Salt-Related Knowledge, Attitudes, and Behaviors and Their Relationship with 24-Hour Urinary Sodium Excretion in Chinese Adults
Abstract
1. Introduction
2. Materials and Methods
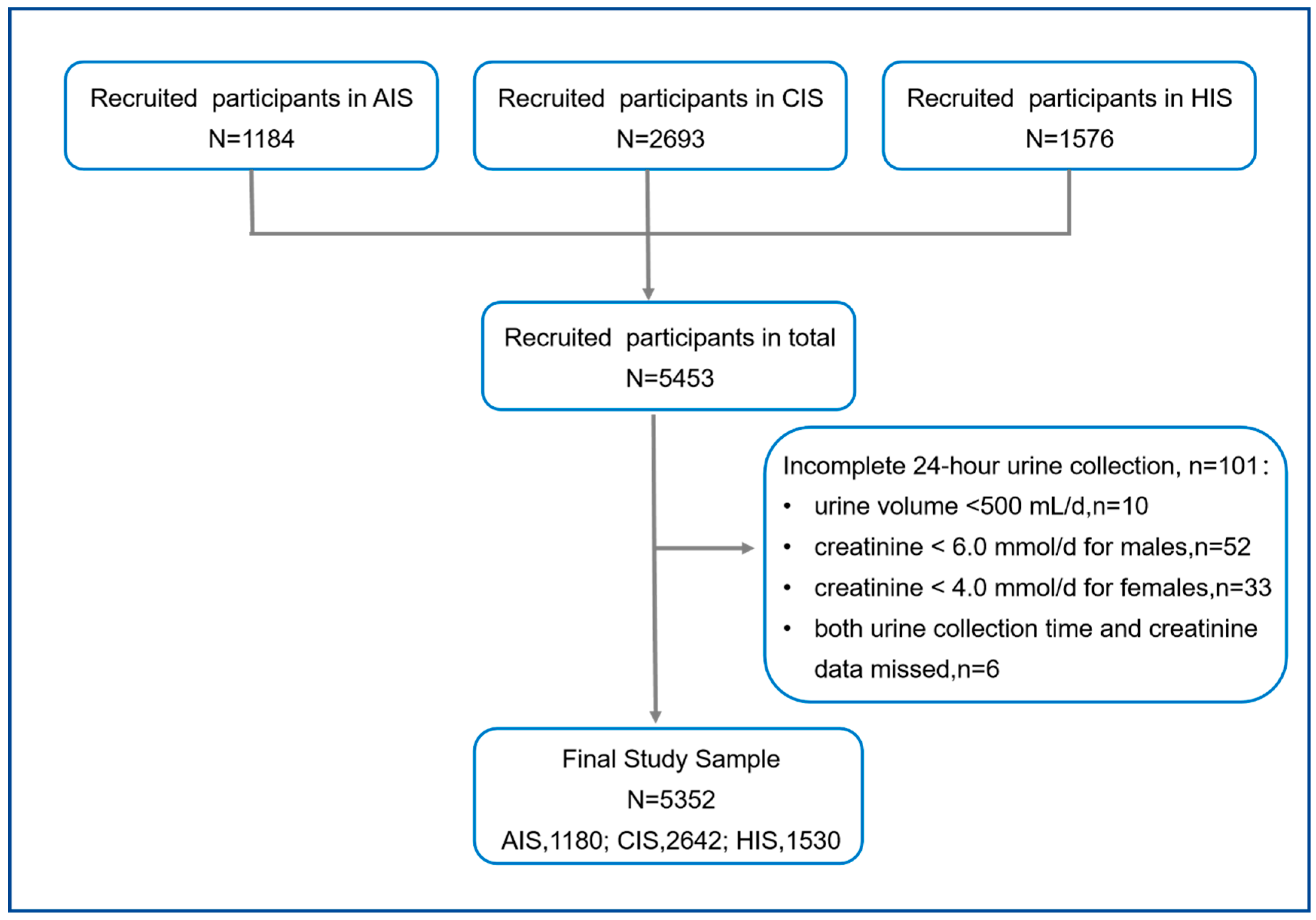
2.1. Study Design and Participants
2.2. Survey Instrument
2.3. Data Analysis
3. Results
3.1. Demographic Characteristics of Participants
3.2. Knowledge, Attitudes, and Behaviors Related to Salt Intake
3.3. Knowledge, Attitude, and Behavior Scores Related to Salt
3.4. Univariate and Multivariate Analysis of Salt-Related KAB Score
3.5. Association of Salt-Related Knowledge and Attitude Scores and the Behavior Score
3.6. Association of Salt-Related KAB Score and 24-h Urinary Sodium Excretion
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, L.; Trieu, K.; Yoshimura, S.; Neal, B.; Woodward, M.; Campbell, N.R.C.; Li, Q.; Lackland, D.T.; Leung, A.A.; Anderson, C.A.M.; et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: Systematic review and meta-analysis of randomised trials. BMJ 2020, 368, m315. [Google Scholar] [CrossRef]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Fahimi, S.; Singh, G.M.; Micha, R.; Khatibzadeh, S.; Engell, R.E.; Lim, S.; Danaei, G.; Ezzati, M.; Powles, J.; et al. Global sodium consumption and death from cardiovascular causes. N. Engl. J. Med. 2014, 371, 624–634. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Li, Y.; Zhang, P.; Wu, J.; Ma, J.; Xu, J.; Zhang, X.; Luo, R.; Liu, M.; Sun, Y.; Li, X.; et al. Twenty-Four-Hour Urinary Sodium and Potassium Excretion and Their Associations with Blood Pressure Among Adults in China: Baseline Survey of Action on Salt China. Hypertension 2020, 76, 1580–1588. [Google Scholar] [CrossRef]
- Healthy China Promotion Committee. The Healthy China Action (2019–2030). Available online: http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm (accessed on 22 May 2022).
- Bhat, S.; Marklund, M.; Henry, M.E.; Appel, L.J.; Croft, K.D.; Neal, B.; Wu, J.H.Y. A Systematic Review of the Sources of Dietary Salt around the World. Adv. Nutr. 2020, 11, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Okuda, N.; Okayama, A.; Miura, K.; Yoshita, K.; Saito, S.; Nakagawa, H.; Sakata, K.; Miyagawa, N.; Chan, Q.; Elliott, P.; et al. Food sources of dietary sodium in the Japanese adult population: The international study of macro-/micronutrients and blood pressure (INTERMAP). Eur. J. Nutr. 2017, 56, 1269–1280. [Google Scholar] [CrossRef]
- Takimoto, H.; Saito, A.; Htun, N.C.; Abe, K. Food items contributing to high dietary salt intake among Japanese adults in the 2012 National Health and Nutrition Survey. Hypertens. Res. 2018, 41, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Hua, Y.; Yang, Y.; Liu, X.; Fan, J.; Zhang, A.; Xiang, J.; Li, M.; Yan, L.L. Salt reduction in China: A state-of-the-art review. Risk Manag. Healthc. Policy 2017, 10, 17–28. [Google Scholar] [CrossRef]
- Du, S.; Wang, H.; Zhang, B.; Popkin, B.M. Dietary Potassium Intake Remains Low and Sodium Intake Remains High, and Most Sodium is Derived from Home Food Preparation for Chinese Adults, 1991–2015 Trends. J. Nutr. 2020, 150, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; He, F.J.; Ding, J.; Li, Y.; Zhang, P.; MacGregor, G.A. Salt content of sauces in the UK and China: Cross-sectional surveys. BMJ Open 2019, 9, e025623. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Reducing Salt Intake in Populations: Report of a WHO Forum and Technical Meeting, 5–7 October 2006; World Health Organization: Paris, France, 2014. [Google Scholar]
- He, F.J.; Brinsden, H.C.; MacGregor, G.A. Salt reduction in the United Kingdom: A successful experiment in public health. J. Hum. Hypertens. 2014, 28, 345–352. [Google Scholar] [CrossRef]
- Xu, A.; Ma, J.; Guo, X.; Wang, L.; Wu, J.; Zhang, J.; Bai, Y.; Xu, J.; Lu, Z.; Xu, Z.; et al. Association of a Province-Wide Intervention With Salt Intake and Hypertension in Shandong Province, China, 2011–2016. JAMA Intern. Med. 2020, 180, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, A.Q.; Ma, J.X.; Shi, X.M.; Guo, X.L.; Engelgau, M.; Yan, L.X.; Li, Y.; Li, Y.C.; Wang, H.C.; et al. Dietary sodium intake: Knowledge, attitudes and practices in Shandong Province, China, 2011. PLoS ONE 2013, 8, e58973. [Google Scholar] [CrossRef]
- Xiao, C.; You, K.; Cheng, W.; Zhang, Y.; Zhang, S.; Zhao, H.; Li, C. Investigation on knowledge, attitude and behavior on salt and health among primary and secondary school students in Shunyi District of Beijing. Occup. Health 2017, 33, 1114–1116. [Google Scholar]
- He, F.J.; Wu, Y.; Feng, X.X.; Ma, J.; Ma, Y.; Wang, H.; Zhang, J.; Yuan, J.; Lin, C.P.; Nowson, C.; et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): Cluster randomised controlled trial. BMJ 2015, 350, h770. [Google Scholar] [CrossRef]
- He, F.J.; Zhang, P.; Li, Y.; MacGregor, G.A. Action on Salt China. Lancet 2018, 392, 7–9. [Google Scholar] [CrossRef]
- He, F.J.; Zhang, P.; Luo, R.; Li, Y.; Chen, F.; Zhao, Y.; Zhao, W.; Li, D.; Chen, H.; Wu, T.; et al. An Application-based programme to reinforce and maintain lower salt intake (AppSalt) in schoolchildren and their families in China. BMJ Open 2019, 9, e027793. [Google Scholar] [CrossRef]
- Zhang, X.; Hu, X.; Ma, J.; Zhang, P.; Li, Y.; Luo, R.; He, F.J.; MacGregor, G.A.; Wang, J.; Yin, Z. Cluster randomised controlled trial of home cook intervention to reduce salt intake in China: A protocol study. BMJ Open 2020, 10, e033842. [Google Scholar] [CrossRef]
- Xu, J.; Tang, B.; Liu, M.; Bai, Y.; Yan, W.; Zhou, X.; Xu, Z.; He, J.; Jin, D.; Sun, J.; et al. A town level comprehensive intervention study to reduce salt intake in China: Protocol for a cluster randomised controlled trial. BMJ Open 2020, 10, e032976. [Google Scholar] [CrossRef] [PubMed]
- Du, W.; Zhang, J.; Li, Y.; He, F.J.; Zhou, X.; Xu, Z.; Gao, Y.; Yin, L.; Chang, X.; Yan, W.; et al. Restaurant interventions for salt reduction in China: Protocol for a randomised controlled trial. BMJ Open 2020, 10, e038744. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.M.; Rose, A.M.C.; Hambleton, I.R.; Howitt, C.; Forouhi, N.G.; Hennis, A.J.M.; Samuels, T.A.; Unwin, N. Sodium and potassium excretion in an adult Caribbean population of African descent with a high burden of cardiovascular disease. BMC Public Health 2018, 18, 998. [Google Scholar] [CrossRef] [PubMed]
- Stolarz-Skrzypek, K.; Kuznetsova, T.; Thijs, L.; Tikhonoff, V.; Seidlerová, J.; Richart, T.; Jin, Y.; Olszanecka, A.; Malyutina, S.; Casiglia, E.; et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. Jama 2011, 305, 1777–1785. [Google Scholar] [CrossRef] [PubMed]
- Hanbazaza, M.A.; Mumena, W.A. Knowledge and Practices Related to Salt Intake among Saudi Adults. Int. J. Environ. Res. Public Health 2020, 17, 5749. [Google Scholar] [CrossRef]
- Bhana, N.; Utter, J.; Eyles, H. Knowledge, Attitudes and Behaviours Related to Dietary Salt Intake in High-Income Countries: A Systematic Review. Curr. Nutr. Rep. 2018, 7, 183–197. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Shan, L.C.; Tao, W.; Lu, T.; Regan, A.; Han, H.; Guo, L.; Deng, T.; Wall, P. A survey of Chinese consumers’ knowledge, beliefs and behavioural intentions regarding salt intake and salt reduction. Public Health Nutr. 2020, 23, 1450–1459. [Google Scholar] [CrossRef]
- Grimes, C.A.; Kelley, S.J.; Stanley, S.; Bolam, B.; Webster, J.; Khokhar, D.; Nowson, C.A. Knowledge, attitudes and behaviours related to dietary salt among adults in the state of Victoria, Australia 2015. BMC Public Health 2017, 17, 532. [Google Scholar] [CrossRef]
- Du, X.; Fang, L.; Xu, J.; Chen, X.; Bai, Y.; Wu, J.; Wu, L.; Zhong, J. The association of knowledge, attitudes and behaviors related to salt with 24-h urinary sodium, potassium excretion and hypertensive status. Sci. Rep. 2022, 12, 13901. [Google Scholar] [CrossRef]
- McKenzie, B.; Santos, J.A.; Trieu, K.; Thout, S.R.; Johnson, C.; Arcand, J.; Webster, J.; McLean, R. The Science of Salt: A focused review on salt-related knowledge, attitudes and behaviors, and gender differences. J. Clin. Hypertens. 2018, 20, 850–866. [Google Scholar] [CrossRef]
- Dickson-Spillmann, M.; Siegrist, M. Consumers’ knowledge of healthy diets and its correlation with dietary behaviour. J. Hum. Nutr. Diet. 2011, 24, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Webster, J.L.; Li, N.; Dunford, E.K.; Nowson, C.A.; Neal, B.C. Consumer awareness and self-reported behaviours related to salt consumption in Australia. Asia Pac. J. Clin. Nutr. 2010, 19, 550–554. [Google Scholar] [PubMed]
- Maimaiti, M.; Zhao, X.; Jia, M.; Ru, Y.; Zhu, S. How we eat determines what we become: Opportunities and challenges brought by food delivery industry in a changing world in China. Eur. J. Clin. Nutr. 2018, 72, 1282–1286. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Lin, W.; Cen, S.; Zhu, H.; Duan, M.; Li, W.; Zhu, S. The online-to-offline (O2O) food delivery industry and its recent development in China. Eur. J. Clin. Nutr. 2021, 75, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.D.; Resqueti, V.R.; Lima, I.; Dias, F.A.; Glynn, L.; Fregonezi, G.A. Educational interventions for improving control of blood pressure in patients with hypertension: A systematic review protocol. BMJ Open 2015, 5, e006583. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.X.; Bhimla, A.; Zhu, L.; Beeber, M.; Aczon, F.; Tan, Y.; Quinn, S.B.; Khan, O.; Gadegbeku, C.A. Development of an Intervention to Promote Physical Activity and Reduce Dietary Sodium Intake for Preventing Hypertension and Chronic Disease in Filipino Americans. J. Racial Ethn. Health Dispar. 2021, 8, 283–292. [Google Scholar] [CrossRef]
- The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on Cardiovascular Health and Diseases Burden in China: An Updated Summary of 2020. Chin. Circ. J. 2021, 36, 521. [Google Scholar]
- Disease Control and Prevention Bureau at National Health Commission. Report on Nutrition and Chronic Diseases in China. 2020. Available online: http://www.scio.gov.cn/xwfbh/xwbfbh/wqfbh/42311/44583/wz44585/Document/1695276/1695276.htm?from=timeline (accessed on 22 May 2022).
- Tan, M.; He, F.; Morris, J.K.; MacGregor, G. Reducing daily salt intake in China by 1 g could prevent almost 9 million cardiovascular events by 2030: A modelling study. BMJ Nutr. Prev. Health 2022, in press. [Google Scholar] [CrossRef]
- Zhang, X.; Du, W.; Zhang, J.; Bai, J.; Ouyang, Y.; Huang, F.; Wang, H. Association between the frequencies of eating out and overweight/obesity among dinners in restaurants aged 18–65 years in 6 Provinces of China. Chin. J. Health Educ. 2020, 36, 779–792. [Google Scholar]
- Song, J.; Brown, M.K.; Tan, M.; MacGregor, G.A.; Webster, J.; Campbell, N.R.C.; Trieu, K.; Ni Mhurchu, C.; Cobb, L.K.; He, F.J. Impact of color-coded and warning nutrition labelling schemes: A systematic review and network meta-analysis. PLoS Med. 2021, 18, e1003765. [Google Scholar] [CrossRef]
- Corvalán, C.; Reyes, M.; Garmendia, M.L.; Uauy, R. Structural responses to the obesity and non-communicable diseases epidemic: Update on the Chilean law of food labelling and advertising. Obes. Rev. 2019, 20, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Kanter, R.; Vanderlee, L.; Vandevijvere, S. Front-of-package nutrition labelling policy: Global progress and future directions. Public Health Nutr. 2018, 21, 1399–1408. [Google Scholar] [CrossRef] [PubMed]
| Participants’ Characteristics | n | % |
|---|---|---|
| Location | ||
| Urban | 1437 | 26.8 |
| Rural | 3915 | 73.2 |
| Sex | ||
| Male | 2601 | 48.6 |
| Female | 2751 | 51.4 |
| Age, year; mean (SD) | 49.76 | 12.84 |
| Age groups; year | ||
| 18–44 | 2014 | 37.6 |
| 45–59 | 1863 | 34.8 |
| ≥60 | 1475 | 27.6 |
| Education levels | ||
| Low | 2136 | 39.9 |
| Medium | 1800 | 33.6 |
| High | 1416 | 26.5 |
| Hypertension * | 1841 | 34.4 |
| No | 3511 | 65.6 |
| Old diagnosed | 1076 | 20.1 |
| New observed | 765 | 14.3 |
| SBP, mm Hg; mean (SD) | 125.62 | 19.16 |
| DBP, mm Hg; mean (SD) | 79.2 | 11.24 |
| Scores; mean (SD) | ||
| Score of knowledge | 4.80 | 5.14 |
| Score of attitudes | 9.33 | 3.93 |
| Score of behaviors | 17.14 | 4.43 |
| Score of overall KAB | 31.27 | 9.18 |
| Urinary volume, mL/24 h; mean (SD) | 1602.97 | 650.98 |
| Urinary creatinine, mmol/24 h; mean (SD) | 10.62 | 3.23 |
| Urinary sodium, mmol/24 h; mean (SD) | 187.70 | 77.48 |
| Questions | n | % |
|---|---|---|
| Knowledge (3 questions) | ||
| Do you know what is the recommended maximum level of salt per day? | ||
| Less than 2 g | 114 | 2.13 |
| Less than 5 g * | 1198 | 22.38 |
| Less than 8 g | 108 | 2.02 |
| Less than 12 g | 78 | 1.46 |
| More than 12 g | 22 | 0.41 |
| Don’t know | 3832 | 71.60 |
| Have you heard of low-sodium salt? | ||
| Yes * | 1638 | 30.61 |
| No | 3714 | 69.39 |
| Which item on this food label represents the salt content? | ||
| Energy | 103 | 1.93 |
| Protein | 60 | 1.12 |
| Fat | 29 | 0.54 |
| Carbohydrates | 225 | 4.20 |
| Sodium * | 2305 | 43.07 |
| Don’t know | 2630 | 49.14 |
| Attitudes (3 questions) | ||
| Do you agree high salt intake would cause hypertension? | ||
| Agree * | 4079 | 76.21 |
| Disagree | 406 | 7.59 |
| Don’t know | 867 | 16.20 |
| Do you agree low salt intake would make people limb weakened? | ||
| Agree | 2965 | 55.40 |
| Disagree * | 1513 | 28.27 |
| Don’t know | 874 | 16.33 |
| Would you like to choose a lower-salt diet? | ||
| Yes * | 4389 | 82.01 |
| No | 907 | 16.95 |
| Don’t know | 56 | 1.04 |
| Behaviors (6 questions) | ||
| What is your usual taste for food? | ||
| More Salty | 1587 | 29.65 |
| Moderate | 2327 | 43.48 |
| Less Salty | 1438 | 26.87 |
| Do you use low-sodium salt at home? | ||
| Yes | 556 | 10.39 |
| No | 835 | 15.60 |
| Don’t know | 3961 | 74.01 |
| How often have you consumed pickled foods in the past month? | ||
| Almost every day | 624 | 11.66 |
| 3–5 days per week | 433 | 8.09 |
| 1–2 days per week | 1046 | 19.54 |
| Once per week or less | 3249 | 60.71 |
| How often have you consumed salty snacks in the past month? | ||
| Almost every day | 39 | 0.73 |
| 3–5 days per week | 68 | 1.27 |
| 1–2 days per week | 327 | 6.11 |
| Once per week or less | 4918 | 91.89 |
| How often did you eat out or order delivery in the past month? | ||
| Almost every day | 198 | 3.70 |
| 3–5 days per week | 348 | 6.50 |
| 1–2 days per week | 705 | 13.17 |
| Once per week or less | 3013 | 56.30 |
| Never | 1088 | 20.33 |
| Have you requested for less-salted meals when eating out in the past month? (n = 4264) a | ||
| Always | 275 | 6.45 |
| Sometimes | 226 | 5.30 |
| Occasionally | 228 | 5.35 |
| Never | 3535 | 82.90 |
| Variables | Score of Knowledge | Score of Attitudes | Score of Behaviors | Score of KAB | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | t/F | p-Value | Mean ± SD | t/F | p-Value | Mean ± SD | t/F | p-Value | Mean ± SD | t/F | p-Value | |
| Location | ||||||||||||
| Urban | 7.25 ± 5.21 | 21.062 | <0.001 | 10.36 ± 3.79 | 12.056 | <0.001 | 17.98 ± 4.67 | 8.313 | <0.001 | 35.59 ± 8.83 | 21.963 | <0.001 |
| Rural | 3.93 ± 4.82 | 8.94 ± 3.92 | 16.80 ± 4.31 | 29.64 ± 8.81 | ||||||||
| Sex | ||||||||||||
| Male | 4.99 ± 5.08 | 2.241 | 0.025 | 8.79 ± 4.14 | −9.726 | <0.001 | 16.54 ± 4.49 | −9.319 | <0.001 | 30.27 ± 9.35 | −7.458 | <0.001 |
| Female | 4.67 ± 5.21 | 9.83 ± 3.66 | 17.67 ± 4.32 | 32.13 ± 8.96 | ||||||||
| Age groups | ||||||||||||
| 18–44 | 6.56 ± 5.16 | 222.543 | <0.001 | 9.88 ± 3.97 | 32.200 | <0.001 | 16.27 ± 4.38 | 97.452 | <0.001 | 32.65 ± 9.49 | 39.706 | <0.001 |
| 45–59 | 4.32 ± 4.96 | 9.02 ± 3.88 | 17.07 ± 4.40 | 30.36 ± 9.17 | ||||||||
| ≥60 | 3.09 ± 4.59 | 8.95 ± 3.87 | 18.36 ± 4.30 | 30.37 ± 8.56 | ||||||||
| Education levels | ||||||||||||
| Low | 1.74 ± 3.19 | 1353.959 | <0.001 | 8.57 ± 3.75 | 112.157 | <0.001 | 17.39 ± 4.22 | 18.544 | <0.001 | 27.69 ± 7.18 | 547.889 | <0.001 |
| Medium | 4.99 ± 4.67 | 9.24 ± 4.05 | 16.60 ± 4.37 | 30.77 ± 8.95 | ||||||||
| High | 9.22 ± 4.81 | 10.55 ± 3.74 | 17.38 ± 4.77 | 37.11 ± 9.29 | ||||||||
| Hypertension | ||||||||||||
| No | 5.34 ± 5.22 | 57.901 | <0.001 | 9.43 ± 4.03 | 5.064 | 0.006 | 17.05 ± 4.43 | 4.838 | 0.008 | 31.77 ± 9.38 | 18.023 | <0.001 |
| Old diagnosed | 4.26 ± 4.98 | 8.94 ± 3.93 | 16.97 ± 4.50 | 30.16 ± 9.20 | ||||||||
| New observed | 3.55 ± 4.73 | 9.25 ± 3.58 | 17.51 ± 4.42 | 30.32 ± 8.40 | ||||||||
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Location | ||||
| Urban | ref | ref | ||
| Rural | −5.924(−6.458, −5.390) | <0.001 | −1.165(−2.488, −0.150) | 0.031 |
| Sex | ||||
| Male | ref | ref | ||
| Female | 1.857(1.364, 2.350) | <0.001 | 2.734(2.291, 3.186) | <0.001 |
| Age groups | ||||
| 18–44 | ref | ref | ||
| 45–59 | −2.297(−2.870, −1.719) | <0.001 | 0.437(−0.129, 0.997) | 0.129 |
| ≥60 | −2.296(−2.913, −1.680) | <0.001 | 1.350(0.696, 2.002) | <0.001 |
| Education levels | ||||
| Low | ref | ref | ||
| Medium | 3.140(2.612, 3.669) | <0.001 | 3.802(3.255, 4.342) | <0.001 |
| High | 9.453(8.888, 10.018) | <0.001 | 9.266(8.628, 9.902) | <0.001 |
| Hypertension | ||||
| No | ref | ref | ||
| Old diagnosed | −1.638(−2.350, −0.923) | <0.001 | −0.345(−0.997, 0.312) | 0.302 |
| New observed | −1.484(−2.110, −0.859) | <0.001 | −0.037(−0.637, 0.567) | 0.905 |
| Variables | Univariate Analysis | Multivariate Analysis * | ||
|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Score of knowledge | 0.102(0.080, 0.126) | <0.001 | 0.143(0.116, 0.169) | <0.001 |
| Score of attitudes | 0.214(0.184, 0.243) | <0.001 | 0.178(0.149, 0.207) | <0.001 |
| Variables | Models | β (95% CI) | p-Value |
|---|---|---|---|
| Score of knowledge | model 1 | −1.046 (−1.478, −0.634) | <0.001 |
| model 2 | −1.456 (−1.893, −1.038) | <0.001 | |
| model 3 | −0.800 (−1.285, −0.312) | 0.001 | |
| Score of attitudes | model 1 | −0.850 (−1.388, −0.323) | 0.002 |
| model 2 | −0.595 (−1.132, −0.067) | 0.029 | |
| model 3 | −0.284 (−0.816, 0.247) | 0.295 | |
| Score of behaviors | model 1 | −2.697 (−3.175, −2.220) | <0.001 |
| model 2 | −2.275 (−2.760, −1.792) | <0.001 | |
| model 3 | −2.200 (−2.673, −1.716) | <0.001 | |
| Scores of overall KAB | model 1 | −1.124 (−1.364, −0.897) | <0.001 |
| model 2 | −1.069 (−1.306, −0.841) | <0.001 | |
| model 3 | −0.851 (−1.095, −0.602) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, F.; Li, Y.; Li, L.; Nie, X.; Zhang, P.; Li, Y.; Luo, R.; Zhang, G.; Wang, L.; He, F.J. Salt-Related Knowledge, Attitudes, and Behaviors and Their Relationship with 24-Hour Urinary Sodium Excretion in Chinese Adults. Nutrients 2022, 14, 4404. https://doi.org/10.3390/nu14204404
Fan F, Li Y, Li L, Nie X, Zhang P, Li Y, Luo R, Zhang G, Wang L, He FJ. Salt-Related Knowledge, Attitudes, and Behaviors and Their Relationship with 24-Hour Urinary Sodium Excretion in Chinese Adults. Nutrients. 2022; 14(20):4404. https://doi.org/10.3390/nu14204404
Chicago/Turabian StyleFan, Fang, Yinghua Li, Li Li, Xueqiong Nie, Puhong Zhang, Yuan Li, Rong Luo, Gang Zhang, Lanlan Wang, and Feng J. He. 2022. "Salt-Related Knowledge, Attitudes, and Behaviors and Their Relationship with 24-Hour Urinary Sodium Excretion in Chinese Adults" Nutrients 14, no. 20: 4404. https://doi.org/10.3390/nu14204404
APA StyleFan, F., Li, Y., Li, L., Nie, X., Zhang, P., Li, Y., Luo, R., Zhang, G., Wang, L., & He, F. J. (2022). Salt-Related Knowledge, Attitudes, and Behaviors and Their Relationship with 24-Hour Urinary Sodium Excretion in Chinese Adults. Nutrients, 14(20), 4404. https://doi.org/10.3390/nu14204404






