Dp-ucMGP as a Biomarker in Sarcopenia
Abstract
:1. Introduction
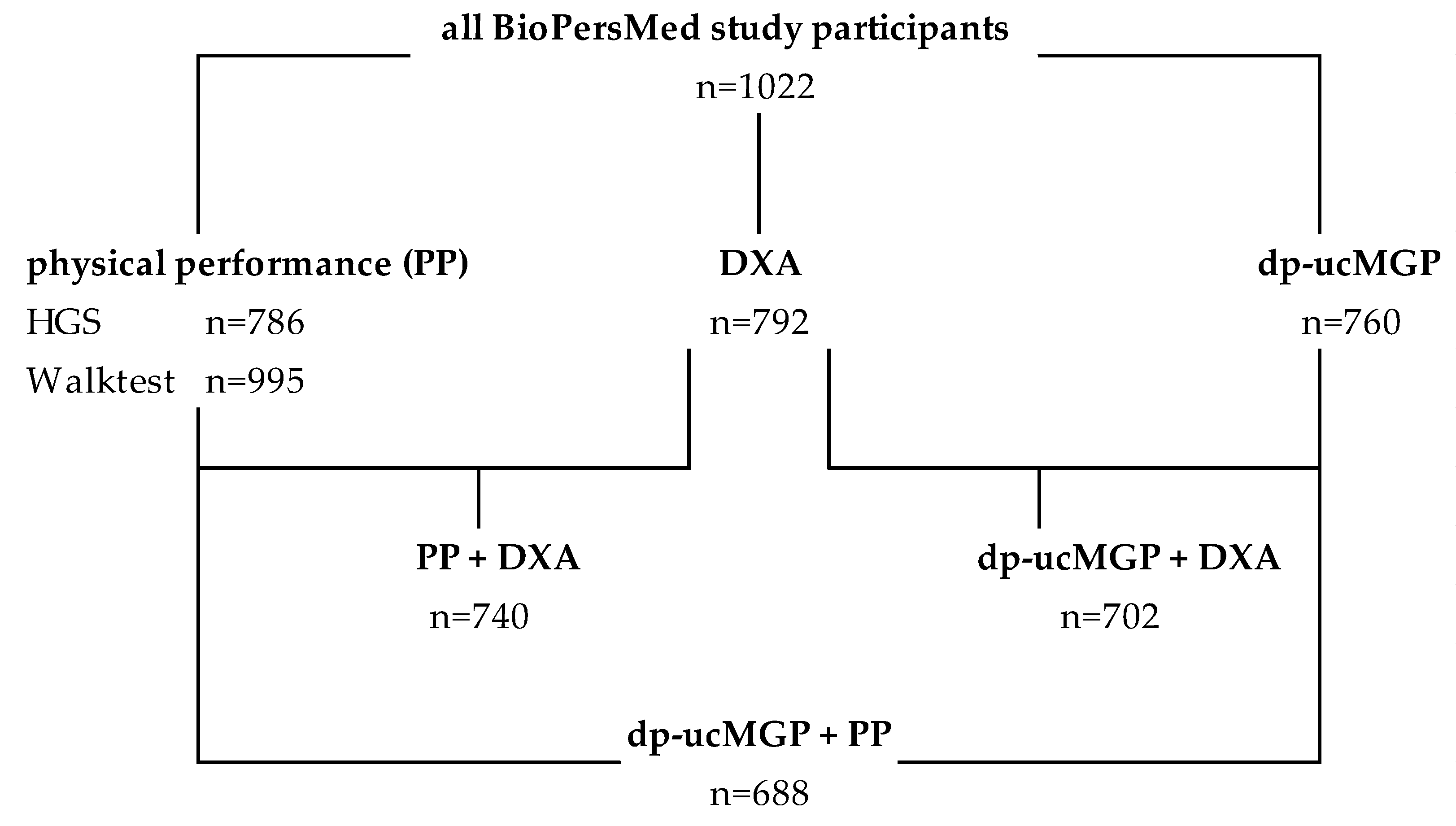
2. Materials and Methods
3. Results
3.1. Description of Study Participants
3.2. Dp-ucMGP Levels in Sarcopenia
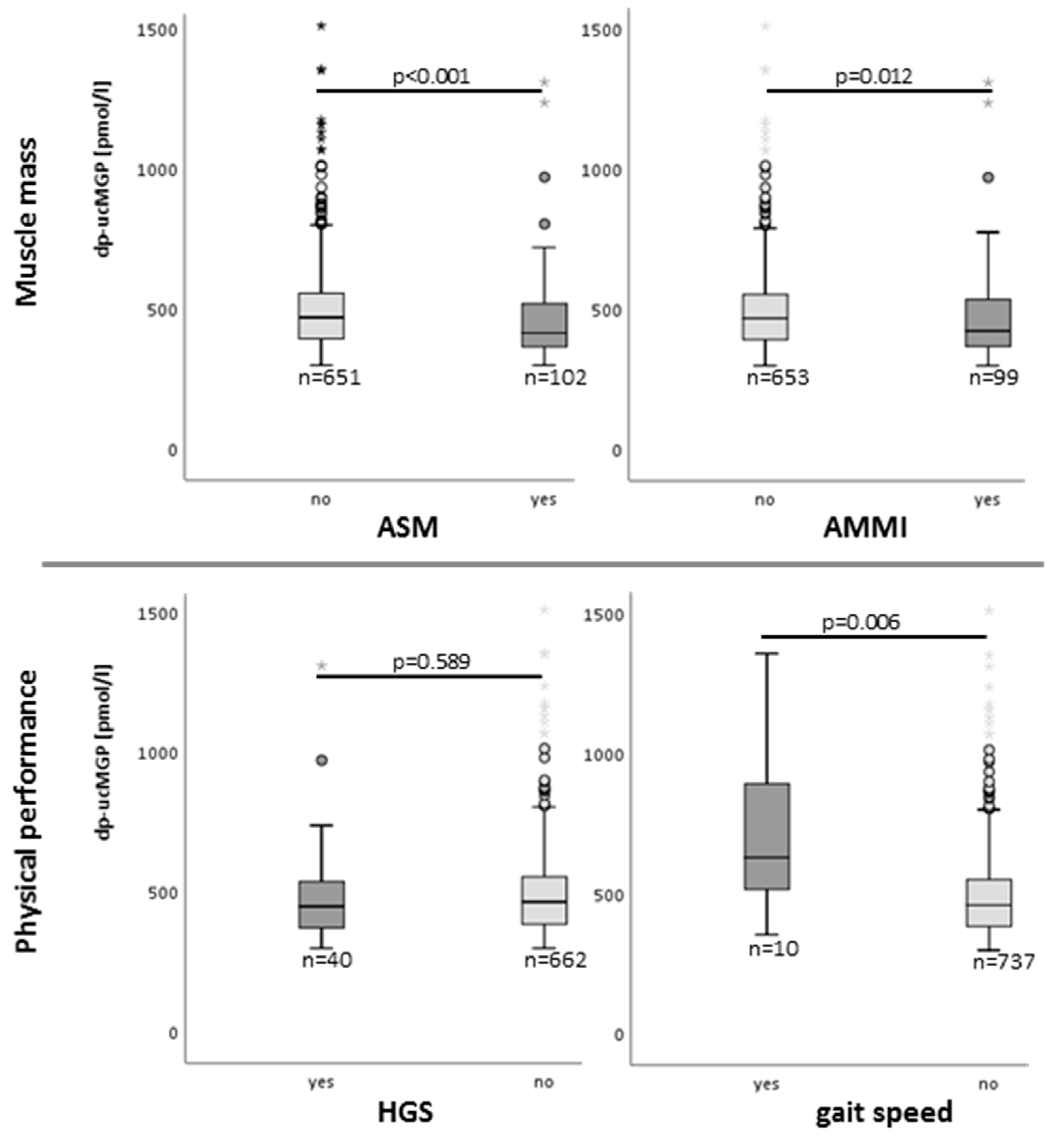
3.3. Dp-ucMGP Serum Levels and Sarcopenia-Related Parameters
3.4. Analysis of Dp-ucMGP Quartiles in Sarcopenia
3.4.1. Baseline Characteristics of the Subgroups
3.4.2. Dp-ucMGP and Sarcopenia Risk
4. Discussion
- Dp-ucMGP plasma levels correlate with the parameters of the three main tissues involved in sarcopenia development (muscle, fat and bone)
- Dp-ucMGP plasma levels correlate with sarcopenia parameters
- ○
- gait speed, ASM and AMMI in all study participants
- ○
- gait speed in sarcopenic participants
- ○
- gait speed, HGS and ASM in all overweight/obese participants
- ○
- gait speed in normal-weight sarcopenic participants
- Dp-ucMGP plasma levels are lower in persons with sarcopenia defined by AMMI and ASM in all persons and higher in persons with reduced physical performance.
- Persons in dp-ucMGP quartile 1 have the highest odds ratio for reduced muscle mass, decreasing with each quartile.
- Persons in dp-ucMGP quartile 4 tend to have the highest risk of reduced muscle strength
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morley, J.E.; Abbatecola, A.M.; Argiles, J.M.; Baracos, V.; Bauer, J.; Bhasin, S.; Cederholm, T.; Coats, A.J.S.; Cummings, S.R.; Evans, W.J.; et al. Sarcopenia with limited mobility: An international Consensus. J. Am. Med. Dir. Assoc. 2011, 12, 403–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- dos Santos, L.; Cyrino, E.S.; Antunes, M.; Santos, D.A.; Sardinha, L.B. Sarcopenia and physical independence in older adults: The independent and synergic role of muscle mass and muscle function. J. Cachexia Sarcopenia Muscle 2016, 8, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Akune, T.; Muraki, S.; Oka, H.; Tanaka, S.; Kawaguchi, H.; Tokimura, F.; Yoshida, H.; Suzuki, T.; Nakamura, K.; Yoshimura, N. Incidence of certified need of care in the long-term care insurance system and its risk factors in the elderly of Japanese population-based cohorts: The ROAD study. Geriatr. Gerontol. Int. 2013, 14, 695–701. [Google Scholar] [CrossRef]
- Steffl, M.; Bohannon Rw Sontakova, L.; Tufano, J.J.; Shiells, K.; Holmerova, I. Relationship-between-sarcopenia-and-physical-activity-in-the. Clin. Interv. Aging 2017, 12, 835–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beaudart, C.; Rizzoli, R.; Bruyère, O.; Reginster, J.-Y.; Biver, E. Sarcopenia: Burden and challenges for public health. Arch. Public Health 2014, 72, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- RCooper, R.; Kuh, D.; Hardy, R. Objectively measured physical capability levels and mortality: Systematic review and meta-analysis. BMJ 2010, 341, 639. [Google Scholar] [CrossRef] [Green Version]
- Vetrano, D.L.; Landi, F.; Volpato, S.; Corsonello, A.; Meloni, E.; Bernabei, R.; Onder, G. Association of sarcopenia with short- and long-term mortality in older adults admitted to acute care wards: Results from the CRIME study. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2014, 69, 1154–1161. [Google Scholar] [CrossRef] [Green Version]
- ACruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- De Buyser, S.L.; Petrovic, M.; Taes, Y.E.; Toye, K.R.C.; Kaufman, J.-M.; Lapauw, B.; Goemaere, S. Validation of the FNIH sarcopenia criteria and SOF frailty index as predictors of long-term mortality in ambulatory older men. Age Ageing 2016, 45, 603–609. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zúñiga, C.; Arai, H.; Boirie, Y.; Chen, L.-K.; Fielding, R.A.; Martin, F.C.; Michel, J.-P.; et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef]
- Grimby, G.; Saltin, B. The ageing muscle. Clin. Physiol. 1983, 3, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B.; et al. The loss of skeletal muscle strength, mass, and quality in older adults: The Health, Aging and Body Composition Study. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2006, 61, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, H.P.; Kinsella, R.; Duque, G. Osteosarcopenia: Where bone, muscle, and fat collide. Osteoporos. Int. 2017, 28, 2781–2790. [Google Scholar] [CrossRef] [PubMed]
- Hoggard, N.; Cruickshank, M.; Moar, K.-M.; Bashir, S.; Mayer, C.-D. Using gene expression to predict differences in the secretome of human omental vs. subcutaneous adipose tissue. Obesity 2012, 20, 1158–1167. [Google Scholar] [CrossRef] [PubMed]
- Akbari, S.; Rasouli-Ghahroudi, A.A. Vitamin K and Bone Metabolism: A Review of the Latest Evidence in Preclinical Studies. BioMed. Res. Int. 2018, 2018, 4629383. [Google Scholar] [CrossRef] [Green Version]
- Wen, L.; Chen, J.; Duan, L.; Li, S. Vitamin K-dependent proteins involved in bone and cardiovascular health (Review). Mol. Med. Rep. 2018, 18, 3–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Ballegooijen, A.J.; van Putten, S.R.; Visser, M.; Beulens, J.W.; Hoogendijk, E.O. Vitamin K status and physical decline in older adults—The Longitudinal Aging Study Amsterdam. Maturitas 2018, 113, 73–79. [Google Scholar] [CrossRef] [Green Version]
- Shea, M.K.; Loeser, R.F.; Hsu, F.-C.; Booth, S.L.; Nevitt, M.; Simonsick, E.M.; Strotmeyer, E.S.; Vermeer, C.; Kritchevsky, S.B. Vitamin K Status and Lower Extremity Function in Older Adults: The Health Aging and Body Composition Study. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2016, 71, 1348–1355. [Google Scholar] [CrossRef] [Green Version]
- Wei, F.-F.; Drummen, N.E.; Thijs, L.; Jacobs, L.; Herfs, M.; Hoofd, C.V.; Vermeer, C.; Staessen, J.A. Vitamin-K-Dependent Protection of the Renal Microvasculature: Histopathological Studies in Normal and Diseased Kidneys. Pulse 2016, 4, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Wei, F.-F.; Huang, Q.-F.; Zhang, Z.-Y.; Van Keer, K.; Thijs, L.; Trenson, S.; Yang, W.-Y.; Cauwenberghs, N.; Mujaj, B.; Kuznetsova, T.; et al. Inactive matrix Gla protein is a novel circulating biomarker predicting retinal arteriolar narrowing in humans. Sci. Rep. 2018, 8, 15088. [Google Scholar] [CrossRef]
- Schurgers, L.J.; Cranenburg, E.C.M.; Vermeer, C. Matrix Gla-protein: The calcification inhibitor in need of vitamin K. Thromb. Haemost. 2008, 100, 593–603. [Google Scholar] [PubMed]
- Cranenburg, E.C.M.; Koos, R.; Schurgers, L.J.; Magdeleyns, E.J.; Schoonbrood, T.H.M.; Landewé, R.B.; Brandenburg, V.M.; Bekers, O.; Vermeer, C. Characterisation and potential diagnostic value of circulating matrix Gla protein (MGP) species. Thromb. Haemost. 2010, 104, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Haudum, C.W.; Kolesnik, E.; Colantonio, C.; Mursic, I.; Url-Michitsch, M.; Tomaschitz, A.; Glantschnig, T.; Hutz, B.; Lind, A.; Schweighofer, N.; et al. Cohort profile: ‘Biomarkers of Personalised Medicine’ (BioPersMed): A single-centre prospective observational cohort study in Graz/Austria to evaluate novel biomarkers in cardiovascular and metabolic diseases. BMJ Open 2022, 12, e058890. [Google Scholar] [CrossRef] [PubMed]
- Boone, S.C.; van Smeden, M.; Rosendaal, F.R.; le Cessie, S.; Groenwold, R.H.H.; Jukema, J.W.; van Dijk, K.W.; Lamb, H.J.; Greenland, P.; Neeland, I.J.; et al. Evaluation of the Value of Waist Circumference and Metabolomics in the Estimation of Visceral Adipose Tissue. Am. J. Epidemiol. 2022, 191, 886–899. [Google Scholar] [CrossRef]
- Ostchega, Y.; Seu, R.; Isfahani, N.S.; Zhang, G.; Hughes, J.P.; Miller, I.M. Waist Circumference Measurement Methodology Study: National Health and Nutrition Examination Survey, 2016; Vital and health statistics. Series 2; National Center for Health Statistics: Hyattsville, MD, USA, 2019; pp. 1–20.
- World Health Organization. The SuRF Report 2, Surveillance Risk Factors Reports Series. 2005, p. 22. Available online: SuRF2(who.int) (accessed on 23 November 2022).
- RDodds, R.M.; Syddall, H.E.; Cooper, R.; Benzeval, M.; Deary, I.J.; Dennison, E.M.; Der, G.; Gale, C.R.; Inskip, H.M.; Jagger, C.; et al. Grip strength across the life course: Normative data from twelve British studies. PLoS ONE 2014, 9, e113637. [Google Scholar] [CrossRef] [Green Version]
- Gould, H.; Brennan, S.L.; Kotowicz, M.A.; Nicholson, G.C.; Pasco, J.A. Total and appendicular lean mass reference ranges for Australian men and women: The Geelong osteoporosis study. Calcif. Tissue Int. 2014, 94, 363–372. [Google Scholar] [CrossRef]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2014, 69, 547–558. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [Green Version]
- Newman, A.B.; Simonsick, E.M.; Naydeck, B.L.; Boudreau, R.M.; Kritchevsky, S.B.; Nevitt, M.C.; Pahor, M.; Satterfield, S.; Brach, J.S.; Studenski, S.A.; et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. J. Am. Med. Assoc. 2006, 295, 2018–2026. [Google Scholar] [CrossRef]
- Stenholm, S.; Harris, T.B.; Rantanen, T.; Visser, M.; Kritchevsky, S.B.; Ferrucci, L. Sarcopenic obesity: Definition, cause and consequences. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 693–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.; Li, J.; He, F.; Li, K.; Li, X.; Zhang, Y. Matrix Gla protein regulates adipogenesis and is serum marker of visceral adiposity. Adipocyte 2020, 9, 68–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mutch, D.M.; Rouault, C.; Keophiphath, M.; Lacasa, D.; Clément, K. Using gene expression to predict the secretome of differentiating human preadipocytes. Int. J. Obes. 2009, 33, 354–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, S.; Jan, A.T.; Baig, M.H.; Lee, E.J.; Choi, I. Matrix gla protein: An extracellular matrix protein regulates myostatin expression in the muscle developmental program. Life Sci. 2017, 172, 55–63. [Google Scholar] [CrossRef]
- Sharma, B.; Albig, A.R. Matrix Gla protein reinforces angiogenic resolution. Microvasc. Res. 2012, 85, 24–33. [Google Scholar] [CrossRef] [Green Version]
- Goodman, C.A.; Hornberger, T.A.; Robling, A.G. Bone and skeletal muscle: Key players in mechanotransduction and potential overlapping mechanisms. Bone 2015, 80, 24–36. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Ma, Z.; Yan, K.; Wang, Y.; Yang, Y.; Wu, X. Matrix Gla Protein Promotes the Bone Formation by Up-Regulating Wnt/β-Catenin Signaling Pathway. Front. Endocrinol. 2019, 10, 891. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, L.; Wang, N.; Li, J.; He, F.; Li, X.; Wu, S. Unexpected Role of Matrix Gla Protein in Osteoclasts: Inhibiting Osteoclast Differentiation and Bone Resorption. Mol. Cell. Biol. 2019, 39, e00012-19. [Google Scholar] [CrossRef] [Green Version]
- Moore, A.E.; Kim, E.; Dulnoan, D.; Dolan, A.L.; Voong, K.; Ahmad, I.; Gorska, R.; Harrington, D.J.; Hampson, G. Serum vitamin K(1) (phylloquinone) is associated with fracture risk and hip strength in post-menopausal osteoporosis: A cross-sectional study. Bone 2020, 141, 115630. [Google Scholar] [CrossRef]
- OKelly, O.J.; Gilman, J.C.; Kim, Y.; Ilich, J.Z. Micronutrient Intake in the Etiology, Prevention and Treatment of Osteosarcopenic Obesity. Curr. Aging Sci. 2016, 9, 260–278. [Google Scholar] [CrossRef]
- van den Heuvel, E.G.H.M.; van Schoor, N.M.; Lips, P.; Magdeleyns, E.J.P.; Deeg, D.J.H.; Vermeer, C.; den Heijer, M. Circulating uncarboxylated matrix Gla protein, a marker of vitamin K status, as a risk factor of cardiovascular disease. Maturitas 2014, 77, 137–141. [Google Scholar] [CrossRef]
- Ma, K.F.; Berends, B.; Vedder, I.R.; Levolger, S.; Gupta, M.; Schuurmann, R.C.; de Vries, J.P.P.M.; Bokkers, R.P. Quantification of muscle mass in the legs of patients with peripheral arterial occlusive disease: Associations between volumetric and cross-sectional single-slice measurements for identification of atrophy and focal sarcopenia. J. Cardiovasc. Surg. 2020, 60, 672–678. [Google Scholar] [CrossRef]
- Southward, K. A hypothetical role for vitamin K2 in the endocrine and exocrine aspects of dental caries. Med. Hypotheses 2015, 84, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, C.; Reese, A.E.; Reynard, L.N.; Loughlin, J. Expression analysis of the osteoarthritis genetic susceptibility mapping to the matrix Gla protein gene MGP. Arthritis Res. Ther. 2019, 21, 149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azuma, K.; Inoue, S. Multiple modes of vitamin K actions in aging-related musculoskeletal disorders. Int. J. Mol. Sci. 2019, 20, 2844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilich, J.Z. Osteosarcopenic adiposity syndrome update and the role of associated minerals and vitamins. Proc. Nutr. Soc. 2021, 80, 344–355. [Google Scholar] [CrossRef]
- Cheng, S.-H.; Chen, K.-H.; Chen, C.; Chu, W.-C.; Kang, Y.-N. The optimal strategy of vitamin d for sarcopenia: A network meta-analysis of randomized controlled trials. Nutrients 2021, 13, 3589. [Google Scholar] [CrossRef]
- Batsis, J.A.; Villareal, D.T. Sarcopenic obesity in older adults: Aetiology, epidemiology and treatment strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef]
- Viegas, C.S.B.; Costa, R.M.; Santos, L.; Videira, P.A.; Silva, Z.; Araújo, N.; Macedo, A.L.; Matos, A.P.; Vermeer, C.; Simes, D.C. Gla-rich protein function as an anti-inflammatory agent in monocytes/macrophages: Implications for calcification-related chronic inflammatory diseases. PLoS ONE 2017, 12, e0177829. [Google Scholar] [CrossRef] [Green Version]
- Feng, Y.; Liao, Y.; Huang, W.; Lai, X.; Luo, J.; Du, C.; Lin, J.; Zhang, Z.; Qiu, D.; Liu, Q.; et al. Mesenchymal stromal cells-derived matrix Gla protein contribute to the alleviation of experimental colitis. Cell Death Dis. 2018, 9, 691. [Google Scholar] [CrossRef]
- Zebboudj, A.F.; Imura, M.; Boström, K. Matrix GLA protein, a regulatory protein for bone morphogenetic protein-2. J. Biol. Chem. 2002, 277, 4388–4394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishimoto, S.K.; Nishimoto, M. Matrix gla protein binds to fibronectin and enhances cell attachment and spreading on fibronectin. Int. J. Cell Biol. 2014, 2014, 807013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.; Lai, S.-T.; Xie, L.; Zhao, J.-D.; Ma, N.-Y.; Zhu, J.; Ren, Z.-G.; Jiang, G.-L. Metformin is associated with reduced risk of pancreatic cancer in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2014, 106, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, A.; Hashemi, R.; Heshmat, R.; Motlagh, A.D.; Esmaillzadeh, A. Patterns of Nutrient Intake in Relation to Sarcopenia and Its Components. Front. Nutr. 2021, 8, 645072. [Google Scholar] [CrossRef]
- Robinson, S.; Granic, A.; Sayer, A.A. Nutrition and muscle strength, as the key component of sarcopenia: An overview of current evidence. Nutrients 2019, 11, 2942. [Google Scholar] [CrossRef] [Green Version]
- Heymsfield, S.B.; Scherzer, R.; Pietrobelli, A.; Lewis, C.E.; Grunfeld, C. Body mass index as a phenotypic expression of adiposity: Quantitative contribution of muscularity in a population-based sample. Int. J. Obes. 2009, 33, 1363–1373. [Google Scholar] [CrossRef] [Green Version]
- Schweighofer, N.; Colantonio, C.; Haudum, C.W.; Hutz, B.; Kolesnik, E.; Mursic, I.; Pilz, S.; Schmidt, A.; Stadlbauer, V.; Zirlik, A.; et al. DXA-Derived Indices in the Characterisation of Sarcopenia. Nutrients 2021, 14, 186. [Google Scholar] [CrossRef]


| Definition of Sarcopenia | |||||
|---|---|---|---|---|---|
| Unit | Calculation | Cut-Off Values | Reference | ||
| males | females | ||||
| HGS | kg | direct measurement | <27 | <16 | [27] |
| AMMI | kg/m2 | ASM/height2 | <7 | <5.5 | [28] |
| ASM | kg | lean mass of arms and legs–bone mass of arms and legs | <20 | <15 | [29] |
| gait speed | m/s | direct measurement | ≤0.8 m/s | [30] | |
| [31] | |||||
| 400 m walk test | min | direct measurement | non-completion or ≥6 min for completion | [32] | |
| All Individuals | Sarcopenia According to AMMI | ||||||
|---|---|---|---|---|---|---|---|
| n = 753 | no | n = 651 | yes | n = 102 | |||
| Mean | SD | Mean | SD | Mean | SD | p-Value | |
| age [years] | 57.1 | 8.7 | 56.6 | 8.2 | 57.8 | 8.7 | 0.204 |
| Muscle parameters | |||||||
| HGS weaker hand [kg] | 31.8 | 10.8 | 32.2 | 10.9 | 29.5 | 9.8 | 0.019 |
| gait speed [min] | 1.4 | 0.3 | 1.4 | 0.3 | 1.4 | 0.2 | 0.297 |
| ASM [kg] | 21.1 | 5.2 | 21.8 | 5.1 | 17.0 | 3.7 | <0.001 |
| AMMI [kg/m2] | 7.3 | 1.3 | 7.5 | 1.2 | 5.8 | 0.8 | <0.001 |
| Fat parameters | |||||||
| fat mass [kg] | 26.6 | 9.3 | 27.5 | 9.4 | 20.7 | 5.4 | <0.001 |
| waist-to-height ratio | 0.54 | 0.08 | 0.55 | 0.08 | 0.48 | 0.06 | <0.001 |
| BMI [kg/m2] | 26.5 | 4.6 | 27.1 | 4.4 | 22.5 | 2.6 | <0.001 |
| Bone parameters | |||||||
| BMD [mg/cm3] | 1.19 | 0.13 | 1.20 | 0.13 | 1.15 | 0.13 | 0.001 |
| T-score | 0.61 | 1.13 | 0.67 | 1.12 | 0.23 | 1.10 | <0.001 |
| All Individuals | Sarcopenia According to AMMI | |||||||
|---|---|---|---|---|---|---|---|---|
| Normal Weight | Overweight/Obese | Normal Weight | Overweight/Obese | |||||
| CC | p-value | CC | p-value | CC | p-value | CC | p-value | |
| Physical performance | n = 275 | n = 423 | n = 76 | n = 18 | ||||
| HGS weaker hand [kg] | −0.064 | 0.290 | −0.163 | 0.001 | −0.113 | 0.331 | −0.294 | 0.294 |
| gait speed [min] | −0.092 | 0.112 | −0.201 | <0.001 | −0.230 | 0.040 | −0.319 | 0.170 |
| Muscle mass | n = 298 | n = 455 | n = 82 | n = 20 | ||||
| ASM [kg] | 0.038 | 0.511 | −0.086 | 0.067 | 0.069 | 0.540 | −0.119 | 0.617 |
| AMMI [kg/m2] | −0.031 | 0.595 | −0.064 | 0.174 | 0.028 | 0.810 | −0.031 | 0.897 |
| Fat parameters | n = 281 | n = 421 | n = 80 | n = 20 | ||||
| fat mass [kg] | 0.270 | <0.001 | 0.334 | <0.001 | 0.230 | 0.040 | −0.074 | 0.758 |
| waist to height ratio | 0.223 | <0.001 | 0.300 | <0.001 | 0.209 | 0.060 | 0.246 | 0.296 |
| Bone parameters | n = 281 | n = 421 | n = 80 | n = 20 | ||||
| BMD [mg/cm3] | −0.122 | 0.041 | −0.048 | 0.327 | −0.088 | 0.440 | 0.098 | 0.682 |
| T-value | −0.154 | 0.010 | 0.004 | 0.934 | −0.161 | 0.150 | 0.106 | 0.656 |
| Dp-ucMGP Q1 | Dp-ucMGP Q2 | Dp-ucMGP Q3 | Dp-ucMGP Q4 | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| dp-ucMGP range [pmol/L] | lowest to 384 | 385 to 462 | 463 to 551 | 552 to highest | |||||
| n | 190 | 190 | 189 | 191 | |||||
| dp-ucMGP [pmol/L] | 345 | ±28 | 423 | ±22 | 502 | ±25 | 706 | ±200 | |
| males | 40% | 44% | 49% | 44% | 0.405 | ||||
| age [years] | 54 | ±7 | 55 | ±7 | 57 | ±8 | 61 | ±9 | <0.001 |
| Waist-to-hip ratio | 0.89 | ±0.09 | 0.92 | ±0.08 | 0.93 | ±0.08 | 0.94 | ±0.08 | <0.001 |
| BMI [kg/m2] | 24.5 | ±4.0 | 25.8 | ±3.7 | 26.8 | ±4.5 | 28.6 | ±4.4 | <0.001 |
| alcohol consumption [drinks/week] | 3 | ±5 | 4 | ±7 | 3 | ±5 | 3 | ±6 | 0.050 |
| bone mass extremities [kg] | 1.34 | ±0.33 | 1.38 | ±0.34 | 1.44 | ±0.34 | 1.39 | ±0.33 | 0.053 |
| ASM [kg] | 20.21 | ±5.24 | 21.19 | ±5.59 | 21.80 | ±5.42 | 21.53 | ±4.99 | 0.012 |
| AMMI [kg/m2] | 6.99 | ±1.32 | 7.28 | ±1.44 | 7.38 | ±1.35 | 7.45 | ±1.27 | 0.004 |
| HGS weaker hand [kg] | 33.07 | ±10.75 | 31.30 | ±11.32 | 32.91 | ±11.35 | 30.59 | ±9.64 | 0.226 |
| Gait speed [m/s] | 1.47 | ±0.25 | 1.46 | ±0.23 | 1.44 | ±0.25 | 1.33 | ±0.24 | <0.001 |
| Smoking [pack years] | 8.1 | ±13.1 | 8.6 | ±13.5 | 6.5 | ±11.3 | 8.3 | ±14.2 | 0.317 |
| Dp-ucMGP Q1 | Dp-ucMGP Q2 | Dp-ucMGP Q3 | Dp-ucMGP Q4 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | p | OR | B-Value | CI | p | OR | B-Value | CI | p | OR | B-Value | CI | p | |||||
| AMMI | ||||||||||||||||||
| unadjusted | 1 | 0.026 | 0.523 | −0.648 | 0.296 | 0.925 | 0.026 | 0.496 | −0.700 | 0.279 | 0.884 | 0.017 | 0.493 | −0.706 | 0.277 | 0.878 | 0.026 | |
| Model 1 | 1 | 0.083 | 0.476 | −0.743 | 0.225 | 1.003 | 0.051 | 0.589 | −0.530 | 0.272 | 1.272 | 0.178 | 0.389 | −0.944 | 0.176 | 0.860 | 0.020 | |
| Model 2 | 1 | 0.049 | 0.463 | −0.770 | 0.217 | 0.986 | 0.046 | 0.504 | −0.685 | 0.229 | 1.109 | 0.088 | 0.346 | −1.062 | 0.154 | 0.779 | 0.010 | |
| ASM | ||||||||||||||||||
| unadjusted | 1 | 0.003 | 0.637 | −0.450 | 0.369 | 1.101 | 0.106 | 0.496 | −0.700 | 0.279 | 0.884 | 0.017 | 0.316 | −1.153 | 0.165 | 0.605 | 0.001 | |
| Model 1 | 1 | 0.002 | 0.506 | −0.681 | 0.241 | 1.063 | 0.072 | 0.430 | −0.845 | 0.191 | 0.969 | 0.042 | 0.164 | −1.809 | 0.064 | 0.418 | <0.001 | |
| Model 2 | 1 | 0.003 | 0.511 | −0.671 | 0.244 | 1.073 | 0.076 | 0.454 | −0.790 | 0.199 | 1.034 | 0.060 | 0.171 | −1.768 | 0.067 | 0.436 | <0.001 | |
| HGS | ||||||||||||||||||
| unadjusted | 1 | 0.795 | 1.084 | 0.081 | 0.465 | 2.257 | 0.851 | 1.325 | 0.282 | 0.544 | 3.230 | 0.536 | 1.536 | 0.429 | 0.612 | 3.855 | 0.360 | |
| Model 1 | 1 | 0.381 | 1.294 | 0.258 | 0.441 | 3.795 | 0.639 | 1.838 | 0.609 | 0.552 | 6.123 | 0.321 | 2.898 | 1.064 | 0.840 | 9.994 | 0.092 | |
| Model 2 | 1 | 0.205 | 1.330 | 0.285 | 0.444 | 3.990 | 0.611 | 2.458 | 0.899 | 0.714 | 8.458 | 0.154 | 3.688 | 1.305 | 1.007 | 13.502 | 0.049 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schweighofer, N.; Haudum, C.W.; Trummer, O.; Lind, A.; Kolesnik, E.; Mursic, I.; Schmidt, A.; Scherr, D.; Zirlik, A.; Pieber, T.R.; et al. Dp-ucMGP as a Biomarker in Sarcopenia. Nutrients 2022, 14, 5400. https://doi.org/10.3390/nu14245400
Schweighofer N, Haudum CW, Trummer O, Lind A, Kolesnik E, Mursic I, Schmidt A, Scherr D, Zirlik A, Pieber TR, et al. Dp-ucMGP as a Biomarker in Sarcopenia. Nutrients. 2022; 14(24):5400. https://doi.org/10.3390/nu14245400
Chicago/Turabian StyleSchweighofer, Natascha, Christoph W. Haudum, Olivia Trummer, Alice Lind, Ewald Kolesnik, Ines Mursic, Albrecht Schmidt, Daniel Scherr, Andreas Zirlik, Thomas R. Pieber, and et al. 2022. "Dp-ucMGP as a Biomarker in Sarcopenia" Nutrients 14, no. 24: 5400. https://doi.org/10.3390/nu14245400
APA StyleSchweighofer, N., Haudum, C. W., Trummer, O., Lind, A., Kolesnik, E., Mursic, I., Schmidt, A., Scherr, D., Zirlik, A., Pieber, T. R., Verheyen, N., & Obermayer-Pietsch, B. (2022). Dp-ucMGP as a Biomarker in Sarcopenia. Nutrients, 14(24), 5400. https://doi.org/10.3390/nu14245400






