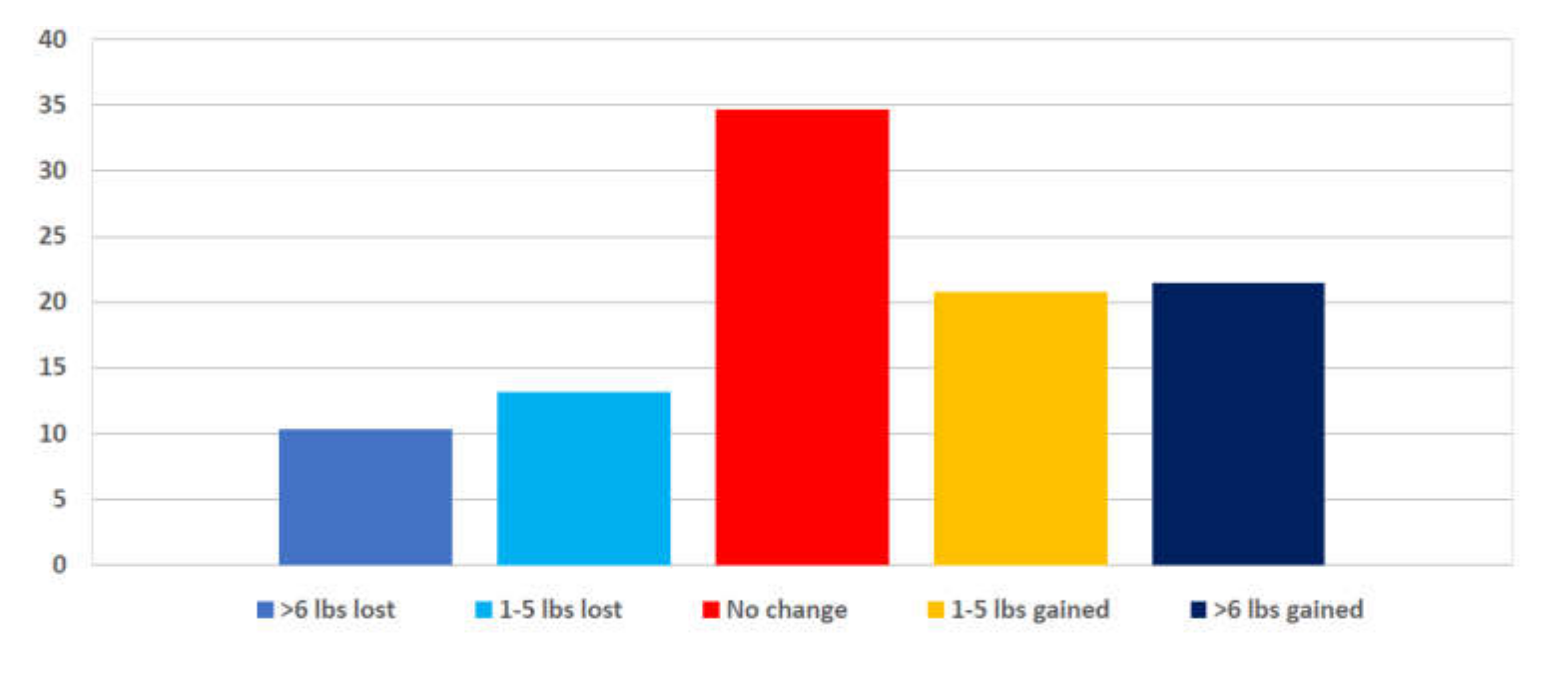
3.3. Weight Change
3.4. Changes in Eating Patterns
3.5. Physical Activity
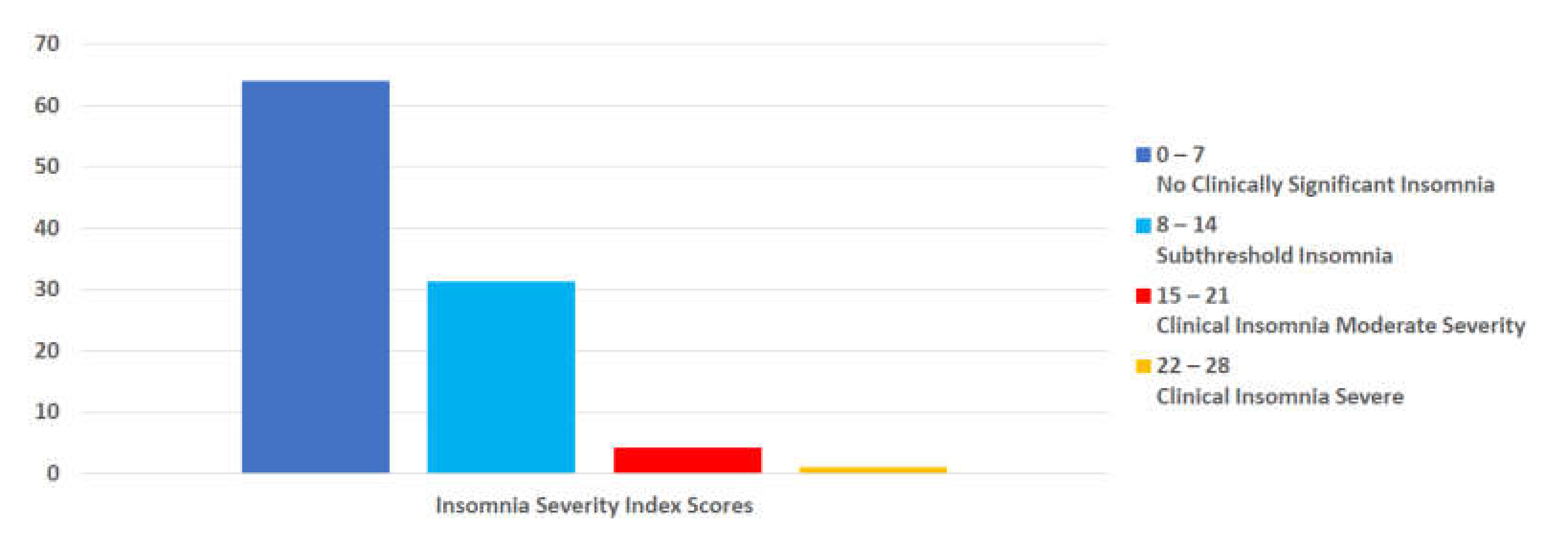
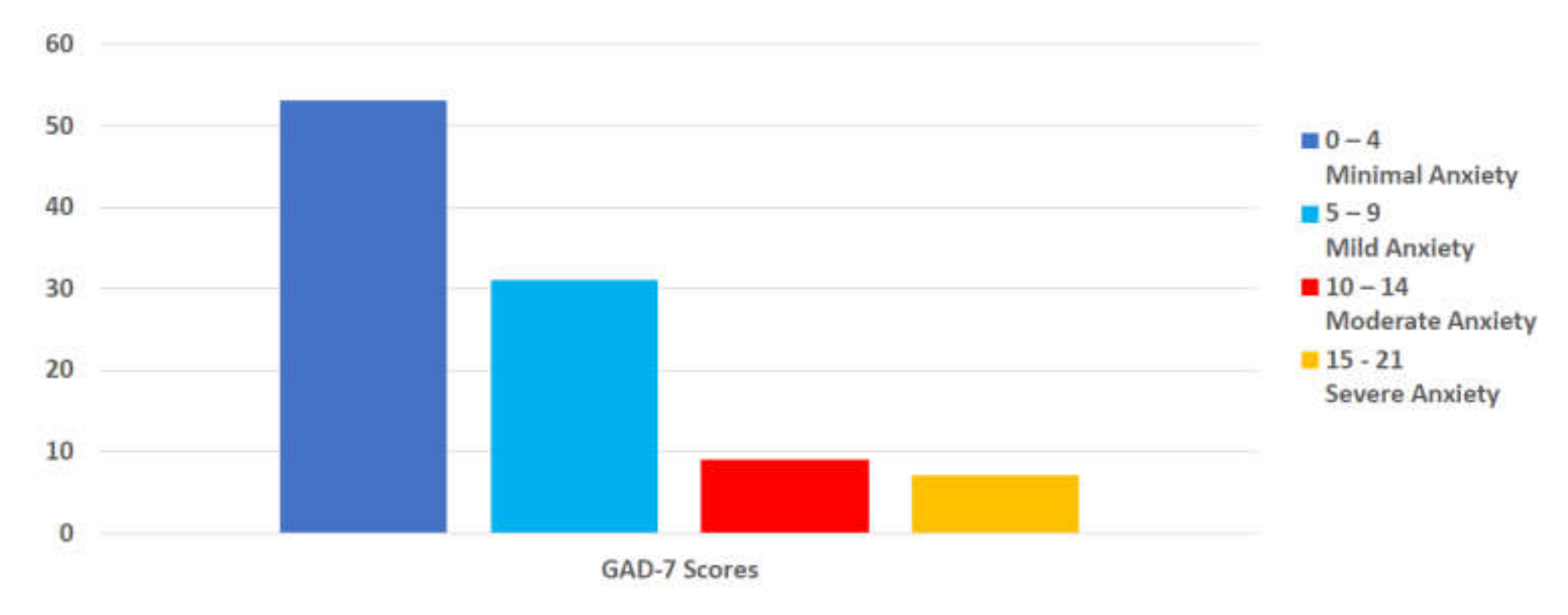
3.6. Psychological Factors
3.7. Family/Caretaking Responsibilities
3.8. Professional Practice
3.9. Qualitative Responses
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Greenberg, N. Mental health of health-care workers in the COVID-19 era. Nat. Rev. Nephrol. 2020, 16, 425–426. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed on 2 December 2021).
- Kazmierski, K.F.M.; Gillespie, M.L.; Kuo, S.; Zurita, T.; Felix, D.; Rao, U. Stress-Induced Eating Among Racial/Ethnic Groups in the United States: A Systematic Review. J. Racial Ethn. Health Disparities 2021, 8, 912–926. [Google Scholar] [CrossRef] [PubMed]
- Khaled, K.; Tsofliou, F.; Hundley, V.; Helmreich, R.; Almilaji, O. Perceived stress and diet quality in women of reproductive age: A systematic review and meta-analysis. Nutr. J. 2020, 19, 92. [Google Scholar] [CrossRef]
- Neill, E.; Meyer, D.; Toh, W.L.; Van Rheenen, T.E.; Phillipou, A.; Tan, E.J.; Rossell, S.L. Alcohol use in Australia during the early days of the COVID-19 pandemic: Initial results from the COLLATE project. Psychiatry Clin. Neurosci. 2020, 74, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Lessard, L.M.; Larson, N.; Eisenberg, M.E.; Neumark-Stzainer, D. Weight Stigma as a Predictor of Distress and Maladaptive Eating Behaviors During COVID-19: Longitudinal Findings from the EAT Study. Ann. Behav. Med. 2020, 54, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, V.; Nixon, M.; Ma, D.; Haines, J.; on behalf of the Guelph Family Health Study. The Impact of COVID-19 on Health Behavior, Stress, Financial and Food Security among Middle to High Income Canadian Families with Young Children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef] [PubMed]
- Academy of Nutrition and Dietetics. Coronavirus (COVID-19) Professional Resource Hub. Available online: https://www.eatrightpro.org/coronavirus-resources (accessed on 4 November 2021).
- De Costa Matos, R.A.; de Cássia Coelho de Almeida Akutsu, R.; Zandonadi, R.P.; Rocha, A.; Botelho, R.B.A. Wellbeing at Work before and during the SARS-COV-2 Pandemic: A Brazilian Nationwide Study among Dietitians. Int. J. Environ. Res. Public Health 2020, 17, 5541. [Google Scholar] [CrossRef] [PubMed]
- Heitman, K. COVID-19 Stories and Experiences; Food & Nutrition Magazine. Available online: https://foodandnutrition.org/covid-19/covid-19-stories-and-experiences (accessed on 20 April 2020).
- Rozga, M.; Handu, D.; Kelley, K.; Jimenez, E.Y.; Martin, H.; Schofield, M.; Steiber, A. Telehealth During the COVID-19 Pandemic: A Cross-Sectional Survey of Registered Dietitian Nutritionists. J. Acad. Nutr. Diet. 2021, 121, 2524–2535. [Google Scholar] [CrossRef] [PubMed]
- Epel, E.; Lapidus, R.; McEwen, B.; Brownell, K. Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology 2001, 26, 37–49. [Google Scholar] [CrossRef]
- O’Connor, D.B.; Jones, F.; Conner, M.; McMillan, B.; Ferguson, E. Effects of daily hassles and eating style on eating behavior. Health Psychol. 2008, 27, S20–S31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donnelly, R.; Keller, H. Challenges Providing Nutrition Care during the COVID-19 Pandemic: Canadian Dietitian Perspectives. J. Nutr. Health Aging 2021, 25, 710–711. [Google Scholar] [CrossRef] [PubMed]
- Naja, F.; Radwan, H.; Ismail, L.C.; Hashim, M.; Rida, W.H.; Abu Qiyas, S.; Bou-Karroum, K.; Alameddine, M. Practices and resilience of dieticians during the COVID-19 pandemic: A national survey in the United Arab Emirates. Hum. Resour. Health 2021, 19, 141. [Google Scholar] [CrossRef] [PubMed]
- Qualtrics. Computer Software; Qualtrics: Seattle, WA, USA, 2021. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bastien, C.H.; Vallieres, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Statistical Package for the Social Sciences—SPSS (Version 24); SPSS Inc.: Chicago, IL, USA, 2020.
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and Standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the General Population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef] [Green Version]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef] [PubMed]
- ATLAS.ti, version 9; ATLAS.ti Scientific Software Development: Berlin, Germany, 2021.
- Handu, D.; Moloney, L.; Rozga, M.; Cheng, F.W. Malnutrition Care During the COVID-19 Pandemic: Considerations for Registered Dietitian Nutritionists. J. Acad. Nutr. Diet. 2021, 121, 979–987. [Google Scholar] [CrossRef]
- Chew, H.; Lopez, V. Global Impact of COVID-19 on Weight and Weight-Related Behaviors in the Adult Population: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 1876. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association. STRESS IN AMERICA™ One Year Later, A New Wave of Pandemic Health Concerns. Available online: https://www.apa.org/news/press/releases/stress/2021/one-year-pandemic-stress (accessed on 15 December 2021).
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef] [PubMed]
- Dunton, G.F.; Wang, S.D.; Do, B.; Courtney, J. Early effects of the COVID-19 pandemic on physical activity locations and behaviors in adults living in the United States. Prev. Med. Rep. 2020, 20, 101241. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Lee, S.H.; Yaroch, A.L.; Blanck, H.M. Reported Changes in Eating Habits Related to Less Healthy Foods and Beverages during the COVID-19 Pandemic among US Adults. Nutrients 2022, 14, 526. [Google Scholar] [CrossRef]
- Lombardo, M.; Guseva, E.; Perrone, M.A.; Müller, A.; Rizzo, G.; Storz, M.A. Changes in Eating Habits and Physical Activity after COVID-19 Pandemic Lockdowns in Italy. Nutrients 2021, 13, 4522. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Health Care Access, Telemedicine, and Mental Health. Available online: https://www.cdc.gov/nchs/covid19/health-care-access-and-mental-health.htm (accessed on 15 January 2022).
- Alimoradi, Z.; Broström, A.; Tsang, H.W.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Lin, C.-Y.; Pakpour, A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine 2021, 36, 100916. [Google Scholar] [CrossRef] [PubMed]
- Stewart, N.H.; Koza, A.; Dhaon, S.; Shoushtari, C.; Martinez, M.; Arora, V.M. Sleep Disturbances in Frontline Health Care Workers During the COVID-19 Pandemic: Social Media Survey Study. J. Med Internet Res. 2021, 23, e27331. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.B.; Neufeld, E.V.; Dolezal, B.A.; Martin, J.L. Sleep deprivation and obesity in adults: A brief narrative review. BMJ Open Sport Exerc. Med. 2018, 4, e000392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Commission on Dietetic Registration. Registry Statistics. Available online: https://www.cdrnet.org/registry-statistics (accessed on 5 January 2021).
- Rogers, D. Report on the Academy/Commission on Dietetic Registration 2020 Needs Satisfaction Survey. J. Acad. Nutr. Diet. 2021, 121, 134–138. [Google Scholar] [CrossRef]
| Variables | Total (n = 477) |
|---|---|
| Gender | n(%) |
| Male, n (%) | 16 (3.4) |
| Female, n (%) | 457 (95.8) |
| Age, mean (SD), years old | 43.96 (±15.04) |
| Race | n(%) |
| Black/African American | 8 (1.7) |
| Latinx/Hispanic | 6 (1.3) |
| White/Non-Hispanic | 443 (92.9) |
| Asian/Pacific Islander | 9 (19) |
| Multi-racial/Mixed ethnicities | 5 (1.0) |
| Other | 2 (0.4) |
| Body Mass Index (n = 448) | |
| BMI, mean (S.D.) | 24.77 (±4.99) |
| Underweight | 11 (2.5) |
| Normal weight | 271 (61.5) |
| Overweight | 98 (22.2) |
| Obesity | 61 (13.8) |
| Highest education level | n(%) |
| Some college or trade school | 1 (0.2) |
| Associates or Technical Degree | 2 (0.4) |
| Bachelor’s Degree | 181 (37.9) |
| Master’s Degree | 264 (55.3) |
| Doctoral Degree (e.g., J.D., MD, PhD) | 25 (5.2) |
| Primary Practice Setting | n(%) |
| Academic Institution | 39 (8.2) |
| Community | 26 (5.5) |
| Foodservice | 13 (2.7) |
| Hospital | 97 (20.3) |
| Not Currently Working | 41 (8.6) |
| Long-Term Care Facility | 74 (15.5) |
| Out-Patient Clinic | 83 (17.4) |
| Private Practice (Inside your home) | 34 (7.1) |
| Private Practice (Outside your home) | 24 (5) |
| Retail | 3 (0.6) |
| Other | 39 (8.2) |
| Employment Status | n(%) |
| Full-Time Student | 3 (0.6) |
| Part-time | 98 (20.5) |
| Full-time (>35 h per week) | 310 (65.0) |
| Retired | 25 (5.2) |
| Unemployed Due to COVID | 8 (1.7) |
| Unemployed not Related to COVID | 10 (2.1) |
| Not Working Due to Disability | 2 (0.4) |
| Other | 17 (3.6) |
| Number of Years in Practice, mean (SD), y | 17.39 (±14.52) |
| Typical Workday | n(%) |
| Flexible hours (make your own schedule) | 83 (17.4) |
| Irregular hours (i.e., changes day to day or week to week) | 17 (3.6) |
| Per diem (as needed) hours | 16 (3.4) |
| Weekday hours | 313 (65.6) |
| I am not currently working | 44 (9.2) |
| Less/Decrease | No Change | More/Increase | |
|---|---|---|---|
| Home meal preparation frequency | 38 (8.0) | 171 (35.8) | 256 (53.7) |
| Snacking/grazing | 35 (7.3) | 218 (45.7) | 212 (44.4) |
| Alcoholic beverage intake | 61 (12.8) | 261 (54.7) | 143 (30.0) |
| Caffeinated beverage intake | 30 (6.3) | 322 (67.5) | 113 (23.7) |
| Fast food or take out consumption | 128 (26.8) | 238 (49.9) | 99 (20.8) |
| Appetite | 54 (11.3) | 314 (65.8) | 97 (20.3) |
| Daily vegetable intake | 45 (9.4) | 334 (70.0) | 86 (18.0) |
| Food portion sizes | 49 (10.3) | 349 (73.2) | 67 (14.0) |
| Daily fruit intake | 38 (8.0) | 362 (75.9) | 65 (13.6) |
| Minutes/Hours/Day | n (%) |
|---|---|
| <15 min | 91 (19.1) |
| 15–30 min | 129 (27.0) |
| 30–45 min | 139 (29.1) |
| 45 min–1 h | 82 (17.2) |
| >1 h | 30 (6.3) |
| Theme | Response Frequency | Definition | Illustrative Quotes |
|---|---|---|---|
| Reduced physical activity | n = 104, 40.8% | Decreased frequency, intensity and/or duration of exercising | “Due to limited home space and quarantine, I have given up continuing with favorite physical activities like yoga or group fitness classes, which I think has impacted my mental health and ability to handle small daily stressors.” “Not being able to go out to my exercise class got me out of habit of exercising and I watch what I eat less if I am NOT exercising. I am also more sedentary working remotely—I would move around more in the office.” |
| Mental health | n = 65, 25.5% | Increase in stress, anxiety, depression, emotional eating, boredom leading to an increase or decrease in food intake | “I have increased my work hours from ~50 to 60–65 h a week. My stress level has increased from an already stressful position, and I believe that this stress has contributed to me not truly caring or able to make sound decisions in healthful behaviors. I feel like I have been in “fight” mode for a year and truly not able to center enough to use my training on a personal level.” “In the very beginning of COVID (March-April (2019) I was terrified of COVID. This caused me to have severe panic attacks and severe anxiety. I was afraid to go to work. My mental health took a huge toll. I was doing my best to maintain physical activity and eating healthy. I lost a few pounds in the beginning due to my anxiety over the pandemic. Come June (2019), I adapted to the “new way of life” and have been fine ever since.” “The stress of the pandemic has been mentally debilitating. Working from home full time, virtual kindergarten and keeping up a household have destroyed my mental stability. Using tools that I know can help me (and my family feel better has been what keeps us going). Cooking ourselves, eating healthy food, exercising regularly and for myself, really not drinking alcohol have been a help but honestly I’m hanging on by a thread.” |
| Unfavorable eating habits | n = 49, 19.2% | Unintentional, detrimental shifts or modifications in dietary patterns | “Food eating habits changed slightly for me in respect to the quality of food. I didn’t necessarily eat more but indulged in “higher energy foods”! For example, using more butter, more chocolate. For my family, I did purchase more processed foods than usual as they seemed to want to “graze” more! For example, ice cream, potato chips. Typically, these were treats that were brought home occasionally.” “COVID-19 has made me lazy. I don’t want to cook anymore, and I look for quick cooking instead (pizza, rice, burgers, frozen foods). I also snack way more often than I ever did before. I used to never buy snack foods and now I have a favorite brand of chips!!! That has never happened before.” |
| Improved eating habits | n = 45, 17.6% | Intentional or unintentional resetting or correction of dietary patterns | “Made a conscious effort to eat b/l/d and snacks on a schedule that reflected our pre-pandemic schedule; also made a pact not to bake desserts/breads. Focused on making fun meals, and not increasing desserts/snack foods.—instead of shopping 3x/wk at different stores, shopped every 10 days at 1 store, decreased variety of fresh f/v and variety of specialty items that I would normally get at the Asian, Mid East, Indian stores.” |
| Subtheme: Intentional weight/diet changes | n = 19, 7.5% | Actively focusing on improving diet to promote healthy weight | “Initially at the start of quarantine—I took the opportunity to do a pantry/fridge/freezer clean out to limit food waste and having to leave the house out of fear. As restrictions eased, cases went down, I became a smarter grocery shopper—from planning, the grocery list, to shopping, more efficient and purposeful.” |
| Increased physical activity | n = 45, 17.6% | Greater frequency, intensity and/or duration of exercising | “Due to gyms being closed, I began yoga at the start of quarantine. A year later, I am still loving the practice. It helps me relax and destress. We created a home gym in the basement as well.” “More leisure time spent being physically active outside.” |
| Job/family/schedule disruptions | n = 42, 16.5% | Changes from usual work or home/family routines significant enough to impact diet, physical activity, or weight | “My job becoming virtual has led to me moving around less... Overall meal balance decreased with an increase in ordering takeout because I was tired often after work and didn’t want to cook. Fatigued by the end of the day often due to looking at the computer screen for 8 h when it used to be only a few hours before with more in person interaction. This has made it difficult to maintain a healthy balance with exercise.” “My main problem with my family’s food intake is the kids desire for constant snacks being home all day or with boredom they’d think they were hungry. It was also more difficult to get grocery shopping scheduled as I typically did this while they were in school. They are in virtual school, and I did not want to take 2 kids out to the grocery store. Some home delivery services were too expensive. I consider myself privileged to have more flexibility and resources and felt bad imagining people in more difficult circumstances.” “At the beginning of the pandemic dietitians in hospital were left to figure things out for themselves to create safe working habits and spaces with slow guidance from hospital and zero from ADA. Worry early on about bringing COVID home to vulnerable family members added stress/poor sleeping and eating habits.” |
| Health/medical conditions | n = 34, 13.3% | Pregnancy or acute/chronic conditions | “At first I was affected as just as COVID was hitting, I had ear surgery and was not allowed to even walk on treadmill for 8 weeks. I gained weight from stress eating. Then I injured my right arm, and it took about 4–6 weeks to heal.” “The biggest challenge for exercise is having a baby/ toddler. I don’t do enough dedicated exercise, but I am active with a toddler.” |
| Change in alcohol use | n = 18, 7% | Increased or decreased consumption of beer, wine, hard liquor | “I was always starving by dinner so I would eat too much. Combine that with too much wine to cope with the stress- and it’s no wonder I gained so much weight. I could almost watch the weight gain … and I felt completely powerless to stop it.” “COVID affected my eating and drinking habits. I was “comfort eating” at times and definitely drinking more wine. There was nothing else to do! I gained 5–10 lbs.” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliver, T.L.; Shenkman, R.; Mensinger, J.L.; Moore, C.; Diewald, L.K. A Study of United States Registered Dietitian Nutritionists during COVID-19: From Impact to Adaptation. Nutrients 2022, 14, 907. https://doi.org/10.3390/nu14040907
Oliver TL, Shenkman R, Mensinger JL, Moore C, Diewald LK. A Study of United States Registered Dietitian Nutritionists during COVID-19: From Impact to Adaptation. Nutrients. 2022; 14(4):907. https://doi.org/10.3390/nu14040907
Chicago/Turabian StyleOliver, Tracy L., Rebecca Shenkman, Janell L. Mensinger, Caroline Moore, and Lisa K. Diewald. 2022. "A Study of United States Registered Dietitian Nutritionists during COVID-19: From Impact to Adaptation" Nutrients 14, no. 4: 907. https://doi.org/10.3390/nu14040907
APA StyleOliver, T. L., Shenkman, R., Mensinger, J. L., Moore, C., & Diewald, L. K. (2022). A Study of United States Registered Dietitian Nutritionists during COVID-19: From Impact to Adaptation. Nutrients, 14(4), 907. https://doi.org/10.3390/nu14040907







