Vitamin D Supplementation Has No Impact on Cardiorespiratory Fitness, but Improves Inflammatory Status in Vitamin D Deficient Young Men Engaged in Resistance Training
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. General Organization of the Study
2.3. Resistance Training and Dietary Supplementation
2.4. Measurement of Maximal Oxygen Uptake
2.5. Blood Sampling and Analyses
2.6. Statistical Analysis
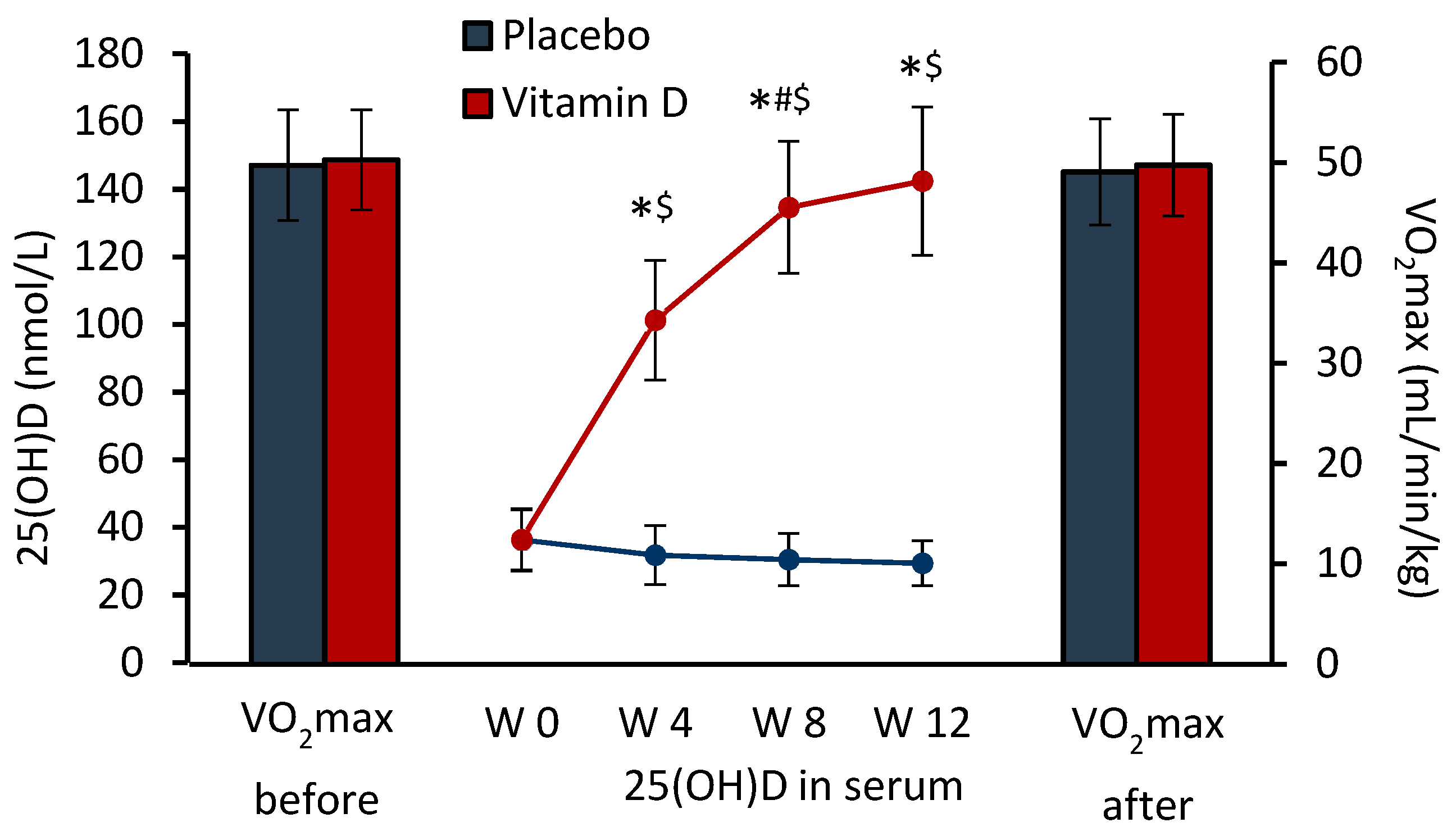
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DeLuca, H.F. Overview of general physiologic features and functions of vitamin D. Am. J. Clin. Nutr. 2004, 80, 1689S–1696S. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D.D. Vitamin D metabolism, mechanism of action, and clinical applications. Chem. Biol. 2014, 21, 319–329. [Google Scholar] [CrossRef]
- Christakos, S.; Dhawan, P.; Verstuyf, A.; Verlinden, L.; Carmeliet, G. Vitamin D: Metabolism, molecular mechanism of action, and pleiotropic effects. Physiol. Rev. 2016, 96, 365–408. [Google Scholar] [CrossRef] [PubMed]
- Zittermann, A. Vitamin D in preventive medicine: Are we ignoring the evidence? Br. J. Nutr. 2003, 89, 552–572. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Medical progress: Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Norman, A.W. From vitamin D to hormone D: Fundamentals of the vitamin D endocrine system essential for good health. Am. J. Clin. Nutr. 2008, 88, 491S–499S. [Google Scholar] [CrossRef]
- Boland, R.L. VDR activation of intracellular signaling pathways in skeletal muscle. Mol. Cell Endocrinol. 2011, 347, 11–16. [Google Scholar] [CrossRef]
- Girgis, C.M. Vitamin D and skeletal muscle: Emerging roles in development, anabolism and repair. Calcif. Tissue Int. 2020, 106, 47–57. [Google Scholar] [CrossRef]
- Lim, K.; Molostvov, G.; Lubczanska, M.; Fletcher, S.; Bland, R.; Hiemstra, T.F.; Zehnder, D. Impaired arterial vitamin D signaling occurs in the development of vascular calcification. PLoS ONE 2020, 15, e0241976. [Google Scholar] [CrossRef]
- Menezes, R.J.; Cheney, R.T.; Husain, A.; Tretiakova, M.; Loewen, G.; Johnson, C.S.; Jayaprakash, V.; Moysich, K.B.; Salgia, R.; Reid, M.E. Vitamin D receptor expression in normal, premalignant, and malignant human lung tissue. Cancer Epidemiol. Biomarkers Prev. 2008, 17, 1104–1110. [Google Scholar] [CrossRef]
- O’Connell, T.D.; Simpson, R.U. Immunochemical identification of the 1,25-dihydroxyvitamin D3 receptor protein in human heart. Cell Biol. Int. 1996, 20, 621–624. [Google Scholar] [CrossRef] [PubMed]
- Bishop, E.L.; Ismailova, A.; Dimeloe, S.; Hewison, M.; White, J.H. Vitamin D and immune regulation: Antibacterial, antiviral, anti-inflammatory. JBMR Plus 2021, 5, e10405. [Google Scholar] [CrossRef] [PubMed]
- Heyward, V.H. Advanced Fitness Assessment and Exercise Prescription, 6th ed.; Human Kinetics: Champaign, IL, USA, 2010; pp. 65–101. [Google Scholar]
- Kenney, W.L.; Wilmore, J.H.; Costill, D.L. Physiology of Sport and Exercise, 6th ed.; Human Kinetics: Champaign, IL, USA, 2015; pp. 262–284. [Google Scholar]
- Smith, E.M.; Tangpricha, V. Vitamin D and anemia: Insights into an emerging association. Curr. Opin. Endocrinol. Diabetes Obes. 2015, 22, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Dahlquist, D.T.; Dieter, B.P.; Koehle, M.S. Plausible ergogenic effects of vitamin D on athletic performance and recovery. J. Int. Soc. Sports Nutr. 2015, 12, 33. [Google Scholar] [CrossRef] [PubMed]
- Ardestani, A.; Parker, B.; Mathur, S.; Clarkson, P.; Pescatello, L.S.; Hoffman, H.J.; Polk, D.M.; Thompson, P.D. Relation of vitamin D level to maximal oxygen uptake in adults. Am. J. Cardiol. 2011, 107, 1246–1249. [Google Scholar] [CrossRef]
- Marawan, A.; Kurbanova, N.; Qayyum, R. Association between serum vitamin D levels and cardiorespiratory fitness in the adult population of the USA. Eur. J. Prev. Cardiol. 2019, 26, 750–755. [Google Scholar] [CrossRef]
- Carson, E.L.; Pourshahidi, L.K.; Hill, T.R.; Cashman, K.D.; Strain, J.J.; Boreham, C.A.; Mulhern, M.S. Vitamin D, muscle function, and cardiorespiratory fitness in adolescents from the young hearts study. J. Clin. Endocrinol. Metab. 2015, 100, 4621–4628. [Google Scholar] [CrossRef]
- Valtueña, J.; Gracia-Marco, L.; Huybrechts, I.; Breidenassel, C.; Ferrari, M.; Gottrand, F.; Dallongeville, J.; Sioen, I.; Gutierrez, A.; Kersting, M.; et al. Cardiorespiratory fitness in males, and upper limbs muscular strength in females, are positively related with 25-hydroxyvitamin D plasma concentrations in European adolescents: The HELENA study. Q. J. Med. 2013, 106, 809–821. [Google Scholar] [CrossRef]
- Karefylakis, C.; Särnblad, S.; Ariander, A.; Ehlersson, G.; Rask, E.; Rask, P. Effect of vitamin D supplementation on body composition and cardiorespiratory fitness in overweight men—A randomized controlled trial. Endocrine 2018, 61, 388–397. [Google Scholar] [CrossRef]
- Carrillo, A.E.; Flynn, M.G.; Pinkston, C.; Markofski, M.M.; Jiang, Y.; Donkin, S.S.; Teegarden, D. Impact of vitamin D supplementation during a resistance training intervention on body composition, muscle function, and glucose tolerance in overweight and obese adults. Clin. Nutr. 2013, 32, 375–381. [Google Scholar] [CrossRef]
- Todd, J.J.; McSorley, E.M.; Pourshahidi, L.K.; Madigan, S.M.; Laird, E.; Healy, M.; Magee, P.J. Vitamin D3 supplementation using an oral spray solution resolves deficiency but has no effect on VO2 max in Gaelic footballers: Results from a randomised, double-blind, placebo-controlled trial. Eur. J. Nutr. 2017, 56, 1577–1587. [Google Scholar] [CrossRef]
- Michalczyk, M.M.; Gołas, A.; Maszczyk, A.; Kaczka, P.; Zaja, A. Influence of sunlight and oral D3 supplementation on serum 25(OH)D concentration and exercise performance in elite soccer players. Nutrients 2020, 12, 1311. [Google Scholar] [CrossRef]
- Scholten, S.D.; Sergeev, I.N.; Song, Q.; Birger, C.B. Effects of vitamin D and quercetin, alone and in combination, on cardiorespiratory fitness and muscle function in physically active male adults. Open Access J. Sports Med. 2015, 6, 229–239. [Google Scholar] [CrossRef]
- Menon, A.S.; Anayath, S.; Garg, M.K.; Ravi, K.; Pisharody, I. The effect of vitamin D supplementation on cardiorespiratory fitness and muscle strength in male adults undergoing basic military training. Med. J. Armed Forces India 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Jastrzębska, M.; Kaczmarczyk, M.; Michalczyk, M.; Radzimiński, L.; Stępień, P.; Jastrzębska, J.; Wakuluk, D.; Suárez, A.D.; Lopez Sánchez, G.F.; Cieszczyk, P.; et al. Can supplementation of vitamin D improve aerobic capacity in well trained youth soccer players? J. Hum. Kinet. 2018, 61, 63–72. [Google Scholar] [CrossRef]
- Ramezani Ahmadi, A.; Mohammadshahi, M.; Alizadeh, A.; Ahmadi Angali, K.; Jahanshahi, A. Effects of vitamin D3 supplementation for 12 weeks on serum levels of anabolic hormones, anaerobic power, and aerobic performance in active male subjects: A randomized, double-blind, placebo-controlled trial. Eur. J. Sport Sci. 2020, 20, 1355–1367. [Google Scholar] [CrossRef]
- Kujach, S.; Lyzwinski, D.; Chroboczek, M.; Bialowas, D.; Antosiewicz, J.; Laskowski, R. The effect of vitamin D3 supplementation on physical capacity among active college-aged males. Nutrients 2020, 12, 1936. [Google Scholar] [CrossRef]
- Ladenvall, P.; Persson, C.U.; Mandalenakis, Z.; Wilhelmsen, L.; Grimby, G.; Svärdsudd, K.; Hansson, P.-O. Low aerobic capacity in middle-aged men associated with increased mortality rates during 45 years of follow-up. Eur. J. Prev. Cardiol. 2016, 23, 1557–1564. [Google Scholar] [CrossRef]
- Salier Eriksson, J.; Ekblom, B.; Andersson, G.; Wallin, P.; Ekblom-Bak, E. Scaling VO2max to body size differences to evaluate associations to CVD incidence and all-cause mortality risk. BMJ Open Sport Exerc. Med. 2021, 7, e000854. [Google Scholar] [CrossRef]
- Willerson, J.T.; Ridker, P.M. Inflammation as a cardiovascular risk factor. Circulation 2004, 109 (Suppl. SII), II-2–II-10. [Google Scholar] [CrossRef]
- Hansson, G.K. Mechanisms of disease: Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 2005, 352, 1685–1695. [Google Scholar] [CrossRef] [PubMed]
- Izzo, M.; Carrizzo, A.; Izzo, C.; Cappello, E.; Cecere, D.; Ciccarelli, M.; Iannece, P.; Damato, A.; Vecchione, C.; Pompeo, F. Vitamin D: Not just bone metabolism but a key player in cardiovascular diseases. Life 2021, 11, 452. [Google Scholar] [CrossRef] [PubMed]
- Cannell, J.J.; Grant, W.B.; Holick, M.F. Vitamin D and inflammation. Dermatoendocrinol. 2014, 6, e983401. [Google Scholar] [CrossRef] [PubMed]
- Colotta, F.; Jansson, B.; Bonelli, F. Modulation of inflammatory and immune responses by vitamin D. J. Autoimmun. 2017, 85, 78–97. [Google Scholar] [CrossRef] [PubMed]
- Giraldo, D.M.; Cardona, A.; Urcuqui-Inchima, S. High-dose of vitamin D supplement is associated with reduced susceptibility of monocyte-derived macrophages to dengue virus infection and proinflammatory cytokine production: An exploratory study. Clin. Chim. Acta 2018, 478, 140–151. [Google Scholar] [CrossRef]
- Stubbs, J.R.; Idiculla, A.; Slusser, J.; Menard, R.; Quarles, L.D. Cholecalciferol supplementation alters calcitriol-responsive monocyte proteins and decreases inflammatory cytokines in ESRD. J. Am. Soc. Nephrol. 2010, 21, 353–361. [Google Scholar] [CrossRef]
- Dadrass, A.; Salamat, K.M.; Hamidi, K.; Azizbeigi, K. Anti-inflammatory effects of vitamin D and resistance training in men with type 2 diabetes mellitus and vitamin D deficiency: A randomized, double-blinded, placebo-controlled clinical trial. J. Diabetes Metab. Disord. 2019, 18, 323–331. [Google Scholar] [CrossRef]
- Eslami, P.; Hekmat, M.; Beheshti, M.; Baghaei, R.; Mirhosseini, S.M.; Pourmotahari, F.; Ziai, S.A.; Foroughi, M. A randomized, double-blind, placebo-controlled, clinical trial of high-dose, short-term vitamin D administration in the prevention of acute kidney injury after cardiac surgery. Cardiorenal Med. 2021, 11, 52–58. [Google Scholar] [CrossRef]
- Silva, B.S.A.; Lira, F.S.; Rossi, F.E.; Ramos, D.; Uzeloto, J.S.; Freire, A.P.C.F.; de Lima, F.F.; Gobbo, L.A.; Ramos, E.M.C. Inflammatory and metabolic responses to different resistance training on chronic obstructive pulmonary disease: A randomized control trial. Front. Physiol. 2018, 9, 262. [Google Scholar] [CrossRef]
- Silveira Martins, M.; Farinha, J.B.; Benetti, C.B.; Courtes, A.A.; Duarte, T.; Nunes da Silva, J.C.; Duarte, M.M.M.F.; Soares, F.A.A.; dos Santos, D.L. Positive effects of resistance training on inflammatory parameters in men with metabolic syndrome risk factors. Nutr. Hosp. 2015, 32, 792–798. [Google Scholar] [CrossRef]
- Miller, E.G.; Nowson, C.A.; Dunstan, D.W.; Kerr, D.A.; Menzies, D.; Daly, R.M. Effects of whey protein plus vitamin D supplementation combined with progressive resistance training on glycaemic control, body composition, muscle function and cardiometabolic risk factors in middle-aged and older overweight/obese adults with type 2 diabetes: A 24-week randomized controlled trial. Diabetes Obes. Metab. 2021, 23, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Forti, L.N.; Van Roie, E.; Njemini, R.; Coudyzer, W.; Beyer, I.; Delecluse, C.; Bautmans, I. Effects of resistance training at different loads on inflammatory markers in young adults. Eur. J. Appl. Physiol. 2017, 117, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Ihalainen, J.K.; Peltonen, H.; Paulsen, G.; Ahtiainen, J.P.; Taipale, R.S.; Hämäläinen, M.; Moilanen, E.; Mero, A.A. Inflammation status of healthy young men: Initial and specific responses to resistance training. Appl. Physiol. Nutr. Metab. 2018, 43, 252–258. [Google Scholar] [CrossRef]
- Savolainen, L.; Timpmann, S.; Mooses, M.; Mäestu, E.; Medijainen, L.; Tõnutare, L.; Ross, F.; Lellsaar, M.; Unt, E.; Ööpik, V. Vitamin D supplementation does not enhance resistance training-induced gains in muscle strength and lean body mass in vitamin D deficient young men. Eur. J. Appl. Physiol. 2021, 121, 2077–2090. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Trummer, C.; Pandis, M.; Verheyen, N.; Grübler, M.R.; Gaksch, M.; Obermayer-Pietsch, B.; Tomaschitz, A.; Pieber, T.R.; Pilz, S.; Schwetz, V. Beneficial effects of UV-radiation: Vitamin D and beyond. Int. J. Environ. Res. Public Health 2016, 13, 1028. [Google Scholar] [CrossRef]
- Ööpik, V.; Timpmann, S.; Rips, L.; Olveti, I.; Kõiv, K.; Mooses, M.; Mölder, M.H.; Varblane, M.A.; Lille, H.-R.; Gapeyeva, H. Anabolic adaptations occur in conscripts during basic military training despite high prevalence of vitamin D deficiency and decrease in iron status. Mil. Med. 2017, 182, e1810. [Google Scholar] [CrossRef]
- Levinger, I.; Goodman, C.; Hare, D.L.; Jerums, G.; Toia, D.; Selig, S. The reliability of the 1RM strength test for untrained middle-aged individuals. J. Sci. Med. Sport 2009, 12, 310–316. [Google Scholar] [CrossRef]
- Pludowski, P.; Holick, M.F.; Grant, W.B.; Konstantynowicz, J.; Mascarenhas, M.R.; Haq, A.; Povoroznyuk, V.; Balatska, N.; Barbosa, A.P.; Karonova, T.; et al. Vitamin D supplementation guidelines. J. Steroid Biochem. Mol. Biol. 2018, 175, 125–135. [Google Scholar] [CrossRef]
- Damas, F.; Phillips, S.M.; Libardi, C.A.; Vechin, F.C.; Lixandrão, M.E.; Jannig, P.R.; Costa, L.A.R.; Bacurau, A.V.; Snijders, T.; Parise, G.; et al. Resistance training-induced changes in integrated myofibrillar protein synthesis are related to hypertrophy only after attenuation of muscle damage. J. Physiol. 2016, 594, 5209–5222. [Google Scholar] [CrossRef]
- Davis, J.A. Direct determination of aerobic power. In Physiological Assessment of Human Fitness, 2nd ed.; Maud, P.J., Foster, C., Eds.; Human Kinetics: Champaign, IL, USA, 2006; pp. 9–18. [Google Scholar]
- Vogeser, M.; König, D.; Frey, I.; Predel, H.G.; Parhofer, K.G.; Berg, A. Fasting serum insulin and the homeostasis model of insulin resistance (HOMA-IR) in the monitoring of lifestyle interventions in obese persons. Clin. Biochem. 2007, 40, 964–968. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analyses for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates Publishers: New York, NY, USA, 1988; pp. 179–213. [Google Scholar]
- Stockton, K.A.; Mengersen, K.; Paratz, J.D.; Kandiah, D.; Bennell, K.L. Effect of vitamin D supplementation on muscle strength: A systematic review and meta-analysis. Osteoporos. Int. 2011, 22, 859–871. [Google Scholar] [CrossRef]
- Martineau, A.R.; Jolliffe, D.A.; Hooper, R.L.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ 2017, 356, i6583. [Google Scholar] [CrossRef]
- Nevill, A.; Brown, D.; Godfrey, R.; Johnson, P.; Romer, L.; Stewart, A.D.; Winter, E.M. Modeling maximum oxygen uptake of elite endurance athletes. Med. Sci. Sports Exerc. 2003, 35, 488–494. [Google Scholar] [CrossRef]
- Ozaki, H.; Loenneke, J.P.; Thiebaud, R.S.; Abe, T. Resistance training induced increase in VO2max in young and older subjects. Eur. Rev. Aging Phys. Act. 2013, 10, 107–116. [Google Scholar] [CrossRef]
- Knuiman, P.; van Loon, L.J.C.; Wouters, J.; Hopman, M.; Mensink, M. Protein supplementation elicits greater gains in maximal oxygen uptake capacity and stimulates lean mass accretion during prolonged endurance training: A double-blind randomized controlled trial. Am. J. Clin. Nutr. 2019, 110, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.M.; Alvarez, J.A.; Martin, G.S.; Zughaier, S.M.; Ziegler, T.R.; Tangpricha, V. Vitamin D deficiency is associated with anaemia among African Americans in a US cohort. Br. J. Nutr. 2015, 113, 1732–1740. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.E.; Guillet, R.; Queenan, R.A.; Cooper, E.M.; Kent, T.R.; Pressman, E.K.; Vermeylen, F.M.; Roberson, M.S.; O’Brien, K. Vitamin D status is inversely associated with anemia and serum erythropoietin during pregnancy. Am. J. Clin. Nutr. 2015, 102, 1088–1095. [Google Scholar] [CrossRef]
- Most, A.; Dörr, O.; Nef, H.; Hamm, C.; Bauer, T.; Bauer, P. Influence of 25-hydroxy-vitamin D insufficiency on maximal aerobic power in elite indoor athletes: A cross-sectional study. Sports Med. Open. 2021, 7, 74. [Google Scholar] [CrossRef]
- Bacchetta, J.; Zaritsky, J.J.; Sea, J.L.; Chun, R.F.; Lisse, T.S.; Zavala, K.; Wesseling-Perry, K.; Westerman, M.; Hollis, B.W.; Isidro, B.S.; et al. Suppression of iron-regulatory hepcidin by vitamin D. J. Am. Soc. Nephrol. 2014, 25, 564–572. [Google Scholar] [CrossRef]
- Moran, D.S.; Heled, Y.; Arbel, Y.; Israeli, E.; Finestone, A.S.; Evans, R.K.; Yanovich, R. Dietary intake and stress fractures among elite male combat recruits. J. Int. Soc. Sports Nutr. 2012, 9, 6. [Google Scholar] [CrossRef]
- Yanovich, R.; Karl, J.P.; Yanovich, E.; Lutz, L.J.; Williams, K.W.; Cable, S.J.; Young, A.J.; Pasiakos, S.M.; McClung, J.P. Effects of basic combat training on iron status in male and female soldiers: A comparative study. US Army Med. Dep. J. 2015, April–June, 67–73. [Google Scholar] [PubMed]
- Behzadnezhad, N.; Esfarjani, F.; Marandi, S.M. Impact of resistance training and basic ferritin on hepcidin, iron status and some inflammatory markers in overweight/obese girls. J. Res. Med. Sci. 2021, 26, 95. [Google Scholar] [CrossRef]
- My, G.; Marsigliante, S.; Bianco, A.; Zangla, D.; Silva, C.M.D.; Muscella, A. Biological, psychological, and physical performance variations in football players during the COVID-19 lockdown: A prospective cohort study. Int. J. Environ. Res. Public Health 2022, 19, 2739. [Google Scholar] [CrossRef]
- Andrews, N.C.; Schmidt, P.J. Iron homeostasis. Annu. Rev. Physiol. 2007, 69, 69–85. [Google Scholar] [CrossRef]
- Umbreit, J. Iron deficiency: A concise review. Am. J. Hematol. 2005, 78, 225–321. [Google Scholar] [CrossRef]
- Peeling, P.; Blee, T.; Goodman, C.; Dawson, B.; Claydon, G.; Beilby, J.; Prins, A. Effect of iron injections on aerobic-exercise performance of iron-depleted female athletes. Int. J. Sport Nutr. Exerc. Metab. 2007, 17, 221–231. [Google Scholar] [CrossRef]
- Barker, T.; Rogers, V.E.; Henriksen, V.T.; Trawick, R.H.; Momberger, N.G.; Lynn Rasmussen, G. Circulating IL-10 is compromised in patients predisposed to developing and in patients with severe knee osteoarthritis. Sci. Rep. 2021, 11, 1812. [Google Scholar] [CrossRef]
- Gogos, C.A.; Drosou, E.; Bassaris, H.P.; Skoutelis, A. Pro- versus anti-inflammatory cytokine profile in patients with severe sepsis: A marker for prognosis and future therapeutic options. J. Infect. Dis. 2000, 181, 176–180. [Google Scholar] [CrossRef]
- Lira, F.S.; Rosa, J.C.; Zanchi, N.E.; Yamashita, A.S.; Lopes, R.D.; Lopes, A.C.; Batista, M.L.; Seelaender, M. Regulation of inflammation in the adipose tissue in cancer cachexia: Effect of exercise. Cell Biochem. Funct. 2009, 27, 71–75. [Google Scholar] [CrossRef]
- Nikseresht, M.; Agha-Alinejad, H.; Azarbayjani, M.A.; Ebrahim, K. Effects of nonlinear resistance and aerobic interval training on cytokines and insulin resistance in sedentary men who are obese. J. Strength Cond. Res. 2014, 28, 2560–2568. [Google Scholar] [CrossRef] [PubMed]
- Vogelmeier, C.F.; Criner, G.J.; Martinez, F.J.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Chen, R.; Decramer, M.; Fabbri, L.M.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am. J. Respir. Crit. Care Med. 2017, 195, 557–582. [Google Scholar] [CrossRef] [PubMed]
- Ellulu, M.S.; Patimah, I.; Khaza’ai, H.; Rahmat, A.; Abed, Y. Obesity and inflammation: The linking mechanism and the complications. Arch. Med. Sci. 2017, 13, 851–863. [Google Scholar] [CrossRef] [PubMed]
- Libardi, C.A.; De Souza, G.V.; Cavaglieri, C.R.; Madruga, V.A.; Chacon-Mikahil, M.P. Effect of resistance, endurance, and concurrent training on TNF-α, IL-6, and CRP. Med. Sci. Sports Exerc. 2012, 44, 50–56. [Google Scholar] [CrossRef]
- Lobo, P.C.B.; Pimentel, G.D. Ursolic acid does not change the cytokine levels following resistance training in healthy men: A pilot balanced, double-blind and placebo-controlled clinical trial. Biomed. Pharmacother. 2022, 145, 112289. [Google Scholar] [CrossRef]
- Hilger, J.; Friedel, A.; Herr, R.; Rausch, T.; Roos, F.; Wahl, D.A.; Pierroz, D.D.; Weber, P.; Hoffmann, K. A systematic review of vitamin D status in populations worldwide. Br. J. Nutr. 2014, 111, 23–45. [Google Scholar] [CrossRef]
- Cashman, K.D.; Dowling, K.G.; Škrabáková, Z.; Gonzalez-Gross, M.; Valtueña, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Mølgaard, C.; et al. Vitamin D deficiency in Europe: Pandemic? Am. J. Clin. Nutr. 2016, 103, 1033–1044. [Google Scholar] [CrossRef]
- Garbossa, S.G.; Folli, F. Vitamin D, sub-inflammation and insulin resistance. A window on a potential role for the interaction between bone and glucose metabolism. Rev. Endocr. Metab. Disord. 2017, 18, 243–258. [Google Scholar] [CrossRef]
- Trimarco, V.; Manzi, M.V.; Mancusi, C.; Strisciuglio, T.; Fucile, I.; Fiordelisi, A.; Pilato, E.; Izzo, R.; Barbato, E.; Lembo, M.; et al. Insulin resistance and vitamin D deficiency: A link beyond the appearances. Front. Cardiovasc. Med. 2022, 9, 859793. [Google Scholar] [CrossRef]
- Belenchia, A.M.; Tosh, A.K.; Hillman, L.S.; Peterson, C.A. Correcting vitamin D insufficiency improves insulin sensitivity in obese adolescents: A randomized controlled trial. Am. J. Clin. Nutr. 2013, 97, 774–781. [Google Scholar] [CrossRef]
- Nikseresht, M. Comparison of serum cytokine levels in men who are obese or men who are lean: Effects of nonlinear periodized resistance training and obesity. J. Strength Cond. Res. 2018, 32, 17871795. [Google Scholar] [CrossRef]
- Agbalalah, T.; Mushtaq, S. Effect of vitamin D3 supplementation on cardiometabolic disease risk among overweight/obese adult males in the UK: A pilot randomised controlled trial. J. Hum. Nutr. Diet 2022, 1–10. [Google Scholar] [CrossRef]
- Hashemilar, M.; Khalili, M.; Rezaeimanesh, N.; Hokmabadi, E.S.; Rasulzade, S.; Shamshirgaran, S.M.; Taheraghdam, A.; Farhoudi, M.; Shaafi, S.; Shakouri, S.K.; et al. Effect of whey protein supplementation on inflammatory and antioxidant markers, and clinical prognosis in acute ischemic stroke (TNS trial): A randomized, double blind, controlled, clinical trial. Adv. Pharm. Bull. 2020, 10, 135–140. [Google Scholar] [CrossRef]
- Prokopidis, K.; Mazidi, M.; Sankaranarayanan, R.; Tajik, B.; McArdle, A.; Isanejad, M. Effects of whey and soy protein supplementation on inflammatory cytokines in older adults: A systematic review and meta-analysis. Br. J. Nutr. 2022, 1–12. [Google Scholar] [CrossRef]
| Variables | Placebo (n = 17) | Vitamin D (n = 20) | ||
|---|---|---|---|---|
| Week 0 | Week 12 | Week 0 | Week 12 | |
| RER | 1.09 ± 0.04 | 1.08 ± 0.05 | 1.07 ± 0.04 | 1.10 ± 0.06 * |
| HR (beats/min) | 198.5 ± 8.6 | 198.0 ± 12.2 | 196.9 ± 10.7 | 195.4 ± 11.2 |
| VE (L/min) | 145.6 ± 18.6 | 145.0 ± 19.3 | 149.0 ± 20.6 | 148.8 ± 15.4 |
| BF (times/min) | 56.2 ± 7.4 | 56.0 ± 8.6 | 54.4 ± 6.6 | 54.7 ± 6.0 |
| Variables | Placebo (n = 18) | Vitamin D (n = 21) | ||
|---|---|---|---|---|
| Week 0 | Week 12 | Week 0 | Week 12 | |
| IL-1α (pg/mL) | 0.18 ± 0.13 | 0.22 ± 0.16 | 0.13 ± 0.07 | 0.19 ± 0.15 |
| IL-1β (pg/mL) | 1.55 ± 1.03 | 1.52 ± 1.29 | 1.01 ± 0.45 | 0.95 ± 0.32 |
| IL-4 (pg/mL) | 1.63 ± 0.37 | 1.67 ± 0.41 | 1.63 ± 0.35 | 1.53 ± 0.28 |
| IL-6 (pg/mL) | 1.07 ± 1.16 | 0.82 ± 0.58 | 0.78 ± 0.62 | 0.97 ± 0.80 |
| IL-8 (pg/mL) | 10.87 ± 3.67 | 11.06 ± 4.88 | 12.80 ± 7.12 | 12.37 ± 9.59 |
| IL-10 (pg/mL) | 0.69 ± 0.32 | 0.76 ± 0.43 | 0.71 ± 0.49 | 0.88 ± 0.58 |
| TNF-α (pg/mL) | 3.59 ± 0.99 | 3.53 ± 1.30 | 3.32 ± 0.87 | 3.06 ± 1.00 |
| IL-10/TNF-α | 0.19 ± 0.07 | 0.22 ± 0.08 | 0.23 ± 0.16 | 0.30 ± 0.19 * |
| MCP-1 (pg/mL) | 171.2 ± 57.4 | 164.6 ± 54.7 | 188.8 ± 91.1 | 172.9 ± 82.6 |
| Variables | Group | Week 0 | Week 8 | Week 12 |
|---|---|---|---|---|
| Glucose (mmol/L) | PLC | 5.32 ± 0.28 | 5.28 ± 0.29 | 5.48 ± 0.32 |
| VD | 5.12 ± 0.34 | 5.14 ± 0.38 | 5.17 ± 0.42 | |
| Ferritin (µg/L) | PLC | 102.9 ± 72.9 | 79.5 ± 59.9 * | 78.0 ± 59.3 * |
| VD | 129.6 ± 80.6 | 107.5 ± 74.5 * | 102.1 ± 81.4 * | |
| Insulin (mU/L) | PLC | 9.22 ± 3.95 | 9.46 ± 2.11 | 9.18 ± 2.20 |
| VD | 7.76 ± 2.26 | 8.13 ± 3.67 | 7.41 ± 1.71 | |
| HOMA-IR | PLC | 2.21 ± 1.04 | 2.21 ± 0.49 | 2.25 ± 0.62 |
| VD | 1.78 ± 0.57 | 1.86 ± 0.90 | 1.71 ± 0.44 |
| Variables | Group | Week 0 | Week 8 | Week 12 |
|---|---|---|---|---|
| Haemoglobin (g/L) | PLC | 155.4 ± 9.9 | 155.4 ± 10.9 | 156.4 ± 9.2 |
| VD | 153.0 ± 9.8 | 151.0 ± 10.8 | 152.5 ± 10.7 | |
| Haematocrit (%) | PLC | 46.0 ± 2.5 | 45.9 ± 2.6 | 45.8 ± 2.0 |
| VD | 44.7 ± 2.2 | 44.2 ± 2.2 | 44.8 ± 2.1 | |
| Erythrocytes (×1012/L) | PLC | 5.26 ± 0.28 | 5.25 ± 0.27 | 5.24 ± 0.24 |
| VD | 5.13 ± 0.23 | 5.08 ± 0.29 | 5.11 ± 0.28 | |
| Leukocytes (×109/L) | PLC | 5.8 ± 1.5 | 5.8 ± 1.4 | 5.6 ± 1.4 |
| VD | 5.9 ± 1.3 | 5.8 ± 1.4 | 6.3 ± 1.9 | |
| Thrombocytes (×109/L) | PLC | 236 ± 49 | 242 ± 50 | 236 ± 39 |
| VD | 237 ± 39 | 243 ± 41 | 239 ± 39 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savolainen, L.; Timpmann, S.; Mooses, M.; Medijainen, L.; Tõnutare, L.; Ross, F.; Lellsaar, M.; Piir, A.; Zilmer, M.; Unt, E.; et al. Vitamin D Supplementation Has No Impact on Cardiorespiratory Fitness, but Improves Inflammatory Status in Vitamin D Deficient Young Men Engaged in Resistance Training. Nutrients 2022, 14, 5302. https://doi.org/10.3390/nu14245302
Savolainen L, Timpmann S, Mooses M, Medijainen L, Tõnutare L, Ross F, Lellsaar M, Piir A, Zilmer M, Unt E, et al. Vitamin D Supplementation Has No Impact on Cardiorespiratory Fitness, but Improves Inflammatory Status in Vitamin D Deficient Young Men Engaged in Resistance Training. Nutrients. 2022; 14(24):5302. https://doi.org/10.3390/nu14245302
Chicago/Turabian StyleSavolainen, Lauri, Saima Timpmann, Martin Mooses, Luule Medijainen, Lisette Tõnutare, Frederik Ross, Märt Lellsaar, Anneli Piir, Mihkel Zilmer, Eve Unt, and et al. 2022. "Vitamin D Supplementation Has No Impact on Cardiorespiratory Fitness, but Improves Inflammatory Status in Vitamin D Deficient Young Men Engaged in Resistance Training" Nutrients 14, no. 24: 5302. https://doi.org/10.3390/nu14245302
APA StyleSavolainen, L., Timpmann, S., Mooses, M., Medijainen, L., Tõnutare, L., Ross, F., Lellsaar, M., Piir, A., Zilmer, M., Unt, E., & Ööpik, V. (2022). Vitamin D Supplementation Has No Impact on Cardiorespiratory Fitness, but Improves Inflammatory Status in Vitamin D Deficient Young Men Engaged in Resistance Training. Nutrients, 14(24), 5302. https://doi.org/10.3390/nu14245302





