Abstract
The association of free sugars intake with metabolic syndrome (MetS) is controversial. This study aimed to examine the association between free sugars intake and risk of MetS in Chinese adults. The data were from seven waves of the China Health and Nutrition Survey (2000–2018), a longitudinal and open prospective cohort study. Dietary intake was calculated based on the data collected by consecutive 3-day 24-h dietary recalls combined with household weighing for foods or condiments. Cox proportion hazard regressions and restricted cubic spline (RCS) were performed to explore the associations between free sugars intake and the risk of MetS. The present study selected 12,048 adults aged 18 years and above. During a median (IQR) follow-up of 9.0 (7.0, 15.0) years with 131,844.0 person-years, 3970 (32.95%) MetS occurred. After adjusting for all potential confounders, compared to adults with free sugars intake of <5 g/day group, adults with free sugars intake of 5–20 g/day were associated with a higher risk of MetS (HR, 1.094; 95% CI, 1.009–1.186). No significant association was observed between free sugars intake of >20 g/day and the risk of MetS (HR, 1.011; 95% CI, 0.800–1.277). There is an urgent need to pay attention to the intake of free sugars and comprehensive measures such as the improvements in the processing of sugary foods, and sugar composition should be included on food nutrition labels to control intake of free sugars in China.
1. Introduction
Metabolic syndrome (MetS) is defined as a cluster of metabolic alterations including abdominal obesity, abnormal high-density lipoprotein cholesterol (HDL-C), elevated triglyceride (TG), high fasting blood glucose, and hypertension [1]. MetS has become a major public health concern, which can contribute to a higher risk of type 2 diabetes (T2D), cardiovascular disease (CVD), stroke, coronary heart disease, and all-cause mortality [2]. The study of the National Health and Nutrition Examination Survey (NHANES, 2011–2016) has shown that the MetS prevalence was 34.7% among adults in the United States [3]. According to data from China Nutrition and Health Surveillance (2015–2017), nearly a third (31.1%) of adults aged 20 and above had MetS in China [4]. Several studies suggest that food and nutrients are thought to play an important role in the development of MetS. “Free sugars” refer to monosaccharides and disaccharides which are added to foods and beverages by the manufacturer, cook, or consumer, and sugars naturally present in syrups, honey, fruit juices, and fruit juice concentrates, according to the World Health Organization (WHO). Free sugars may promote a positive energy balance and increase overall energy intake [5]. More and more epidemiologic studies have proven that intake of free sugars—particularly in the form of sugar-sweetened beverages (SSBs)—contribute to weight gain, MetS, and increased risk of noncommunicable diseases (NCDs) [6,7,8,9,10]. Nevertheless, the association of free sugars intake with MetS remains controversial [11]. Studies have found that sugar consumption can increase the risk of MetS that associates with excess ectopic fat accumulation [12]. Okuda et al. showed that there are no significant associations between high added sugars intake and MetS among Japanese adolescents [13]. Data from some RCTs and meta-analyses showed that there are no significant linkages between various adverse metabolic health effects and sugar consumption at normal levels within diets [14]. Given the sugary foods intake and increasing prevalence of MetS of Chinese residents, it is especially important to determine whether free sugars intake is associated with the risk of MetS. Therefore, the present study investigated the association between the intake of free sugars and the risk of MetS in Chinese adults aged 18 and above from the China Health and Nutrition Survey (CHNS 2000–2018) and put forward specific suggestions and strategies to reduce sugar intake and prevent MetS.
2. Materials and Methods
2.1. Study Population
All data used in current study were derived from the CHNS, which was a prospective and longitudinal cohort survey in China. A multistage, random cluster process was used to draw the sample in each province to ensure that urban and rural areas were represented. The CHNS aimed to develop a longitudinal survey that would understand how demographic and social economic changes in China affected health and health behaviors. The CHNS was designed to provide a representation of rural and urban areas varying in economy, geography, and health indicators with examining household-level and individual-level demographic factors, diet, health behavior, physical activity, and behavior changes. The background, aims, design, and methods of the survey have been described in detail elsewhere [15,16].
Our analysis used the seven waves of survey data between 2000 and 2018. All participants aged 18 and above who had complete data on dietary, socioeconomic, demographic, anthropometric, and other lifestyle factors were included. We excluded those that had MetS at baseline; those with implausible energy intakes (men: <800 kcal per day or >6000 kcal; women: <600 kcal or >4000 kcal); those with missing weight, height, serum lipids, blood pressure, blood glucose; those only in one wave before MetS was diagnosed; and those pregnant or lactating women during the survey. A total of 12,048 adults (5812 men and 6236 women) were included in the current analysis.
The survey was approved by the Institutional Review Committees of the University of North Carolina at Chapel Hill (UNC-CH) and the National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention (No. 201524). Written informed consent was obtained from all subjects.
2.2. Definition of Metabolic Syndrome
According to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria, MetS was defined if three out of five of the following components are present: (1) waist circumference ≥90 cm for men and ≥80 cm for women; (2) fasting triglycerides (TG) ≥ 150 mg/dL or specific treatment for lipid abnormality; (3) high-density lipoprotein cholesterol (HDL-C) < 1.0 mmol/L in men and 1.3 mmol/L in women; (4) diastolic blood pressure ≥ 85 mmHg or systolic blood pressure ≥ 130 mmHg, or treatment of previously diagnosed hypertension; (5) Fasting plasma glucose ≥ 6.0 mmol/L or diagnosed type 2 diabetes previously [17].
2.3. Measurement of Indicators
At least two trained health workers or nurses calibrated the instrument before taking physical measurements. Waist circumference, weight, and height were measured using a non-retractable material flexible ruler, electronic weight scale, SECA206 altimeter. Blood pressure was measured by a standard mercury sphygmomanometer (SBP and DBP were determined according to Korotkoff sound). After at least five minutes of rest in a quiet room, the participants were in a seated position and with the bladder emptied, and three consecutive standard measurements were taken for each participant to obtain the average value. TG and HDL-C were measured using cholesterol oxidase-phenol and an amino phenazone method. Fasting plasma glucose was measured by a Roche 702 instrument using the hexokinase method.
2.4. Assessment of Dietary Free Sugars
Dietary data were collected by consecutive 3-day 24-h dietary recalls (2 weekdays and 1 weekend) for each individual and seasonings in the household inventory were weighed. Quantities and types of all food consumed at home and away from home during the preceding 24 h were collected by trained investigators. Food consumption at the household level, such as oil, salt, sugar, and other condiments, was calculated by the ratio of each participant’s energy intake to the energy intake of the whole family and times of eating at home.
For the free sugars content in food, we used High performance Liquid Chromatography (HPLC) to determine the content of different kinds of food including SSBs, bakery products, candies, and chocolate. For some foods such as sauces and honey, the free sugars content was used from the China Food Composition Table (2004/2009) [18,19] and Food Nutrition Facts.
2.5. Definition of Covariates
Covariates including gender, age, education, geographic region, per capita annual family income, alcohol drinking history, smoking history, and physical activity were collected by trained interviewers through standard questionnaires. All activities including leisure time, household chores, occupational, and transportation activities in average hours per week were reported by participants, and then were converted into a metabolic equivalent-hours/week (MET-h/week) based on the American College of Sports Medicine Association’s recommended standard [20]. The individual annual income, physical activity, and energy intake were categorized into tertiles (low, medium, and high) in the analyses.
2.6. Statistical Analysis
Chi-square test for categorical variables were used to examine the differences of sociodemographic characteristics and lifestyles across different daily free sugars intake levels. The association between free sugars intake and the risk of MetS was explored by a multivariable Cox of proportional hazards model to estimate the hazard ratios (HRs) and 95% CIs. We constructed three sequential models. Model 1 adjusted for baseline age, gender, educational level, place of residence, region of residence, educational level, individual annual income, drinking history, and smoking history. Model 2 was further adjusted for physical activity based on Model 1. Model 3 was further adjusted for total energy intake based on Model 2.
To assess the nonlinear association between free sugars intake and the risk of MetS, restricted cubic spine (RCS) regressions were performed with the same covariates adjusted in the primary analysis among overall participants and subgroups for men and women.
All statistical analyses were performed using SAS version 9.4 software (SAS Institute Inc., Cary, NC, USA) and R version 4.1.0 (R Development Core Team, Vienna, Austria). All statistical tests were two-tailed and considered significant at p < 0.05.
3. Results
3.1. Basic Characteristics of Participants
A total of 12,048 participants were included in our study; 5812 (48.2%) were men and 6236 (51.8%) were women. Of the participants, 9056 (75.2%) consumed free sugars < 5 g/day, 2645 (22.0%) consumed 5–20 g/day, and 347 (2.9%) consumed >20 g/day. The median (IQR) age at baseline was 43.9 (33.9, 54.4) years. Among all the subgroups, the proportion was higher among participants who consumed free sugars < 5 g/day than those who consumed 5–20 g/day or >20 g/day. The proportion of participants that had a senior high education level, from urban areas, and had high income was almost about one third, respectively (Table 1).

Table 1.
Basic characteristics of overall participants according to different levels of free sugars intake, CHNS.
For men, the proportion was higher among participants who had drinking history or smoking history with free sugars intake of <5 g/day and 5–20 g/day, respectively. The proportion was lower among participants who had low energy intake with free sugars intake of <5 g/day and 5–20 g/day, respectively. For women, the opposite is true for men (Table 2 and Table 3).

Table 2.
Basic characteristics of men according to different levels of free sugars intake, CHNS.

Table 3.
Basic characteristics of women according to different levels of free sugars intake, CHNS.
3.2. Association between Free Sugars Intake and the Risk of MetS
Table 2 shows the longitudinal association between free sugars intake and the risk of MetS in overall participants and stratified by gender. During a median (IQR) follow-up of 9.0 (7.0, 15.0) years with 131,844.0 person-years, 3970 (32.95%) MetS occurred. After adjusting for potential confounders in each model, compared to adults with free sugars intake <5 g/day group, adults with free sugars intake of 5–20 g/day were associated with a higher risk of MetS (HR, 1.094; 95% CI, 1.009–1.186). No significant association was observed between free sugars intake of >20 g/day and the risk of MetS (HR, 1.011; 95% CI, 0.800–1.277).
The results were different between gender-stratified analyses. No association was observed among men with free sugars intake of 5–20 g/day (HR, 1.077; 95% CI, 0.957–1.213) and >20 g/day (HR, 1.073; 95% CI, 0.782–1.473) compared to <5 g/day free sugars intake group. Women with free sugars intake of 5–20 g/day were associated with a higher risk of MetS (HR, 1.122; 95% CI, 1.003–1.255) (Table 4).

Table 4.
Association between free sugars intake and the risk of MetS.
3.3. Nonlinear Associations between Free Sugars Intake and the Risk of MetS
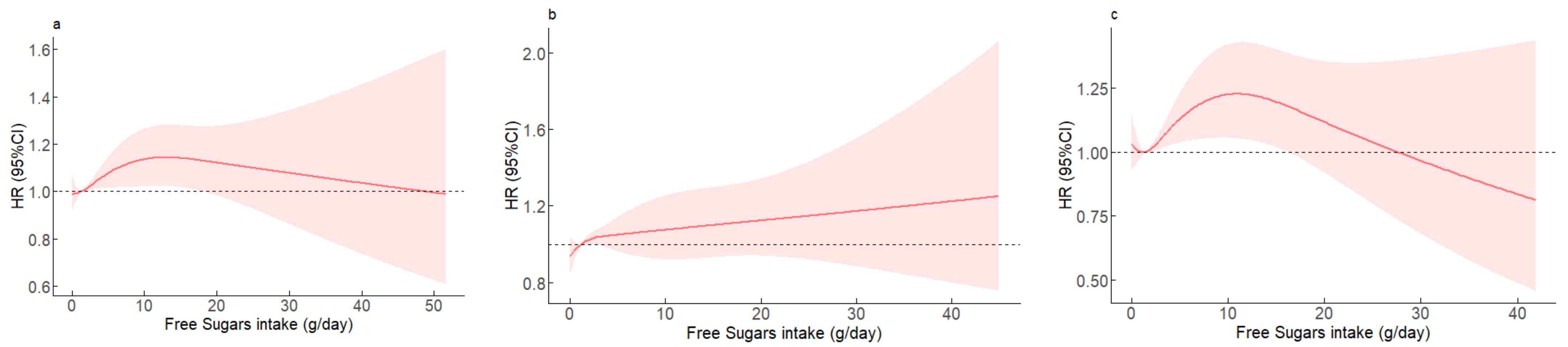
Estimated associations between free sugars intake and the risk of MetS are shown from nonlinear RCS models among the overall participants, men, and women (Figure 1). Among the overall participants, free sugars intake of 5–20 g/day was associated with a higher risk of MetS, whereas >20 g/day was not associated with MetS. Women with free sugars intake of 5–20 g/day were associated with a higher risk of MetS while no significant association was observed for men.
Figure 1.
The relationships between free sugars intake and the risk of MetS during follow-up. The hazard ratio for MetS with the corresponding 95% confidence interval as a function of free sugars intake from Cox proportional hazard regression models adjusted for gender, age, educational level, place of residence, region of residence, individual annual income, drinking history, smoking history, physical activity, and total energy. (a) overall participants, p for nonlinear = 0.1623; (b) men, p for nonlinear = 0.4183; (c) women, p for nonlinear = 0.0374.
4. Discussion
Using CHNS 2000–2018, this study examined the association between free sugars intake and risk of MetS among Chinese adults. A significantly higher consumption of free sugars was found among adults who had senior high school or above education, lived in urban areas, had higher income, or had lower physical activity. We found that high consumption of free sugars was associated with an increased risk of MetS. Furthermore, free sugars intake of 5–20 g/day was positively associated with MetS in Chinese women, whereas a similar association was not observed in Chinese men.
The health effects of free sugars intake on people have been discussed for many years. More and more studies focus on the association between free sugars intake and chronic noncommunicable diseases such as overweight/obesity [21,22], diabetes [23], and cardiovascular diseases [6]. In a cross-sectional analysis of the NHANES (2005–2012), Rodríguez et al. found that, in the highest quintile of added sugar intake, the risk of MetS increased by 8.7 times in adolescents (POR = 8.7, 95% CI = 1.4–54.9) [24]. In the study of 7005 adults aged 40–69 years in Korea, the males had a significantly higher odds of MetS (OR = 1.332, 95% CI = 1.038–1.709) than those who with a lower ratio of energy from total sugar, but women did not [25]. Nevertheless, in our study, we found a positive association between free sugars intake and MetS in women, but not in men. It is unclear why men and women showed a different association between sugar intake and metabolic disease. It might be explained by dietary behavior differences between men and women that could alter the metabolic profile and level of hormones, which could affect metabolic disease.
There are several explanations and mechanisms for the association between sugar intake and cardiometabolic risk factors. Free sugars were provided mostly by SSBs and sweet products in the diet [26,27]. The energy can be absorbed rapidly with the form of free sugar or SSBs. Then, a positive energy balance happened and increased weight [28]. Moreover, some evidence suggests that free sugars (glucose, sucrose, and fructose) seem to interfere with the metabolism of essential fatty acids and decrease the formation of arachidonic acid, eicosapentaenoic acid, and docosahexaenoic acid, which could predispose to the development of metabolic syndrome [29].
In 2015, WHO recommended a reduced intake of free sugars throughout one’s whole life. Furthermore, it is recommended to reduce the intake of free sugars to <10% of total energy intake and a further reduction of the intake of free sugars to <5% of total energy intake for adults [30]. Dietary Guidelines for Americans (2020–2025) recommend that a healthy dietary pattern limits added sugars to less than 10 percent of calories per day [31]. According to the dietary guidelines for Chinese residents, it recommended to limit the intake of added sugars to no more than 50 g/day, preferably under 25 g/day [32]. In this study, free sugars intake of 5–20 g/day was positively associated with MetS among adults. A modeling study has found that a reduction in free sugars added to sugar-sweetened beverages was predicted to reduce the prevalence of overweight, obesity, and type 2 diabetes [33].
Many current studies indicate that both added and free sugars are recommended to be consumed in moderation. Compared with the consumption level of western countries, the consumption of free sugars—particularly in the form of SSBs—in China is still at a relatively low level. Thus, the risk of chronic non-communicable diseases is relatively low with free sugars intake at lower levels in China [26,34]. Nevertheless, with the development of the economy and changes of lifestyle, the eating behavior and diet is also changing in China. Traditional dietary patterns in China are shifting to western dietary patterns with an increase in packaged foods consumption such as SSBs [35]. Mullee et al. showed that higher all-cause mortality was found in participants who consumed ≥2 glasses per day of SSBs compared to consumers of <1 glass per month [36]. A recent study showed that the number of deaths was 46,633 in 2019 attributed to high SSBs intake in China, which is about double the number in 1990 [37]. Considering the growing trend of sugary food and SSBs consumption and the increasing prevalence of MetS, it is necessary to pay more attention to the problem of excessive intake of free sugars in Chinese adults.
The strengths of our study include using a large participant size and longer follow-up data from CHNS. Moreover, we adopted a multivariable Cox of proportional hazards model to classify the association between free sugars intake and the risk of MetS. However, our study still had several limitations that deserve discussion. Firstly, it may be possible for recall bias to occur because of the dietary intake assessment using three 24 h recalls. Secondly, the possibility of residual confounding cannot be excluded completely on the account of the nature of observational studies. Thirdly, we used the sugar content of sugary foods that are commonly available on the market. There may be differences of sugar content among different batches of sugary foods.
5. Conclusions
This present prospective study provides evidence that free sugars intake of 5–20 g/day is positively correlated with MetS in Chinese adults, especially among women. Therefore, the mechanism of free sugars with MetS and its single component between sexes is worth detailed study in the future. We suggest that attention should be paid to the intake of free sugars and comprehensive measures such as the improvements in the processing of sugary foods, and sugar composition should be included on food nutrition labels to control the intake of free sugars in China.
Author Contributions
Data preparation, statistical analysis, and original draft preparation, F.P.; data collection, paper revision, and guidance, Z.W., H.W., C.S., J.Z., W.D., X.J., L.W., H.J. and W.L.; research guidance, paper review, and administrative support, H.W. and B.Z.; research design, funding support, paper revision, and review, Z.W. and G.D. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Study of Diet and Nutrition Assessment and Intervention Technology (No. 2020YFC2006300) from the Active Health and Aging Technologic Solutions Major Project of the National Key R&D Program; the Chinese Center for Disease Control National Institute of Nutrition and Health, the National Institutes of Health (NIH) (R01-HD30880 and R01-HD38700); The Ministry of Finance of the Republic of China (13103110700015005).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Committees of the University of North Carolina at Chapel Hill (UNC-CH) and the National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention (No. 201524).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data sharing is not applicable to this article.
Acknowledgments
The authors thank all the participants and staff involved in CHNS.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Hirode, G.; Wong, R.J. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011–2016. JAMA 2020, 323, 2526–2528. [Google Scholar] [CrossRef] [PubMed]
- Yao, F.; Bo, Y.; Zhao, L.; Li, Y.; Ju, L.; Fang, H.; Piao, W.; Yu, D.; Lao, X. Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients 2021, 13, 4475. [Google Scholar] [CrossRef] [PubMed]
- Elia, M.; Cummings, J.H. Physiological aspects of energy metabolism and gastrointestinal effects of carbohydrates. Eur. J. Clin. Nutr. 2007, 61, S40–S74. [Google Scholar] [CrossRef]
- Vos, M.B.; Kaar, J.L.; Welsh, J.A.; Van Horn, L.V.; Feig, D.I.; Anderson, C.A.M.; Patel, M.J.; Cruz Munos, J.; Krebs, N.F.; Xanthakos, S.A.; et al. Added Sugars and Cardiovascular Disease Risk in Children: A Scientific Statement From the American Heart Association. Circulation 2017, 135, e1017–e1034. [Google Scholar] [CrossRef]
- Malik, V.S.; Pan, A.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and weight gain in children and adults: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 1084–1102. [Google Scholar] [CrossRef]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Despres, J.P.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care 2010, 33, 2477–2483. [Google Scholar] [CrossRef]
- Lin, T.K.; Teymourian, Y.; Tursini, M.S. The effect of sugar and processed food imports on the prevalence of overweight and obesity in 172 countries. Glob. Health 2018, 14, 35. [Google Scholar] [CrossRef]
- de Koning, L.; Malik, V.S.; Kellogg, M.D.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation 2012, 125, 1735–1741. [Google Scholar] [CrossRef]
- Stanhope, K.L. Sugar consumption, metabolic disease and obesity: The state of the controversy. Crit. Rev. Clin. Lab. Sci. 2016, 53, 52–67. [Google Scholar] [CrossRef] [PubMed]
- Taskinen, M.R.; Packard, C.J.; Boren, J. Dietary Fructose and the Metabolic Syndrome. Nutrients 2019, 11, 1987. [Google Scholar] [CrossRef] [PubMed]
- Okuda, M.; Fujiwara, A.; Sasaki, S. Added and Free Sugars Intake and Metabolic Biomarkers in Japanese Adolescents. Nutrients 2020, 12, 2046. [Google Scholar] [CrossRef] [PubMed]
- Rippe, J.M.; Angelopoulos, T.J. Sugars, obesity, and cardiovascular disease: Results from recent randomized control trials. Eur. J. Nutr. 2016, 55, 45–53. [Google Scholar] [CrossRef]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989–2011. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2014, 15, 2–7. [Google Scholar] [CrossRef]
- University of North Carolina; Chinese Center for Disease Control and Prevention. Available online: https://www.cpc.unc.edu/projects/china (accessed on 27 June 2015).
- Heng, D.; Ma, S.; Lee, J.J.; Tai, B.C.; Mak, K.H.; Hughes, K.; Chew, S.K.; Chia, K.S.; Tan, C.E.; Tai, E.S. Modification of the NCEP ATP III definitions of the metabolic syndrome for use in Asians identifies individuals at risk of ischemic heart disease. Atherosclerosis 2006, 186, 367–373. [Google Scholar] [CrossRef]
- Yang, Y. China Food Composition 2004; Peking University Medical Press: Beijing, China, 2005. [Google Scholar]
- Yang, Y.; Wang, Y.; Pan, X. China Food Composition 2009; Peking University Medical Press: Beijing, China, 2010. [Google Scholar]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sport. Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef]
- Ahmad, R.; Mok, A.; Rangan, A.M.; Louie, J.C.Y. Association of free sugar intake with blood pressure and obesity measures in Australian adults. Eur. J. Nutr. 2020, 59, 651–659. [Google Scholar] [CrossRef]
- de Ruyter, J.C.; Olthof, M.R.; Seidell, J.C.; Katan, M.B. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N. Engl. J. Med. 2012, 367, 1397–1406. [Google Scholar] [CrossRef]
- Johnson, R.J.; Sanchez-Lozada, L.G.; Andrews, P.; Lanaspa, M.A. Perspective: A Historical and Scientific Perspective of Sugar and Its Relation with Obesity and Diabetes. Adv. Nutr. 2017, 8, 412–422. [Google Scholar] [CrossRef]
- Rodriguez, L.A.; Madsen, K.A.; Cotterman, C.; Lustig, R.H. Added sugar intake and metabolic syndrome in US adolescents: Cross-sectional analysis of the National Health and Nutrition Examination Survey 2005–2012. Public Health Nutr. 2016, 19, 2424–2434. [Google Scholar] [CrossRef] [PubMed]
- Seo, E.H.; Kim, H.; Kwon, O. Association between Total Sugar Intake and Metabolic Syndrome in Middle-Aged Korean Men and Women. Nutrients 2019, 11, 2042. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Hu, F.B. Sugar-Sweetened Beverages and Cardiometabolic Health: An Update of the Evidence. Nutrients 2019, 11, 1840. [Google Scholar] [CrossRef]
- Azais-Braesco, V.; Sluik, D.; Maillot, M.; Kok, F.; Moreno, L.A. A review of total & added sugar intakes and dietary sources in Europe. Nutr. J. 2017, 16, 6. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Després, J.-P.; Hu, F.B. Sugar-Sweetened Beverages, Obesity, Type 2 Diabetes Mellitus, and Cardiovascular Disease Risk. Circulation 2010, 121, 1356–1364. [Google Scholar] [CrossRef]
- Das, U.N. Sucrose, fructose, glucose, and their link to metabolic syndrome and cancer. Nutrition 2015, 31, 249–257. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025; US Government Publishing Office: Washington, DC, USA, 2020.
- Chinese Nutrition Society. Chinese Dietary Guidelines; People’s Medical Publishing House Press: Beijing, China, 2022. [Google Scholar]
- Ma, Y.; He, F.J.; Yin, Y.; Hashem, K.M.; MacGregor, G.A. Gradual reduction of sugar in soft drinks without substitution as a strategy to reduce overweight, obesity, and type 2 diabetes: A modelling study. Lancet Diabetes Endocrinol. 2016, 4, 105–114. [Google Scholar] [CrossRef]
- Liu, S.; Munasinghe, L.L.; Ohinmaa, A.; Veugelers, P.J. Added, free and total sugar content and consumption of foods and beverages in Canada. Health Rep. 2020, 31, 14–24. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Z.; Du, W.; Huang, F.; Jiang, H.; Bai, J.; Zhang, X.; Zhang, B.; Wang, H. Twenty-Five-Year Trends in Dietary Patterns among Chinese Adults from 1991 to 2015. Nutrients 2021, 13, 1327. [Google Scholar] [CrossRef]
- Mullee, A.; Romaguera, D.; Pearson-Stuttard, J.; Viallon, V.; Stepien, M.; Freisling, H.; Fagherazzi, G.; Mancini, F.R.; Boutron-Ruault, M.C.; Kuhn, T.; et al. Association Between Soft Drink Consumption and Mortality in 10 European Countries. JAMA Intern. Med. 2019, 179, 1479–1490. [Google Scholar] [CrossRef]
- Jiang, Y.; Xu, T.; Dong, W.; Chu, C.; Zhou, M. Study on the death and disease burden caused by high sugar-sweetened beverages intake in China from 1990 to 2019. Eur. J. Public Health 2022, 32, 773–778. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).