Vitamin D Status for Chinese Children and Adolescents in CNNHS 2016–2017
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethics
2.2. Data Collection, Body Measurement and Blood Sample Detection
2.3. Data Collection and Definition
2.4. Data Analyses
3. Results
3.1. Basic Characteristics
3.2. Vitamin D Nutritional Status
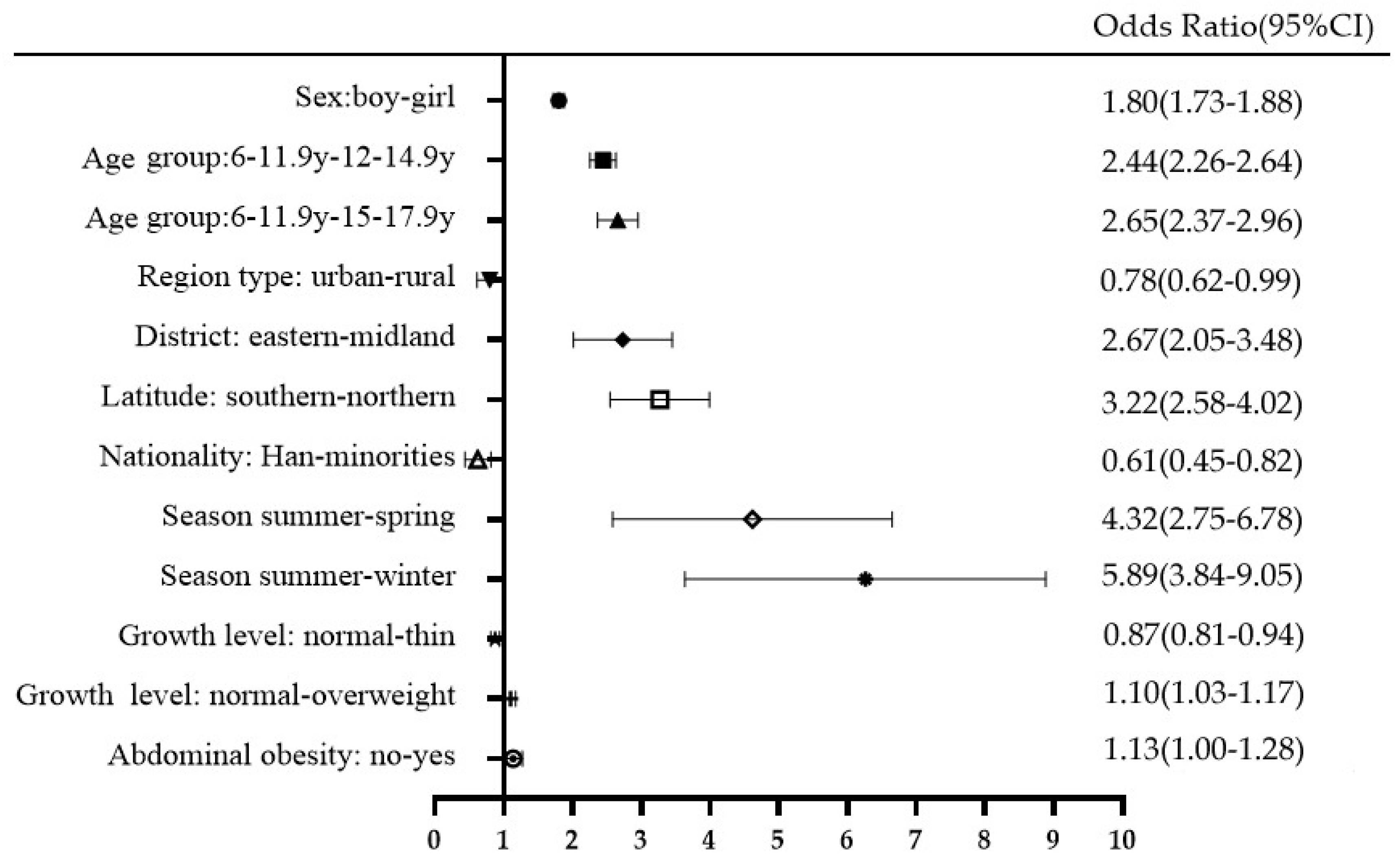
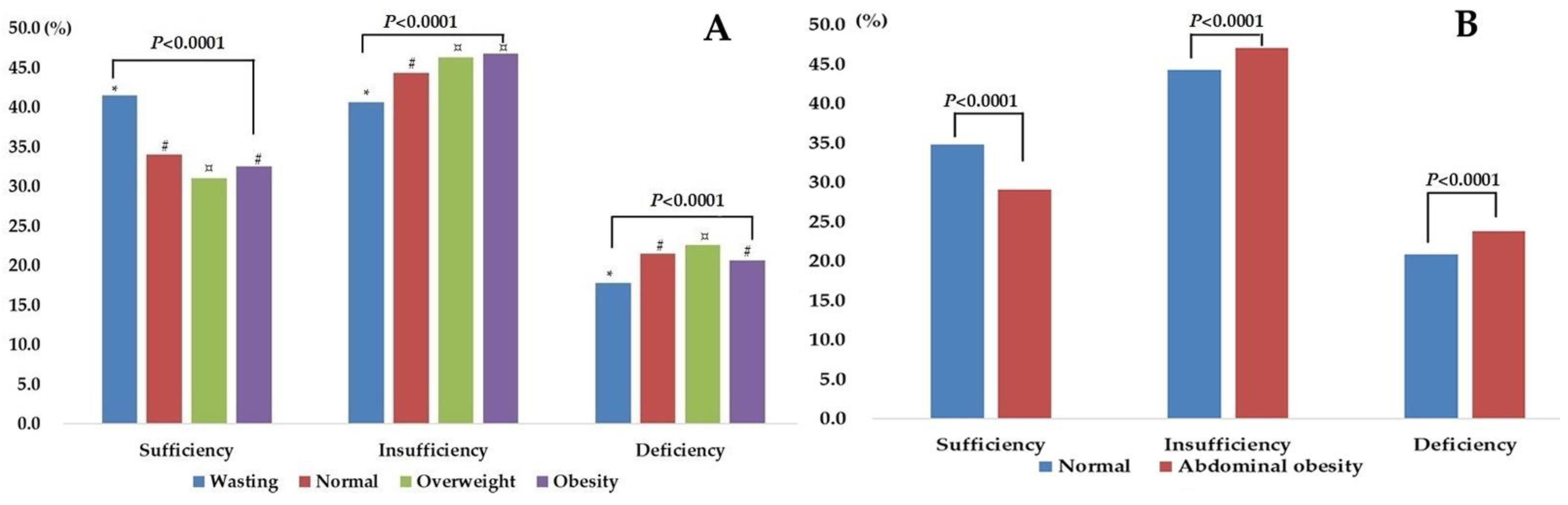
3.3. Risk Factors of Vitamin D Inadequacy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid. Biochem. 2014, 144, 138–145. [Google Scholar] [CrossRef]
- Motiwala, S.R.; Wang, T.J. Vitamin D and Cardiovascular Risk. Curr. Hypertens. Rep. 2012, 14, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Feldman, D.; Krishnan, A.V.; Swami, S.; Giovannucci, E.; Feldman, B.J. The role of vitamin D in reducing cancer risk and progression. Nat. Rev. Cancer 2014, 14, 342–357. [Google Scholar] [CrossRef] [PubMed]
- Aranow, C. Vitamin D and the Immune System. J. Investig. Med. 2011, 59, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Abrams, S.A.; Aloia, J.; Bergeron, G.; Bourassa, M.W.; Brown, K.H.; Calvo, M.S.; Cashman, K.D.; Combs, G.; De-Regil, L.M.; et al. Global prevalence and disease burden of vitamin D deficiency: A roadmap for action in low- and middle-income countries. Ann. N. Y. Acad. Sci. 2018, 1430, 44–79. [Google Scholar] [CrossRef]
- Schoor, N.V.; Lips, P. Global Overview of Vitamin D Status. Endocrinol. Metab. Clin. N. Am. 2017, 46, 845–870. [Google Scholar] [CrossRef]
- Binkley, N.; Dawson-Hughes, B.; Durazo-Arvizu, R.; Thamm, M.; Tian, L.; Merkel, J.; Jones, J.; Carter, G.; Sempos, C. Vitamin D measurement standardization: The way out of the chaos. J. Steroid Biochem. Mol. Biol. 2016, 173, 117–121. [Google Scholar] [CrossRef]
- Ross, A.C.; Taylor, C.L.; Yaktine, A.L.; Del Valle, H.B. Dietary Reference Intakes for Calcium and Vitamin D; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellof, M.; Fewtrell, M.; Hojsak, I.; Mihatsch, W.; Molgaard, C.; Shamir, R.; et al. Vitamin D in the Healthy European Paediatric Population. J. Craniofacial Surg. 2013, 56, 692–701. [Google Scholar] [CrossRef]
- Ding, G. Tracking New Challenges of Nutrition Transition and Developing Specific Strategies to Promote Healthy China. China CDC Wkly. 2021, 3, 179–180. [Google Scholar] [CrossRef]
- Shi, J.; He, L.; Yu, D.; Ju, L.; Guo, Q.; Piao, W.; Xu, X.; Zhao, L.; Yuan, X.; Cao, Q.; et al. Prevalence and Correlates of Metabolic Syndrome and Its Components in Chinese Children and Adolescents Aged 7–17: The China National Nutrition and Health Survey of Children and Lactating Mothers from 2016–2017. Nutrients 2022, 14, 3348. [Google Scholar] [CrossRef]
- Ma, X.W. China Health Statistics Yearbook in 2018; China Union Medical University Press: Beijing, China, 2018. [Google Scholar]
- China CDC. Workbook of China National Nutrition and Health Survey of Children and Lactating Mothers (2016–2017); China CDC: Beijing, China, 2016; Unpublished Work.
- WS/T456-2014; Screening Standard for Malnutrition of School-Age Children and Adolescents. National Health Commission of People’s Republic of China: Beijing, China, 2014.
- WS/T611-2018; High Waist Circumference Screening Threshold among Children and Adolescents Aged 7–17 Years. National Health and Family Planning Commission of People’s Republic of China: Beijing, China, 2018.
- WS/T677-2020; Method for Vitamin D Deficiency Screening. National Health Commission of People’s Republic of China: Beijing, China, 2018.
- Hu, Y.; Chen, J.; Wang, R.; Li, M.; Yun, C.; Li, W.; Yang, Y.; Piao, J.; Yang, X.; Yang, L. Vitamin D Nutritional Status and Its Related Factors for Chinese Children and Adolescents in 2010–2012. Nutrients 2017, 9, 1024. [Google Scholar] [CrossRef] [PubMed]
- Ouweland, J.M.V.D.; Beijers, A.M.; Demacker, P.N.; van Daal, H. Measurement of 25-OH-vitamin D in human serum using liquid chromatography tandem-mass spectrometry with comparison to radioimmunoassay and automated immunoassay. J. Chromatogr. B 2010, 878, 1163–1168. [Google Scholar] [CrossRef] [PubMed]
- Yun, C.; Chen, J.; Yang, C.; Li, Y.; Piao, J.; Yang, X. Comparison of two 25-hydroxyvitamin D immunoassays to liquid chromatography–tandem mass spectrometry in assessing samples from the Chinese population. Clin. Chim. Acta 2015, 448, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Wang, R.; Mao, D.; Chen, J.; Li, M.; Li, W.; Yang, Y.; Zhao, L.; Zhang, J.; Piao, J.; et al. Vitamin D Nutritional Status of Chinese Pregnant Women, Comparing the Chinese National Nutrition Surveillance (CNHS) 2015–2017 with CNHS 2010–2012. Nutrients 2021, 13, 2237. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Hong, I.Y.; Chung, J.W.; Choi, H.S. Vitamin D status in South Korean population: Seven-year trend from the KNHANES. Medicine 2018, 97, e11032. [Google Scholar] [CrossRef] [PubMed]
- Ritu, G.; Gupta, A. Vitamin D Deficiency in India: Prevalence, Causalities and Interventions. Nutrients 2014, 6, 729–775. [Google Scholar] [CrossRef]
- Khadilkar, A.; Kajale, N.; Oza, C.; Oke, R.; Gondhalekar, K.; Patwardhan, V.; Khadilkar, V.; Mughal, Z.; Padidela, R. Vitamin D status and determinants in Indian children and adolescents: A multicentre study. Sci. Rep. 2022, 12, 16790. [Google Scholar] [CrossRef]
- Schleicher, R.L.; Sternberg, M.R.; Lacher, D.A.; Sempos, C.T.; Looker, A.C.; Durazo-Arvizu, R.A.; Yetley, E.A.; Chaudhary-Webb, M.; Maw, K.L.; Pfeiffer, C.M.; et al. The vitamin D status of the US population from 1988 to 2010 using standardized serum concentrations of 25-hydroxyvitamin D shows recent modest increases. Am. J. Clin. Nutr. 2016, 104, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Herrick, K.A.; Storandt, R.; Afful, J.; Pfeiffer, C.M.; Schleicher, R.L.; Gahche, J.J.; Potischman, N. Vitamin D status in the United States, 2011–2014. Am. J. Clin. Nutr. 2019, 110, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Berger, C.; Greene-Finestone, L.S.; Langsetmo, L.; Kreiger, N.; Joseph, L.; Kovacs, C.; Richards, J.B.; Hidiroglou, N.; Sarafin, K.; Davison, K.S.; et al. Temporal trends and determinants of longitudinal change in 25-hydroxyvitamin D and parathyroid hormone levels. J. Bone Miner. Res. 2012, 27, 1381–1389. [Google Scholar] [CrossRef] [PubMed]
- Dudenkov, D.V.; Yawn, B.P.; Oberhelman, S.S.; Fischer, P.R.; Singh, R.J.; Cha, S.S.; Maxson, J.A.; Quigg, S.M.; Thacher, T. Changing Incidence of Serum 25-Hydroxyvitamin D Values Above 50 ng/mL: A 10-Year Population-Based Study. Mayo Clin. Proc. 2015, 90, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Calvo, M.S.; Whiting, S.J. Survey of current vitamin D food fortification practices in the United States and Canada. J. Steroid Biochem. Mol. Biol. 2013, 136, 211–213. [Google Scholar] [CrossRef]
- Fulgoni, V.L., 3rd; Keast, D.R.; Bailey, R.L.; Dwyer, J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J. Nutr. 2011, 141, 1847–1854. [Google Scholar] [CrossRef]
- Isa, H.; Almaliki, M.; Alsabea, A.; Mohamed, A. Vitamin D deficiency in healthy children in Bahrain: Do gender and age matter? East. Mediterr. Health J. 2020, 26, 260–267. [Google Scholar] [CrossRef]
- Schleicher, R.L.; Sternberg, M.R.; Looker, A.C.; Yetley, E.A.; Lacher, D.A.; Sempos, C.T.; Taylor, C.L.; Durazo-Arvizu, R.A.; Maw, K.L.; Chaudhary-Webb, M.; et al. National Estimates of Serum Total 25-Hydroxyvitamin D and Metabolite Concentrations Measured by Liquid Chromatography–Tandem Mass Spectrometry in the US Population during 2007–2010. J. Nutr. 2016, 146, 1051–1061. [Google Scholar] [CrossRef]
- Agarwal, K.S.; Mughal, M.Z.; Upadhyay, P.; Berry, J.L.; Mawer, E.B.; Puliyel, J.M. The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi, India. Arch. Dis. Child. 2002, 87, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Vierucci, F.; Del Pistoia, M.; Fanos, M.; Gori, M.; Carlone, G.; Erba, P.; Massimetti, G.; Federico, G.; Saggese, G. Vitamin D status and predictors of hypovitaminosis D in Italian children and adolescents: A cross-sectional study. Eur. J. Pediatr. 2013, 172, 1607–1617. [Google Scholar] [CrossRef] [PubMed]
- Lian, X.Y.; Meng, Z.D. Relationship between quantity of illumination and human vitamin D concentration and bone mineral density in different region. Chin. J. Osteoporos. 2012, 18, 183–189. [Google Scholar]
- Karacan, M.; Usta, A.; Biçer, S.; Baktir, G.; İpek Gündogan, G.; Sancakli Usta, C.; Akinci, G. Serum vitamin D levels in healthy urban population at reproductive age: Effects of age, gender and season. Cent. Eur. J. Public Health 2020, 28, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.L.; Wang, H.Y.; Wen, H.K.; Tao, H.Q.; Zhao, X.W. Vitamin D status among infants, children, and adolescents in southeastern China. J. Zhejiang Univ.-Sci. B (Biomed. Biotechnol.) 2016, 17, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Arimitsu, T.; Hara-Isono, K.; Ikeda, K. Seasonal variation in vitamin D status of Japanese infants starts to emerge at 2 months of age: A retrospective cohort study. Br. J. Nutr. 2022, 26, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.C.; Yalamanchili, V.; Smith, L.M. The effect of vitamin D supplementation on serum 25(OH)D in thin and obese women. J. Steroid Biochem. Mol. Biol. 2013, 136, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Rojas, L.Z.; Quintero-Lesmes, D.C.; Gamboa-Delgado, E.M.; Guio, E.; Serrano, N.C. Prevalence of vitamin D status and its association with overweight or obesity in a population of Colombian children and adolescents. J. Nutr. Sci. 2020, 9, e55. [Google Scholar] [CrossRef] [PubMed]
- Plesner, J.L.; Dahl, M.; Fonvig, C.E.; Nielsen, T.R.H.; Kloppenborg, J.T.; Pedersen, O.; Hansen, T.; Holm, J.-C. Obesity is associated with vitamin D deficiency in Danish children and adolescents. J. Pediatr. Endocrinol. Metab. 2017, 31, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Hajhashemy, Z.; Lotfi, K.; Heidari, Z.; Saneei, P. Serum Vitamin D Levels in Relation to Abdominal Obesity in Children and Adolescents: A Systematic Review and Dose-Response Meta-Analysis. Front. Nutr. 2022, 9, 806459. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | No. | 25(OH)D Concentration (ng/mL) | Vitamin D Nutritional Status (%, 95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Median (P25–P75) | p Value | Sufficient | Insufficient | Deficiency | p Value | ||
| Total | 64,391 | 17.70 (13.20–22.68) | / | 34.02 (31.09–36.94) | 44.69 (43.14–46.24) | 21.29 (19.00–23.59) | / |
| Sex | <0.0001 | <0.0001 | |||||
| Boys | 32,168 | 18.70 (14.10–23.80) | 39.58 (36.43–42.74) | 43.34 (41.53–45.15) | 17.08 (15.00–19.15) | ||
| Girls | 32,223 | 16.60 (12.40–21.40) | 28.01 (25.24–30.76) | 46.14 (44.54–47.74) | 25.85 (23.23–28.48) | ||
| Age group | <0.0001 | <0.0001 | |||||
| 6–11.9 y | 35,780 | 19.20 (14.60–24.10) c | 43.53 (40.25–46.81) | 42.59 (40.57–44.60) | 13.88 (12.05–15.72) | ||
| 12–14.9 y | 15,801 | 15.90 (11.90–20.70) b | 27.11 (24.13–30.08) | 46.62 (44.81–48.44) | 26.27 (23.43–29.11) | ||
| 15–17.9 y | 12,810 | 15.50 (11.60–20.40) a | 26.69 (23.63–29.74) | 45.89 (43.99–47.79) | 27.42 (24.38–30.47) | ||
| Region type | <0.0001 | 0.51 | |||||
| Urban | 30,703 | 17.40 (13.00–22.30) | 32.66 (28.44–36.88) | 45.15 (42.94–47.36) | 22.19 (18.80–25.59) | ||
| Rural | 33,688 | 17.90 (13.30–23.00) | 35.36 (31.32–39.40) | 44.24 (42.07–46.40) | 20.40 (17.32–23.48) | ||
| District | <0.0001 | <0.0001 | |||||
| Eastern | 23,386 | 18.90 (14.10–23.82) c | 39.77 (34.87–44.67) | 42.61 (40.16–45.06) | 17.62 (14.27–20.97) | ||
| Midlands | 20,015 | 15.70 (11.90–20.30) a | 22.84 (19.04–26.65) | 48.46 (45.90–51.01) | 28.70 (24.39–33.02) | ||
| Western | 20,990 | 18.30 (13.70–23.40) b | 38.15 (32.72–43.58) | 43.47 (40.58–46.35) | 18.38 (14.47–22.29) | ||
| Latitude | <0.0001 | <0.0001 | |||||
| Northern | 27,677 | 15.12 (11.30–20.00) | 22.71 (19.42–25.99) | 45.62 (44.02–47.22) | 31.67 (28.27–35.08) | ||
| Southern | 36,714 | 19.48 (15.10–24.18) | 43.41 (39.44–47.38) | 43.92 (41.42–46.42) | 12.67 (10.45–14.89) | ||
| Ethnicity | <0.0001 | 0.0004 | |||||
| Han | 57,660 | 17.48 (13.03–22.40) | 32.84 (29.92–35.76) | 45.24 (43.70–46.78) | 21.92 (19.56–24.28) | ||
| Minorities | 6731 | 19.60 (14.50–24.50) | 44.35 (36.98–51.71) | 39.86 (35.53–44.20) | 15.79 (10.90–20.69) | ||
| Growth level | <0.0001 | <0.0001 | |||||
| Thin | 6492 | 19.00 (14.00–24.30) c | 41.52 (37.61–45.44) | 40.66 (38.18–43.14) | 17.82 (15.34–20.30) | ||
| Normal | 44,840 | 17.60 (13.10–22.60) b | 34.08 (31.14–37.03) | 44.39 (42.82–45.96) | 21.53 (19.18–23.88) | ||
| Overweight | 7191 | 17.20 (13.00–21.80) a | 31.06 (28.01–34.10) | 46.33 (44.52–48.15) | 22.61 (20.08–25.14) | ||
| Obesity | 5868 | 17.50 (13.10–22.31) b | 32.52 (29.15–35.89) | 46.79 (44.72–48.85) | 20.69 (17.98–23.41) | ||
| Abdominal obesity | <0.0001 | <0.0001 | |||||
| No | 58,384 | 17.80 (13.21–22.80) | 34.82 (31.87–37.78) | 44.31 (42.74–45.88) | 20.87 (18.61–23.12) | ||
| Yes | 6007 | 16.60 (12.50–21.50) | 28.85 (25.61–32.08) | 47.12 (45.02–49.22) | 24.03 (20.94–27.12) | ||
| Season * | <0.0001 | <0.0001 | |||||
| Spring | 11,545 | 17.30 (12.90–22.40) b | 32.33 (25.95–38.71) | 45.14 (41.59–48.70) | 22.53 (17.26–27.79) | ||
| Summer | 2361 | 21.70 (17.40–26.20) d | 55.02 (46.39–63.64) | 38.46 (32.10–44.82) | 6.52 (3.24–9.81) | ||
| Autumn | 19,223 | 19.20 (14.80–23.97) c | 41.70 (37.39–46.02) | 45.20 (42.32–48.07) | 13.10 (10.70–15.51) | ||
| Winter | 31,262 | 16.50 (12.19–21.50) a | 28.31 (24.39–32.23) | 44.68 (42.65–46.72) | 27.01 (23.70–30.31) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, Y.; Jiang, S.; Lu, J.; Yang, Z.; Yang, X.; Yang, L. Vitamin D Status for Chinese Children and Adolescents in CNNHS 2016–2017. Nutrients 2022, 14, 4928. https://doi.org/10.3390/nu14224928
Hu Y, Jiang S, Lu J, Yang Z, Yang X, Yang L. Vitamin D Status for Chinese Children and Adolescents in CNNHS 2016–2017. Nutrients. 2022; 14(22):4928. https://doi.org/10.3390/nu14224928
Chicago/Turabian StyleHu, Yichun, Shan Jiang, Jiaxi Lu, Zhenyu Yang, Xiaoguang Yang, and Lichen Yang. 2022. "Vitamin D Status for Chinese Children and Adolescents in CNNHS 2016–2017" Nutrients 14, no. 22: 4928. https://doi.org/10.3390/nu14224928
APA StyleHu, Y., Jiang, S., Lu, J., Yang, Z., Yang, X., & Yang, L. (2022). Vitamin D Status for Chinese Children and Adolescents in CNNHS 2016–2017. Nutrients, 14(22), 4928. https://doi.org/10.3390/nu14224928






