The Effect of Healthy Lifestyle Strategies on the Management of Insulin Resistance in Children and Adolescents with Obesity: A Narrative Review
Abstract
:1. Introduction
2. Methods
3. Childhood Obesity, Insulin Resistance and Adipose Tissue
3.1. Childhood Obesity and Insulin Resistance
3.2. Adipose Tissue and Insulin Resistance
4. Exercise Benefits on Insulin Sensitivity
4.1. Benefits of Exercise on Insulin Resistance
4.2. Molecular Effects of the Exercise on Insulin Resistance
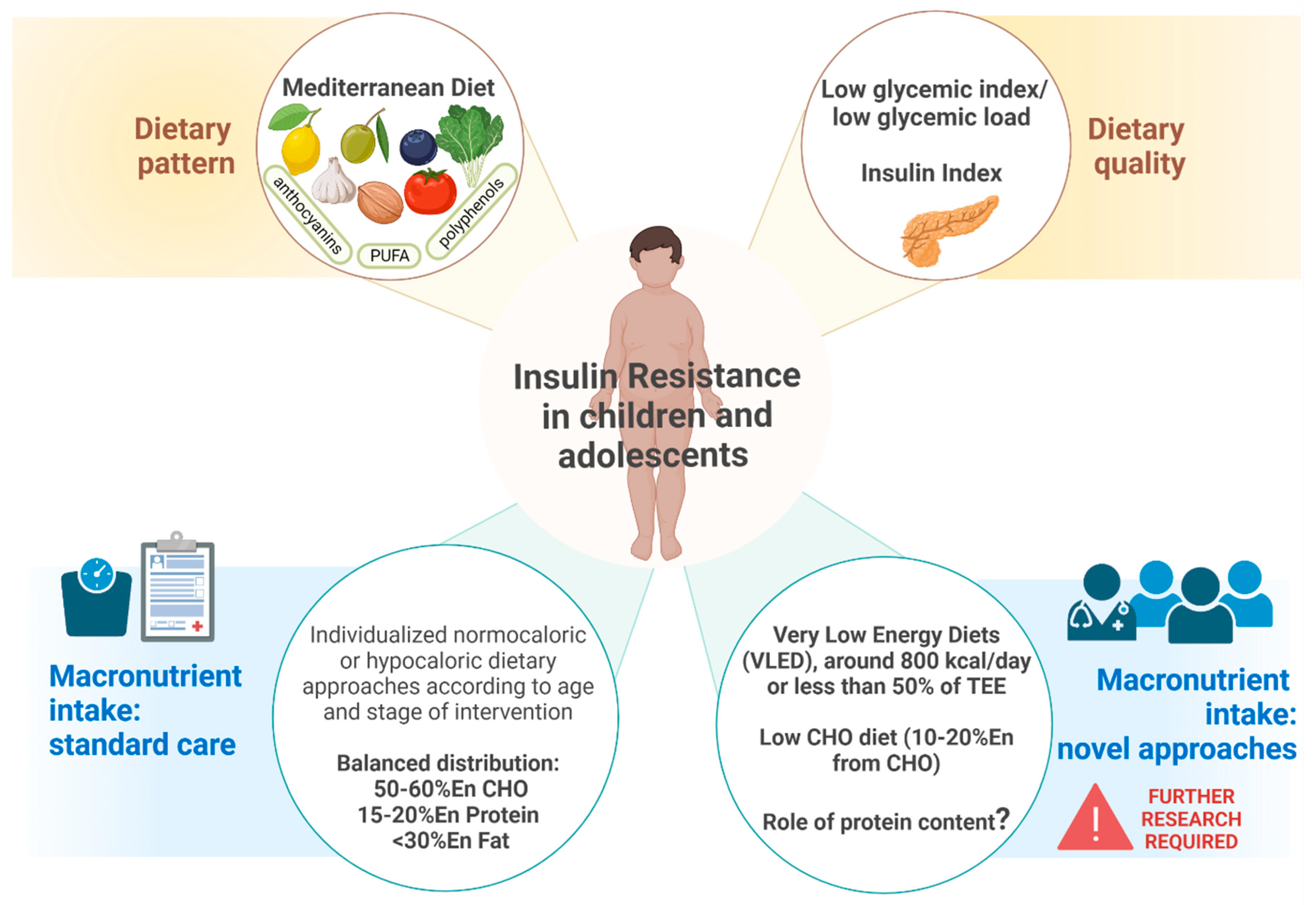
5. Nutritional Strategies for Modulation of Insulin Resistance
5.1. Dietary Approach
5.2. Nutritional Supplementation
5.2.1. Probiotics
5.2.2. Fiber
5.2.3. Long Chain Polyunsaturated Fatty Acids
5.2.4. Vitamin D
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weiss, R.; Kaufman, F.R. Metabolic Complications of Childhood Obesity: Identifying and Mitigating the Risk. Diabetes Care 2008, 31 (Suppl. 2), S310–S316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiarelli, F.; Marcovecchio, M.L. Insulin Resistance and Obesity in Childhood. Eur. J. Endocrinol. 2008, 159, S67–S74. [Google Scholar] [CrossRef] [Green Version]
- Tagi, V.M.; Chiarelli, F. Obesity and Insulin Resistance in Children. Curr. Opin. Pediatr. 2020, 32, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Caprio, S. Diabetes and Insulin Resistance in Pediatric Obesity. Pediatr. Clin. N. Am. 2011, 58, 1355–1361. [Google Scholar] [CrossRef]
- Fasshauer, M.; Blüher, M. Adipokines in Health and Disease. Trends Pharmacol. Sci. 2015, 36, 461–470. [Google Scholar] [CrossRef]
- Ohashi, K.; Shibata, R.; Murohara, T.; Ouchi, N. Role of Anti-Inflammatory Adipokines in Obesity-Related Diseases. Trends Endocrinol. Metab. TEM 2014, 25, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.T.; Denniss, A.R. An Introduction to Writing Narrative and Systematic Reviews—Tasks, Tips and Traps for Aspiring Authors. Heart Lung Circ. 2018, 27, 893–898. [Google Scholar] [CrossRef] [Green Version]
- Caprio, S.; Santoro, N.; Weiss, R. Childhood Obesity and the Associated Rise in Cardiometabolic Complications. Nat. Metab. 2020, 2, 223–232. [Google Scholar] [CrossRef]
- Shulman, G.I. Ectopic Fat in Insulin Resistance, Dyslipidemia, and Cardiometabolic Disease. N. Engl. J. Med. 2014, 371, 1131–1141. [Google Scholar] [CrossRef]
- Kim, G.W.; Lin, J.E.; Blomain, E.S.; Waldman, S.A. Antiobesity Pharmacotherapy: New Drugs and Emerging Targets. Clin. Pharmacol. Ther. 2013, 95, 53–66. [Google Scholar] [CrossRef]
- Marson, E.C.; Delevatti, R.S.; Prado, A.K.G.; Netto, N.; Kruel, L.F.M. Effects of Aerobic, Resistance, and Combined Exercise Training on Insulin Resistance Markers in Overweight or Obese Children and Adolescents: A Systematic Review and Meta-Analysis. Prev. Med. 2016, 93, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.; Liu, W.; Zhao, X.; Li, S.; Yu, C. Effect of Supervised Exercise Intervention on Metabolic Risk Factors and Physical Fitness in Chinese Obese Children in Early Puberty. Obes. Rev. 2008, 9, 135–141. [Google Scholar] [CrossRef]
- Castorani, V.; Polidori, N.; Giannini, C.; Blasetti, A.; Chiarelli, F. Insulin Resistance and Type 2 Diabetes in Children. Ann. Pediatr. Endocrinol. Metab. 2020, 25, 217–226. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Tobin, J.D.; Andres, R. Glucose Clamp Technique: A Method for Quantifying Insulin Secretion and Resistance. Am. J. Physiol. Endocrinol. Metab. 1979, 237, E214. [Google Scholar] [CrossRef] [PubMed]
- Cutfield, W.S.; Jefferies, C.A.; Jackson, W.E.; Robinson, E.M.; Hofman, P.L. Evaluation of HOMA and QUICKI as Measures of Insulin Sensitivity in Prepubertal Children: HOMA and QUICKI. Pediatr. Diabetes 2003, 4, 119–125. [Google Scholar] [CrossRef]
- Kurtoğlu, S.; Hatipoğlu, N.; Mazıcıoğlu, M.; Kendirci, M.; Keskin, M.; Kondolot, M. Insulin Resistance in Obese Children and Adolescents: HOMA-IR Cut-Off Levels in the Prepubertal and Pubertal Periods—Original Article. J. Clin. Res. Pediatr. Endocrinol. 2010, 2, 100–106. [Google Scholar] [CrossRef]
- Calcaterra, V.; Montalbano, C.; de Silvestri, A.; Pelizzo, G.; Regalbuto, C.; Paganelli, V.; Albertini, R.; Cave, F.D.; Larizza, D.; Cena, H. Triglyceride Glucose Index as a Surrogate Measure of Insulin Sensitivity in a Caucasian Pediatric Population. J. Clin. Res. Pediatr. Endocrinol. 2020. [Google Scholar] [CrossRef]
- Bambace, C.; Pedrotti, M.; Ferrara, G.; Zamboni, M. Obesità, Tessuto Adiposo e Infiammazione. Biochim. Clin. 2011, 35, 275. [Google Scholar]
- Choy, E.H.S.; Panayi, G.S. Cytokine Pathways and Joint Inflammation in Rheumatoid Arthritis. N. Engl. J. Med. 2001, 344, 907–916. [Google Scholar] [CrossRef]
- Kahn, S.E.; Hull, R.L.; Utzschneider, K.M. Mechanisms Linking Obesity to Insulin Resistance and Type 2 Diabetes. Nature 2006, 444, 840–846. [Google Scholar] [CrossRef]
- Biddinger, S.B.; Kahn, C.R. From Mice to Men: Insights into the Insulin Resistance Syndromes. Annu. Rev. Physiol. 2006, 68, 123–158. [Google Scholar] [CrossRef] [PubMed]
- Attie, A.D.; Scherer, P.E. Adipocyte Metabolism and Obesity. J. Lipid Res. 2009, 50, S395–S399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory Links between Obesity and Metabolic Disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olefsky, J.M.; Glass, C.K. Macrophages, Inflammation, and Insulin Resistance. Annu. Rev. Physiol. 2010, 72, 219–246. [Google Scholar] [CrossRef]
- Shoelson, S.E.; Herrero, L.; Naaz, A. Obesity, Inflammation, and Insulin Resistance. Gastroenterology 2007, 132, 2169–2180. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2009, 32, S62–S67. [CrossRef] [Green Version]
- White, M.F. Insulin Signaling in Health and Disease. Science 2003, 302, 1710–1711. [Google Scholar] [CrossRef] [Green Version]
- Lennarz, W.J.; Plitch, P.F. (Eds.) Insulin Receptor Family. In Encyclopedia of Biological Chemistry; Elsevier: Amsterdam, The Netherlands, 2013; pp. 436–440. ISBN 978-0-12-378630-2. [Google Scholar]
- White, M.F. IRS Proteins and the Common Path to Diabetes. Am. J. Physiol. Endocrinol. Metab. 2002, 283, E413–E422. [Google Scholar] [CrossRef] [Green Version]
- Ye, J.; Gimble, J.M. Regulation of Stem Cell Differentiation in Adipose Tissue by Chronic Inflammation. Clin. Exp. Pharmacol. Physiol. 2011, 38, 872–878. [Google Scholar] [CrossRef] [Green Version]
- Ye, J. Regulation of PPARgamma Function by TNF-Alpha. Biochem. Biophys. Res. Commun. 2008, 374, 405–408. [Google Scholar] [CrossRef] [Green Version]
- Ye, J. Role of Insulin in the Pathogenesis of Free Fatty Acid-Induced Insulin Resistance in Skeletal Muscle. Endocr. Metab. Immune Disord. Drug Targets 2007, 7, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Tilg, H.; Moschen, A.R. Adipocytokines: Mediators Linking Adipose Tissue, Inflammation and Immunity. Nat. Rev. Immunol. 2006, 6, 772–783. [Google Scholar] [CrossRef] [PubMed]
- Hotamisligil, G.S. Inflammation and Metabolic Disorders. Nature 2006, 444, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Hirosumi, J.; Tuncman, G.; Chang, L.; Görgün, C.Z.; Uysal, K.T.; Maeda, K.; Karin, M.; Hotamisligil, G.S. A Central Role for JNK in Obesity and Insulin Resistance. Nature 2002, 420, 333–336. [Google Scholar] [CrossRef]
- Aguirre, V.; Uchida, T.; Yenush, L.; Davis, R.; White, M.F. The C-Jun NH(2)-Terminal Kinase Promotes Insulin Resistance during Association with Insulin Receptor Substrate-1 and Phosphorylation of Ser(307). J. Biol. Chem. 2000, 275, 9047–9054. [Google Scholar] [CrossRef] [Green Version]
- Yuan, M.; Konstantopoulos, N.; Lee, J.; Hansen, L.; Li, Z.W.; Karin, M.; Shoelson, S.E. Reversal of Obesity- and Diet-Induced Insulin Resistance with Salicylates or Targeted Disruption of Ikkbeta. Science 2001, 293, 1673–1677. [Google Scholar] [CrossRef]
- Arkan, M.C.; Hevener, A.L.; Greten, F.R.; Maeda, S.; Li, Z.-W.; Long, J.M.; Wynshaw-Boris, A.; Poli, G.; Olefsky, J.; Karin, M. IKK-Beta Links Inflammation to Obesity-Induced Insulin Resistance. Nat. Med. 2005, 11, 191–198. [Google Scholar] [CrossRef]
- Kaneto, H.; Nakatani, Y.; Miyatsuka, T.; Kawamori, D.; Matsuoka, T.; Matsuhisa, M.; Kajimoto, Y.; Ichijo, H.; Yamasaki, Y.; Hori, M. Possible Novel Therapy for Diabetes with Cell-Permeable JNK-Inhibitory Peptide. Nat. Med. 2004, 10, 1128–1132. [Google Scholar] [CrossRef]
- Kim, J.K.; Kim, Y.J.; Fillmore, J.J.; Chen, Y.; Moore, I.; Lee, J.; Yuan, M.; Li, Z.W.; Karin, M.; Perret, P.; et al. Prevention of Fat-Induced Insulin Resistance by Salicylate. J. Clin. Investig. 2001, 108, 437–446. [Google Scholar] [CrossRef]
- Kamei, N.; Tobe, K.; Suzuki, R.; Ohsugi, M.; Watanabe, T.; Kubota, N.; Ohtsuka-Kowatari, N.; Kumagai, K.; Sakamoto, K.; Kobayashi, M.; et al. Overexpression of Monocyte Chemoattractant Protein-1 in Adipose Tissues Causes Macrophage Recruitment and Insulin Resistance. J. Biol. Chem. 2006, 281, 26602–26614. [Google Scholar] [CrossRef] [Green Version]
- Weisberg, S.P.; Hunter, D.; Huber, R.; Lemieux, J.; Slaymaker, S.; Vaddi, K.; Charo, I.; Leibel, R.L.; Ferrante, A.W. CCR2 Modulates Inflammatory and Metabolic Effects of High-Fat Feeding. J. Clin. Investig. 2006, 116, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Neels, J.G.; Olefsky, J.M. Inflamed Fat: What Starts the Fire? J. Clin. Investig. 2006, 116, 33–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suganami, T.; Nishida, J.; Ogawa, Y. A Paracrine Loop between Adipocytes and Macrophages Aggravates Inflammatory Changes: Role of Free Fatty Acids and Tumor Necrosis Factor Alpha. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 2062–2068. [Google Scholar] [CrossRef] [Green Version]
- Scott, T.; Owens, M.D. Thrombocytes Respond to Lipopolysaccharide through Toll-like Receptor-4, and MAP Kinase and NF-KappaB Pathways Leading to Expression of Interleukin-6 and Cyclooxygenase-2 with Production of Prostaglandin E2. Mol. Immunol. 2008, 45, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, C.N.; Bodzin, J.L.; Saltiel, A.R. Obesity Induces a Phenotypic Switch in Adipose Tissue Macrophage Polarization. J. Clin. Investig. 2007, 117, 175–184. [Google Scholar] [CrossRef] [Green Version]
- Fève, B.; Bastard, J.-P. The Role of Interleukins in Insulin Resistance and Type 2 Diabetes Mellitus. Nat. Rev. Endocrinol. 2009, 5, 305–311. [Google Scholar] [CrossRef]
- Hotamisligil, G.S. Mechanisms of TNF-Alpha-Induced Insulin Resistance. Exp. Clin. Endocrinol. Diabetes Off. J. Ger. Soc. Endocrinol. Ger. Diabetes Assoc. 1999, 107, 119–125. [Google Scholar] [CrossRef]
- Hotamisligil, G.S.; Shargill, N.S.; Spiegelman, B.M. Adipose Expression of Tumor Necrosis Factor-Alpha: Direct Role in Obesity-Linked Insulin Resistance. Science 1993, 259, 87–91. [Google Scholar] [CrossRef]
- Stephens, J.M.; Pekala, P.H. Transcriptional Repression of the C/EBP-Alpha and GLUT4 Genes in 3T3-L1 Adipocytes by Tumor Necrosis Factor-Alpha. Regulations Is Coordinate and Independent of Protein Synthesis. J. Biol. Chem. 1992, 267, 13580–13584. [Google Scholar] [CrossRef]
- Holland, W.L.; Bikman, B.T.; Wang, L.-P.; Yuguang, G.; Sargent, K.M.; Bulchand, S.; Knotts, T.A.; Shui, G.; Clegg, D.J.; Wenk, M.R.; et al. Lipid-Induced Insulin Resistance Mediated by the Proinflammatory Receptor TLR4 Requires Saturated Fatty Acid-Induced Ceramide Biosynthesis in Mice. J. Clin. Investig. 2011, 121, 1858–1870. [Google Scholar] [CrossRef] [Green Version]
- Schenk, S.; Saberi, M.; Olefsky, J.M. Insulin Sensitivity: Modulation by Nutrients and Inflammation. J. Clin. Investig. 2008, 118, 2992–3002. [Google Scholar] [CrossRef] [PubMed]
- Schmitz-Peiffer, C. Targeting Ceramide Synthesis to Reverse Insulin Resistance. Diabetes 2010, 59, 2351–2353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanda, H.; Tateya, S.; Tamori, Y.; Kotani, K.; Hiasa, K.; Kitazawa, R.; Kitazawa, S.; Miyachi, H.; Maeda, S.; Egashira, K.; et al. MCP-1 Contributes to Macrophage Infiltration into Adipose Tissue, Insulin Resistance, and Hepatic Steatosis in Obesity. J. Clin. Investig. 2006, 116, 1494–1505. [Google Scholar] [CrossRef]
- Winer, S.; Chan, Y.; Paltser, G.; Truong, D.; Tsui, H.; Bahrami, J.; Dorfman, R.; Wang, Y.; Zielenski, J.; Mastronardi, F.; et al. Normalization of Obesity-Associated Insulin Resistance through Immunotherapy. Nat. Med. 2009, 15, 921–929. [Google Scholar] [CrossRef] [PubMed]
- Winer, D.A.; Winer, S.; Shen, L.; Wadia, P.P.; Yantha, J.; Paltser, G.; Tsui, H.; Wu, P.; Davidson, M.G.; Alonso, M.N.; et al. B Cells Promote Insulin Resistance through Modulation of T Cells and Production of Pathogenic IgG Antibodies. Nat. Med. 2011, 17, 610–617. [Google Scholar] [CrossRef]
- DeFuria, J.; Belkina, A.C.; Jagannathan-Bogdan, M.; Snyder-Cappione, J.; Carr, J.D.; Nersesova, Y.R.; Markham, D.; Strissel, K.J.; Watkins, A.A.; Zhu, M.; et al. B Cells Promote Inflammation in Obesity and Type 2 Diabetes through Regulation of T-Cell Function and an Inflammatory Cytokine Profile. Proc. Natl. Acad. Sci. USA 2013, 110, 5133–5138. [Google Scholar] [CrossRef] [Green Version]
- Talukdar, S.; Oh, D.Y.; Bandyopadhyay, G.; Li, D.; Xu, J.; McNelis, J.; Lu, M.; Li, P.; Yan, Q.; Zhu, Y.; et al. Neutrophils Mediate Insulin Resistance in Mice Fed a High-Fat Diet through Secreted Elastase. Nat. Med. 2012, 18, 1407–1412. [Google Scholar] [CrossRef] [Green Version]
- Wu, D.; Molofsky, A.B.; Liang, H.-E.; Ricardo-Gonzalez, R.R.; Jouihan, H.A.; Bando, J.K.; Chawla, A.; Locksley, R.M. Eosinophils Sustain Adipose Alternatively Activated Macrophages Associated with Glucose Homeostasis. Science 2011, 332, 243–247. [Google Scholar] [CrossRef] [Green Version]
- Feuerer, M.; Herrero, L.; Cipolletta, D.; Naaz, A.; Wong, J.; Nayer, A.; Lee, J.; Goldfine, A.B.; Benoist, C.; Shoelson, S.; et al. Lean, but Not Obese, Fat Is Enriched for a Unique Population of Regulatory T Cells That Affect Metabolic Parameters. Nat. Med. 2009, 15, 930–939. [Google Scholar] [CrossRef]
- Cipolletta, D.; Feuerer, M.; Li, A.; Kamei, N.; Lee, J.; Shoelson, S.E.; Benoist, C.; Mathis, D. PPAR-γ Is a Major Driver of the Accumulation and Phenotype of Adipose Tissue Treg Cells. Nature 2012, 486, 549–553. [Google Scholar] [CrossRef] [Green Version]
- Lynch, L.; Nowak, M.; Varghese, B.; Clark, J.; Hogan, A.E.; Toxavidis, V.; Balk, S.P.; O’Shea, D.; O’Farrelly, C.; Exley, M.A. Adipose Tissue Invariant NKT Cells Protect against Diet-Induced Obesity and Metabolic Disorder through Regulatory Cytokine Production. Immunity 2012, 37, 574–587. [Google Scholar] [CrossRef]
- Wu, L.; Parekh, V.V.; Gabriel, C.L.; Bracy, D.P.; Marks-Shulman, P.A.; Tamboli, R.A.; Kim, S.; Mendez-Fernandez, Y.V.; Besra, G.S.; Lomenick, J.P.; et al. Activation of Invariant Natural Killer T Cells by Lipid Excess Promotes Tissue Inflammation, Insulin Resistance, and Hepatic Steatosis in Obese Mice. Proc. Natl. Acad. Sci. USA 2012, 109, E1143–E1152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mantell, B.S.; Stefanovic-Racic, M.; Yang, X.; Dedousis, N.; Sipula, I.J.; O’Doherty, R.M. Mice Lacking NKT Cells but with a Complete Complement of CD8+ T-Cells Are Not Protected against the Metabolic Abnormalities of Diet-Induced Obesity. PLoS ONE 2011, 6, e19831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ji, Y.; Sun, S.; Xu, A.; Bhargava, P.; Yang, L.; Lam, K.S.L.; Gao, B.; Lee, C.-H.; Kersten, S.; Qi, L. Activation of Natural Killer T Cells Promotes M2 Macrophage Polarization in Adipose Tissue and Improves Systemic Glucose Tolerance via Interleukin-4 (IL-4)/STAT6 Protein Signaling Axis in Obesity. J. Biol. Chem. 2012, 287, 13561–13571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohmura, K.; Ishimori, N.; Ohmura, Y.; Tokuhara, S.; Nozawa, A.; Horii, S.; Andoh, Y.; Fujii, S.; Iwabuchi, K.; Onoé, K.; et al. Natural Killer T Cells Are Involved in Adipose Tissues Inflammation and Glucose Intolerance in Diet-Induced Obese Mice. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 193–199. [Google Scholar] [CrossRef]
- Huh, J.Y.; Kim, J.I.; Park, Y.J.; Hwang, I.J.; Lee, Y.S.; Sohn, J.H.; Lee, S.K.; Alfadda, A.A.; Kim, S.S.; Choi, S.H.; et al. A Novel Function of Adipocytes in Lipid Antigen Presentation to INKT Cells. Mol. Cell. Biol. 2013, 33, 328–339. [Google Scholar] [CrossRef] [Green Version]
- Stephens, J.M.; Lee, J.; Pilch, P.F. Tumor Necrosis Factor-Alpha-Induced Insulin Resistance in 3T3-L1 Adipocytes Is Accompanied by a Loss of Insulin Receptor Substrate-1 and GLUT4 Expression without a Loss of Insulin Receptor-Mediated Signal Transduction. J. Biol. Chem. 1997, 272, 971–976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheung, A.T.; Ree, D.; Kolls, J.K.; Fuselier, J.; Coy, D.H.; Bryer-Ash, M. An In Vivo Model for Elucidation of the Mechanism of Tumor Necrosis Factor-Alpha (TNF-Alpha)-Induced Insulin Resistance: Evidence for Differential Regulation of Insulin Signaling by TNF-Alpha. Endocrinology 1998, 139, 4928–4935. [Google Scholar] [CrossRef]
- De Taeye, B.M.; Novitskaya, T.; McGuinness, O.P.; Gleaves, L.; Medda, M.; Covington, J.W.; Vaughan, D.E. Macrophage TNF-Alpha Contributes to Insulin Resistance and Hepatic Steatosis in Diet-Induced Obesity. Am. J. Physiol. Endocrinol. Metab. 2007, 293, E713–E725. [Google Scholar] [CrossRef]
- Jager, J.; Grémeaux, T.; Cormont, M.; Le Marchand-Brustel, Y.; Tanti, J.-F. Interleukin-1beta-Induced Insulin Resistance in Adipocytes through down-Regulation of Insulin Receptor Substrate-1 Expression. Endocrinology 2007, 148, 241–251. [Google Scholar] [CrossRef] [Green Version]
- Lagathu, C.; Yvan-Charvet, L.; Bastard, J.-P.; Maachi, M.; Quignard-Boulangé, A.; Capeau, J.; Caron, M. Long-Term Treatment with Interleukin-1beta Induces Insulin Resistance in Murine and Human Adipocytes. Diabetologia 2006, 49, 2162–2173. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Howard, C.P.; Walter, V.; Everett, B.; Libby, P.; Hensen, J.; Thuren, T.; CANTOS Pilot Investigative Group. Effects of Interleukin-1β Inhibition with Canakinumab on Hemoglobin A1c, Lipids, C-Reactive Protein, Interleukin-6, and Fibrinogen: A Phase IIb Randomized, Placebo-Controlled Trial. Circulation 2012, 126, 2739–2748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turer, A.T.; Scherer, P.E. Adiponectin: Mechanistic Insights and Clinical Implications. Diabetologia 2012, 55, 2319–2326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamauchi, T.; Kamon, J.; Waki, H.; Terauchi, Y.; Kubota, N.; Hara, K.; Mori, Y.; Ide, T.; Murakami, K.; Tsuboyama-Kasaoka, N.; et al. The Fat-Derived Hormone Adiponectin Reverses Insulin Resistance Associated with Both Lipoatrophy and Obesity. Nat. Med. 2001, 7, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, R.S.; Funahashi, T.; Hanson, R.L.; Matsuzawa, Y.; Tanaka, S.; Tataranni, P.A.; Knowler, W.C.; Krakoff, J. Adiponectin and Development of Type 2 Diabetes in the Pima Indian Population. Lancet Lond. Engl. 2002, 360, 57–58. [Google Scholar] [CrossRef]
- Li, S.; Shin, H.J.; Ding, E.L.; van Dam, R.M. Adiponectin Levels and Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis. JAMA 2009, 302, 179–188. [Google Scholar] [CrossRef] [Green Version]
- Maeda, N.; Takahashi, M.; Funahashi, T.; Kihara, S.; Nishizawa, H.; Kishida, K.; Nagaretani, H.; Matsuda, M.; Komuro, R.; Ouchi, N.; et al. PPARgamma Ligands Increase Expression and Plasma Concentrations of Adiponectin, an Adipose-Derived Protein. Diabetes 2001, 50, 2094–2099. [Google Scholar] [CrossRef] [Green Version]
- Hong, E.-G.; Ko, H.J.; Cho, Y.-R.; Kim, H.-J.; Ma, Z.; Yu, T.Y.; Friedline, R.H.; Kurt-Jones, E.; Finberg, R.; Fischer, M.A.; et al. Interleukin-10 Prevents Diet-Induced Insulin Resistance by Attenuating Macrophage and Cytokine Response in Skeletal Muscle. Diabetes 2009, 58, 2525–2535. [Google Scholar] [CrossRef] [Green Version]
- van Exel, E.; Gussekloo, J.; de Craen, A.J.M.; Frölich, M.; Bootsma-Van Der Wiel, A.; Westendorp, R.G.J.; Leiden 85 Plus Study. Low Production Capacity of Interleukin-10 Associates with the Metabolic Syndrome and Type 2 Diabetes: The Leiden 85-Plus Study. Diabetes 2002, 51, 1088–1092. [Google Scholar] [CrossRef] [Green Version]
- CDC Centers for Disease Control and Prevention How Much Physical Activity Do Children Need? Available online: https://www.cdc.gov/physicalactivity/basics/children/index.htm (accessed on 30 September 2022).
- McMurray, R.G.; Berry, D.C.; Schwartz, T.A.; Hall, E.G.; Neal, M.N.; Li, S.; Lam, D. Relationships of Physical Activity and Sedentary Time in Obese Parent-Child Dyads: A Cross-Sectional Study. BMC Public Health 2015, 16, 124. [Google Scholar] [CrossRef] [Green Version]
- Bülbül, S. Çocuklarda Obezite Tedavisinde Egzersiz. Türk Pediatri Arş. 2019, 55, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Hills, A.P.; Andersen, L.B.; Byrne, N.M. Physical Activity and Obesity in Children. Br. J. Sports Med. 2011, 45, 866–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoner, L.; Rowlands, D.; Morrison, A.; Credeur, D.; Hamlin, M.; Gaffney, K.; Lambrick, D.; Matheson, A. Efficacy of Exercise Intervention for Weight Loss in Overweight and Obese Adolescents: Meta-Analysis and Implications. Sports Med. Auckl. NZ 2016, 46, 1737–1751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imierska, M.; Kurianiuk, A.; Błachnio-Zabielska, A. The Influence of Physical Activity on the Bioactive Lipids Metabolism in Obesity-Induced Muscle Insulin Resistance. Biomolecules 2020, 10, 1665. [Google Scholar] [CrossRef] [PubMed]
- Willis, L.H.; Slentz, C.A.; Bateman, L.A.; Shields, A.T.; Piner, L.W.; Bales, C.W.; Houmard, J.A.; Kraus, W.E. Effects of Aerobic and/or Resistance Training on Body Mass and Fat Mass in Overweight or Obese Adults. J. Appl. Physiol. 2012, 113, 1831–1837. [Google Scholar] [CrossRef]
- Sung, K.-D.; Pekas, E.J.; Scott, S.D.; Son, W.-M.; Park, S.-Y. Correction to: The Effects of a 12-Week Jump Rope Exercise Program on Abdominal Adiposity, Vasoactive Substances, Inflammation, and Vascular Function in Adolescent Girls with Prehypertension. Eur. J. Appl. Physiol. 2020, 120, 1203. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Son, W.-M.; Headid, R.J.; Pekas, E.J.; Noble, J.M.; Park, S.-Y. Corrigendum to: The Effects of a 12-Week Jump Rope Exercise Program on Body Composition, Insulin Sensitivity, and Academic Self-Efficacy in Obese Adolescent Girls. J. Pediatr. Endocrinol. Metab. 2020, 33, 681. [Google Scholar] [CrossRef]
- Dias, K.A.; Ingul, C.B.; Tjønna, A.E.; Keating, S.E.; Gomersall, S.R.; Follestad, T.; Hosseini, M.S.; Hollekim-Strand, S.M.; Ro, T.B.; Haram, M.; et al. Effect of High-Intensity Interval Training on Fitness, Fat Mass and Cardiometabolic Biomarkers in Children with Obesity: A Randomised Controlled Trial. Sports Med. 2018, 48, 733–746. [Google Scholar] [CrossRef]
- Meng, C.; Yucheng, T.; Shu, L.; Yu, Z. Effects of School-Based High-Intensity Interval Training on Body Composition, Cardiorespiratory Fitness and Cardiometabolic Markers in Adolescent Boys with Obesity: A Randomized Controlled Trial. BMC Pediatr. 2022, 22, 112. [Google Scholar] [CrossRef]
- Zhu, L.; Liu, J.; Yu, Y.; Tian, Z. Effect of High-Intensity Interval Training on Cardiometabolic Risk Factors in Childhood Obesity: A Meta-Analysis. J. Sports Med. Phys. Fitness 2021, 61, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Cordellat, A.; Padilla, B.; Grattarola, P.; García-Lucerga, C.; Crehuá-Gaudiza, E.; Núñez, F.; Martínez-Costa, C.; Blasco-Lafarga, C. Multicomponent Exercise Training Combined with Nutritional Counselling Improves Physical Function, Biochemical and Anthropometric Profiles in Obese Children: A Pilot Study. Nutrients 2020, 12, 2723. [Google Scholar] [CrossRef] [PubMed]
- Shaibi, G.Q.; Cruz, M.L.; Ball, G.D.C.; Weigensberg, M.J.; Salem, G.J.; Crespo, N.C.; Goran, M.I. Effects of Resistance Training on Insulin Sensitivity in Overweight Latino Adolescent Males. Med. Sci. Sports Exerc. 2006, 38, 1208–1215. [Google Scholar] [CrossRef] [Green Version]
- Davis, J.N.; Gyllenhammer, L.E.; Vanni, A.A.; Meija, M.; Tung, A.; Schroeder, E.T.; Spruijt-Metz, D.; Goran, M.I. Startup Circuit Training Program Reduces Metabolic Risk in Latino Adolescents. Med. Sci. Sports Exerc. 2011, 43, 2195–2203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.; Libman, I.; Hughan, K.; Kuk, J.L.; Jeong, J.H.; Zhang, D.; Arslanian, S. Effects of Exercise Modality on Insulin Resistance and Ectopic Fat in Adolescents with Overweight and Obesity: A Randomized Clinical Trial. J. Pediatr. 2019, 206, 91–98.e1. [Google Scholar] [CrossRef]
- Wong, P.C.H.; Chia, M.Y.H.; Tsou, I.Y.Y.; Wansaicheong, G.K.L.; Tan, B.; Wang, J.C.K.; Tan, J.; Kim, C.G.; Boh, G.; Lim, D. Effects of a 12-Week Exercise Training Programme on Aerobic Fitness, Body Composition, Blood Lipids and C-Reactive Protein in Adolescents with Obesity. Ann. Acad. Med. Singap. 2008, 37, 286–293. [Google Scholar]
- Bell, L.M.; Watts, K.; Siafarikas, A.; Thompson, A.; Ratnam, N.; Bulsara, M.; Finn, J.; O’Driscoll, G.; Green, D.J.; Jones, T.W.; et al. Exercise Alone Reduces Insulin Resistance in Obese Children Independently of Changes in Body Composition. J. Clin. Endocrinol. Metab. 2007, 92, 4230–4235. [Google Scholar] [CrossRef] [Green Version]
- Penagini, F.; Calcaterra, V.; Dilillo, D.; Vandoni, M.; Gianolio, L.; Gatti, A.; Rendo, G.; Giuriato, M.; Cococcioni, L.; De Silvestri, A.; et al. Self-Perceived Physical Level and Fitness Performance in Children and Adolescents with Inflammatory Bowel Disease. Children 2022, 9, 1399. [Google Scholar] [CrossRef]
- Vandoni, M.; Lovecchio, N.; Carnevale Pellino, V.; Codella, R.; Fabiano, V.; Rossi, V.; Zuccotti, G.V.; Calcaterra, V. Self-Reported Physical Fitness in Children and Adolescents with Obesity: A Cross-Sectional Analysis on the Level of Alignment with Multiple Adiposity Indexes. Child. Basel Switz. 2021, 8, 476. [Google Scholar] [CrossRef]
- Calcaterra, V.; Larizza, D.; Codrons, E.; De Silvestri, A.; Brambilla, P.; Abela, S.; Arpesella, M.; Vandoni, M. Improved Metabolic and Cardiorespiratory Fitness during a Recreational Training Program in Obese Children. J. Pediatr. Endocrinol. Metab. JPEM 2013, 26, 271–276. [Google Scholar] [CrossRef]
- Vandoni, M.; Carnevale Pellino, V.; Gatti, A.; Lucini, D.; Mannarino, S.; Larizza, C.; Rossi, V.; Tranfaglia, V.; Pirazzi, A.; Biino, V.; et al. Effects of an Online Supervised Exercise Training in Children with Obesity during the COVID-19 Pandemic. Int. J. Environ. Res. Public. Health 2022, 19, 9421. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.M.; Semenkovich, C.F.; Gulve, E.A.; Gao, J.; Holloszy, J.O. Exercise Induces Rapid Increases in GLUT4 Expression, Glucose Transport Capacity, and Insulin-Stimulated Glycogen Storage in Muscle. J. Biol. Chem. 1994, 269, 14396–14401. [Google Scholar] [CrossRef]
- Bradley, H.; Shaw, C.S.; Bendtsen, C.; Worthington, P.L.; Wilson, O.J.; Strauss, J.A.; Wallis, G.A.; Turner, A.M.; Wagenmakers, A.J.M. Visualization and Quantitation of GLUT4 Translocation in Human Skeletal Muscle Following Glucose Ingestion and Exercise. Physiol. Rep. 2015, 3, e12375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, A.P. PGC-1alpha and Exercise: Important Partners in Combating Insulin Resistance. Curr. Diabetes Rev. 2005, 1, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Sangwung, P.; Petersen, K.F.; Shulman, G.I.; Knowles, J.W. Mitochondrial Dysfunction, Insulin Resistance, and Potential Genetic Implications. Endocrinology 2020, 161, bqaa017. [Google Scholar] [CrossRef]
- Gutiérrez-Rodelo, C.; Roura-Guiberna, A.; Olivares-Reyes, J.A. Molecular Mechanisms of Insulin Resistance: An Update. Gac. Med. Mex. 2017, 153, 214–228. [Google Scholar]
- Kelley, G.A.; Kelley, K.S. Aerobic Exercise and Lipids and Lipoproteins in Children and Adolescents: A Meta-Analysis of Randomized Controlled Trials. Atherosclerosis 2007, 191, 447–453. [Google Scholar] [CrossRef] [Green Version]
- Nassis, G.P.; Papantakou, K.; Skenderi, K.; Triandafillopoulou, M.; Kavouras, S.A.; Yannakoulia, M.; Chrousos, G.P.; Sidossis, L.S. Aerobic Exercise Training Improves Insulin Sensitivity without Changes in Body Weight, Body Fat, Adiponectin, and Inflammatory Markers in Overweight and Obese Girls. Metabolism 2005, 54, 1472–1479. [Google Scholar] [CrossRef]
- Agostinis-Sobrinho, C.; Kievišienė, J.; Rauckienė-Michaelsson, A.; Dubey, V.P.; Norkiene, S.; Moreira, C.; Lopes, L.; Santos, R. Cardiovascular Health Behavior and Cardiorespiratory Fitness in Adolescents: A Longitudinal Study. Eur. J. Pediatr. 2022. [Google Scholar] [CrossRef]
- Racil, G.; Zouhal, H.; Elmontassar, W.; Ben Abderrahmane, A.; De Sousa, M.V.; Chamari, K.; Amri, M.; Coquart, J.B. Plyometric Exercise Combined with High-Intensity Interval Training Improves Metabolic Abnormalities in Young Obese Females More so than Interval Training Alone. Appl. Physiol. Nutr. Metab. Physiol. Appl. Nutr. Metab. 2016, 41, 103–109. [Google Scholar] [CrossRef] [Green Version]
- Światowy, W.J.; Drzewiecka, H.; Kliber, M.; Sąsiadek, M.; Karpiński, P.; Pławski, A.; Jagodziński, P.P. Physical Activity and DNA Methylation in Humans. Int. J. Mol. Sci. 2021, 22, 12989. [Google Scholar] [CrossRef] [PubMed]
- Bonilauri, B.; Dallagiovanna, B. Long Non-Coding RNAs Are Differentially Expressed after Different Exercise Training Programs. Front. Physiol. 2020, 11, 567614. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.; Åkerström, T.; Rinnov, A.; Yfanti, C.; Scheele, C.; Pedersen, B.K.; Laye, M.J. The MiRNA Plasma Signature in Response to Acute Aerobic Exercise and Endurance Training. PLoS ONE 2014, 9, e87308. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef] [Green Version]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in Children and Adolescents: Epidemiology, Causes, Assessment, and Management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef]
- Rozga, M.; Handu, D. Current Systems-Level Evidence on Nutrition Interventions to Prevent and Treat Cardiometabolic Risk in the Pediatric Population: An Evidence Analysis Center Scoping Review. J. Acad. Nutr. Diet. 2021, 121, 2501–2523. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Garnett, S.P.; Baur, L.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Effectiveness of Lifestyle Interventions in Child Obesity: Systematic Review with Meta-Analysis. Pediatrics 2012, 130, e1647–e1671. [Google Scholar] [CrossRef] [Green Version]
- Mohammadi, S.; Lotfi, K.; Mirzaei, S.; Asadi, A.; Akhlaghi, M.; Saneei, P. Adherence to Mediterranean Diet and Its Association with Metabolic Health Status in Overweight and Obese Adolescents. Int. J. Clin. Pract. 2022, 2022, 9925267. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Vasilopoulou, E. Mediterranean Diet. In Encyclopedia of Food and Health; Caballero, B., Finglas, P.M., Toldrá, F., Eds.; Academic Press: Oxford, UK, 2016; pp. 711–714. ISBN 978-0-12-384953-3. [Google Scholar]
- Gallardo-Escribano, C.; Vargas-Candela, A.; Vilches-Perez, A.; Muñoz-Melero, M.; Ruiz-Moreno, M.I.; Benitez-Porres, J.; Romance-Garcia, A.R.; Rodriguez-Ortega, R.; Rosa-López, A.; Rosales-Jaime, A.; et al. Lifestyle Modification Improves Insulin Resistance and Carotid Intima-Media Thickness in a Metabolically Healthy Obese Prepubescent Population. J. Pediatr. Gastroenterol. Nutr. 2021, 72, 127–134. [Google Scholar] [CrossRef]
- Blancas-Sánchez, I.M.; Del Rosal Jurado, M.; Aparicio-Martínez, P.; Quintana Navarro, G.; Vaquero-Abellan, M.; Castro Jiménez, R.A.; Fonseca Pozo, F.J. A Mediterranean-Diet-Based Nutritional Intervention for Children with Prediabetes in a Rural Town: A Pilot Randomized Controlled Trial. Nutrients 2022, 14, 3614. [Google Scholar] [CrossRef]
- Mirabelli, M.; Chiefari, E.; Arcidiacono, B.; Corigliano, D.M.; Brunetti, F.S.; Maggisano, V.; Russo, D.; Foti, D.P.; Brunetti, A. Mediterranean Diet Nutrients to Turn the Tide against Insulin Resistance and Related Diseases. Nutrients 2020, 12, 1066. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Amore, S.; Vacca, M.; Cariello, M.; Graziano, G.; D’Orazio, A.; Salvia, R.; Sasso, R.C.; Sabbà, C.; Palasciano, G.; Moschetta, A. Genes and MiRNA Expression Signatures in Peripheral Blood Mononuclear Cells in Healthy Subjects and Patients with Metabolic Syndrome after Acute Intake of Extra Virgin Olive Oil. Biochim. Biophys. Acta 2016, 1861, 1671–1680. [Google Scholar] [CrossRef] [PubMed]
- Di Profio, E.; Magenes, V.C.; Fiore, G.; Agostinelli, M.; La Mendola, A.; Acunzo, M.; Francavilla, R.; Indrio, F.; Bosetti, A.; D’Auria, E.; et al. Special Diets in Infants and Children and Impact on Gut Microbioma. Nutrients 2022, 14, 3198. [Google Scholar] [CrossRef] [PubMed]
- Fiore, G.; Magenes, V.C.; DI Profio, E.; Milanta, C.; Calcaterra, V.; Diamanti, A.; Campoy, C.; Zuccotti, G.V.; Verduci, E. Gut Microbiota in Obesity and Related Comorbidities in Children and Adolescents: The Role of Biotics in Treatment. Minerva Pediatr. 2022. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, R.; Shively, C.A.; Register, T.C.; Craft, S.; Yadav, H. Gut Microbiome-Mediterranean Diet Interactions in Improving Host Health. F1000Research 2019, 8, 699. [Google Scholar] [CrossRef] [Green Version]
- Riva, A.; Borgo, F.; Lassandro, C.; Verduci, E.; Morace, G.; Borghi, E.; Berry, D. Pediatric Obesity Is Associated with an Altered Gut Microbiota and Discordant Shifts in Firmicutes Populations. Environ. Microbiol. 2017, 19, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Garnett, S.P.; Baur, L.A.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Impact of Dietary and Exercise Interventions on Weight Change and Metabolic Outcomes in Obese Children and Adolescents: A Systematic Review and Meta-Analysis of Randomized Trials. JAMA Pediatr. 2013, 167, 759–768. [Google Scholar] [CrossRef]
- Barlow, S.E.; Expert Committee. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef] [Green Version]
- Valerio, G.; Maffeis, C.; Saggese, G.; Ambruzzi, M.A.; Balsamo, A.; Bellone, S.; Bergamini, M.; Bernasconi, S.; Bona, G.; Calcaterra, V.; et al. Diagnosis, Treatment and Prevention of Pediatric Obesity: Consensus Position Statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics. Ital. J. Pediatr. 2018, 44, 88. [Google Scholar] [CrossRef] [Green Version]
- Albert Pérez, E.; Mateu Olivares, V.; Martínez-Espinosa, R.M.; Molina Vila, M.D.; Reig García-Galbis, M. New Insights about How to Make an Intervention in Children and Adolescents with Metabolic Syndrome: Diet, Exercise vs. Changes in Body Composition. A Systematic Review of RCT. Nutrients 2018, 10, 878. [Google Scholar] [CrossRef] [Green Version]
- Elloumi, M.; Ben Ounis, O.; Makni, E.; Van Praagh, E.; Tabka, Z.; Lac, G. Effect of Individualized Weight-Loss Programmes on Adiponectin, Leptin and Resistin Levels in Obese Adolescent Boys. Acta Paediatr. Oslo Nor. 2009, 98, 1487–1493. [Google Scholar] [CrossRef] [PubMed]
- Giussani, M.; Orlando, A.; Tassistro, E.; Lieti, G.; Patti, I.; Antolini, L.; Parati, G.; Genovesi, S. Impact of Lifestyle Modifications on Alterations in Lipid and Glycemic Profiles and Uric Acid Values in a Pediatric Population. Nutrients 2022, 14, 1034. [Google Scholar] [CrossRef] [PubMed]
- Shalitin, S.; Ashkenazi-Hoffnung, L.; Yackobovitch-Gavan, M.; Nagelberg, N.; Karni, Y.; Hershkovitz, E.; Loewenthal, N.; Shtaif, B.; Gat-Yablonski, G.; Phillip, M. Effects of a Twelve-Week Randomized Intervention of Exercise and/or Diet on Weight Loss and Weight Maintenance, and Other Metabolic Parameters in Obese Preadolescent Children. Horm. Res. 2009, 72, 287–301. [Google Scholar] [CrossRef]
- Andela, S.; Burrows, T.L.; Baur, L.A.; Coyle, D.H.; Collins, C.E.; Gow, M.L. Efficacy of Very Low-Energy Diet Programs for Weight Loss: A Systematic Review with Meta-Analysis of Intervention Studies in Children and Adolescents with Obesity. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2019, 20, 871–882. [Google Scholar] [CrossRef] [PubMed]
- Ebbeling, C.B.; Leidig, M.M.; Sinclair, K.B.; Hangen, J.P.; Ludwig, D.S. A Reduced-Glycemic Load Diet in the Treatment of Adolescent Obesity. Arch. Pediatr. Adolesc. Med. 2003, 157, 773–779. [Google Scholar] [CrossRef]
- Iannuzzi, A.; Licenziati, M.R.; Vacca, M.; De Marco, D.; Cinquegrana, G.; Laccetti, M.; Bresciani, A.; Covetti, G.; Iannuzzo, G.; Rubba, P.; et al. Comparison of Two Diets of Varying Glycemic Index on Carotid Subclinical Atherosclerosis in Obese Children. Heart Vessels 2009, 24, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Mirza, N.M.; Palmer, M.G.; Sinclair, K.B.; McCarter, R.; He, J.; Ebbeling, C.B.; Ludwig, D.S.; Yanovski, J.A. Effects of a Low Glycemic Load or a Low-Fat Dietary Intervention on Body Weight in Obese Hispanic American Children and Adolescents: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2013, 97, 276–285. [Google Scholar] [CrossRef] [Green Version]
- Ramon-Krauel, M.; Salsberg, S.L.; Ebbeling, C.B.; Voss, S.D.; Mulkern, R.V.; Apura, M.M.; Cooke, E.A.; Sarao, K.; Jonas, M.M.; Ludwig, D.S. A Low-Glycemic-Load versus Low-Fat Diet in the Treatment of Fatty Liver in Obese Children. Child. Obes. Print 2013, 9, 252–260. [Google Scholar] [CrossRef] [Green Version]
- Visuthranukul, C.; Hurst, C.; Chomtho, S. Effects of Low-Glycemic Index Diet on Plasma Adipokines in Obese Children. Pediatr. Res. 2021, 90, 1009–1015. [Google Scholar] [CrossRef]
- Jenkins, D.J.; Wolever, T.M.; Taylor, R.H.; Barker, H.; Fielden, H.; Baldwin, J.M.; Bowling, A.C.; Newman, H.C.; Jenkins, A.L.; Goff, D.V. Glycemic Index of Foods: A Physiological Basis for Carbohydrate Exchange. Am. J. Clin. Nutr. 1981, 34, 362–366. [Google Scholar] [CrossRef] [Green Version]
- Salmerón, J.; Ascherio, A.; Rimm, E.B.; Colditz, G.A.; Spiegelman, D.; Jenkins, D.J.; Stampfer, M.J.; Wing, A.L.; Willett, W.C. Dietary Fiber, Glycemic Load, and Risk of NIDDM in Men. Diabetes Care 1997, 20, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Joslowski, G.; Halim, J.; Goletzke, J.; Gow, M.; Ho, M.; Louie, J.C.-Y.; Buyken, A.E.; Cowell, C.T.; Garnett, S.P. Dietary Glycemic Load, Insulin Load, and Weight Loss in Obese, Insulin Resistant Adolescents: RESIST Study. Clin. Nutr. Edinb. Scotl. 2015, 34, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hobl, L.P.; Hoffmann, G. Effects of Low Glycaemic Index/Low Glycaemic Load vs. High Glycaemic Index/High Glycaemic Load Diets on Overweight/Obesity and Associated Risk Factors in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutr. J. 2015, 14, 87. [Google Scholar] [CrossRef]
- Kirk, S.; Brehm, B.; Saelens, B.E.; Woo, J.G.; Kissel, E.; D’Alessio, D.; Bolling, C.; Daniels, S.R. Role of Carbohydrate Modification in Weight Management among Obese Children: A Randomized Clinical Trial. J. Pediatr. 2012, 161, 320–327.e1. [Google Scholar] [CrossRef] [Green Version]
- Hite, A.H.; Feinman, R.D.; Guzman, G.E.; Satin, M.; Schoenfeld, P.A.; Wood, R.J. In the Face of Contradictory Evidence: Report of the Dietary Guidelines for Americans Committee. Nutrition 2010, 26, 915–924. [Google Scholar] [CrossRef] [PubMed]
- Gow, M.L.; Ho, M.; Burrows, T.L.; Baur, L.A.; Stewart, L.; Hutchesson, M.J.; Cowell, C.T.; Collins, C.E.; Garnett, S.P. Impact of Dietary Macronutrient Distribution on BMI and Cardiometabolic Outcomes in Overweight and Obese Children and Adolescents: A Systematic Review. Nutr. Rev. 2014, 72, 453–470. [Google Scholar] [CrossRef]
- Caferoglu, Z.; Hatipoglu, N.; Gokmen Ozel, H. Does Food Insulin Index in the Context of Mixed Meals Affect Postprandial Metabolic Responses and Appetite in Obese Adolescents with Insulin Resistance? A Randomised Cross-over Trial. Br. J. Nutr. 2019, 122, 942–950. [Google Scholar] [CrossRef]
- Nimptsch, K.; Brand-Miller, J.C.; Franz, M.; Sampson, L.; Willett, W.C.; Giovannucci, E. Dietary Insulin Index and Insulin Load in Relation to Biomarkers of Glycemic Control, Plasma Lipids, and Inflammation Markers. Am. J. Clin. Nutr. 2011, 94, 182–190. [Google Scholar] [CrossRef] [Green Version]
- Dorenbos, E.; Drummen, M.; Adam, T.; Rijks, J.; Winkens, B.; Martínez, J.A.; Navas-Carretero, S.; Stratton, G.; Swindell, N.; Stouthart, P.; et al. Effect of a High Protein/Low Glycaemic Index Diet on Insulin Resistance in Adolescents with Overweight/Obesity-A PREVIEW Randomized Clinical Trial. Pediatr. Obes. 2021, 16, e12702. [Google Scholar] [CrossRef]
- Garnett, S.P.; Gow, M.; Ho, M.; Baur, L.A.; Noakes, M.; Woodhead, H.J.; Broderick, C.R.; Chisholm, K.; Briody, J.; De, S.; et al. Improved Insulin Sensitivity and Body Composition, Irrespective of Macronutrient Intake, after a 12 Month Intervention in Adolescents with Pre-Diabetes; RESIST a Randomised Control Trial. BMC Pediatr. 2014, 14, 289. [Google Scholar] [CrossRef] [Green Version]
- Damsgaard, C.T.; Papadaki, A.; Jensen, S.M.; Ritz, C.; Dalskov, S.-M.; Hlavaty, P.; Saris, W.H.M.; Martinez, J.A.; Handjieva-Darlenska, T.; Andersen, M.R.; et al. Higher Protein Diets Consumed Ad Libitum Improve Cardiovascular Risk Markers in Children of Overweight Parents from Eight European Countries. J. Nutr. 2013, 143, 810–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.T.; Nieuwdorp, M.; Bäckhed, F. Microbial Modulation of Insulin Sensitivity. Cell Metab. 2014, 20, 753–760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Indiani, C.M.D.S.P.; Rizzardi, K.F.; Castelo, P.M.; Ferraz, L.F.C.; Darrieux, M.; Parisotto, T.M. Childhood Obesity and Firmicutes/Bacteroidetes Ratio in the Gut Microbiota: A Systematic Review. Child. Obes. Print 2018, 14, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.J.; West, N.P.; Cripps, A.W. Obesity, Inflammation, and the Gut Microbiota. Lancet Diabetes Endocrinol. 2015, 3, 207–215. [Google Scholar] [CrossRef]
- Utzschneider, K.M.; Kratz, M.; Damman, C.J.; Hullar, M. Mechanisms Linking the Gut Microbiome and Glucose Metabolism. J. Clin. Endocrinol. Metab. 2016, 101, 1445–1454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Górowska-Kowolik, K.; Chobot, A. The Role of Gut Micorbiome in Obesity and Diabetes. World J. Pediatr. WJP 2019, 15, 332–340. [Google Scholar] [CrossRef]
- Verma, A.; Nelson, M.T.; DePaolo, W.R.; Hampe, C.; Roth, C.L. A Randomized Double-Blind Placebo Controlled Pilot Study of Probiotics in Adolescents with Severe Obesity. J. Diabetes Metab. Disord. 2021, 20, 1289–1300. [Google Scholar] [CrossRef]
- Solito, A.; Bozzi Cionci, N.; Calgaro, M.; Caputo, M.; Vannini, L.; Hasballa, I.; Archero, F.; Giglione, E.; Ricotti, R.; Walker, G.E.; et al. Supplementation with Bifidobacterium Breve BR03 and B632 Strains Improved Insulin Sensitivity in Children and Adolescents with Obesity in a Cross-over, Randomized Double-Blind Placebo-Controlled Trial. Clin. Nutr. Edinb. Scotl. 2021, 40, 4585–4594. [Google Scholar] [CrossRef]
- Sanchis-Chordà, J.; Del Pulgar, E.M.G.; Carrasco-Luna, J.; Benítez-Páez, A.; Sanz, Y.; Codoñer-Franch, P. Bifidobacterium Pseudocatenulatum CECT 7765 Supplementation Improves Inflammatory Status in Insulin-Resistant Obese Children. Eur. J. Nutr. 2019, 58, 2789–2800. [Google Scholar] [CrossRef]
- Benítez-Páez, A.; Gómez Del Pugar, E.M.; López-Almela, I.; Moya-Pérez, Á.; Codoñer-Franch, P.; Sanz, Y. Depletion of Blautia Species in the Microbiota of Obese Children Relates to Intestinal Inflammation and Metabolic Phenotype Worsening. mSystems 2020, 5, e00857-19. [Google Scholar] [CrossRef] [Green Version]
- Institute of Medicine (U.S.) (Ed.) Dietary Reference Intakes: Proposed Definition of Dietary Fiber; The Compass Series; National Academy Press: Washington, DC, USA, 2001; ISBN 978-0-309-07564-0. [Google Scholar]
- Lyon, M.R.; Kacinik, V. Is There a Place for Dietary Fiber Supplements in Weight Management? Curr. Obes. Rep. 2012, 1, 59–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, M.; Canfora, E.E.; Blaak, E.E. Gastrointestinal Transit Time, Glucose Homeostasis and Metabolic Health: Modulation by Dietary Fibers. Nutrients 2018, 10, 275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falony, G.; Joossens, M.; Vieira-Silva, S.; Wang, J.; Darzi, Y.; Faust, K.; Kurilshikov, A.; Bonder, M.J.; Valles-Colomer, M.; Vandeputte, D.; et al. Population-Level Analysis of Gut Microbiome Variation. Science 2016, 352, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Korczak, R.; Kamil, A.; Fleige, L.; Donovan, S.M.; Slavin, J.L. Dietary Fiber and Digestive Health in Children. Nutr. Rev. 2017, 75, 241–259. [Google Scholar] [CrossRef]
- Canfora, E.E.; Jocken, J.W.; Blaak, E.E. Short-Chain Fatty Acids in Control of Body Weight and Insulin Sensitivity. Nat. Rev. Endocrinol. 2015, 11, 577–591. [Google Scholar] [CrossRef]
- Moreno, L.A.; Tresaco, B.; Bueno, G.; Fleta, J.; Rodríguez, G.; Garagorri, J.M.; Bueno, M. Psyllium Fibre and the Metabolic Control of Obese Children and Adolescents. J. Physiol. Biochem. 2003, 59, 235–242. [Google Scholar] [CrossRef]
- Fornari, E.; Morandi, A.; Piona, C.; Tommasi, M.; Corradi, M.; Maffeis, C. Policaptil Gel Retard Intake Reduces Postprandial Triglycerides, Ghrelin and Appetite in Obese Children: A Clinical Trial. Nutrients 2020, 12, 214. [Google Scholar] [CrossRef] [Green Version]
- Visuthranukul, C.; Kwanbunbumpen, T.; Chongpison, Y.; Chamni, S.; Panichsillaphakit, E.; Uaariyapanichkul, J.; Maholarnkij, S.; Chomtho, S. The Impact of Dietary Fiber as a Prebiotic on Inflammation in Children with Obesity. Foods Basel Switz. 2022, 11, 2856. [Google Scholar] [CrossRef]
- Fatahi, S.; Sayyari, A.A.; Salehi, M.; Safa, M.; Sohouli, M.; Shidfar, F.; Santos, H.O. The Effects of Chitosan Supplementation on Anthropometric Indicators of Obesity, Lipid and Glycemic Profiles, and Appetite-Regulated Hormones in Adolescents with Overweight or Obesity: A Randomized, Double-Blind Clinical Trial. BMC Pediatr. 2022, 22, 527. [Google Scholar] [CrossRef]
- Van Hulst, A.; Paradis, G.; Harnois-Leblanc, S.; Benedetti, A.; Drapeau, V.; Henderson, M. Lowering Saturated Fat and Increasing Vegetable and Fruit Intake May Increase Insulin Sensitivity 2 Years Later in Children with a Family History of Obesity. J. Nutr. 2018, 148, 1838–1844. [Google Scholar] [CrossRef] [Green Version]
- Aldámiz-Echevarría, L.; Prieto, J.A.; Andrade, F.; Elorz, J.; Sanjurjo, P.; Rodríguez Soriano, J. Arachidonic Acid Content in Adipose Tissue Is Associated with Insulin Resistance in Healthy Children. J. Pediatr. Gastroenterol. Nutr. 2007, 44, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. Omega-3 Polyunsaturated Fatty Acids and Inflammatory Processes: Nutrition or Pharmacology? Br. J. Clin. Pharmacol. 2013, 75, 645–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burrows, T.; Collins, C.E.; Garg, M.L. Omega-3 Index, Obesity and Insulin Resistance in Children. Int. J. Pediatr. Obes. IJPO Off. J. Int. Assoc. Study Obes. 2011, 6, e532–e539. [Google Scholar] [CrossRef]
- Sánchez Meza, K.; Tene Pérez, C.E.; Sánchez Ramírez, C.A.; Muñiz Valencia, R.; Del Toro Equihua, M. Levels of Eicosapentaenoic Acid in Obese Schoolchildren with and without Insulin Resistance. Nutr. Hosp. 2014, 31, 1102–1108. [Google Scholar] [CrossRef] [PubMed]
- Marth, S.; Börnhorst, C.; Mehlig, K.; Russo, P.; Moreno, L.A.; De Henauw, S.; Veidebaum, T.; Molnár, D.; Tornaritis, M.; Risé, P.; et al. Associations of Whole Blood Polyunsaturated Fatty Acids and Insulin Resistance among European Children and Adolescents. Eur. J. Pediatr. 2020, 179, 1647–1651. [Google Scholar] [CrossRef] [PubMed]
- López-Alarcón, M.; Inda-Icaza, P.; Márquez-Maldonado, M.C.; Armenta-Álvarez, A.; Barbosa-Cortés, L.; Maldonado-Hernández, J.; Piña-Aguero, M.; Barradas-Vázquez, A.; Núñez-García, B.A.; Rodríguez-Cruz, M.; et al. A Randomized Control Trial of the Impact of LCPUFA-Ω3 Supplementation on Body Weight and Insulin Resistance in Pubertal Children with Obesity. Pediatr. Obes. 2019, 14, e12499. [Google Scholar] [CrossRef]
- Juárez-López, C.; Klünder-Klünder, M.; Madrigal-Azcárate, A.; Flores-Huerta, S. Omega-3 Polyunsaturated Fatty Acids Reduce Insulin Resistance and Triglycerides in Obese Children and Adolescents. Pediatr. Diabetes 2013, 14, 377–383. [Google Scholar] [CrossRef]
- Calle, C.; Maestro, B.; García-Arencibia, M. Genomic Actions of 1,25-Dihydroxyvitamin D3 on Insulin Receptor Gene Expression, Insulin Receptor Number and Insulin Activity in the Kidney, Liver and Adipose Tissue of Streptozotocin-Induced Diabetic Rats. BMC Mol. Biol. 2008, 9, 65. [Google Scholar] [CrossRef] [Green Version]
- Wortsman, J.; Matsuoka, L.Y.; Chen, T.C.; Lu, Z.; Holick, M.F. Decreased Bioavailability of Vitamin D in Obesity. Am. J. Clin. Nutr. 2000, 72, 690–693. [Google Scholar] [CrossRef] [Green Version]
- Smotkin-Tangorra, M.; Purushothaman, R.; Gupta, A.; Nejati, G.; Anhalt, H.; Ten, S. Prevalence of Vitamin D Insufficiency in Obese Children and Adolescents. J. Pediatr. Endocrinol. Metab. JPEM 2007, 20, 817–823. [Google Scholar] [CrossRef]
- Corica, D.; Zusi, C.; Olivieri, F.; Marigliano, M.; Piona, C.; Fornari, E.; Morandi, A.; Corradi, M.; Miraglia Del Giudice, E.; Gatti, D.; et al. Vitamin D Affects Insulin Sensitivity and β-Cell Function in Obese Non-Diabetic Youths. Eur. J. Endocrinol. 2019, 181, 439–450. [Google Scholar] [CrossRef] [PubMed]
- Javed, A.; Vella, A.; Balagopal, P.B.; Fischer, P.R.; Weaver, A.L.; Piccinini, F.; Dalla Man, C.; Cobelli, C.; Giesler, P.D.; Laugen, J.M.; et al. Cholecalciferol Supplementation Does Not Influence β-Cell Function and Insulin Action in Obese Adolescents: A Prospective Double-Blind Randomized Trial. J. Nutr. 2015, 145, 284–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelishadi, R.; Salek, S.; Salek, M.; Hashemipour, M.; Movahedian, M. Effects of Vitamin D Supplementation on Insulin Resistance and Cardiometabolic Risk Factors in Children with Metabolic Syndrome: A Triple-Masked Controlled Trial. J. Pediatr. (Rio J.) 2014, 90, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Bilici, M.E.; Erdeve, Ş.S.; Çetinkaya, S.; Aycan, Z. The Effect of 2000 Iu/Day Vitamin D Supplementation on Insulin Resistance and Cardiovascular Risk Parameters in Vitamin D Deficient Obese Adolescents. Turk. J. Pediatr. 2019, 61, 723–732. [Google Scholar] [CrossRef]
- Nader, N.S.; Aguirre Castaneda, R.; Wallace, J.; Singh, R.; Weaver, A.; Kumar, S. Effect of Vitamin D3 Supplementation on Serum 25(OH)D, Lipids and Markers of Insulin Resistance in Obese Adolescents: A Prospective, Randomized, Placebo-Controlled Pilot Trial. Horm. Res. Paediatr. 2014, 82, 107–112. [Google Scholar] [CrossRef]
- Sethuraman, U.; Zidan, M.A.; Hanks, L.; Bagheri, M.; Ashraf, A. Impact of Vitamin D Treatment on 25 Hydroxy Vitamin D Levels and Insulin Homeostasis in Obese African American Adolescents in a Randomized Trial. J. Clin. Transl. Endocrinol. 2018, 12, 13–19. [Google Scholar] [CrossRef]
- Hauger, H.; Laursen, R.P.; Ritz, C.; Mølgaard, C.; Lind, M.V.; Damsgaard, C.T. Effects of Vitamin D Supplementation on Cardiometabolic Outcomes in Children and Adolescents: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur. J. Nutr. 2020, 59, 873–884. [Google Scholar] [CrossRef]
- Canas, J.A.; Damaso, L.; Altomare, A.; Killen, K.; Hossain, J.; Balagopal, P.B. Insulin Resistance and Adiposity in Relation to Serum β-Carotene Levels. J. Pediatr. 2012, 161, 58–64.e1–2. [Google Scholar] [CrossRef]

| Supplementation | Type of Study | Subjects | Intervention | Intoleranceand/or Side Effect | Observed Effects |
|---|---|---|---|---|---|
| Probiotics | DB—placebo—RCT [160] | Randomized = 15 Drop out = 7 Placebo = 4 Probiotic = 4 Age: adolescents | Supplementation: Multi oral multi-strain probiotic: Lactobacillus casei + Lactobacillus rhamnosus + Bifidobacteria No Dietary adviceDuration: 12 weeks | Gastrointestinal intolerance: 1 patients |
|
| CO-DB-RCT [161] | 101 children affected by obesity and IR Age: 6–18 years | Dietary advice Supplementation: B. breve BR03 + B. breve B632 or placebo Duration: 8 weeks with 4 weeks wash out period | No adverse events |
| |
| RCT [162] | 48 children with obesity and IR Age: 10–15 years | Dietary advice Supplementation: Bifidobacterium pseudocatenulatum CECT 7765 strains or placebo Dose: single-dose capsules containing between 1 × 109 and 1 × 1010 colony forming units (CFU) per day Duration: 13 weeks | No adverse events |
| |
| RCT [163] | 51 children Age: 5–17 years N° = 35 obesity N° = 16 normal nutritional status | Microbiota analysis Duration: not indicated | No adverse events |
| |
| Fiber | DB-placebo-RCT [171] | 46 children with obesity Age: 8–12 years | No dietary advice Intervention: Policaptil Gel Retard (PGR) or placebo: 2 PGR tablets or placebo were given in fasting condition, before the ingestion of a mixed meal (15 kcal/kg lean body mass). Blood samples were taken at baseline and after 4 h. Duration: 1 day | No adverse events |
|
| DB-placebo-RCT [172] | 155 Thai children with obesity Age: 7–15 years | Dietary advice Low-energy and low-fat diet 1° Group: 13 g of isocaloric oligofructose enriched inulin extracted from the Thai Jerusalem artichoke daily at 30 min prior to dinner 2° Group: 11 g of isocaloric maltodextrin 3° Group: dietary fiber advice group Duration: 6 months | No adverse events |
| |
| DB-RCT [173] | 61 adolescents with overweight and obesity Age: 10–19 years | Chitosan supplementation (n = 31): 1.5 g (twice a day a totalof 3 g) Placebo (n = 30): maltodextrin Timing: daily 30 min to 1 h before lunch and dinner Duration: 12 weeks | No adverse events |
| |
| Lcpufa | Observational Study [177] | 24 children without 24 children with obesity Age: 5–12 years | No intervention | No adverse events |
|
| RCT [178] | 56 children with obesity Age: mean age was 109.2 months | No intervention | No adverse events |
| |
| Longitudinal Study [179] | 705 European children Age: 2–9 years old—subsample of IDEFICS Study | No intervention Duration: association was investigated at baseline and after 2- and 6-year follow-ups | No adverse events |
| |
| DB- placebo- parallel RCT [180] | 245 children Age: 12–18 years | Dietary advice Hypocaloric diet Supplementation: daily doses of 800 mg EPA + 400 mg DHA Placebo: 1 g sunflower oil Duration: 3 months | No adverse events | At baseline:
No effect on insulin concentration | |
| RCT [181] | 201 adolescents with obesity and IR | No dietary advice Supplementation: N°98 Metformin—Dose: 500 mg N°103 omega 3 PUFA—Dose 1.8 g Duration: 12 weeks | No adverse events | Metformin effects:
| |
| Vitamin d | Cross sectional study [185] | 122 Caucasian children with overweight and obesity Age: 12.8 ± 2.3 years | No intervention | No adverse events |
|
| DB-RCT [186] | 46 Caucasian adolescents with obesity Age: 12–18 years | Supplementation:
| No adverse events |
| |
| Placebo—RCT [187] | 43 children Age: 10–16 years | Supplementation:
| No adverse events | In the intervention group:
| |
| RCT [188] | 96 children Age: 10–18 years | Supplementation:
Duration: 3 months | No adverse events |
| |
| DB-placebo-RCT [189] | 44 adolescents with obesity Age: 12–18 years | Supplementation:
| No adverse events |
| |
| DB-placebo-RCT [190,191] | 29 children with obesity Age: 13–17 years | Supplementation:
| No adverse events |
| |
| RCT [192] | 39 prepubertal boys | Supplementation:
| No adverse events |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calcaterra, V.; Verduci, E.; Vandoni, M.; Rossi, V.; Fiore, G.; Massini, G.; Berardo, C.; Gatti, A.; Baldassarre, P.; Bianchi, A.; et al. The Effect of Healthy Lifestyle Strategies on the Management of Insulin Resistance in Children and Adolescents with Obesity: A Narrative Review. Nutrients 2022, 14, 4692. https://doi.org/10.3390/nu14214692
Calcaterra V, Verduci E, Vandoni M, Rossi V, Fiore G, Massini G, Berardo C, Gatti A, Baldassarre P, Bianchi A, et al. The Effect of Healthy Lifestyle Strategies on the Management of Insulin Resistance in Children and Adolescents with Obesity: A Narrative Review. Nutrients. 2022; 14(21):4692. https://doi.org/10.3390/nu14214692
Chicago/Turabian StyleCalcaterra, Valeria, Elvira Verduci, Matteo Vandoni, Virginia Rossi, Giulia Fiore, Giulia Massini, Clarissa Berardo, Alessandro Gatti, Paola Baldassarre, Alice Bianchi, and et al. 2022. "The Effect of Healthy Lifestyle Strategies on the Management of Insulin Resistance in Children and Adolescents with Obesity: A Narrative Review" Nutrients 14, no. 21: 4692. https://doi.org/10.3390/nu14214692
APA StyleCalcaterra, V., Verduci, E., Vandoni, M., Rossi, V., Fiore, G., Massini, G., Berardo, C., Gatti, A., Baldassarre, P., Bianchi, A., Cordaro, E., Cavallo, C., Cereda, C., Bosetti, A., & Zuccotti, G. (2022). The Effect of Healthy Lifestyle Strategies on the Management of Insulin Resistance in Children and Adolescents with Obesity: A Narrative Review. Nutrients, 14(21), 4692. https://doi.org/10.3390/nu14214692










