Correlation between Mild Cognitive Impairment and Sarcopenia: The Prospective Role of Lipids and Basal Metabolic Rate in the Link
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sarcopenia Assessment
2.3. Cognitive Assessment
2.4. Dietary Assessment
2.5. Physical Activity Evaluation
2.6. Blood Sample Collection
2.7. Nontargeted Lipidomics
2.8. MRM Targeted Measurement
2.9. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics of Participants
3.2. Comparison of Dietary Consumption in Different Groups
3.3. Performance of BMR and Dietary Consumption on MoCA Score and Skeletal Muscle Index
3.4. The Role of Dietary Fats and BMR in the Relationship between MCI and SA
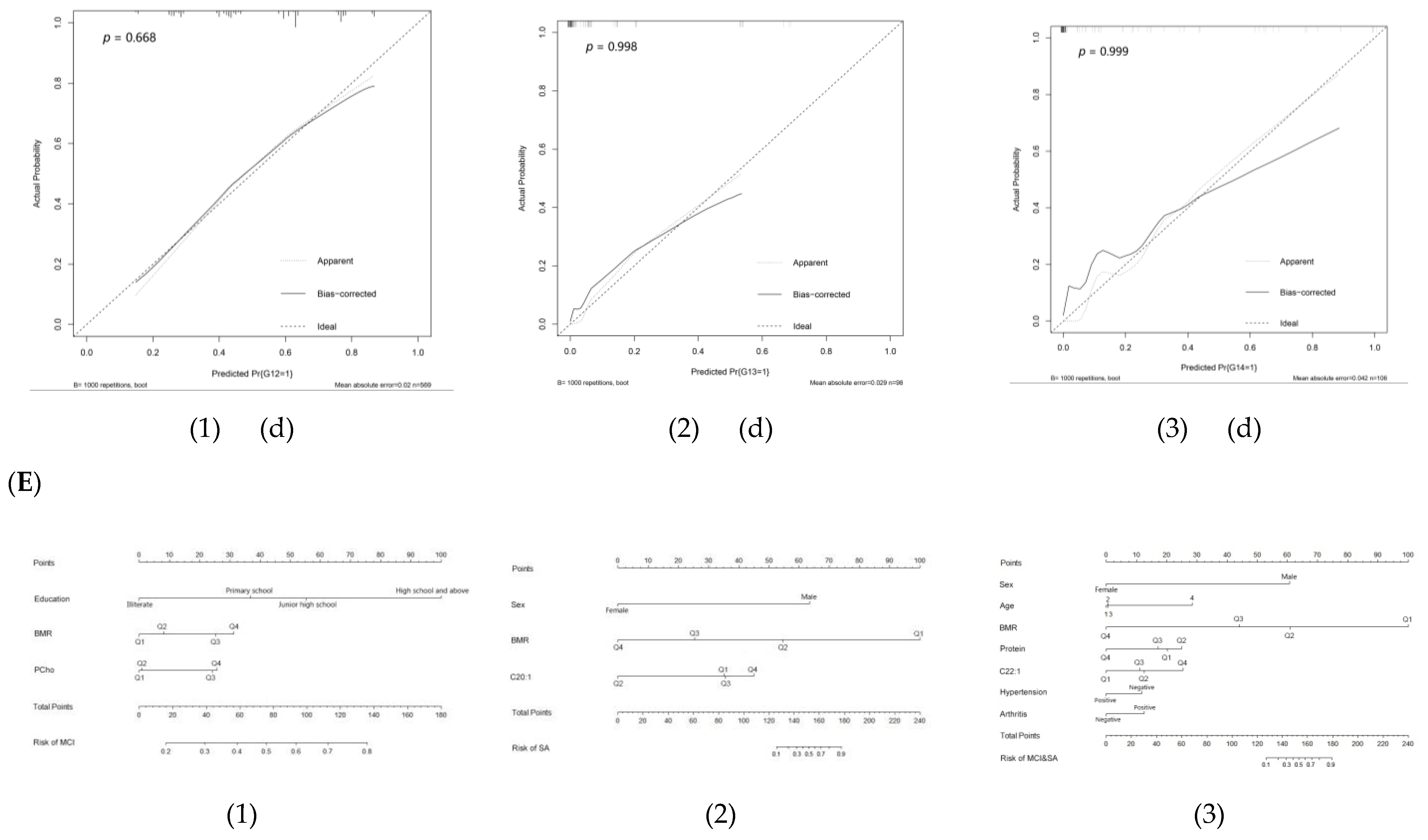
3.5. Nomogram for the Prediction Models of Multivariate Logistic Regression
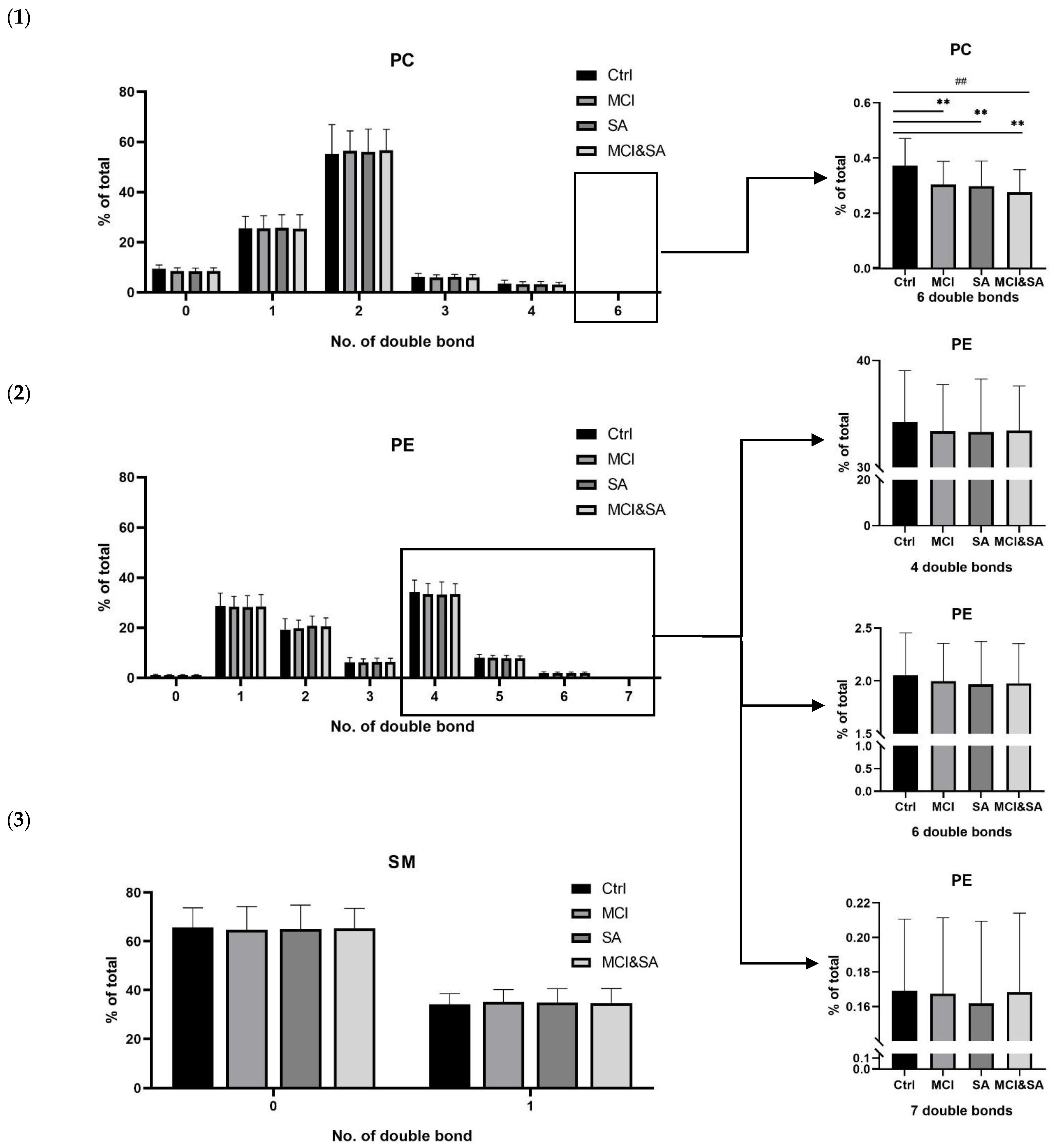
3.6. Nontargeted Lipidomics Analysis
3.7. MRM Targeted Measurement
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ogawa, Y.; Kaneko, Y.; Sato, T.; Shimizu, S.; Kanetaka, H.; Hanyu, H. Sarcopenia and Muscle Functions at Various Stages of Alzheimer Disease. Front. Neurol. 2018, 9, 710. [Google Scholar] [CrossRef]
- Liu, X.; Xia, X.; Hu, F.; Hou, L.; Jia, S.; Liu, Y.; Deng, L.; Zhang, Y.; Zhao, W.; Zhang, G.; et al. Nutrition status mediates the association between cognitive decline and sarcopenia. Aging 2021, 13, 8599–8610. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.H.; Kim, K.M.; Choi, S.H.; Lim, S.; Park, K.S.; Jang, H.C. Sarcopenia as a predictor of future cognitive impairment in older adults. J. Nutr. Health Aging 2016, 20, 496–502. [Google Scholar] [CrossRef] [PubMed]
- An, Y.; Zhang, X.; Wang, Y.; Wang, Y.; Liu, W.; Wang, T.; Qin, Z.; Xiao, R. Longitudinal and nonlinear relations of dietary and Serum cholesterol in midlife with cognitive decline: Results from EMCOA study. Mol. Neurodegener. 2019, 14, 51. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, Y.; Liu, W.; Wang, T.; Wang, L.; Hao, L.; Ju, M.; Xiao, R. Diet quality, gut microbiota, and microRNAs associated with mild cognitive impairment in middle-aged and elderly Chinese population. Am. J. Clin. Nutr. 2021, 114, 429–440. [Google Scholar] [CrossRef]
- Bhasin, S.; Travison, T.G.; Manini, T.M.; Patel, S.; Pencina, K.M.; Fielding, R.A.; Magaziner, J.M.; Newman, A.B.; Kiel, D.P.; Cooper, C.; et al. Sarcopenia Definition: The Position Statements of the Sarcopenia Definition and Outcomes Consortium. J. Am. Geriatr. Soc. 2020, 68, 1410–1418. [Google Scholar] [CrossRef]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar] [CrossRef]
- Dodds, R.M.; Murray, J.C.; Granic, A.; Hurst, C.; Uwimpuhwe, G.; Richardson, S.; Brayne, C.; Matthews, F.E.; Sayer, A.A.; Cfas, M. Prevalence and factors associated with poor performance in the 5-chair stand test: Findings from the Cognitive Function and Ageing Study II and proposed Newcastle protocol for use in the assessment of sarcopenia. J. Cachexia Sarcopenia Muscle 2021, 12, 308–318. [Google Scholar] [CrossRef]
- Kitamura, A.; Seino, S.; Abe, T.; Nofuji, Y.; Yokoyama, Y.; Amano, H.; Nishi, M.; Taniguchi, Y.; Narita, M.; Fujiwara, Y.; et al. Sarcopenia: Prevalence, associated factors, and the risk of mortality and disability in Japanese older adults. J. Cachex-Sarcopenia Muscle 2021, 12, 30–38. [Google Scholar] [CrossRef]
- Qin, H.; Zhu, B.; Hu, C.; Zhao, X. Later-Onset Hypertension Is Associated With Higher Risk of Dementia in Mild Cognitive Impairment. Front. Neurol. 2020, 11, 557977. [Google Scholar] [CrossRef]
- Wang, X.; Li, T.; Li, H.; Li, D.; Wang, X.; Zhao, A.; Liang, W.; Xiao, R.; Xi, Y. Association of Dietary Inflammatory Potential with Blood Inflammation: The Prospective Markers on Mild Cognitive Impairment. Nutrients 2022, 14, 2417. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Ma, G.; Zhai, F.; Li, Y.; Hu, Y.; Feskens, E.J.; Yang, X. Dietary Patterns and Glucose Tolerance Abnormalities in Chinese Adults. Diabetes Care 2009, 32, 1972–1976. [Google Scholar] [CrossRef]
- Ma, Y.; Shen, X.; Xu, W.; Huang, Y.; Li, H.; Tan, L.; Tan, C.; Dong, Q.; Tan, L.; Yu, J.; et al. A panel of blood lipids associated with cognitive performance, brain atrophy, and Alzheimer’s diagnosis: A longitudinal study of elders without dementia. Alzheimer’s Dementia Diagn. Assess. Dis. Monit. 2020, 12, e12041. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.A.; Smith, K.W.; Jette, A.M.; Janney, C.A. The physical activity scale for the elderly (PASE): Development and evaluation. J. Clin. Epidemiol. 1993, 46, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, T.; Ding, H.; Liu, Y.; Liu, X.; Yu, K.; Xiao, R.; Xi, Y. The role of dietary patterns and erythrocyte membrane fatty acid patterns on mild cognitive impairment. Front Nutr. 2022, 9, 1005857. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Li, C. A Predictive Model for the Risk of Cognitive Impairment in Patients with Gallstones. BioMed Res. Int. 2021, 2021, 3792407. [Google Scholar] [CrossRef]
- Wang, L.; Li, P.; Hou, M.; Zhang, X.; Cao, X.; Li, H. Construction of a risk prediction model for Alzheimer’s disease in the elderly population. BMC Neurol. 2021, 21, 271. [Google Scholar] [CrossRef]
- Zhou, J.; Lv, Y.; Mao, C.; Duan, J.; Gao, X.; Wang, J.; Yin, Z.; Shi, W.; Luo, J.; Kang, Q.; et al. Development and Validation of a Nomogram for Predicting the 6-Year Risk of Cognitive Impairment among Chinese Older Adults. J. Am. Med. Dir. Assoc. 2020, 21, 864–871. [Google Scholar] [CrossRef]
- Kim, H.-T.; Kim, H.; Ahn, H.-Y.; Hong, Y.-H. An analysis of age-related loss of skeletal muscle mass and its significance on osteoarthritis in a Korean population. Korean J. Intern. Med. 2016, 31, 585–593. [Google Scholar] [CrossRef]
- Roberts, S.; Collins, P.; Rattray, M. Identifying and Managing Malnutrition, Frailty and Sarcopenia in the Community: A Narrative Review. Nutrients 2021, 13, 2316. [Google Scholar] [CrossRef]
- Chang, K.-V.; Hsu, T.-H.; Wu, W.-T.; Huang, K.-C.; Han, D.-S. Association between Sarcopenia and Cognitive Impairment: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1164–1167. [Google Scholar] [CrossRef] [PubMed]
- Peng, T.-C.; Chen, W.-L.; Wu, L.-W.; Chang, Y.-W.; Kao, T.-W. Sarcopenia and cognitive impairment: A systematic review and meta-analysis. Clin. Nutr. 2020, 39, 2695–2701. [Google Scholar] [CrossRef] [PubMed]
- Sui, S.X.; Williams, L.J.; Holloway-Kew, K.L.; Hyde, N.K.; Anderson, K.B.; Tembo, M.C.; Addinsall, A.B.; Leach, S.; Pasco, J.A. Skeletal Muscle Density and Cognitive Function: A Cross-Sectional Study in Men. Calcif. Tissue Res. 2021, 108, 165–175. [Google Scholar] [CrossRef]
- Batsis, J.A.; Haudenschild, C.; Roth, R.M.; Gooding, T.L.; Roderka, M.N.; Masterson, T.; Brand, J.; Lohman, M.C.; Mackenzie, T.A. Incident Impaired Cognitive Function in Sarcopenic Obesity: Data From the National Health and Aging Trends Survey. J. Am. Med. Dir. Assoc. 2021, 22, 865–872. [Google Scholar] [CrossRef] [PubMed]
- Soysal, P.; Bulut, E.A.; Yavuz, I.; Isik, A.T. Decreased Basal Metabolic Rate Can Be an Objective Marker for Sarcopenia and Frailty in Older Males. J. Am. Med. Dir. Assoc. 2019, 20, 58–63. [Google Scholar] [CrossRef]
- Mateș, L.; Popa, D.-S.; Rusu, M.E.; Fizeșan, I.; Leucuța, D. Walnut Intake Interventions Targeting Biomarkers of Metabolic Syndrome and Inflammation in Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Antioxidants 2022, 11, 1412. [Google Scholar] [CrossRef] [PubMed]
- Lefèvre-Arbogast, S.; Hejblum, B.P.; Helmer, C.; Klose, C.; Manach, C.; Low, D.Y.; Urpi-Sarda, M.; Andres-Lacueva, C.; González-Domínguez, R.; Aigner, L.; et al. Early signature in the blood lipidome associated with subsequent cognitive decline in the elderly: A case-control analysis nested within the Three-City cohort study. eBioMedicine 2021, 64, 103216. [Google Scholar] [CrossRef] [PubMed]
- Marksteiner, J.; Oberacher, H.; Humpel, C. Acyl-Alkyl-Phosphatidlycholines are Decreased in Saliva of Patients with Alzheimer’s Disease as Identified by Targeted Metabolomics. J. Alzheimers Dis. 2019, 68, 583–589. [Google Scholar] [CrossRef]
- Simpson, B.N.; Kim, M.; Chuang, Y.-F.; Beason-Held, L.; Kitner-Triolo, M.; Kraut, M.; Lirette, S.T.; Windham, B.G.; Griswold, M.E.; Legido-Quigley, C.; et al. Blood metabolite markers of cognitive performance and brain function in aging. J. Cereb. Blood Flow Metab. 2016, 36, 1212–1223. [Google Scholar] [CrossRef]
- Yuki, D.; Sugiura, Y.; Zaima, N.; Akatsu, H.; Takei, S.; Yao, I.; Maesako, M.; Kinoshita, A.; Yamamoto, T.; Kon, R.; et al. DHA-PC and PSD-95 decrease after loss of synaptophysin and before neuronal loss in patients with Alzheimer’s disease. Sci. Rep. 2014, 4, 7130. [Google Scholar] [CrossRef]
- Whiley, L.; Sen, A.; Heaton, J.; Proitsi, P.; García-Gómez, D.; Leung, R.; Smith, N.; Thambisetty, M.; Kloszewska, I.; Mecocci, P.; et al. Evidence of altered phosphatidylcholine metabolism in Alzheimer’s disease. Neurobiol. Aging 2014, 35, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Proitsi, P.; Kim, M.; Whiley, L.; Simmons, A.; Sattlecker, M.; Velayudhan, L.; Lupton, M.K.; Soininen, H.; Kloszewska, I.; Mecocci, P.; et al. Association of blood lipids with Alzheimer’s disease: A comprehensive lipidomics analysis. Alzheimer’s Dement. 2017, 13, 140–151. [Google Scholar] [CrossRef]
- Proitsi, P.; Kim, M.; Whiley, L.; Pritchard, M.R.; Leung, R.; Soininen, H.; Kloszewska, I.; Mecocci, P.; Tsolaki, M.; Vellas, B.; et al. Plasma lipidomics analysis finds long chain cholesteryl esters to be associated with Alzheimer’s disease. Transl. Psychiatry 2015, 5, e494. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-M.; Lee, S.H.; Jung, Y.; Lee, Y.; Yoon, J.H.; Choi, J.Y.; Hwang, C.Y.; Son, Y.H.; Park, S.S.; Hwang, G.-S.; et al. FABP3-mediated membrane lipid saturation alters fluidity and induces ER stress in skeletal muscle with aging. Nat. Commun. 2020, 11, 5661. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-C.; Guo, Y.; Zhou, M.-M.; Xue, C.-H.; Chang, Y.-G.; Zhang, T.-T.; Wang, Y.-M. Comparative studies of DHA-enriched phosphatidylcholine and recombination of DHA-ethyl ester with egg phosphatidylcholine on ameliorating memory and cognitive deficiency in SAMP8 mice. Food Funct. 2019, 10, 938–950. [Google Scholar] [CrossRef] [PubMed]
- Tallima, H.; El Ridi, R. Arachidonic acid: Physiological roles and potential health benefits—A review. J. Adv. Res. 2018, 11, 33–41. [Google Scholar] [CrossRef]
- Blondelle, J.; Ohno, Y.; Gache, V.; Guyot, S.; Storck, S.; Blanchard-Gutton, N.; Barthélémy, I.; Walmsley, G.; Rahier, A.; Gadin, S.; et al. HACD1, a regulator of membrane composition and fluidity, promotes myoblast fusion and skeletal muscle growth. J. Mol. Cell Biol. 2015, 7, 429–440. [Google Scholar] [CrossRef]




| Total | Categories | p Value | ||||
|---|---|---|---|---|---|---|
| Ctrl | MCI | SA | MCI & SA | |||
| Demographic characteristics | ||||||
| N | 1050 | 440 | 490 | 41 | 79 | |
| Age | 70 (67, 73) | 70 (67, 72) a,b | 69 (67, 73) c,d | 72 (68, 78) a,c | 73 (69, 77) b,d | <0.001 ** |
| female, n (%) | 629 (59.9%) | 291 (66.1%) a | 275 (56.1%) a | 22 (53.7%) | 41 (51.9%) | 0.005 ** |
| Education | ||||||
| Illiterate n (%) | 234 (22.3%) | 144 (32.7%) a | 52 (10.6%) a,b,c | 21 (51.2%) b,d | 17 (21.5%) c,d | <0.001 ** |
| Primary school n (%) | 353 (33.6%) | 181 (41.1%) a,b | 140 (28.6%) a | 13 (31.7%) | 19 (24.1%) b | <0.001 ** |
| Junior high school n (%) | 376 (35.8%) | 81 (18.4%) a,b | 256 (52.2%) a,c | 5 (12.2%) c,d | 34 (43.0%) b,d | <0.001 ** |
| High school and above n (%) | 87 (8.3%) | 34 (7.7%) | 42 (8.6%) | 2 (4.9%) | 9 (11.4%) | <0.001 ** |
| BMI (kg/m2) | 25.9 (23.7, 28.2) | 26.7 (24.3, 28.9) a | 26.3 (24.1, 28.2) b | 21.6 (19.8, 23.6) a,b | 22.1 (20.4, 23.8) a,b | <0.001 ** |
| Emaciation n (%) | 14 (1.3%) | 2 (0.5%) a,b | 4 (0.8%) c | 2 (4,9%) a | 6 (7.6%) b,c | <0.001 ** |
| Normal n (%) | 278 (26.5%) | 90 (20.5%) a,b | 103 (21.0%) c,d | 30 (73.2%) a,c | 55 (69.6%) b,d | <0.001 ** |
| Overweight n (%) | 458 (43.6%) | 196 (44.5%) a,b | 237 (48.4%) c,d | 8 (19.5%) a,c | 17 (21.5%) b,d | <0.001 ** |
| Obesity n (%) | 300 (28.6%) | 152 (34.5%) a,b | 146 (29.8%) c,d | 1 (2.4%) a,c | 1 (1.3%) b,d | <0.001 ** |
| BMR (kcal) | 1258 (1153, 1387) | 1276 (1169, 1396) a,b | 1273 (1168, 1426) c,d | 1120 (1067, 1249) a,c | 1138 (1045, 1282) b,d | <0.001 ** |
| MoCA | 21 (17, 23) | 22 (20, 25) a,b,c | 19 (16, 22) a | 20 (15, 24) b,d | 18 (12, 21) c,d | <0.001 ** |
| Chronic diseases | ||||||
| Arthritis n (%) | 110 (11.6%) | 42 (10.4%) a | 49 (11.1%) b | 4 (11.4%) | 15 (22.7%) a,b | 0.034 * |
| Hypertension n (%) | 621 (65.6%) | 279 (69.1%) | 285 (64.5%) | 22 (62.9%) | 35 (53.0%) | 0.068 |
| Diabetes n (%) | 215 (22.7%) | 91 (22.5%) | 105 (23.8%) | 7 (20.0%) | 12 (18.2%) | 0.753 |
| Dyslipidemia n (%) | 352 (34.5%) | 151 (35.2%) | 165 (34.7%) | 9 (22.0%) | 27 (36.5%) | 0.379 |
| Serum Cholesterol | ||||||
| N | 1020 | 429 | 476 | 41 | 74 | |
| TC (mmol/L) | 4.659 ± 0.975 | 4.690 (3.970, 5.290) | 4.565 (3.943, 5.228) | 4.610 (4.035, 5.100) | 4.825 (4.068, 5.493) | 0.284 |
| TAG (mmol/L) | 1.310 (0.940, 1.868) | 1.340 (0.990, 1.915) | 1.320 (0.943, 1.865) | 1.040 (0.770, 1.490) | 1.160 (0.875, 1.595) | 0.014 * |
| HDL-C (mmol/L) | 1.250 (1.070, 1.450) | 1.250 (1.090, 1.450) | 1.240 (1.050, 1.430) | 1.300 (1.095, 1.590) | 1.230 (1.018, 1.603) | 0.207 |
| LDL-C (mmol/L) | 3.007 ± 0.893 | 3.005 ± 0.910 | 2.972 ± 0.881 | 3.076 ± 0.730 | 3.209 ± 0.939 | 0.189 |
| Dietary intakes | ||||||
| N | 975 | 407 | 457 | 35 | 76 | |
| Energy (kcal/d) | 1781 (1424, 2155) | 1841 (1467, 2208) | 1750 (1364, 2128) | 1925 (1574, 2345) | 1741 (1365, 2044) | 0.031 * |
| Protein (g/d) | 59.0 (44.0, 75.2) | 61.6 (47.5, 79.2) a,b | 58.1 (41.9, 72.1) a | 65.5 (40.2, 86.8) c | 52.5 (37.5, 65.3) b,c | <0.001 ** |
| CHO (g/d) | 202.0 (155.0, 264.8) | 211.3 (159.4, 285.1) a | 197.7 (152.4, 253.5) a | 204.1 (156.6, 271.8) | 185.8 (148.4, 241.8) | 0.015 * |
| Fat (g/d) | 75.8 (58.1, 95.6) | 75.7 (59.9, 96.8) | 75.3 (57.4, 94.1) | 92.9 (72.8, 107.2) | 79.1 (53.0, 100.4) | 0.069 |
| Cholesterol (mg/d) | 333.3 (204.5, 397.5) | 347.5 (225.7, 405.0) | 329.8 (192.3, 390.7) | 361.7 (294.2, 450.4) a | 298.4 (146.9, 373.9) a | 0.004 ** |
| PC (mg/d) | 82.610 (59.586, 101.892) | 85.472 (62.950, 106.057) a | 80.987 (58.946, 100.311) | 86.742 (75.755, 107.382) b | 69.074 (45.724, 95.031) a,b | 0.001 ** |
| SM (mg/d) | 4.136 (2.917, 5.536) | 4.356 (3.020, 5.876) a | 3.969 (2.889, 5.403) | 4.780 (3.437, 5.733) | 3.417 (2.313, 5.248) a | 0.003 ** |
| Total fatty acid (g/d) | 68.677 (53.198, 87.310) | 68.253 (53.575, 87.361) | 68.222 (52.203, 86.382) | 85.462 (66.905, 99.918) | 72.251 (47.977, 91.911) | 0.061 |
| SFA (g/d) | 19.029 (13.081, 24.502) | 19.013 (13.698, 25.468) | 18.730 (12.988, 23.976) | 21.590 (14.421, 29.010) | 18.308 (12.175, 23.532) | 0.027 * |
| MUFA (g/d) | 13.168 (9.404, 17.986) | 13.641 (10.290, 18.947) a | 13.014 (8.776, 17.355) | 15.523 (10.026, 20.032) | 11.160 (8.146, 15.677) a | 0.001 ** |
| PUFA (g/d) | 4.908 (3.164, 7.836) | 5.154 (3.376, 8.022) a | 4.874 (3.078, 7.797) b | 6.268 (3.732, 8.734) c | 3.776 (2.392, 6.318) a,b,c | 0.001 ** |
| Betaine (mg/d) | 110.0 (78.2, 157.8) | 121.7 (84.0, 168.1) a,b | 107.3 (78.9, 145.8) a | 108.5 (66.5, 139.2) | 86.5 (64.4, 142.1) b | <0.001 ** |
| GPC (mg/d) | 7.769 (5.656, 10.420) | 8.142 (6.057, 11.190) a | 7.737 (5.596, 10.164) b | 6.972 (5.381, 10.278) | 6.251 (4.622, 9.184) a,b | <0.001 ** |
| Phosphatidylcholine (mg/d) | 2.450 (1.685, 3.297) | 2.627 (1.848, 3.391) a,b | 2.381 (1.681, 3.237) a,c | 2.674 (1.714, 3.615) | 1.848 (1.337, 2.901) b,c | <0.001 ** |
| Model1 | Model2 | |||||||
|---|---|---|---|---|---|---|---|---|
| MoCA | SMI | MoCA | SMI | |||||
| B | p Value | B | p Value | B | p Value | B | p Value | |
| BMR (kcal) | 0.004 | 0.002 ** | 0.005 | 0.007 ** | 0.002 | <0.001 ** | 0.002 | <0.001 ** |
| BMR (kcal) | 0.004 | 0.018 * | 0.002 | <0.001 ** | 0.004 | 0.015 * | 0.002 | <0.001 ** |
| Energy (kcal/d) | 0.001 | 0.002 ** | −0.000 | 0.095 | 0.001 | 0.039 * | −0.000 | 0.040 * |
| BMR (kcal) | 0.003 | 0.030 * | 0.002 | <0.001 ** | 0.003 | 0.043 * | 0.002 | <0.001 ** |
| Protein (g/d) | 0.037 | 0.001 ** | 0.002 | 0.008 ** | 0.044 | 0.001 ** | 0.002 | 0.138 |
| CHO (g/d) | −0.001 | 0.672 | −0.000 | 0.040 * | −0.002 | 0.593 | −0.000 | 0.314 |
| Fat (g/d) | −0.013 | 0.032 * | −0.002 | 0.001 ** | −0.022 | 0.004 ** | −0.002 | 0.001 ** |
| BMR (kcal) | 0.004 | 0.012 * | 0.002 | <0.001 ** | 0.004 | 0.017 * | 0.002 | <0.001 ** |
| Cholesterol (mg/d) | 0.002 | 0.014 * | −0.000 | 0.544 | 0.003 | 0.012 * | −0.000 | 0.332 |
| BMR (kcal/d) | 0.004 | 0.018 * | 0.002 | <0.001 ** | 0.004 | 0.021 * | 0.002 | <0.001 ** |
| PC (mg/d) | 0.012 | 0.002 ** | −0.000 | 0.753 | 0.014 | 0.002 * | −0.000 | 0.292 |
| BMR (kcal) | 0.004 | 0.014 * | 0.002 | <0.001 ** | 0.004 | 0.016 * | 0.002 | <0.001 ** |
| SM (mg/d) | 0.140 | 0.019 * | 0.000 | 0.978 | 0.156 | 0.023 * | −0.007 | 0.238 |
| BMR (kcal) | 0.004 | 0.009 ** | 0.002 | <0.001 ** | 0.004 | 0.010 * | 0.002 | <0.001 ** |
| Total fatty acid (g/d) | 0.003 | 0.600 | −0.001 | 0.019 * | −0.002 | 0.746 | −0.002 | 0.003 * |
| BMR (kcal) | 0.004 | 0.013 * | 0.002 | <0.001 ** | 0.004 | 0.015 * | 0.002 | <0.001 ** |
| SFA (g/d) | 0.038 | 0.034 * | −0.001 | 0.489 | 0.032 | 0.126 | −0.003 | 0.094 |
| BMR (kcal) | 0.003 | 0.023 * | 0.002 | <0.001 ** | 0.004 | 0.025 * | 0.002 | <0.001 ** |
| MUFA (g/d) | 0.077 | <0.001 ** | 0.001 | 0.503 | 0.077 | 0.002 ** | −0.001 | 0.668 |
| BMR (kcal) | 0.003 | 0.020 * | 0.002 | <0.001 ** | 0.004 | 0.023 * | 0.002 | <0.001 ** |
| PUFA (g/d) | 0.106 | 0.001 ** | 0.002 | 0.58 | 0.095 | 0.012 * | 0.000 | 0.970 |
| BMR (kcal) | 0.003 | 0.019 * | 0.002 | <0.001 ** | 0.004 | 0.018 * | 0.002 | <0.001 ** |
| Betaine (mg/d) | 0.008 | <0.001 ** | −0.000 | 0.983 | 0.008 | 0.001 ** | −0.000 | 0.604 |
| BMR (kcal) | 0.004 | 0.020 * | 0.002 | <0.001 ** | 0.004 | 0.019 * | 0.002 | <0.001 ** |
| GPC (mg/d) | 0.091 | 0.007 ** | 0.003 | 0.333 | 0.100 | 0.010 * | −0.002 | 0.621 |
| BMR (kcal) | 0.003 | 0.046 * | 0.002 | <0.001 ** | 0.004 | 0.030 * | 0.002 | <0.001 ** |
| Phosphatidylcholine (mg/d) | 0.549 | <0.001 ** | −0.000 | 0.987 | 0.466 | 0.001 ** | −0.006 | 0.599 |
| BMR (kcal) | 0.001 | 0.423 | -- | -- | 0.002 | 0.299 | -- | -- |
| SMI (kg) | 1.282 | 0.001 ** | -- | -- | 1.153 | 0.015* | -- | -- |
| BMR (kcal) | -- | -- | 0.002 | <0.001 ** | -- | -- | 0.002 | <0.001 ** |
| MoCA | -- | -- | 0.009 | 0.001 ** | -- | -- | 0.008 | 0.018 * |
| Q1 | Q2 | Q3 | Q4 | p Value | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | p Value | OR (95%CI) | p Value | OR (95%CI) | p Value | |||
| MCI vs. Ctrl a | ||||||||
| BMR (kcal) | Ref | 1.175 (0.745, 1.852) | 0.488 | 0.580 (0.364, 0.923) | 0.022 * | 0.671 (0.421, 1.07) | 0.094 | 0.008 ** |
| Phosphatidylcholine (mg/d) | Ref | 0.978 (0.624, 1.534) | 0.922 | 0.552 (0.354, 0.860) | 0.009 ** | 0.569 (0.364, 0.890) | 0.013* | 0.006 ** |
| SA vs. Ctrl a | ||||||||
| BMR (kcal) | Ref | 0.021 (0.002 0.242) | <0.001 ** | 0.002 (0.000, 0.027) | <0.001 ** | <0.001 (0.000, 0.005) | <0.001 ** | <0.001 ** |
| C20:1 (g/d) | Ref | 0.051 (0.004, 0.608) | 0.019 * | 1.075 (0.321, 3.606) | 0.907 | 2.293 (0.767, 6.854) | 0.137 | 0.017 * |
| MCI and SA vs. Ctrl a | ||||||||
| BMR (kcal) | Ref | 0.038 (0.008,0.184) | <0.001 ** | 0.009 (0.001,0.059) | <0.001 ** | <0.001 (0,0.003) | <0.001 ** | <0.001 ** |
| Protein (g/d) | Ref | 1.538 (0.608,3.891) | 0.363 | 0.794 (0.306,2.065) | 0.637 | 0.185 (0.053,0.653) | 0.009 ** | 0.011 * |
| C22:1 (g/d) | Ref | 2.905 (0.916,9.215) | 0.070 | 2.543 (0.716,9.028) | 0.149 | 8.249 (2.545,26.733) | <0.001 ** | 0.003 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Xiao, R.; Li, H.; Li, T.; Guan, L.; Ding, H.; Li, X.; Zheng, H.; Yu, K.; Zhao, A.; et al. Correlation between Mild Cognitive Impairment and Sarcopenia: The Prospective Role of Lipids and Basal Metabolic Rate in the Link. Nutrients 2022, 14, 5321. https://doi.org/10.3390/nu14245321
Wang X, Xiao R, Li H, Li T, Guan L, Ding H, Li X, Zheng H, Yu K, Zhao A, et al. Correlation between Mild Cognitive Impairment and Sarcopenia: The Prospective Role of Lipids and Basal Metabolic Rate in the Link. Nutrients. 2022; 14(24):5321. https://doi.org/10.3390/nu14245321
Chicago/Turabian StyleWang, Xuan, Rong Xiao, Hongrui Li, Tiantian Li, Lizheng Guan, Huini Ding, Xiaoying Li, Huaguang Zheng, Kang Yu, Ai Zhao, and et al. 2022. "Correlation between Mild Cognitive Impairment and Sarcopenia: The Prospective Role of Lipids and Basal Metabolic Rate in the Link" Nutrients 14, no. 24: 5321. https://doi.org/10.3390/nu14245321
APA StyleWang, X., Xiao, R., Li, H., Li, T., Guan, L., Ding, H., Li, X., Zheng, H., Yu, K., Zhao, A., Liang, W., & Xi, Y. (2022). Correlation between Mild Cognitive Impairment and Sarcopenia: The Prospective Role of Lipids and Basal Metabolic Rate in the Link. Nutrients, 14(24), 5321. https://doi.org/10.3390/nu14245321






