Be Healthy in Pregnancy (BHIP): A Randomized Controlled Trial of Nutrition and Exercise Intervention from Early Pregnancy to Achieve Recommended Gestational Weight Gain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Data Collection, and Ethical Aspects
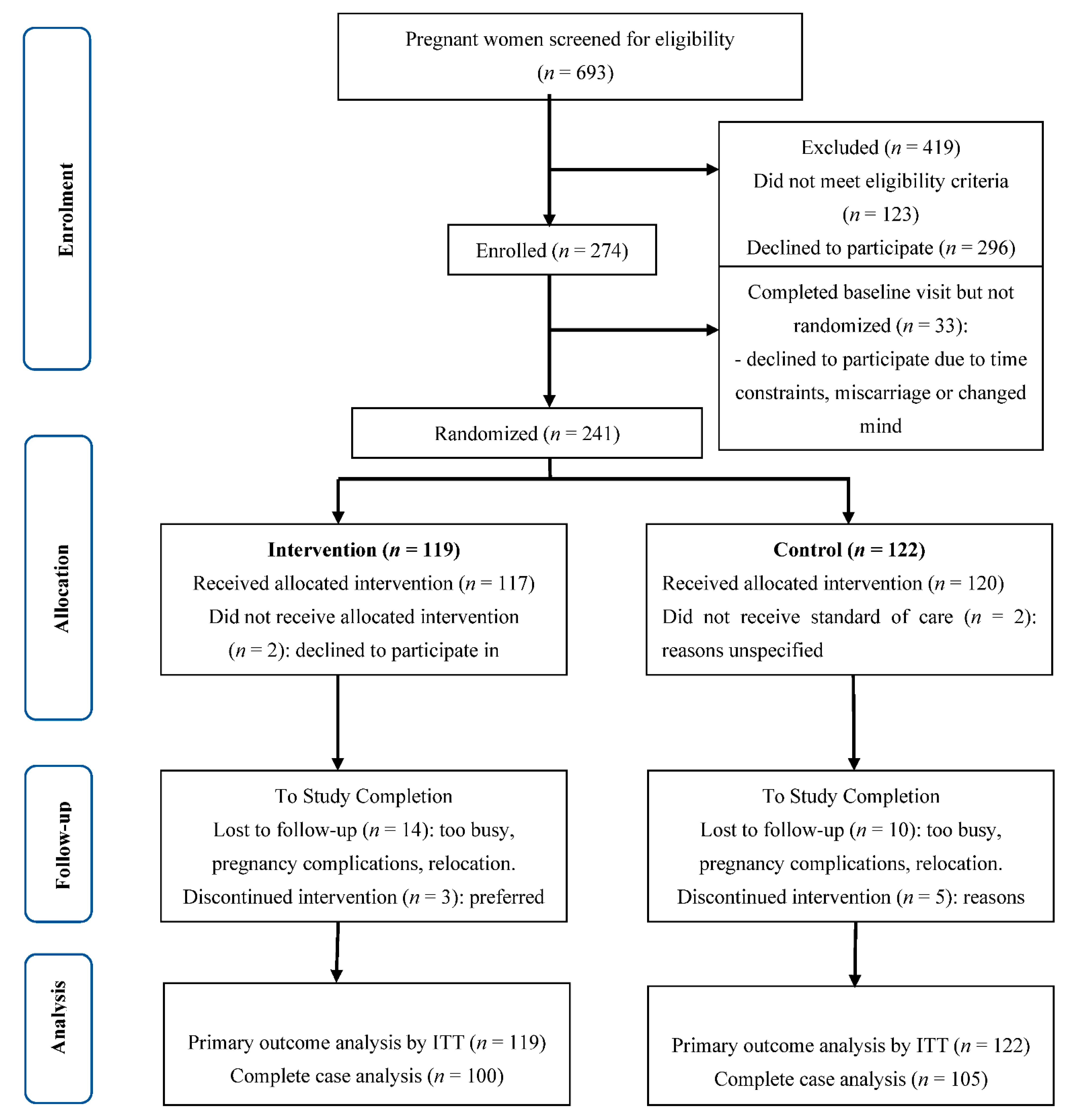
2.2. Recruitment, Randomization, and Followup
2.2.1. Intervention
2.2.2. Usual Care
2.3. Outcomes and Measurements
2.4. Sample Size and Statistical Analysis
3. Results
3.1. Participant Recruitment and Characteristics
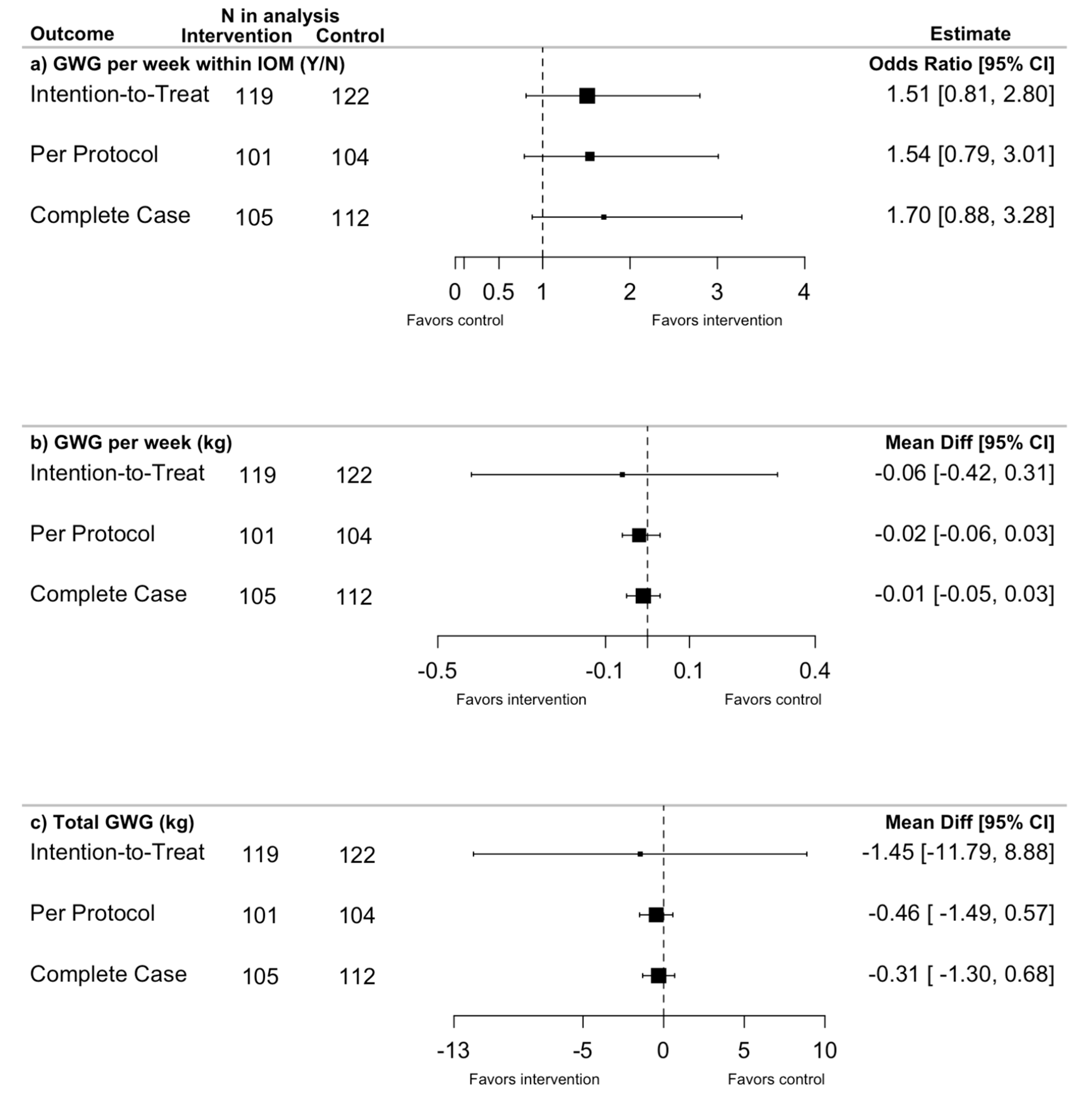
3.2. Gestational Weight Gain (Primary Outcome)
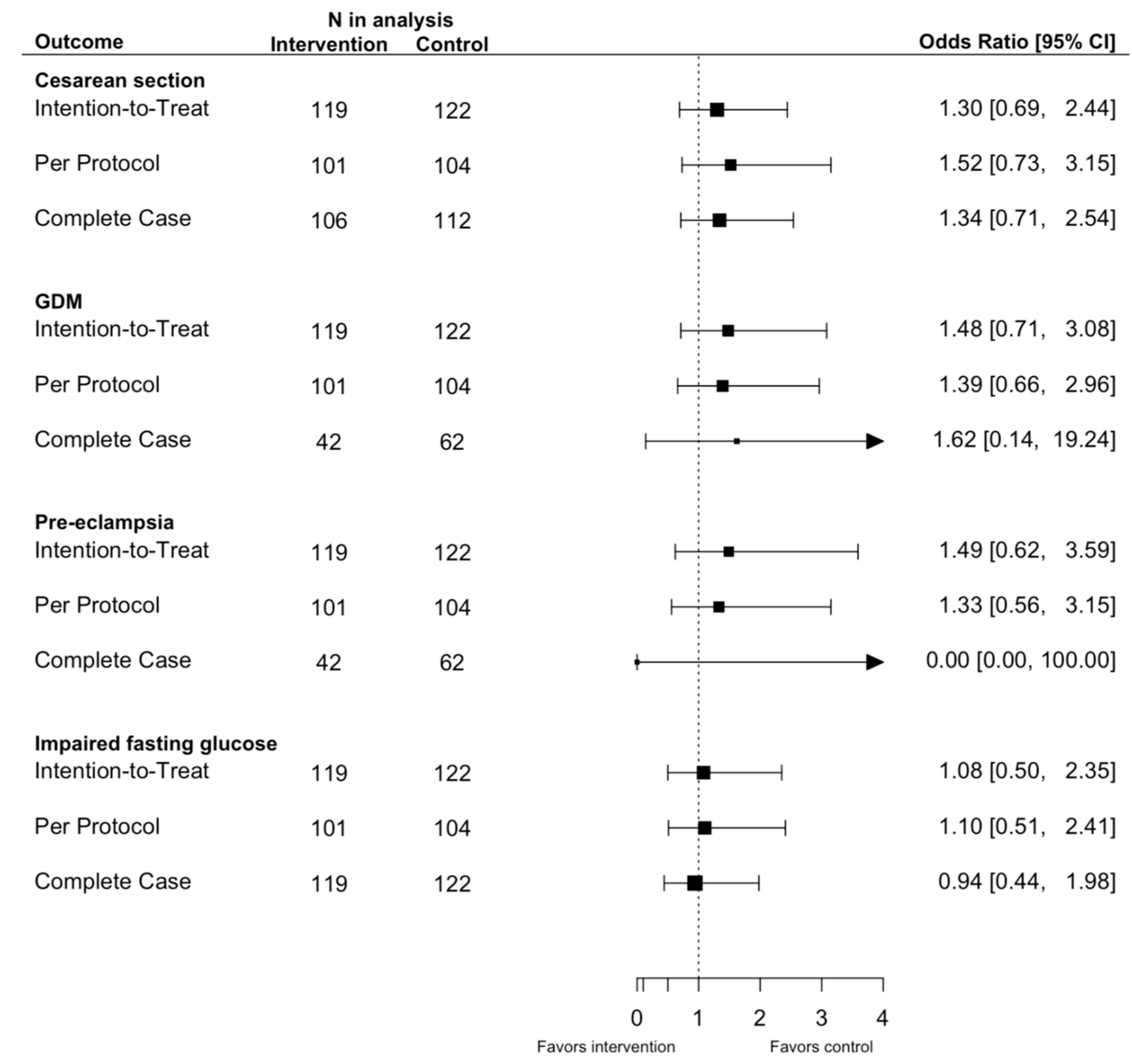
3.3. Pre-Specified Pregnancy and Birth Outcomes
3.4. Pre-Specified Maternal Health Outcomes
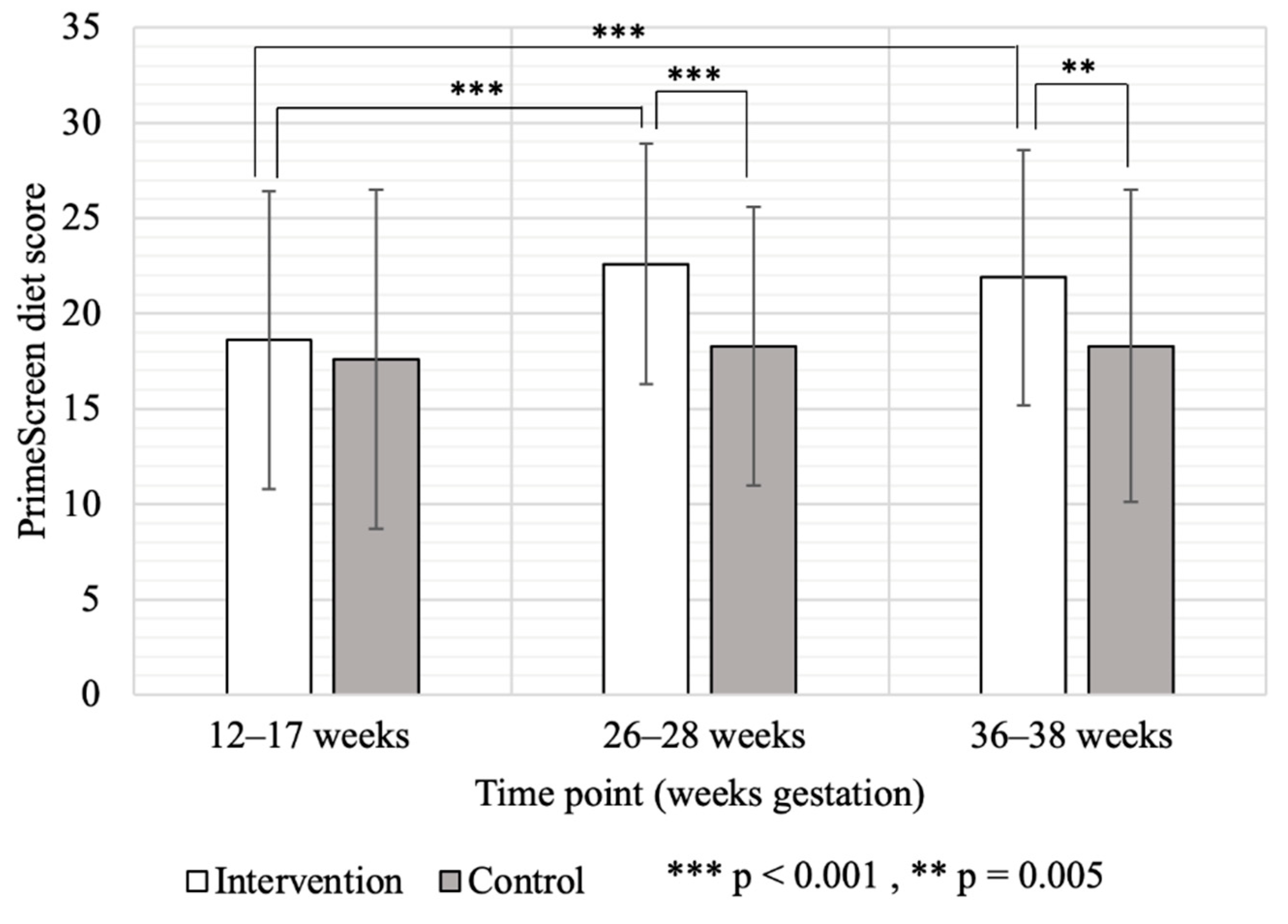
3.5. Dietary and Physical Activity Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Institute of Medicine. IOM—Weight Gain during Pregnancy; National Academies Press: Washington, DC, USA, 2009; Available online: http://www.nap.edu/catalog/12584 (accessed on 12 June 2021).
- Murray-Davis, B.; Berger, H.; Melamed, N.; Hasan, H.; Mawjee, K.; Syed, M.; Ray, J.G.; Geary, M.; Barrett, J.; McDonald, S.D. Weight gain during pregnancy: Does the antenatal care provider make a difference? A retrospective cohort study. CMAJ Open 2019, 7, E283–E293. [Google Scholar] [CrossRef] [Green Version]
- Siega-Riz, A.M.; Bodnar, L.M.; Stotland, N.E.; Stang, J. The Current Understanding of Gestational Weight Gain among Women with Obesity and the Need for Future Research. NAM Perspect. 2020, 2020, E283–E293. [Google Scholar] [CrossRef] [PubMed]
- Dzakpasu, S.; Fahey, J.; Kirby, R.S.; Tough, S.C.; Chalmers, B.; Heaman, M.I.; Bartholomew, S.; Biringer, A.; Darling, E.K.; Lee, L.S.; et al. Contribution of prepregnancy body mass index and gestational weight gain to caesarean birth in Canada. BMC Pregnancy Childbirth 2014, 14, 106. [Google Scholar] [CrossRef] [Green Version]
- Durst, J.K.; Sutton, A.L.M.; Cliver, S.P.; Tita, A.T.; Biggio, J.R. Impact of Gestational Weight Gain on Perinatal Outcomes in Obese Women. Am. J. Perinatol. 2016, 33, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Shen, S.; Sun, L.; Yang, H.; Jin, B.; Cao, X. Metabolic Syndrome Risk after Gestational Diabetes: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e87863. [Google Scholar] [CrossRef] [Green Version]
- Bellamy, L.; Casas, J.-P.; Hingorani, A.D.; Williams, D. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet 2009, 373, 1773–1779. [Google Scholar] [CrossRef]
- Garovic, V.D.; August, P. Preeclampsia and the future risk of hypertension: The pregnant evidence. Curr. Hypertens. Rep. 2013, 15, 114–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siega-Riz, A.M.; Viswanathan, M.; Moos, M.-K.; Deierlein, A.; Mumford, S.; Knaack, J.; Thieda, P.; Lux, L.J.; Lohr, K.N. A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: Birthweight, fetal growth, and postpartum weight retention. Am. J. Obstet. Gynecol. 2009, 201, 339.e1–339.e14. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, J.G.; Sandboge, S.; Salonen, M.K.; Kajantie, E.; Osmond, C. Long-term consequences of maternal overweight in pregnancy on offspring later health: Findings from the Helsinki Birth Cohort Study. Ann. Med. 2014, 46, 434–438. [Google Scholar] [CrossRef]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L.; Kim, Y.J.; et al. Association of Gestational Weight Gain with Maternal and Infant Outcomes. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef]
- Goldstein, R.F.; Abell, S.K.; Ransinha, S.; Misso, M.L.; Boyule, J.A.; Harrison, C.L.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; et al. Gestational weight gain across continents and ethnicity: Systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018, 16, 153. [Google Scholar] [CrossRef] [PubMed]
- Perreault, M.; Atkinson, S.A.; Mottola, M.F.; Phillips, S.M.; Bracken, K.; Hutton, E.K.; Xie, F.; Meyre, D.; Morassut, R.E.; Prapavessis, H.; et al. Structured diet and exercise guidance in pregnancy to improve health in women and their offspring: Study protocol for the Be Healthy in Pregnancy (BHIP) randomized controlled trial. Trials 2018, 19, 691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gardner, B.; Wardle, J.; Poston, L.; Croker, H. Changing diet and physical activity to reduce gestational weight gain: A meta-analysis. Obes Rev. 2011, 12, e602-20. [Google Scholar] [CrossRef] [PubMed]
- Ronnberg, A.; Nilsson, K. Interventions during pregnancy to reduce excessive gestational weight gain: A systematic review assessing current clinical evidence using the Grading of Recommendations. Assessment. Developmenmt and Evaluation (GRADE) system. BJOG 2010, 117, 1327–1334. [Google Scholar] [CrossRef]
- Streuling, I.; Beyerlein, A.; Rosenfeld, E.; Hofmann, H.; Schulz, T.; von Kries, R. Physical activity and gestational weight gain: A meta-analysis of intervention trials. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 278–284. [Google Scholar] [CrossRef]
- Be Healthy in Pregnancy (BHIP) with Nutrition and Exercise. Available online: https://clinicaltrials.gov/ct2/show/NCT01689961 (accessed on 5 January 2022).
- Health Canada. Prenatal Nutrition Guidelines for Health Professionals: Gestational Weight Gain—Canada.ca. 2010. Available online: https://www.canada.ca/en/health-canada/services/canada-food-guide/resources/prenatal-nutrition/eating-well-being-active-towards-healthy-weight-gain-pregnancy-2010.html (accessed on 12 June 2021).
- Health Canada. Pregnancy Weight Gain Calculator—Nutrition and Healthy Eating—Health Canada. 2011. Available online: https://health.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/prenatal-nutrition/pregnancy-weight-gain-calculator.html (accessed on 12 June 2021).
- Health Canada. Eating Well with Canada’s Food Guide. 2007. Available online: https://www.hc-sc.gc.ca/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/print_eatwell_bienmang-eng.pdf (accessed on 12 June 2021).
- Josse, A.R.; Atkinson, S.A.; Tarnopolsky, M.A.; Phillips, S.M. Increased consumption of dairy foods and protein during diet and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenopausal women. J. Nutr. 2011, 141, 1626–1634. [Google Scholar] [CrossRef] [Green Version]
- Davies, G.A.L.; Wolfe, L.A.; Mottola, M.F.; MacKinnon, C. Joint SOGC/CSEP clinical practice guideline: Exercise in pregnancy and the postpartum period. Can. J. Appl. Physiol. 2003, 28, 330–341. [Google Scholar] [CrossRef]
- Walji, R.; Wahoush, O.; Atkinson, S.A. Feasibility and Acceptance of a Novel Nutrition and Exercise Intervention to Manage Excess Gestational Weight Gain: Focus group study in Ontario, Canada. Prim. Health Care 2013, 3, 2. [Google Scholar] [CrossRef]
- Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fibre, Fat, Fatty Acid, Cholesterol, Protein and Amino Acids (Macronutrients); National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Cox, J.L.; Holdenand, J.M.; Sagovsky, R. Detection of Postnatal Depression Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Rifas-Shiman, S.L.; Willett, W.C.; Lobb, R.; Kotch, J.; Dart, C.; Gillman, M.W. PrimeScreen, a brief dietary screening tool: Reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr. 2001, 4, 249–254. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Child Growth Standards. Dev. Med. Child. Neurol. 2009, 51, 1002. [Google Scholar] [CrossRef]
- Society of Obstetricians and Gynaecology of Canada. Society of Obstetricians and Gynaecologists of Canada—Gestational hypertension—Pregnancy Info. The Society of Obstetricians and Gynaecologists of Canada. Available online: https://www.pregnancyinfo.ca/your-pregnancy/special-consideration/diabetes-and-hypertension/ (accessed on 12 June 2021).
- Peaceman, A.M.; Clifton, R.G.; Phelan, S.; Gallagher, D.; Evans, M.; Redman, L.M.; Knowler, W.C.; Joshipura, K.; Haire-Joshu, D.; Yanovski, S.Z.; et al. Lifestyle Interventions Limit Gestational Weight Gain in Women with Overweight or Obesity: LIFE-Moms Prospective Meta-Analysis. Obesity 2018, 26, 1396–1404. [Google Scholar] [CrossRef]
- Frangakis, C.E.; Rubin, D.B. Addressing complications of intention-to-treat analysis in the combined presence of all-or-none treatment-noncompliance and subsequent missing outcomes. Biometrika 1999, 86, 365–379. [Google Scholar] [CrossRef]
- Ruifrok, A.E.; Van Poppel, M.N.M.; Van Wely, M.; Rogozińska, E.; Khan, K.S.; De Groot, C.J.M.; Thangaratinam, S.; Mol, B.W. Association between Weight Gain during Pregnancy and Pregnancy Outcomes after Dietary and Lifestyle Interventions: A Meta-Analysis. Am. J. Perinatol. 2014, 31, 353–364. [Google Scholar]
- Phelan, S.; Phipps, M.G.; Abrams, B.; Darroch, F.; Scaffner, A.; Wing, R.R. Randomized trial of a behavioral intervention to prevent excessive wieght gain: The Fit for Delievery Study. Am. J. Clin. Nurt. 2011, 93, 772–779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dodd, J.M.; Deussen, A.R.; Louise, J. A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial. Nutrients 2019, 11, 2911. [Google Scholar] [CrossRef] [Green Version]
- International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity-based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. BMJ 2017, 358, j3119. [Google Scholar]
- Peacock, L.; Seed, P.T.; Dalrymple, K.V.; White, S.L.; Poston, L.; Flynn, A.C. The UK Pregnancies Better Eating and Activity Trial (UPBEAT); Pregnancy Outcomes and Health Behaviours by Obesity Class. Int. J. Environ. Res. Public Health 2020, 17, 4712. [Google Scholar] [CrossRef]
- Poston, L.; Bell, R.; Croker, H.; Flynn, A.C.; Godfrey, K.M.; Goff, L.; Hayes, L.; Khazaezadeh, N.; Nelson, S.M.; Oteng-Ntim, E.; et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): A multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015, 3, 767–777. [Google Scholar] [CrossRef]
- da Silva, S.G.; Hallal, P.C.; Domingues, M.R.; Bertoldi, A.D.; da Silveira, M.F.; Bassani, D.; da Silva, I. A randomized controlled trial of exercise during pregnancy on maternal and neonatal outcomes: Results from the PAMELA study. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 175. [Google Scholar] [CrossRef] [Green Version]
- Farpour-Lambert, N.J.; Ells, L.J.; Martinez de Tejada, B.; Scott, C. Obesity and Weight Gain in Pregnancy and Postpartum: An Evidence Review of Lifestyle Interventions to Inform Maternal and Child Health Policies. Front. Endocrinol. 2018, 9, 546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oteng-Ntim, E.; Varma, R.; Croker, H.; Poston, L.; Doyle, P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: Systematic review and meta-analysis. BMC Med. 2012, 10, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckingham-Schutt, L.M.; Ellingson, L.D.; Vazou, S.; Campbell, C.G. The Behavioral Wellness in Pregnancy study: A randomized controlled trial of a multi-component intervention to promote appropriate weight gain. Am. J. Clin. Nutr. 2019, 109, 1071–1079. [Google Scholar] [CrossRef] [PubMed]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.; Davies, G.; Poitras, V.; Gray, C.; Jaramillo, A.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 Canadian Guideline for Physical Activity throughout Pregnancy. J. Obstet. Gynaecol. Can. 2018, 40, 1468–1483. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.M.; Shiroma, E.J.; Kamada, M.; Bassett, D.R.; Matthews, C.E.; Buring, J.E. Association of Step Volume and Intensity with All-Cause Mortality in Older Women. In: JAMA Internal Medicine. JAMA Intern. Med. 2019, 179, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- McKinley, M.C.; Allen-Walker, V.; McGirr, C.; Rooney, C.; Woodside, J.V. Weight loss after pregnancy: Challenges and opportunities. Nutr. Res Rev. 2018, 31, 225–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray-Davis, B.; Grenier, L.; Atkinson, S.A.; Mottola, M.F.; Wahoush, O.; Thabane, L.; Xie, F.; Vickers-Manzin, J.; Moore, C.; Hutton, E.K. Experiences regarding nutrition and exercise among women during early postpartum: A qualitative grounded theory study. BMC Pregnancy Childbirth 2019, 19, 368. [Google Scholar] [CrossRef] [Green Version]
- Connelly, M.; Brown, H.; Van Der Pligt, P.; Teychenne, M. Modifiable barriers to leisure-time physical activity during pregnancy: A qualitative study investigating first time mother’s views and experiences. BMC Pregnancy Childbirth 2015, 15, 100. [Google Scholar] [CrossRef] [Green Version]
- Coll, C.V.N.; Domingues, M.R.; Gonçalves, H.; Bertoldi, A.D. Perceived barriers to leisure-time physical activity during pregnancy: A literature review of quantitative and qualitative evidence. J. Sci. Med. Sport 2017, 20, 17–25. [Google Scholar] [CrossRef]
- Davenport, M.H.; Ruchat, S.M.; Sobierajski, F.; Poitras, V.J.; Gray, C.E.; Yoo, C.; Skow, R.J.; Jaramillo Garcia, A.; Barrowman, N.; Meah, V.L.; et al. The impact of prenatal exercise on maternal harms, labour and delivery outcomes: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 99–107. [Google Scholar] [CrossRef]
- Elango, R.; Ball, R.O. Protein and amino acid requirements during pregnancy. Adv. Nutr. 2016, 7, 839S–844S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Demographic Characteristic | Intervention (n = 119) | Control (n = 122) |
|---|---|---|
| Mean (SD) 1 | Mean (SD) | |
| Maternal age (year) | 31.6 (3.9) | 31.3 (4.3) |
| Gestational age at randomization (week) | 13.75 (1.75) | 13.60 (1.61) |
| Maternal weight, kg | 72.4 (13.4) | 71.8 (13.1) |
| Pre-pregnancy BMI 2 (kg/m2) | 25.7 (4.5) | 25.3 (4.6) |
| n (%) | n (%) | |
| Pre-pregnancy BMI (kg/m2) category | ||
| Underweight (<18.5) | 2 (1.7) | 2 (1.6) |
| Normal weight (18.5–24.9) | 61 (51.3) | 62 (50.8) |
| Overweight (25.0–29.9) | 34 (28.6) | 37 (30.3) |
| Obese (30.0–39.9) | 22 (18.5) | 21 (17.2) |
| University education | 114 (99.1) | 114 (95.8) |
| Missing | 4 | 3 |
| Race/ethnicity | ||
| European descent | 105 (88.2) | 107 (87.7) |
| Mixed/other | 14 (11.8) | 13 (10.7) |
| Missing | 0 | 2 |
| Total family income | ||
| <$45,000 | 7 (5.9) | 10 (8.9) |
| $45,000–$74,999 | 19 (16.2) | 25 (22.1) |
| >$75,000 | 91 (77.8) | 78 (69.0) |
| Missing (=Unknown) | 2 | 9 |
| Married/living with significant other | 117 (98.3) | 114 (96.6) |
| Missing | 0 | 4 |
| Nulliparous | 58 (49.15) | 56 (47.46) |
| Missing | 1 | 4 |
| Study site (city) | ||
| Western U (London) | 38 (31.9) | 39 (32.0) |
| McMaster U (Hamilton/Burlington) | 81 (68.1) | 83 (68.0) |
| Physical and Metabolic Measures | Mean (SD) | Mean (SD) |
| Maternal fat mass | ||
| Bioelectrical impedence (BIA), % body fat | 33.98 (6.55) | 34.11 (7.14) |
| Missing | 8 | 3 |
| Sum of skinfolds (SFT) (mm) | 72.28 (23.32) | 72.07 (26.15) |
| Missing | 3 | 4 |
| Maternal blood pressure (mmHg) | ||
| Systolic | 109.20 (10.43) | 108.95 (10.49) |
| Missing | 2 | 3 |
| Diastolic | 68.96 (7.54) | 69.24 (7.69) |
| Missing | 2 | 3 |
| Maternal physical activity | ||
| Energy expenditure (kcal/day) | 2085 (312) | 2084 (356) |
| Missing | 11 | 11 |
| Average daily step count | 7043 (2655) | 6587 (2545) |
| Missing | 11 | 11 |
| Maternal depression score | 4.34 (3.13) | 4.24 (2.79) |
| Missing | 1 | 1 |
| Maternal metabolic outcomes | ||
| Fasting glucose (mmol/L) | 4.84 (0.60) | 4.77 (0.47) |
| Missing | 13 | 10 |
| Triglycerides (mmol/L) | 1.29 (0.60) | 1.28 (0.42) |
| Missing | 13 | 10 |
| Total cholesterol (mmol/L) | 5.42 (1.18) | 5.24 (0.97) |
| Missing | 13 | 10 |
| HDL-cholesterol (mmol/L) | 1.86 (0.44) | 1.81 (0.39) |
| Missing | 13 | 10 |
| LDL-cholesterol (mmol/L) | 2.97 (0.81) | 2.85 (0.71) |
| Missing | 14 | 10 |
| Leptin (ng/mL) | 31.76 (25.31) | 30.14 (25.54) |
| Missing | 9 | 7 |
| Insulin (pmol/L) | 42.43 (34.81) | 40.88 (29.55) |
| Missing | 10 | 8 |
| Adiponectin (µg/mL) | 8.19 (3.17) | 8.45 (4.10) |
| Missing | 9 | 7 |
| CRP (mg/L) | 6.29 (4.86) | 6.21 (5.65) |
| Missing | 9 | 8 |
| Intervention (n = 119) 1 % Participants | Control (n = 122) 1 % Participants | Intervention Effect | Interaction p | ||
|---|---|---|---|---|---|
| OR 2 (95% CI) 3 | Mean Difference (95% CI) 3 | ||||
| Within IOM guidelines for GWG/week | |||||
| Normal Weight 4 | 49.2% | 34.4% | 1.92 (0.93, 4.00) | . | |
| Overweight 4 | 10.3% | 3.1% | 1.38 (0.23, 8.27) | 0.739 | |
| Obese 4 | 5.9% | 15.8% | 0.26 (0.02, 2.74) | 0.110 | |
| GWG per week (kg/week) 5 | Mean (SD) | Mean (SD) | |||
| Normal Weight 4 IOM recommendation (0.42 kg/week) | n = 58 0.48 (0.15) | n = 61 0.49 (0.16) | −0.03 (−0.08, 0.02) | . | |
| Overweight 4 IOM recommendation (0.28 kg/week) | n = 30 0.48 (0.13) | n = 32 0.53 (0.15) | −0.01 (−0.07, 0.07) | 0.962 | |
| Obese 4 IOM recommendation (0.22 kg/week) | n = 17 0.45 (0.16) | n = 19 0.38 (0.22) | −0.22 (−2.25, 1.81) | 0.813 | |
| Total GWG (kg) | |||||
| Normal Weight 4 IOM recommendation (11.5–16.0 kg) | n = 58 11.02 (3.40) | n = 61 11.43 (3.67) | −0.69 (−1.94, 0.55) | . | |
| Overweight 4 IOM recommendation (7.0–11.5 kg) | n = 30 11.30 (3.11) | n = 32 12.22 (3.69) | −0.33 (−2.02, 1.36) | 0.764 | |
| Obese 4 IOM recommendation (5.0–9.0 kg) | n = 17 10.02 (3.67) | n = 19 8.92 (5.34) | −0.40 (−3.60, 4.41) | 0.539 | |
| Intervention n = 119 | Control n = 122 | Intervention Effect by ITT Mean Difference (95%CI) 1 | p | |
|---|---|---|---|---|
| Birth weight (g) | 3553 (508) | 3476 (456) | 138.10 (−217.72, 493.93) | 0.432 |
| Missing | 12 | 11 | ||
| Gestational age (weeks) | 39.76 (1.30) | 39.72 (1.29) | 0.26 (−1.27, 1.80) | 0.718 |
| Missing | 13 | 10 | ||
| Birth weight category, n (%) 2 | ||||
| Small for gestational age < 10% | 8 (7.55) | 7 (6.31) | 2 | |
| Appropriate for gestational age 10–90% | 87 (82.08) | 97 (87.39) | ||
| Large for gestational age > 90% | 11 (10.38) | 7 (6.31) | ||
| Missing | 13 | 11 | ||
| Birth trauma, n (%) | 3 (2.91) | 0 | 2 | |
| Missing | 16 | 16 | ||
| 5-min Apgar score | 8.92 (0.05) | 8.93 (0.40) | 2 | |
| Missing | 17 | 16 |
| Outcome | Intervention (n = 119) n (%) | Control (n = 122) n (%) | Intervention Effect | |||
|---|---|---|---|---|---|---|
| Complete Case Analysis | ITT Analysis | |||||
| Mean Difference (95% CI) 1 | p | Mean Difference (95% CI) | p | |||
| Maternal Fat Mass | ||||||
| % body fat by BIA | 38.1 (6.1) | 37.7 (5.9) | 0.09 (−0.76, 0.95) | 0.829 | 0.25 (−0.65, 1.15) | 0.582 |
| Missing | 24 | 26 | 55 | − | ||
| Sum of Skinfolds (mm) | 77.1 (22.9) | 75.8 (24.3) | −1.07 (4.86, 2.72) | 0.579 | 1.55 (−31.01, 34.11) | 0.919 |
| Missing | 22 | 26 | 49 | − | ||
| Maternal Blood Pressure (mmHg) | ||||||
| Systolic | 113 (12) | 113 (11) | −0.40 (−3.28, 2.48) | 0.784 | −2.43 (−11.78, 6.91) | 0.593 |
| Missing | 22 | 26 | 49 | − | ||
| Diastolic | 73 (9) | 74 (9) | −1.17 (−3.38, 1.05) | 0.300 | −2.64 (−8.55, 3.26) | 0.371 |
| Missing | 22 | 26 | 49 | |||
| Maternal depression score, median | 3.0 (1,5) | 3.0 (1,6) | −0.06 (−0.30, 0.18) 2 | 0.609 | −0.10 (−0.32, 0.13) 2 | 0.400 |
| Missing | 23 | 25 | 50 | − | ||
| Group Mean (SD) Median (Q1, Q3) 1 | Intervention Effect | |||||
|---|---|---|---|---|---|---|
| Complete Case Analysis | ITT Analysis | |||||
| Metabolite | Intervention n = 119 | Control n = 122 | Mean Difference (95% CI) | p | Mean Difference (95% CI) | p |
| Glucose, mmol/L | 4.6 (0.5) | 4.6 (0.5) | −0.04 (−0.17, 0.08) | 0.481 | −0.02 (−0.16, 0.12) | 0.787 |
| Missing | 31 | 26 | 61 | |||
| HDL, mmol/L | 1.88 (0.44) | 1.87 (0.46) | −0.03 (−0.12, 0.07) | 0.601 | −0.02 (−0.12, 0.09) | 0.759 |
| Missing | 30 | 28 | 62 | |||
| LDL, mmol/L | 4.00 (1.11) | 4.17 (1.09) | −0.31 (−0.57, −0.06) | 0.015 | −0.24 (−0.50, 0.02) | 0.073 |
| Missing | 31 | 30 | 66 | |||
| Triglycerides, mmol/L | 2.53 (0.80) | 2.66 (0.79) | −0.18 (−0.36, 0.01) | 0.062 | −0.16 (−0.38, 0.07) | 0.172 |
| Missing | 30 | 28 | 62 | |||
| Total cholesterol, mmol/L | 7.03 (1.38) | 7.26 (1.33) | −0.41 (−0.72, −0.09) | 0.012 | −0.29 (−0.62, 0.05) | 0.096 |
| Missing | 30 | 28 | 62 | |||
| Insulin, pmol/L | 52.08 (34.06, 82.36) | 47.95 (32.16, 74.31) | <0.01 (−0.15, 0.15) 2 | 0.999 | −0.04 (−0.21, 0.13) 2 | 0.633 |
| Missing | 27 | 25 | 56 | |||
| Leptin, ng/mL | 29.83 (15.97, 49.35) | 30.32 (15.47, 54.63) | −1.37 (−6.67, 3.92) | 0.609 | −0.94 (−8.56, 6.68) 2 | 0.805 |
| Missing | 26 | 25 | 54 | |||
| Adiponectin, ug/mL | 6.97 (2.62) | 7.32 (3.21) | 0.02 (−0.55, 0.58) | 0.956 | −0.05 (−0.97, 0.87) | 0.915 |
| Missing | 26 | 25 | 54 | |||
| CRP, mg/L | 4.29 (2.39, 7.37) | 4.53 (1.92, 7.36) | 0.21 (<0.01, 0.42) 2 | 0.046 | −0.11 (−0.33, 0.55) 2 | 0.600 |
| Missing | 26 | 25 | 55 | |||
| Gestation | 12–17 Weeks | 26–28 Weeks | 36–38 Weeks | |||
|---|---|---|---|---|---|---|
| Group | Intervention | Control | Intervention | Control | Intervention | Control |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| n = 115 | n = 117 | n = 84 | n = 91 | n = 91 | n = 89 | |
| Diet/Physical Activity Measure | ||||||
| 3-day Food Record Data | ||||||
| Energy intake; kcal/day | 2148 1 (491) | 2149 (539) | 2195 (423) | 2129 (499) | 2203 (545) | 2152 (496) |
| Protein intake; g/day | 84.6 (22.5) | 87.5 (23.8) | 108.6 (26.8) | 87.9 (23.2) | 104.4 (25.4) | 87.4 (23.2) |
| Body Media Data | ||||||
| Energy Expenditure; kcal/day | 2085 (312) | 2084 (357) | 2152 (338) | 2127 (387) | 2185 (375) | 2157 (325) |
| Daily step count | 7043 (2655) | 6588 (2545) | 6938 (2717) | 6337 (2647) | 5538 (2490) | 5563 (2208) |
| Outcome Measure 1 | Intervention Effect As at 26–28 Week Gestation | Intervention Effect at 36–38 Week Gestation | ||||||
|---|---|---|---|---|---|---|---|---|
| Complete Case Analysis | ITT Analysis | Complete Case Analysis | ITT Analysis | |||||
| Mean Difference (95%CI) | p | Mean Difference (95%CI) | p | Mean Difference (95% CI) 1 | p | Mean Difference (95% CI) | p | |
| Energy Intake, kcal/day | 60 (−59, 180) | 0.320 | 28 (−984, 154) | 0.662 | 56 (−83, 195) | 0.429 | 32 (−136, 200) | 0.700 |
| Missing | 66 | 61 | ||||||
| Protein Intake, g/day | 21.3 (14.4, 28.1) | <0.001 | 15.0 (8.1, 21.9) | <0.001 | 19.2 (12.8, 25.5) | <0.001 | 15.2 (9.4, 21.1) | <0.001 |
| Missing | 66 | 61 | ||||||
| Energy Expenditure, kcal/day 2 | 0.02 (−0.02, 0.06) | 0.337 | <0.01 (−0.02, 0.02) | 0.904 | <0.01 (−0.04, 0.04) | 0.922 | <0.01 (−0.02, 0.02) | 0.971 |
| Missing | 67 | 94 | ||||||
| Step count/day | 225 (−45, 1901) | 0.512 | 69 (−554, 692) | 0.827 | −415 (−1056, 226) | 0.203 | −315 (−900, 271) | 0.286 |
| Missing | 67 | 91 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atkinson, S.A.; Maran, A.; Dempsey, K.; Perreault, M.; Vanniyasingam, T.; Phillips, S.M.; Hutton, E.K.; Mottola, M.F.; Wahoush, O.; Xie, F.; et al. Be Healthy in Pregnancy (BHIP): A Randomized Controlled Trial of Nutrition and Exercise Intervention from Early Pregnancy to Achieve Recommended Gestational Weight Gain. Nutrients 2022, 14, 810. https://doi.org/10.3390/nu14040810
Atkinson SA, Maran A, Dempsey K, Perreault M, Vanniyasingam T, Phillips SM, Hutton EK, Mottola MF, Wahoush O, Xie F, et al. Be Healthy in Pregnancy (BHIP): A Randomized Controlled Trial of Nutrition and Exercise Intervention from Early Pregnancy to Achieve Recommended Gestational Weight Gain. Nutrients. 2022; 14(4):810. https://doi.org/10.3390/nu14040810
Chicago/Turabian StyleAtkinson, Stephanie A., Atherai Maran, Kendra Dempsey, Maude Perreault, Thuva Vanniyasingam, Stuart M. Phillips, Eileen K. Hutton, Michelle F. Mottola, Olive Wahoush, Feng Xie, and et al. 2022. "Be Healthy in Pregnancy (BHIP): A Randomized Controlled Trial of Nutrition and Exercise Intervention from Early Pregnancy to Achieve Recommended Gestational Weight Gain" Nutrients 14, no. 4: 810. https://doi.org/10.3390/nu14040810
APA StyleAtkinson, S. A., Maran, A., Dempsey, K., Perreault, M., Vanniyasingam, T., Phillips, S. M., Hutton, E. K., Mottola, M. F., Wahoush, O., Xie, F., & Thabane, L. (2022). Be Healthy in Pregnancy (BHIP): A Randomized Controlled Trial of Nutrition and Exercise Intervention from Early Pregnancy to Achieve Recommended Gestational Weight Gain. Nutrients, 14(4), 810. https://doi.org/10.3390/nu14040810







