Abstract
A balanced diet and protein source intake are reportedly good for health. However, many people skip breakfast or have a light breakfast. Thus, this study aimed to examine the influence of breakfast styles on eating habits among Japanese workers, including traditional Japanese-style breakfast (JB), a pattern in which Japanese foods are eaten; Japanese-Western-style breakfast (J–W B), a pattern in which Japanese and Western foods are eaten alternately; Western-style breakfast (WB), a pattern in which Western foods are eaten; and cereal-style breakfast (CB), a pattern in which cereal is eaten. We hypothesized that breakfast style may be related to good eating habits. Data from 4274 respondents (67.97% male, 33.03% female, age 48.12 ± 0.19 years), excluding night shift workers and breakfast absentees out of a total of 5535 respondents, were analyzed. The results suggest that Japanese food is linked to the intake of protein sources such as fish, eggs, and soy. Furthermore, it was suggested that Japanese food breakfast is effective for good eating habits, such as not eating irregular amounts of food, not eating snacks, not drinking sweet juices, and having a balanced diet.
1. Introduction
Healthy eating habits are an important factor for good health [1,2,3]. The Japanese diet, known as washoku, is attracting worldwide attention as a healthy diet. In 2013, traditional Japanese food was included in the UNESCO Intangible Cultural Heritage list. Consumption of Japanese food is characterized by (1) frequent consumption of a wide variety of seasonal foods, including vegetables, fish, soy products, seaweed, fruits, mushrooms, and potatoes; (2) food preparation based on large amounts of high-quality water; and (3) balanced nutrition [4,5]. Japanese foods are known to have a positive impact on health as the Japanese diet is associated with a lower risk of non-alcoholic fatty liver disease in Japanese men [6] and a lower incidence of sarcopenia in both men and women [7]. In addition, the traditional Japanese diet has been introduced as a healthy diet for the prevention of cardiovascular disease (CVD) in Western countries, and a modified Japanese diet as for the DASH diet, reduced hypertension [8,9]. By contrast, the results of dietary patterns of Japanese adults in the 2012 National Health and Nutrition Survey showed that the bread pattern was associated with higher total cholesterol levels in women and higher low-density lipoprotein cholesterol levels in both men and women [10]. Soy-based foods such as fermented miso and tofu, which are typical of the Japanese diet, are known to reduce blood pressure and blood glucose levels [11,12]. The Japanese diet has long attracted interest from other countries, mainly because of its potential contribution to the low rates of coronary artery disease and increased life expectancy [13].
Breakfast intake is associated with lower BMI [14,15] and lower prevalence of chronic diseases such as coronary heart disease [16] and type 2 diabetes [17,18], with a positive impact on longevity [19].
The Japanese style of breakfast intake includes rice and miso soup as the main ingredients; the Western style of breakfast intake includes bread, milk/soy, coffee/tea, and Western/Chinese soup; and the Japanese/Western style involves eating Japanese and Western food alternately depending on the day. Meanwhile, the cereal-breakfast style is considered convenient because people commonly tend to be busy or not hungry in the morning [20].
In Japan, people who eat breakfast often have a healthy lifestyle, including a healthy diet and regular exercise habits. A higher ratio of total energy intake to fat energy intake in the morning may result in lower absolute energy intake throughout the day [21], and breakfast intake has been demonstrated to prevent excessive energy intake. Additionally, increased protein source intake at breakfast during resistance exercise training is positively associated with muscle hypertrophy in middle-aged women [22]. However, the actual problem is that many working Japanese people tend to miss breakfast or finish with simple meals. Skipping staple foods at breakfast and excessive intake of staple foods at lunch and dinner may be associated with poor sleep–wake regularity [23]. Skipping breakfast was also associated with obesity, suggesting that skipping breakfast was a predictor of being overweight among men aged 20–49 years [24]. Evening-types, who are more likely to skip breakfast, have also been demonstrated to be associated with a higher risk of obesity and cardiometabolic disease and poorer health than morning-types. Furthermore, evening-types had a higher tendency to consume harmful foods such as sugary drinks, alcohol, and chocolate than healthy foods such as fish, fruit, and vegetables. Hence, chronotype was independently associated with abdominal obesity and visceral fat [25,26,27,28]. Breakfast is the most important meal of the day for children and adults to maintain their morning chronotype.
Consuming breakfast is important; however, dietary differences, such as eating out, high salt intake, and insufficient chewing, are also important factors for health. For example, eating out more frequently has been reported to affect the quality of dietary intake [29], particularly in relation to inadequate intake of dietary fiber, vitamin C, minerals (iron, magnesium, and potassium), low vegetable intake, and high oil and fat intake [30]. High salt intake in the diet increases blood pressure and the risk of kidney disease [31,32]. Salt restriction has been demonstrated to stabilize blood pressure [33]. As Japan is a hyper-aged society compared to other countries, preventing hypertension among the Japanese population is increasingly important as older age is associated with a higher risk of CVD, which reduces healthy life expectancy [9].
Although it is widely known that Japanese food has a positive impact on health and that breakfast is important, the impact of different breakfast styles on health remains unknown. This study aimed to investigate the impact of breakfast styles on eating habits among working Japanese individuals, including Japanese-style breakfast (JB), a pattern in which Japanese food items such as rice are included; Japanese–Western-style breakfast (J–WB), a pattern in which Japanese and Western food items are eaten alternately; Western-style breakfast (WB), a pattern in which bread is included; and cereal breakfast (CB), a pattern in which cereal is included for breakfast. We hypothesized that good eating habits are related to breakfast style.
2. Materials and Methods
2.1. Ethical Approval
This study was approved by the Ethics Review Committee on Research with Human Subjects of Waseda University and the Lion Corporation (No. 2020-046 and No. 352, respectively) and followed the guidelines laid down in the Declaration of Helsinki.
2.2. Target Population and Data Collection
The target population comprised Japanese male and female workers aged 20–69 years living in Japan (from Hokkaido to Okinawa). The survey respondents were recruited from the Lion Corporation, Tokyo, Japan. The Internet-based questionnaire survey was conducted from 18 to 22 June 2021.
2.3. Questionnaire
The online questionnaire consisted of 18–21 items regarding basic information on the respondent, such as sex, age, body mass index (BMI), residential area, and job description, and 60–82 questions on the respondent’s lifestyle, including work and personal life stress, health and personality, diet, and COVID-19 status. The study was designed by the Lion Corporation and the Shibata Laboratory at Waseda University and conducted by a WEB search company ordered by Lion Corporation, and the purpose of the questionnaire was to determine the lifestyle, eating habits, exercise habits, and health awareness of the Japanese workers.
The questionnaire was designed to take approximately 30 min to answer a total of 103 questions, but some people took more time to finish. Moreover, because this was an Internet-based questionnaire, people who met any of the following criteria were excluded from the survey: age ≤19 years and ≥70 years; unemployed; officers (directors and executive directors); working less than 2 working days in a week; and did not respond to any of the questions. Residential areas were equally included from northern to southern areas and from rural to urban areas. Jobs were equally included from civil servants to private companies and large to small companies. The number of participants who completely answered all questionnaires was 5534 (male n= 3849, female n = 1685) people. The results of the questionnaire responses from male and female workers who worked night shifts (22:00–5:00 the following day) (n = 808, male n = 614, female n = 194) were excluded, and residual participants were (n = 4726, male n = 3235, female n = 1491). To examine the impact of breakfast consumption on eating habits, data from those who reported missing breakfast (n = 452; male n = 330, female n = 122) were excluded. Thus, the ratio of breakfast missing was 10% for males and 8% for females, and these data had slightly lower values than the results (male 14%, female 9%) of Japanese adults in the 2018 National Health and Nutrition Survey. The final numbers for analysis in this report were n = 4274 (male n = 2905, female n = 1369) (Supplemental Figure S1). The data from these questionnaires were on sex, age, BMI, and breakfast style (JB, J-W B, WB, and CB). The intake of food items in the usual diet (7 levels) and eating habits in the usual diet (7 levels) was assessed using questionnaires (Supplemental Tables S1–S4).
2.4. Statistical Analysis
Statistical analyses were conducted using IBM SPSS Statistics (version 28; IBM Japan, Ltd., Tokyo, Japan). A non-parametric analysis (Mann–Whitney U test) was used to compare the results of breakfast style, respondent characteristics, and eating habits between men and women. A multiple regression analysis was conducted to examine the impact of breakfast style on eating habits. Between-group comparisons of breakfast style were made using the Kruskal–Wallis test and Dunn’s test. Statistical significance was set at p < 0.05. Data are expressed as mean and standard error.
3. Results
3.1. Participant Characteristics
The participants (n = 4274) comprised 67.97% of males and 33.03% of females (Supplemental Table S5). The mean age and BMI of the participants were 48.12 ± 0.19 years old and 22.68 ± 0.05 kg/m2, respectively. Daily intake of protein sources other than fish was significantly higher in women than in men. The daily intake of vegetables, fruits, and snacks was significantly higher in women than in men, while the intake of juice and alcohol was lower in women than in men. Regarding eating habits, smaller scores indicate healthier eating habits. Women were shown to have healthier eating habits than men in the categories ‘eat less food’, ‘eat out less’, and ‘don’t eat too much salt’.
3.2. Relationship between Breakfast Style and Usual Protein Source Intake
To examine the association between breakfast style and daily protein source intake, a multiple regression analysis was performed (Table 1). Protein source intake scores were entered as the objective variable, breakfast style (JB, J-W B, WB, or CB) as the explanatory variable, and sex, age, and BMI as adjustment factors. Similarly, the multiple regression analysis revealed that JB was associated with fish, egg, and bean intake in the usual diet. By contrast, WB and CB were related to the intake of dairy products in the usual diet. The mean scores (on a scale of 5) of the participants’ protein source intake were averaged and compared between the groups. Kruskal–Wallis and Dunn’s tests were used for between-group comparisons (Figure 1). The intake frequency of fish and eggs was high in the JB and J-W B groups. The intake frequency of beans was high in the JB group. The intake frequency of dairy products was higher in the WB and CB groups than in the JB and J-W B groups.

Table 1.
Results of multiple regression analysis of the relationship between breakfast style and protein source intake.
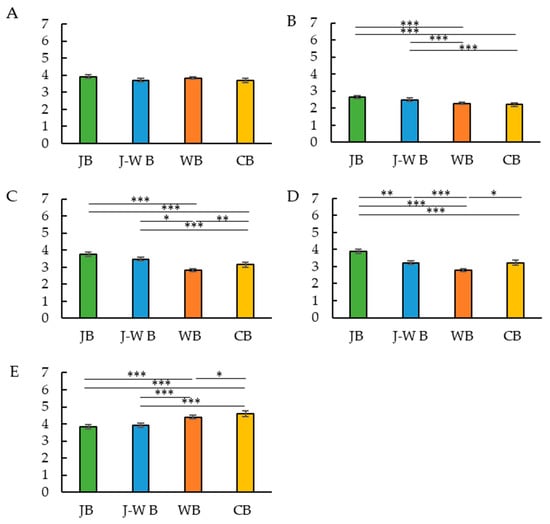
Figure 1.
Breakfast style and usual protein source intake score. Breakfast style and meat score (A). Breakfast style and fish score (B). Breakfast style and eggs score (C). Breakfast style and beans score (D). Breakfast style and dairy products score (E). * p < 0.05, ** p < 0.005, *** p < 0.001 (Dunn’s test).
3.3. Relationship between Breakfast Style and Usual Food Intake
A multiple regression analysis was conducted to examine the relationship between breakfast style and staple foods, vegetables, fruits, and beverages (Table 2). Food and beverage intake scores were entered as objective variables, breakfast style (JB, J-W B, WB, or CB) as explanatory variables, and sex, age, and BMI as adjustment factors. Multiple regression analysis revealed that consuming a JB or WB was related to consuming staple food in their usual diet. Consuming JB is associated with the consumption of vegetables and fruits in the usual diet. The consumption of WB is associated with the consumption of fruits and snacks in the usual diet. Participants’ scores for whether they consumed staple foods (on a scale of 5) and their average score for food intake (on a scale of 5) were averaged and compared between the groups. The Kruskal–Wallis test and Dunn’s tests were used for this between-group comparison (Figure 2). The staple food intake frequency was higher in the JB and WB groups and lower in the J-W B and CB groups. The consumption of snacks and juice frequency was lower in the JB, J-W B, and WB groups, in that order. Meanwhile, the frequency of alcohol consumption was higher in the JB and J-W B groups.

Table 2.
Results of the multiple regression analysis of the relationship between breakfast style and food intake.
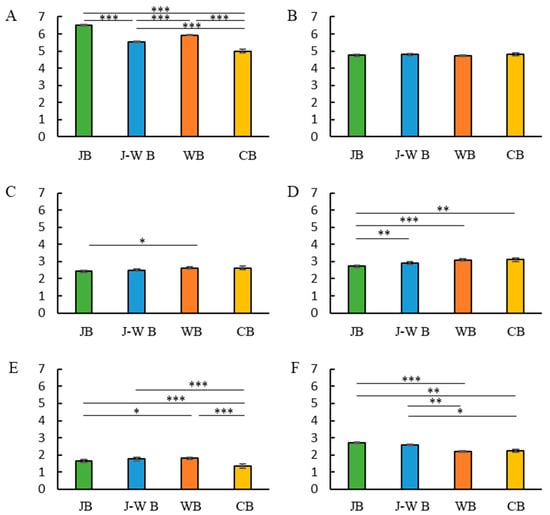
Figure 2.
Breakfast style and usual food score. Breakfast style and staple food score (A). Breakfast style and vegetable score (B). Breakfast style and fruits score (C). Breakfast style and snack score (D). Breakfast style and juice score (E). Breakfast style and alcohol score (F). * p < 0.05, ** p < 0.005, *** p < 0.001 (Dunn’s test).
3.4. Relationship between Breakfast Style and Usual Eating Habits
A multiple regression analysis was performed to examine the relationship between breakfast style and eating habits (Table 3). Eating habit scores were entered as the objective variable, breakfast style (JB, J-W B, WB, or CB) as the explanatory variable, and sex, age, and BMI as adjustment factors. Multiple regression analysis revealed that consuming a Japanese breakfast had an impact on consuming regular amounts of food, not eating too much food in one sitting, having balanced nutrition, and not having excessive salt intake. Participants’ eating habit scores (on a scale of 7) were averaged and compared between the groups. Kruskal–Wallis and Dunn’s tests were used for between-group comparisons (Figure 3). Consuming irregular amounts of food was lower in the JB group than in the J-W B group. The frequency of unbalanced nutrition and eating full meals was lower in the JB group than in the WB group.

Table 3.
Results of multiple regression analysis of the relationship between breakfast style and eating habits.
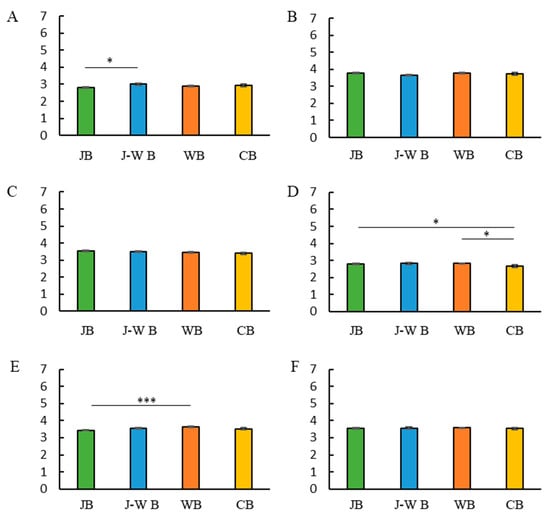
Figure 3.
Breakfast style and usual eating habits. Breakfast style and irregular amount of food score (A). Breakfast style and less chewing (B). Breakfast style and large amounts of food (C). Breakfast style and frequent eating out (D). Breakfast style and nutritional imbalance (E). Breakfast style and excessive salt intake (F). * p < 0.05, *** p < 0.001 (Dunn’s test).
4. Discussion
To the best of our knowledge, this is the first cross-sectional study to assess the association between breakfast type and eating habits among Japanese workers. Our results demonstrate that even a light breakfast, such as cereals, has a positive impact on eating habits, but that JB, in particular, has a positive impact on eating habits throughout the day, not just in the morning.
4.1. Risks of Skipping Breakfast
Many previous studies have examined breakfast skipping. Skipping breakfast has been demonstrated to affect elements of energy balance [34], although it has also been suggested to be a predictor of being overweight [34,35]. Weight control is often cited as the reason for not eating breakfast. Weight control has been reported to be associated with unhealthy behaviors, poor diet, and lower physical activity [36,37,38,39], and is also associated with higher metabolic risk, that is, higher BMI. Here, not skipping breakfast was linked to vegetable intake and eating a balanced diet. We focused on the type of breakfast rather than skipping breakfast because skipping breakfast is considered unhealthy.
4.2. Japanese Food Styles and Their Effects
The study primarily aimed to examine what kind of breakfast, if any, would have health benefits. Previous studies have reported that soy, traditionally consumed in Japan, is expected to prevent lifestyle-related diseases such as stroke and coronary heart disease [40]. Furthermore, eating fish regularly has also been reported to prevent lifestyle-related diseases, such as hypertension and diabetes [41,42]. Japanese food is generally rich in soy, seafood, miso, soy sauce, vegetables, potatoes, and mushrooms; therefore, consuming a Japanese breakfast is a good way to consume these foods. The consumption of seafood provides dietary amino acids, which play an important role in protein synthesis [43]. Additionally, soy provides an important source of protein, dietary fiber, vitamins such as folate, and minerals such as iron, zinc, and magnesium. Increasing the intake of these nutrients can enhance the quality of the diet. Saponins and tannins in pulses also have antioxidant and anti-carcinogenic properties, indicating that pulses may have significant anti-cancer properties [44]. The Japan National Health and Nutrition Survey 2012 revealed that more than 95% of the participants met recommended levels of protein suggested by the Dietary Reference Intake in Japan [45]. Thus, the current study suggests that the Japanese breakfast leads to not only an increased volume of protein source intake but also to a variety of protein sources such as fish, eggs, and soy throughout the day.
The main sources of energy in the diet should be complex carbohydrates, and it is not a bad sign if the reduction in protein source intake is compensated by carbohydrates with a small addition of fat. On the other hand, if the proportion of protein sources in the diet decreases, too much excess energy intake from non-protein energy nutrients (carbohydrates and fats) may be driven to compensate for the energy deficit caused by reduced protein source intake [46,47]. Interestingly, Japan National Health and Nutrition Surveys during the period from 1995 to 2016 have demonstrated that total energy intake showed a decreasing trend in both males and females, but energy intake from protein decreased and energy intake (%) from fat increased in both sexes [48]. Thus, excessive intake of carbohydrates and fats leads to obesity. Among proteins, soy-based foods, such as miso and tofu, are known to reduce blood pressure and blood glucose levels [11,12], and fish oil, DHA, and EPA found in fish can reduce or improve the risk of CVD [49,50,51,52]. Sugar intake causes CVD, type 2 diabetes, obesity, metabolic syndrome, and inflammation [53,54]. Furthermore, the consumption of Japanese food is negatively related to the intake of sugar-sweetened drinks such as juices. Consuming Japanese food may prevent excessive sugar intake; thus, it may have a positive impact on health. In this study, the consumption of Japanese food was positively related to alcoholic beverage consumption. However, the mechanism behind the association between the consumption of Japanese food and alcohol intake is unknown. The current study suggests that traditional Japanese diets lead to a high intake of fish and beans. Consuming a Japanese diet has also been epidemiologically associated with a lower risk of CVD [55,56] and beneficial for blood pressure if salt intake is optimized [10]. Here, no association between excessive salt intake and consumption of Japanese breakfast food was identified.
4.3. Eating Habits and Breakfast Intake Style
Eating habits and breakfast intake styles are related, and these have a direct connection to health. When we consume food with irregular rhythms, the thermic effect of food is significantly less than with normal dietary patterns, and the increased responsiveness to glucose may have adverse effects on health, such as causing obesity and reduced metabolism [57,58], Metabolic syndrome has been linked to BMI, and cardiovascular metabolic risk factors such as blood pressure have also been suggested to be at higher risk [59]. A healthy balanced diet provides the human body with energy (macronutrients) and all necessary micronutrients (vitamins, minerals, protein-producing amino acids, and omega fatty acids) required for the maintenance of all metabolic processes [60]. This suggests the importance of a healthy and balanced diet. Several studies have suggested that a diet rich in antioxidants and anti-inflammatory components, such as fruits, nuts, vegetables, and fish, can reduce the risk of age-related cognitive decline and various neurodegenerative diseases [61]. A balanced and nutritious diet is important for maintaining good health, and the current study suggests that a balanced diet can be achieved by JB. Among American adults, the number of daily snacks increased by approximately one snack per day between 1977 and 2006 [62]. Thus, owing to the prevalence of snacks in today’s society, energy-dense and low-quality snacks, including high-fat and high-sugar snack foods, are associated with an increased risk of obesity and CVD [62,63,64]. High-fiber snacks may have a positive effect, such as lowering blood glucose levels [65], and high-protein snacks may promote further satiety [64] and reduce overconsumption at the next meal [64]; therefore, what you eat may or may not be detrimental to your health. Being full is one of the important psychobiological mechanisms that function to inhibit post-intake of food and drinks and is an important factor in reducing overconsumption that can lead to being overweight and obesity [64,66], in addition to the fact that snacking still leads to obesity. Here, a negative correlation between consuming a JB and consuming snacks was identified, suggesting that consuming Japanese food for breakfast tends to make people less likely to consume snacks. On the other hand, snacking plays an important role in replenishing what is lacking in nutrition from regular meals. In the current study, participants were workers, and it is possible to eat snacks for replenishing lacking energy between meal times.
4.4. Breakfast Realities and History
Many Japanese people consider it ideal to consume Japanese food such as rice and miso soup for breakfast. In reality, most people consume Western (bread-based) breakfasts. One of the reasons behind the gap between the ideal and reality is that many people believe that they do not have time in the morning [67]. This survey was conducted on only 107 Japanese adults in Tokyo. On the other hand, the present results revealed that JB and WB were 28% and 41%. In addition, recently our paper demonstrated that 2571 participants were categorized by JB (31% for male, 24% for female) and WB (28% for male, 31% for female) [68]. Thus, there was not a big difference in the ratio of Japanese style and Western style breakfast. It is much easier to bake bread and spread jam than to cook rice and make side dishes and miso soup, and even easier to make a CB-style breakfast, which is completed simply by adding milk to cereal. Thus, those who can afford to consume Japanese food in the morning may be able to pay attention to a balanced diet, the amount of food they eat, and their vegetable and protein source intake.
In Japan, Western-style eating did not begin until after World War II, when Japan imported food from other countries to solve malnutrition. However, Western-style diets are said to lead to overeating and obesity, which may affect lifestyle-related diseases and other health problems [69].
4.5. Limitation of Current Study
There are some limitations to our study. First, food items and eating habits were collected through self-reports, and this self-reporting may have resulted in self-efficacy. Second, although there are 21 characteristics of respondence, we used only three variables in this paper (gender, age, BMI). Therefore, more variables should be used to analyze the associations. Third, “eating out” is an inadequate question, because we do not define whether eating out means nutrition balanced healthy meals or oily unhealthy fast food. Fourth, “snack intake” is also an inadequate question, because we do not define whether snack intake is for the replenishing of what is lacking or for just fun. Fifth, we want to know the association between food items/eating habits and not only breakfast style, but lunch and dinner meal style to understand the role of traditional Japanese food in healthy eating behavior.
5. Conclusions
Different types of breakfast have different effects on eating habits, such as daily intake of items and eating habits. The intake of JB may have a positive impact on eating habits, as it is related to the regularity and quantity of fish, eggs, and beans in the usual diet and balanced diet. Meanwhile, the intake of WB and CB is positively related to the intake of dairy products in the usual diet, and consuming WB is negatively related to the intake of soy, so a JB and occasionally a WB, may lead to a more balanced diet.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14235143/s1, Supplemental Table S1: Participants’ characteristics; Supplemental Table S2: Content of question about breakfast style; Supplemental Table S3: Content of question about weekly protein source intake; Supplemental Table S4: Content of question about weekly food items intake; Supplemental Table S5: Content of question about eating habits. Figure S1: Flow design of the study participants.
Author Contributions
Conceptualization and research idea, Y.T. and S.S.; methodology and data collection, T.S. and Y.N.; data analysis, writing the original draft and editing, M.K.; funding acquisition, formal analysis, writing the revised draft and review, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Japan Society for the Promotion of Science (JSPS) KAKENHI (Kiban A 19H01089) and the JST-Mirai Program (Grant Number: JMPJM120d5) by S. Shibata.
Institutional Review Board Statement
The Ethics Review Committee on Research with Human Subjects at Waseda University and the Lion Corporation approved this experiment (No. 2020-046 and No. 352, respectively), and the guidelines laid down in the Declaration of Helsinki were followed. Informed consent statement: Informed consent was obtained from all the subjects involved in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be sent upon request from the corresponding author. The data are not publicly available because of patent preparation.
Acknowledgments
The authors are grateful to Marketing Directions Inc., Japan, for supporting the design of the questionnaires. They were not involved in the study design, data collection, analysis, reporting of the results, or writing of the manuscript. All authors agreed this statement.
Conflicts of Interest
T.S. and Y.N. are full-time employees of the Lion Corporation. The company’s policy was not involved in the study design, collection, analysis, interpretation of data, or writing of the manuscript. The other authors declare no conflict of interest.
References
- Cadenas-Sanchez, C.; Medrano, M.; Arenaza, L.; Amasene, M.; Osés, M.; Labayen, I. Association between Mediterranean Dietary Pattern and Breakfast Quality with Physical Fitness in School Children: The HIIT Project. Nutrients 2021, 13, 1353. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. PREDIMED Study Investigators. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. New Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Gabriel, A.S.; Ninomiya, K.; Uneyama, H. The Role of the Japanese Traditional Diet in Healthy and Sustainable Dietary Patterns around the World. Nutrients 2017, 10, 173. [Google Scholar] [CrossRef]
- Yatsuya, H.; Tsugane, S. What constitutes healthiness of Washoku or Japanese diet? Eur. J. Clin. Nutr. 2021, 75, 863–864. [Google Scholar] [CrossRef]
- Nakashita, C.; Xi, L.; Inoue, Y.; Kabura, R.; Masuda, S.; Yamano, Y.; Katoh, K. Impact of dietary compositions and patterns on the prevalence of nonalcoholic fatty liver disease in Japanese men: A cross-sectional study. BMC Gastroenterol. 2021, 21, 342. [Google Scholar] [CrossRef] [PubMed]
- Suthuvoravut, U.; Takahashi, K.; Murayama, H.; Tanaka, T.; Akishita, M.; Iijima, K. Association between Traditional Japanese Diet Washoku and Sarcopenia in Community-Dwelling Older Adults: Findings from the Kashiwa Study. J. Nutr. Health Aging 2020, 24, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Tsugane, S.; Sawada, N. The JPHC Study: Design and Some Findings on the Typical Japanese Diet. Jpn. J. Clin. Oncol. 2014, 44, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, A.; Kajiya, K.; Kishi, H.; Inagaki, J.; Mitarai, M.; Oda, H.; Umemoto, S.; Kobayashi, S. The Nutritional Characteristics of the Hypotensive WASHOKU-modified DASH Diet: A Sub-analysis of the DASH-JUMP Study. Curr. Hypertens. Rev. 2018, 14, 56–65. [Google Scholar] [CrossRef]
- Htun, N.C.; Suga, H.; Imai, S.; Shimizu, W.; Ishikawa-Takata, K.; Takimoto, H. Dietary pattern and its association with blood pressure and blood lipid profiles among Japanese adults in the 2012 Japan National Health and Nutrition Survey. Asia Pac. J. Clin. Nutr. 2018, 27, 1048–1061. [Google Scholar]
- Rivas, M.; Garay, R.P.; Escanero, J.F.; Cia, P.; Cia, P.; Alda, J.O. Soy milk lowers blood pressure in men and women with mild to moderate essential hypertension. J. Nutr. 2002, 132, 1900–1902. [Google Scholar] [CrossRef]
- Jayagopal, V.; Albertazzi, P.; Kilpatrick, E.S.; Howarth, E.M.; Jennings, P.E.; Hepburn, D.A.; Atkin, S.L. Beneficial effects of soy phytoestrogen intake in postmenopausal women with type 2 diabetes. Diabetes Care 2002, 25, 1709–1714. [Google Scholar] [CrossRef]
- Murakami, K.; Livingstone, M.B.E.; Shinozaki, N.; Sugimoto, M.; Fujiwara, A.; Masayasu, S.; Sasaki, S. Food Combinations in Relation to the Quality of Overall Diet and Individual Meals in Japanese Adults: A Nationwide Study. Nutrients 2020, 12, 327. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Dietrich, M.; Brown, C.J.; Clark, C.A.; Block, G. The effect of breakfast type on total daily energy intake and body mass index: Results from the Third National Health and Nutrition Examination Survey (NHANES III). J. Am. Coll. Nutr. 2003, 22, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Purslow, L.R.; Sandhu, M.S.; Forouhi, N.; Young, E.H.; Luben, R.N.; Welch, A.A.; Khaw, K.T.; Bingham, S.A.; Wareham, N.J. Energy intake at breakfast and weight change: Prospective study of 6764 middle-aged men and women. Am. J. Epidemiol. 2008, 167, 188–192. [Google Scholar] [CrossRef]
- Cahill, L.E.; Chiuve, S.E.; Mekary, R.A.; Jensen, M.K.; Flint, A.J.; Hu, F.B.; Rimm, E.B. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 2013, 128, 337–343. [Google Scholar] [CrossRef]
- Mekary, R.A.; Giovannucci, E.; Willett, W.C.; van Dam, R.M.; Hu, F.B. Eating patterns and type 2 diabetes risk in men: Breakfast omission, eating frequency, and snacking. Am. J. Clin. Nutr. 2012, 95, 1182–1189. [Google Scholar] [CrossRef]
- Roshanmehr, F.; Hayashi, H.; Tahara, Y.; Suiko, T.; Nagamori, Y.; Iwai, T.; Shibata, S. Association between Breakfast Meal Categories and Timing of Physical Activity of Japanese Workers. Foods 2022, 11, 2609. [Google Scholar] [CrossRef] [PubMed]
- Osera, T.; Awai, M.; Kobayashi, M.; Tsutie, S.; Kurihara, N. Relationship between Self-Rated Health and Lifestyle and Food Habits in Japanese High School Students. Behav. Sci. 2017, 7, 71. [Google Scholar] [CrossRef]
- Murakami, K.; Livingstone, M.B.E.; Sasaki, S. Meal-specific dietary patterns and their contribution to overall dietary patterns in the Japanese context: Findings from the 2012 National Health and Nutrition Survey, Japan. Nutrition 2019, 59, 108–115. [Google Scholar] [CrossRef]
- Tani, Y.; Asakura, K.; Sasaki, S.; Hirota, N.; Notsu, A.; Todoriki, H.; Miura, A.; Fukui, M.; Date, C. Higher proportion of total and fat energy intake during the morning may reduce absolute intake of energy within the day. An observational study in free-living Japanese adults. Appetite 2015, 92, 66–73. [Google Scholar] [CrossRef]
- Yasuda, M.; Murata, K.; Hasegawa, T.; Yamamura, M.; Maeo, S.; Takegaki, J.; Tottori, N.; Yokokawa, T.; Mori, R.; Mori, T.; et al. Relationship between protein intake and resistance training-induced muscle hypertrophy in middle-aged women: A pilot study. Nutrition 2022, 97, 111607. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Uemura, H.; Katsuura-Kamano, S.; Nakamoto, M.; Hiyoshi, M.; Takami, H.; Sawachika, F.; Juta, T.; Arisawa, K. Relationship of dietary factors and habits with sleep-wake regularity. Asia Pac. J. Clin. Nutr. 2013, 22, 457–465. [Google Scholar]
- Kito, K.; Kuriyama, A.; Takahashi, Y.; Nakayama, N. Impacts of skipping breakfast and late dinner on the incidence of being overweight: A 3-year retrospective cohort study of men aged 20-49 years. J. Hum. Nutr. Diet. 2019, 32, 349–355. [Google Scholar] [CrossRef]
- Maukonen, M.; Kanerva, N.; Partonen, T.; Kronholm, E.; Konttinen, H.; Wennman, H.; Männistö, S. The associations between chronotype, a healthy diet and obesity. Chronobiol. Int. 2016, 33, 972–981. [Google Scholar] [CrossRef]
- Merikanto, I.; Lahti, T.; Puolijoki, H.; Vanhala, M.; Peltonen, M.; Laatikainen, T.; Vartiainen, E.; Salomaa, V.; Kronholm, E.; Partonen, T. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol. Int. 2013, 30, 470–477. [Google Scholar] [CrossRef]
- Kanerva, N.; Kronholm, E.; Partonen, T.; Ovaskainen, M.-L.; Kaartinen, N.E.; Konttinen, H.; Broms, U.; Männistö, S. Tendency toward eveningness is associated with unhealthy dietary habits. Chronobiol. Int. 2012, 29, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Sato-Mito, N.; Shibata, S.; Sasaki, S.; Sato, K. Dietary intake is associated with human chronotype as assessed by both morningness-eveningness score and preferred midpoint of sleep in young Japanese women. Int. J. Food Sci. Nutr. 2011, 62, 525–532. [Google Scholar] [CrossRef]
- Beydoun, M.A.; Powell, L.M.; Wang, Y. Reduced away-from-home food expenditure and better nutrition knowledge and belief can improve quality of dietary intake among US adults. Public Health Nutr. 2009, 12, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Saito, A.; Okada, C.; Okada, E.; Tajima, R.; Takimoto, H. Consumption of meals prepared away from home is associated with inadequacy of dietary fiber, vitamin C and mineral intake among Japanese adults: Analysis from the 2015 National Health and Nutrition Survey. Nutr. J. 2021, 20, 40. [Google Scholar] [CrossRef] [PubMed]
- Malta, D.; Petersen, K.S.; Johnson, C.; Trieu, K.; Rae, S.; Jefferson, K.; Santos, J.A.; Wong, M.M.Y.; Raj, T.S.; Webster, J.; et al. High sodium intake increases blood pressure and risk of kidney disease. From the Science of Salt: A regularly updated systematic review of salt and health outcomes (August 2016 to March 2017). J. Clin. Hypertens. 2018, 20, 1654–1665. [Google Scholar] [CrossRef] [PubMed]
- Katsuya, T.; Ishikawa, K.; Sugimoto, K.; Rakugi, H.; Ogihara, T. Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens. Res. 2003, 26, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Michikawa, T.; Nishiwaki, Y.; Okamura, T.; Asakura, K.; Nakano, M.; Takebayashi, T. A The taste of salt measured by a simple test and blood pressure in Japanese women and men. Hypertens. Res. 2009, 32, 399–403. [Google Scholar] [PubMed]
- Betts, J.A.; Chowdhury, E.A.; Gonzalez, J.T.; Richardson, J.D.; Tsintzas, K.; Thompson, D. Is breakfast the most important meal of the day? Proc. Nutr. Soc. 2016, 75, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Chen, Q.; Pu, Y.; Guo, M.; Jiang, Z.; Huang, W.; Lomg, Y.; Xu, Y. Skipping breakfast is associated with overweight and obesity: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2020, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ruxton, H.C.; Kirk, R.T. Breakfast: A review of associations with measures of dietary intake, physiology and biochemistry. Br. J. Nutr. 1997, 78, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Song, W.O.; Chun, O.K.; Obayashi, S.; Cho, S.; Chung, C.E. Is consumption of breakfast associated with body mass index in US adults? J. Am. Diet. Assoc. 2005, 105, 1373–1382. [Google Scholar] [CrossRef]
- Timlin, M.T.; Pereira, M.A.; Story, M.; Neumark-Sztainer, D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008, 121, e638–e645. [Google Scholar] [CrossRef]
- Van der Heijden, A.A.; Hu, F.B.; Rimm, E.B.; van Dam, R.M. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity 2007, 15, 2463–2469. [Google Scholar] [CrossRef]
- Uesugi, T.; Fukui, Y.; Yamori, Y. Beneficial Effects of Soybean Isoflavone Supplementation on Bone Metabolism and Serum Lipids in Postmenopausal Japanese Women: A Four-week Study. J. Am. Coll. Nutr. 2002, 21, 97–102. [Google Scholar]
- Yamori, Y.; Liu, L.; Ikeda, K.; Miura, A.; Mizushima, S.; Miki, T.; Nara, Y. WHO-Cardiovascular Disease and Alimentary Comprarison (CARDIAC) Study Group, Distribution of 24-hour Urinary Taurine Excretion and Association with Ischemic Heart Disease Mortality in 24 Populations of 16 Countries: Results from the WHO-CARDIAC Study. Hypertens. Res. 2001, 24, 453–457. [Google Scholar] [CrossRef]
- Mori, T.A.; Burke, V.; Puddey, I.B.; Watts, G.F.; O’Neal, D.N.; Best, J.D.; Beilin, L.J. Purified Eicosapentaenoic and Docosahexaenoic Acids have Differential Effects on Serum Lipids and Lipoproteins, LDL Particle Size, Glucose, and Insulin in Mildly Hyperlipidemic Men. Am. J. Clin. Nutr. 2000, 71, 1085–1094. [Google Scholar] [CrossRef]
- Andersen, S.M.; Waadgø, R.; Espe, M. Functional amino acids in fish health and welfare. Front. Biosci. Elite Is Front Biosci. (Elite Ed) 2016, 8, 143–169. [Google Scholar] [PubMed]
- Mudryj, A.N.; Yu, N.; Aukema, H.M. Nutritional and health benefits of pulses. Appl. Physiol. Nutr. Metab. 2014, 39, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa-Takata, K.; Takimoto, H. Current protein and amino acid intakes among Japanese people: Analysis of the 2012 National Health and Nutrition Survey. Geriatr. Gerontol. Int. 2018, 18, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Gosby, A.K.; Conigrave, A.D.; Raubenheimer, D.; Simpson, S.J. Protein leverage and energy intake. Obes. Rev. 2014, 15, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Simonson, M.; Boirie, Y.; Guillet, C. Protein, amino acids and obesity treatment. Rev. Endocr. Metab. Disord. 2020, 21, 341–353. [Google Scholar] [CrossRef]
- Saito, A.; Imai, S.; Htun, N.C.; Okada, E.; Yoshita, K.; Yoshiike, N.; Takimoto, H. The trends in total energy, macronutrients and sodium intake among Japanese: Findings from the 1995-2016 National Health and Nutrition Survey. Br. J. Nutr. 2018, 120, 424–434. [Google Scholar] [CrossRef]
- Cottin, S.C.; Sanders, T.A.; Hall, W.L. The differential effects of EPA and DHA on cardiovascular risk factors. Proc. Nutr. Soc. 2011, 70, 215–231. [Google Scholar] [CrossRef]
- Innes, J.K.; Calder, P.C. Marine Omega-3 (N-3) Fatty Acids for Cardiovascular Health: An Update for 2020. Int. J. Mol. Sci. 2020, 21, 1362. [Google Scholar] [CrossRef]
- Kromann, N.; Green, A. Epidemiological studies in the Upernavik district, Greenland. Incidence of some chronic diseases 1950–1974. Acta Med. Scand. 1980, 208, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Bjerregaard, P.; Dyerberg, J. Mortality from ischaemic heart disease and cerebrovascular disease in Greenland. Int. J. Epidemiol. 1988, 17, 514–519. [Google Scholar] [CrossRef]
- Stanhope, K.L. Sugar consumption, metabolic disease and obesity: The state of the controversy Critical Reviews in Clinical. Lab. Sci. 2016, 53, 52–67. [Google Scholar] [CrossRef]
- Freeman, C.R.; Zehra, A.; Ramirez, V.; Wiers, C.E.; Volkow, N.D.; Wang, G. Impact of sugar on the body, brain, and behavior. Front. Biosci. 2018, 23, 2255–2266. [Google Scholar]
- Yamori, Y.; Sagara, M.; Arai, Y.; Kobayashi, H.; Kishimoto, K.; Matsuno, K.; Mori, H.; Mori, M. Correction: Soy and fish as features of the Japanese diet and cardiovascular disease risks. PLoS ONE 2017, 12, e0186533. [Google Scholar] [CrossRef]
- Yamori, Y.; Sagara, M.; Arai, Y.; Kobayashi, H.; Kishimoto, K.; Matsuno, I.; Mori, H.; Mori, M. Cross-Sectional Inverse Association of Regular Soy Intake with Insulin Resistance in Japanese Elderly. J. Nutr. Gerontol. Geriatr. 2018, 37, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Alhussain, M.H.; Macdonald, I.A.; Taylor, M.A. Irregular meal-pattern effects on energy expenditure, metabolism, and appetite regulation: A randomized controlled trial in healthy normal-weight women. Am. J. Clin. Nutr. 2016, 104, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Alhussain, M.H.; Macdonald, I.A.; Taylor, M.A. Impact of isoenergetic intake of irregular meal patterns on thermogenesis, glucose metabolism, and appetite: A randomized controlled trial. Am. J. Clin. Nutr. 2022, 115, 284–297. [Google Scholar] [CrossRef]
- Pot, G.K.; Almoosawi, S.; Stephen, A.M. Meal irregularity and cardiometabolic consequences: Results from observational and intervention studies. Proc. Nutr. Soc. 2016, 75, 475–486. [Google Scholar] [CrossRef]
- Schlüter, N.; Groß, P. Special aspects of nutrition in elderly. Swiss Dent. J. 2019, 129, 929–936. [Google Scholar]
- Melzer, T.M.; Manosso, L.M.; Yau, S.; Gil-Mohapel, J.; Brocardo, P.S. In Pursuit of Healthy Aging: Effects of Nutrition on Brain Function. Int. J. Mol. Sci. 2021, 22, 5026. [Google Scholar] [CrossRef] [PubMed]
- Piernas, C.; Popkin, B.M. Snacking increased among U.S. adults between 1977 and 2006. J. Nutr. 2010, 140, 325–332. [Google Scholar] [CrossRef]
- Piernas, C.; Popkin, B.M. Trends in snacking among U.S. children. Health Aff. 2010, 29, 398–404. [Google Scholar] [CrossRef]
- Njike, V.Y.; Smith, T.M.; Shuval, O.; Shuval, K.; Edshteyn, I.; Kalantari, V.; Yaroch, A.L. Snack Food, Satiety, and Weight. Adv. Nutr. 2016, 7, 866–878. [Google Scholar] [CrossRef]
- Kuwahara, M.; Kim, H.; Ozaki, M.; Nanba, T.; Chijiki, H.; Fukazawa, M.; Okubo, J.; Mineshita, Y.; Takahashi, M.; Shibata, S. Consumption of Biscuits with a Beverage of Mulberry or Barley Leaves in the Afternoon Prevents Dinner-Induced High, but Not Low, Increases in Blood Glucose among Young Adults. Nutrients 2020, 12, 1580. [Google Scholar] [CrossRef]
- Tremblay, A.; Bellisle, F. Nutrients, satiety, and control of energy intake. Appl. Physiol. Nutr. Metab. 2015, 40, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Melby, M.K.; Takeda, W. Lifestyle constraints, not inadequate nutrition education, cause gap between breakfast ideals and realities among Japanese in Tokyo. Appetite 2014, 72, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Roshanmehr, F.; Tahara, Y.; Makino, S.; Tada, A.; Abe, N.; Michie, M.; Shibata, S. Association of Japanese Breakfast Intake with Macro- and Micronutrients and Morning Chronotype. Nutrients 2022, 14, 3496. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T. The integration of school nutrition program into health promotion and prevention of lifestyle-related diseases in Japan. Asia Pac. J. Clin. Nutr. 2008, 17, 349–351. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).