The Mediterranean Diet and the Western Diet in Adolescent Depression-Current Reports
Abstract
1. Introduction
2. Materials and Methods
- (1)
- Studies published in English.
- (2)
- Longitudinal, cross-sectional, case-control, clinical, interventional studies carried out mainly on humans, carried out in a group of adolescents.
- (3)
- Research on the relationship between diet quality or patterns and depression or major depressive disorder.
- (1)
- Studies published in a language other than English.
- (2)
- Research carried out in groups other than adolescents.
- (3)
- Research on eating disorders and the relationship between body weight and depression.
- (4)
- Depression reported as a secondary problem to other diseases.
- (5)
- Studies that determined the effects of drugs or psychological treatments on depression.
- (6)
- Research on the influence of family practices and parental attitudes on food consumption and child mental health.
- (7)
- Studies with pregnant teenagers.
- (8)
- Animal studies.
3. Adolescent Depression as a Current Social and Health Problem
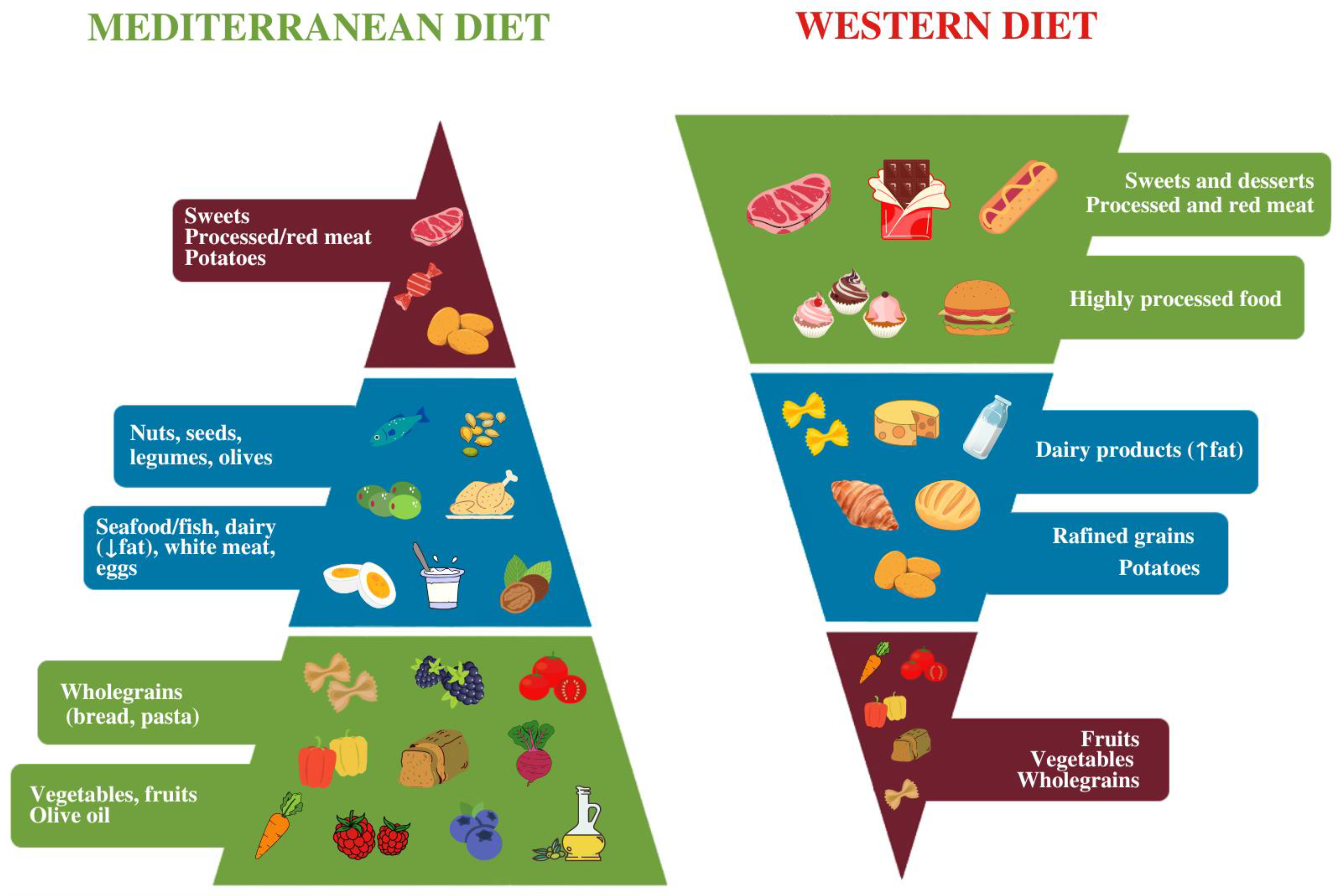
4. Mediterranean Diet-Characteristics and Potential in Adolescent Depression
5. Analysis of Eating Behavior/Patterns in the Context of the Mediterranean Diet
6. Analysis of Nutrient Intake/Condition in the Context of the Mediterranean Diet
7. Limitations and Future Directions
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Adolescent Health. Available online: https://www.who.int/health-topics/adolescent-health (accessed on 2 September 2022).
- WHO. Adolescent Mental Health. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 2 September 2022).
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Mayne, S.L.; Hannan, C.; Davis, M.; Young, J.F.; Kelly, M.K.; Powell, M.; Dalembert, G.; McPeak, K.E.; Jenssen, B.P.; Fiks, A.G. COVID-19 and Adolescent Depression and Suicide Risk Screening Outcomes. Pediatrics 2021, 148, e2021051507. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; DSM-5; American Psychiatric Publishing: Arlington, TX, USA, 2013. [Google Scholar]
- Price, R.B.; Rosen, D.; Siegle, G.J.; Ladouceur, C.D.; Tang, K.; Allen, K.B.; Ryan, N.D.; Dahl, R.E.; Forbes, E.E.; Silk, J.S. From anxious youth to depressed adolescents: Prospective prediction of 2-year depression symptoms via attentional bias measures. J. Abnorm. Psychol. 2016, 125, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Thapar, A.; Collishaw, S.; Pine, D.S.; Thapar, A.K. Depression in adolescence. Lancet 2012, 379, 1056–1067. [Google Scholar] [CrossRef]
- Cairns, K.E.; Yap, M.B.; Pilkington, P.D.; Jorm, A.F. Risk and protective factors for depression that adolescents can modify: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2014, 169, 61–75. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Kovacs, M.; Obrosky, S.; George, C. The course of major depressive disorder from childhood to young adulthood: Recovery and recurrence in a longitudinal observational study. J. Affect. Disord. 2016, 203, 374–381. [Google Scholar] [CrossRef]
- Beirao, D.; Monte, H.; Amaral, M.; Longras, A.; Matos, C.; Villas-Boas, F. Depression in adolescence: A review. Middle East Curr. Psychiatry 2020, 27, 50. [Google Scholar] [CrossRef]
- Forman-Hoffman, V.; McClure, E.; McKeeman, J.; Wood, C.T.; Middleton, J.C.; Skinner, A.C.; Perrin, E.M.; Viswanathan, M. Screening for major depressive disorder in children and adolescents: A systematic review for the US preventive services task force. Ann. Intern. Med. 2016, 164, 342. [Google Scholar] [CrossRef]
- Eskin, M. Suicidal Behavior in the Mediterranean Countries. Clin. Pract. Epidemiol. Ment. Health 2020, 16, 93–100. [Google Scholar] [CrossRef]
- Available online: https://www.cdc.gov/healthyyouth/mental-health/index.html (accessed on 2 September 2022).
- Devitt, P. Can we expect an increased suicide rate due to Covid-19? Ir. J. Psychol. Med. 2020, 37, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Estradé, A.; Thompson, T.; Agorastos, A.; Radua, J.; Cortese, S.; Dragioti, E.; Leisch, F.; Vancampfort, D.; Thygesen, L.C.; et al. Physical and mental health impact of COVID-19 on children, adolescents, and their families: The Collaborative Outcomes study on Health and Functioning during Infection Times—Children and Adolescents (COH-FIT-C&A). J. Affect. Disord. 2022, 299, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain. Behav. Immun. 2020, 87, 49–50. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child. Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors Associated with Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Solomou, I.; Constantinidou, F. Prevalence and Predictors of Anxiety and Depression Symptoms during the COVID-19 Pandemic and Compliance with Precautionary Measures: Age and Sex Matter. Int. J. Environ. Res. Public Health 2020, 17, 4924. [Google Scholar] [CrossRef]
- Tang, S.; Xiang, M.; Cheung, T.; Xiang, Y.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef]
- Shah, S.M.A.; Mohammad, D.; Qureshi, M.F.H.; Abbas, M.Z.; Aleem, S. Prevalence, Psychological Responses and Associated Correlates of Depression, Anxiety and Stress in a Global Population, During the Coronavirus Disease (COVID-19) Pandemic. Community Ment. Health J. 2021, 57, 101–110. [Google Scholar] [CrossRef]
- Nearchou, F.; Flinn, C.; Niland, R.; Subramaniam, S.S.; Hennessy, E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8479. [Google Scholar] [CrossRef] [PubMed]
- Marques de Miranda, D.; da Silva Athanasio, B.; Sena Oliveira, A.C.; Simoes-E-Silva, A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster. Risk. Reduct. 2020, 51, 101845. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child. Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef] [PubMed]
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr. Neurosci. 2019, 22, 474–487. [Google Scholar] [CrossRef] [PubMed]
- Opie, R.S.; O’Neil, A.; Jacka, F.N.; Pizzinga, J.; Itsiopoulos, C. A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial. Nutr. Neurosci. 2018, 21, 487–501. [Google Scholar] [CrossRef]
- Sadeghi, O.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Adherence to Mediterranean dietary pattern is inversely associated with depression, anxiety and psychological distress. Nutr. Neurosci. 2021, 24, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Francis, H.M.; Stevenson, R.J.; Chambers, J.R.; Gupta, D.; Newey, B.; Lim, C.K. A brief diet intervention can reduce symptoms of depression in young adults—A randomised controlled trial. PLoS ONE 2019, 14, e0222768. [Google Scholar] [CrossRef]
- Li, Y.; Lv, M.R.; Wei, Y.J.; Sun, L.; Zhang, J.X.; Zhang, H.G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Cabrera-Suárez, B.; Molero, P.; González-Pinto, A.; Chiclana-Actis, C.; Cabrera, C.; Lahortiga-Ramos, F.; Florido-Rodríguez, M.; Vega-Pérez, P.; Pla, J.; et al. Preventing the recurrence of depression with a Mediterranean diet supplemented with extra-virgin olive oil. The PREDI-DEP trial: Study protocol. BMC Psychiatry 2019, 19, 63. [Google Scholar] [CrossRef]
- Masana, M.F.; Haro, J.M.; Mariolis, A.; Piscopo, S.; Valacchi, G.; Bountziouka, V.; Anastasiou, F.; Zeimbekis, A.; Tyrovola, D.; Gotsis, E.; et al. Mediterranean diet and depression among older individuals: The multinational MEDIS study. Exp. Gerontol. 2018, 110, 67–72. [Google Scholar] [CrossRef]
- Valls-Pedret, C.; Sala-Vila, A.; Serra-Mir, M.; Corella, D.; de la Torre, R.; Martínez-González, M.Á.; Martínez-Lapiscina, E.H.; Fitó, M.; Pérez-Heras, A.; Salas-Salvadó, J.; et al. Mediterranean Diet and Age-Related Cognitive Decline: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Mantzorou, M.; Vadikolias, K.; Pavlidou, E.; Tryfonos, C.; Vasios, G.; Serdari, A.; Giaginis, C. Mediterranean diet adherence is associated with better cognitive status and less depressive symptoms in a Greek elderly population. Aging Clin. Exp. Res. 2021, 33, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Vall Castelló, J.; Tubianosa, C. Linking Mediterranean Diet and Lifestyle with Cardio Metabolic Disease and Depressive Symptoms: A Study on the Elderly in Europe. Int. J. Environ. Res. Public Health 2020, 17, 7053. [Google Scholar] [CrossRef] [PubMed]
- Rice, F.; Riglin, L.; Lomax, T.; Souter, E.; Potter, R.; Smith, D.J.; Thapar, A.K.; Thapar, A. Adolescent and adult differences in major depression symptom profiles. J. Affect. Disord. 2019, 243, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Locher, C.; Koechlin, H.; Zion, S.R.; Werner, C.; Pine, D.S.; Kirsch, I.; Kessler, R.C.; Kossowsky, J. Efficacy and Safety of Selective Serotonin Reuptake Inhibitors, Serotonin-Norepinephrine Reuptake Inhibitors, and Placebo for Common Psychiatric Disorders Among Children and Adolescents: A Systematic Review and Meta-analysis. JAMA Psychiatry 2017, 74, 1011–1020. [Google Scholar] [CrossRef]
- Lu, C.Y.; Zhang, F.; Lakoma, M.D.; Madden, J.M.; Rusinak, D.; Penfold, R.B.; Simon, G.; Ahmedani, B.K.; Clarke, G.; Hunkeler, E.M.; et al. Changes in antidepressant use by young people and suicidal behavior after FDA warnings and media coverage: Quasi-experimental study. BMJ 2014, 348, g3596. [Google Scholar] [CrossRef] [PubMed]
- Marx, W.; Moseley, G.; Berk, M.; Jacka, F. Nutritional psychiatry: The present state of the evidence. Proc. Nutr. Soc. 2017, 76, 427–436. [Google Scholar] [CrossRef]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sánchez-Villegas, A.; Kivimäki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef]
- Opie, R.S.; Itsiopoulos, C.; Parletta, N.; Sanchez-Villegas, A.; Akbaraly, T.N.; Ruusunen, A.; Jacka, F.N. Dietary recommendations for the prevention of depression. Nutr. Neurosci. 2017, 20, 161–171. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef]
- Morris, L.; Bhatnagar, D. The Mediterranean diet. Curr. Opin. Lipidol. 2016, 27, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet; a Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef] [PubMed]
- Guilleminault, L.; Williams, E.J.; Scott, H.A.; Berthon, B.S.; Jensen, M.; Wood, L.G. Diet and Asthma: Is It Time to Adapt Our Message? Nutrients 2017, 9, 1227. [Google Scholar] [CrossRef]
- Sureda, A.; Bibiloni, M.D.M.; Julibert, A.; Bouzas, C.; Argelich, E.; Llompart, I.; Pons, A.; Tur, J.A. Adherence to the Mediterranean Diet and Inflammatory Markers. Nutrients 2018, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- Orlando, L.; Savel, K.A.; Madigan, S.; Colasanto, M.; Korczak, D.J. Dietary patterns and internalizing symptoms in children and adolescents: A meta-analysis. Aust. N. Zeal. J. Psychiatry 2022, 56, 617–641. [Google Scholar] [CrossRef] [PubMed]
- Khanna, P.; Chattu, V.K.; Aeri, B.T. Nutritional Aspects of Depression in Adolescents—A Systematic Review. Int. J. Prev. Med. 2019, 10, 42. [Google Scholar] [CrossRef] [PubMed]
- Marx, W.; Lane, M.; Hockey, M.; Aslam, H.; Berk, M.; Walder, K.; Borsini, A.; Firth, J.; Pariante, C.M.; Berding, K.; et al. Diet and depression: Exploring the biological mechanisms of action. Mol. Psychiatry 2021, 26, 134–150. [Google Scholar] [CrossRef]
- Marx, W.; Lane, M.M.; Hockey, M.; Aslam, H.; Walder, K.; Borsini, A.; Firth, J.; Pariante, C.M.; Berding, K.; Cryan, J.F.; et al. Diet and depression: Future needs to unlock the potential. Mol. Psychiatry 2022, 27, 778–780. [Google Scholar] [CrossRef]
- Dehghan, P.; Nejati, M.; Vahid, F.; Almasi-Hashiani, A.; Saleh-Ghadimi, S.; Parsi, R.; Jafari-Vayghan, H.; Shivappa, N.; Hébert, J.R. The association between dietary inflammatory index, dietary antioxidant index, and mental health in adolescent girls: An analytical study. BMC Public Health 2022, 22, 1513. [Google Scholar] [CrossRef]
- Korczak, D.J.; Perruzza, S.; Chandrapalan, M.; Cost, K.; Cleverley, K.; Birken, C.S.; McCrindle, B.M. The association of diet and depression: An analysis of dietary measures in depressed, non-depressed, and healthy youth. Nutr. Neurosci. 2021, 25, 1948–1955. [Google Scholar] [CrossRef]
- Khalid, S.; Williams, C.M.; Reynolds, S.A. Is there an association between diet and depression in children and adolescents? A systematic review. Br. J. Nutr. 2016, 116, 2097–2108. [Google Scholar] [CrossRef] [PubMed]
- Voltas, N.; Arija, V.; Aparicio, E.; Canals, J. Longitudinal study of psychopathological, anthropometric and sociodemographic factors related to the level of Mediterranean diet adherence in a community sample of Spanish adolescents. Public Health Nutr. 2016, 19, 1812–1822. [Google Scholar] [CrossRef]
- Wilson, J.E.; Blizzard, L.; Gall, S.L.; Magnussen, C.G.; Oddy, W.H.; Dwyer, T.; Venn, A.J.; Smith, K.J. Youth diet quality and hazard of mood disorder in adolescence and adulthood among an Australian cohort. J. Affect. Disord. 2020, 276, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Winpenny, E.M.; van Harmelen, A.L.; White, M.; van Sluijs, E.M.; Goodyer, I.M. Diet quality and depressive symptoms in adolescence: No cross-sectional or prospective associations following adjustment for covariates. Public Health Nutr. 2018, 21, 2376–2384. [Google Scholar] [CrossRef] [PubMed]
- Chopra, C.; Mandalika, S.; Kinger, N. Does diet play a role in the prevention and management of depression among adolescents? A narrative review. Nutr. Health. 2021, 27, 243–263. [Google Scholar] [CrossRef] [PubMed]
- Oddy, W.H.; Allen, K.L.; Trapp, G.S.A.; Ambrosini, G.L.; Black, L.J.; Huang, R.C.; Rzehak, P.; Runions, K.C.; Pan, F.; Beilin, L.J.; et al. Dietary patterns, body mass index and inflammation: Pathways to depression and mental health problems in adolescents. Brain Behav. Immun. 2018, 69, 428–439. [Google Scholar] [CrossRef] [PubMed]
- Haapakoski, R.; Mathieu, J.; Ebmeier, K.P.; Alenius, H.; Kivimäki, M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav. Immun. 2015, 49, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Zalli, A.; Jovanova, O.; Hoogendijk, W.J.; Tiemeier, H.; Carvalho, L.A. Low-grade inflammation predicts persistence of depressive symptoms. Psychopharmacol. 2016, 233, 1669–1678. [Google Scholar] [CrossRef]
- Colasanto, M.; Madigan, S.; Korczak, D.J. Depression and inflammation among children and adolescents: A meta-analysis. J. Affect. Disord. 2020, 277, 940–948. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Marx, W.; Dash, S.; Carney, R.; Teasdale, S.B.; Solmi, M.; Stubbs, B.; Schuch, F.B.; Carvalho, A.F.; Jacka, F.; et al. The Effects of Dietary Improvement on Symptoms of Depression and Anxiety: A Meta-Analysis of Randomized Controlled Trials. Psychosom. Med. 2019, 81, 265–280. [Google Scholar] [CrossRef]
- Arouca, A.; Michels, N.; Moreno, L.A.; González-Gil, E.M.; Marcos, A.; Gómez, S.; Díaz, L.E.; Widhalm, K.; Molnár, D.; Manios, Y.; et al. Associations between a Mediterranean diet pattern and inflammatory biomarkers in European adolescents. Eur. J. Nutr. 2018, 57, 1747–1760. [Google Scholar] [CrossRef] [PubMed]
- Arouca, A.B.; Santaliestra-Pasías, A.M.; Moreno, L.A.; Marcos, A.; Widhalm, K.; Molnár, D.; Manios, Y.; Gottrand, F.; Kafatos, A.; Kersting, M.; et al. Diet as a moderator in the association of sedentary behaviors with inflammatory biomarkers among adolescents in the HELENA study. Eur. J. Nutr. 2019, 58, 2051–2065. [Google Scholar] [CrossRef]
- Carvalho, K.M.B.; Ronca, D.B.; Michels, N.; Huybrechts, I.; Cuenca-Garcia, M.; Marcos, A.; Molnár, D.; Dallongeville, J.; Manios, Y.; Schaan, B.D.; et al. Does the Mediterranean Diet Protect against Stress-Induced Inflammatory Activation in European Adolescents? The HELENA Study. Nutrients 2018, 10, 1770. [Google Scholar] [CrossRef]
- Esteban-Cornejo, I.; Izquierdo-Gomez, R.; Gómez-Martínez, S.; Padilla-Moledo, C.; Castro-Piñero, J.; Marcos, A.; Veiga, O.L. Adherence to the Mediterranean diet and academic performance in youth: The UP&DOWN study. Eur. J. Nutr. 2016, 55, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Hemmati, A.; Ghoreishy, S.M.; Karami, K.; Imani, H.; Farsani, G.M.; Mousavi, S.E.; Asoudeh, F.; Shariati-Bafghi, S.E.; Karamati, M. The association between dietary patterns and depression in adolescents: A cross-sectional study. Clin. Nutr. ESPEN 2021, 46, 271–275. [Google Scholar] [CrossRef]
- Hryhorczuk, C.; Florea, M.; Rodaros, D.; Poirier, I.; Daneault, C.; Des Rosiers, C.; Arvanitogiannis, A.; Alquier, T.; Fulton, S. Dampened Mesolimbic Dopamine Function and Signaling by Saturated but not Monounsaturated Dietary Lipids. Neuropsychopharmacology 2016, 41, 811–821. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Ordaz, R.; Wall-Medrano, A.; Goñi, M.G.; Ramos-Clamont-Montfort, G.; Ayala-Zavala, J.F.; González-Aguilar, G.A. Effect of phenolic compounds on the growth of selected probiotic and pathogenic bacteria. Lett. Appl. Microbiol. 2018, 66, 25–31. [Google Scholar] [CrossRef]
- Robertson, R.C.; Seira Oriach, C.; Murphy, K.; Moloney, G.M.; Cryan, J.F.; Dinan, T.G.; Paul Ross, R.; Stanton, C. Omega-3 polyunsaturated fatty acids critically regulate behaviour and gut microbiota development in adolescence and adulthood. Brain Behav. Immun. 2017, 59, 21–37. [Google Scholar] [CrossRef]
- Pasinetti, G.M.; Singh, R.; Westfall, S.; Herman, F.; Faith, J.; Ho, L. The Role of the Gut Microbiota in the Metabolism of Polyphenols as Characterized by Gnotobiotic Mice. J. Alzheimers. Dis. 2018, 63, 409–421. [Google Scholar] [CrossRef]
- Gopinath, B.; Flood, V.M.; Kifley, A.; Louie, J.C.; Mitchell, P. Association Between Carbohydrate Nutrition and Successful Aging Over 10 Years. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1335–1340. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Díaz, I.; Fernández-Navarro, T.; Sánchez, B.; Margolles, A.; González, S. Mediterranean diet and faecal microbiota: A transversal study. Food Funct. 2016, 7, 2347–2356. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.M.; Shivappa, N.; Hébert, J.R.; Perry, I.J. Dietary inflammatory index and mental health: A cross-sectional analysis of the relationship with depressive symptoms, anxiety and well-being in adults. Clin. Nutr. 2018, 37, 1485–1491. [Google Scholar] [CrossRef] [PubMed]
- Adjibade, M.; Andreeva, V.A.; Lemogne, C.; Touvier, M.; Shivappa, N.; Hébert, J.R.; Wirth, M.D.; Hercberg, S.; Galan, P.; Julia, C.; et al. The Inflammatory Potential of the Diet Is Associated with Depressive Symptoms in Different Subgroups of the General Population. J. Nutr. 2017, 147, 879–887. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Ruíz-Canela, M.; de la Fuente-Arrillaga, C.; Gea, A.; Shivappa, N.; Hébert, J.R.; Martínez-González, M.A. Dietary inflammatory index, cardiometabolic conditions and depression in the Seguimiento Universidad de Navarra cohort study. Br. J. Nutr. 2015, 114, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- Akbaraly, T.; Kerlau, C.; Wyart, M.; Chevallier, N.; Ndiaye, L.; Shivappa, N.; Hébert, J.R.; Kivimäki, M. Dietary inflammatory index and recurrence of depressive symptoms: Results from the Whitehall II Study. Clin. Psychol. Sci. 2016, 4, 1125–1134. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Schoenaker, D.A.; Hebert, J.R.; Mishra, G.D. Association between inflammatory potential of diet and risk of depression in middle-aged women: The Australian Longitudinal Study on Women’s Health. Br. J. Nutr. 2016, 116, 1077–1086. [Google Scholar] [CrossRef]
- Tehrani, A.N.; Salehpour, A.; Beyzai, B.; Farhadnejad, H.; Moloodi, R.; Hekmatdoost, A.; Rashidkhani, B. Adherence to Mediterranean dietary pattern and depression, anxiety and stress among high-school female adolescents. Mediterr. J. Nutr. Metab. 2018, 11, 73–83. [Google Scholar] [CrossRef]
- Sangouni, A.A.; Vasmehjani, A.A.; Ghayour-Mobarhan, M.; Ferns, G.A.; Khayyatzadeh, S.S. The association between dietary phytochemical index with depression and quality of life in iranian adolescent girls. Biopsychosoc. Med. 2022, 16, 5. [Google Scholar] [CrossRef]
- Hong, S.A.; Peltzer, K. Dietary behaviour, psychological well-being and mental distress among adolescents in Korea. Child Adolesc. Psychiatry Ment. Health 2017, 11, 56. [Google Scholar] [CrossRef]
- Hoare, E.; Hockey, M.; Ruusunen, A.; Jacka, F.N. Does Fruit and Vegetable Consumption During Adolescence Predict Adult Depression? A Longitudinal Study of US Adolescents. Front. Psychiatry 2018, 9, 581. [Google Scholar] [CrossRef]
- Ferrer-Cascales, R.; Sánchez-SanSegundo, M.; Ruiz-Robledillo, N.; Albaladejo-Blázquez, N.; Laguna-Pérez, A.; Zaragoza-Martí, A. Eat or Skip Breakfast? The Important Role of Breakfast Quality for Health-Related Quality of Life, Stress and Depression in Spanish Adolescents. Int. J. Environ. Res. Public Health 2018, 15, 1781. [Google Scholar] [CrossRef]
- Zhu, Z.; Cui, Y.; Gong, Q.; Huang, C.; Guo, F.; Li, W.; Zhang, W.; Chen, Y.; Cheng, X.; Wang, Y. Frequency of breakfast consumption is inversely associated with the risk of depressive symptoms among Chinese university students: A cross-sectional study. PLoS ONE 2019, 14, e0222014. [Google Scholar] [CrossRef] [PubMed]
- Khayyatzadeh, S.S.; Shafiee, M.; Far, P.E.; Ziaee, S.S.; Bagherniya, M.; Ebrahimi, S.; Boromand, N.; Ferns, G.A.; Ghayour-Mobarhan, M. Adherence to a healthy dietary pattern is associated with less severe depressive symptoms among adolescent girls. Psychiatry Res. 2019, 272, 467–473. [Google Scholar] [CrossRef]
- Tanaka, M.; Hashimoto, K. Impact of consuming green and yellow vegetables on the depressive symptoms of junior and senior high school students in Japan. PLoS ONE 2019, 14, e0211323. [Google Scholar] [CrossRef]
- Khayyatzadeh, S.S.; Omranzadeh, A.; Miri-Moghaddam, M.M.; Arekhi, S.; Naseri, A.; Ziaee, A.; Khajavi, L.; Nejati Salehkhani, F.; Ferns, G.A.; Ghayour-Mobarhan, M. Dietary antioxidants and fibre intake and depressive symptoms in Iranian adolescent girls. Public Health Nutr. 2021, 24, 5650–5656. [Google Scholar] [CrossRef]
- Gao, C.; Sun, Y.; Zhang, F.; Zhou, F.; Dong, C.; Ke, Z.; Wang, Q.; Yang, Y.; Sun, H. Prevalence and correlates of lifestyle behavior, anxiety and depression in Chinese college freshman: A cross-sectional survey. Int. J. Nurs. Sci. 2021, 8, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Cao, R.; Gao, T.; Ren, H.; Hu, Y.; Qin, Z.; Liang, L.; Li, C.; Mei, S. Unique and cumulative effects of lifestyle-related behaviors on depressive symptoms among Chinese adolescents. Int. J. Soc. Psychiatry 2022, 68, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Sangouni, A.A.; Beigrezaei, S.; Akbarian, S.; Ghayour-Mobarhan, M.; Yuzbashian, E.; Salehi-Abargouei, A.; Ferns, G.A.; Khayyatzadeh, S.S. Association between dietary behaviors and depression in adolescent girls. BMC Public Health 2022, 22, 1169. [Google Scholar] [CrossRef] [PubMed]
- Georgieff, M.K.; Ramel, S.E.; Cusick, S.E. Nutritional influences on brain development. Acta Paediatr. 2018, 107, 1310–1321. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Morze, J.; Hoffmann, G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br. J. Pharmacol. 2020, 177, 1241–1257. [Google Scholar] [CrossRef]
- Khanna, P.; Aeri, B.T. Association of Quantity and Quality of Protein Intake with Depression and Anxiety Symptoms among Adolescent Boys and Girls (13-15 Years) Studying in Public Schools of Delhi. J. Nutr. Sci. Vitaminol. 2020, 66, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Farhadnejad, H.; Neshatbini Tehrani, A.; Salehpour, A.; Hekmatdoost, A. Antioxidant vitamin intakes and risk of depression, anxiety and stress among female adolescents. Clin. Nutr. ESPEN 2020, 40, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.P.; Su, K.P. Nutritional Neuroscience as Mainstream of Psychiatry: The Evidence- Based Treatment Guidelines for Using Omega-3 Fatty Acids as a New Treatment for Psychiatric Disorders in Children and Adolescents. Clin. Psychopharmacol. Neurosci. 2020, 18, 469–483. [Google Scholar] [CrossRef]
- Chang, J.P.; Chang, S.S.; Yang, H.T.; Chen, H.T.; Chien, Y.C.; Yang, B.; Su, H.; Su, K.P. Omega-3 polyunsaturated fatty acids in cardiovascular diseases comorbid major depressive disorder—Results from a randomized controlled trial. Brain Behav. Immun. 2020, 85, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Trebatická, J.; Hradečná, Z.; Böhmer, F.; Vaváková, M.; Waczulíková, I.; Garaiova, I.; Luha, J.; Škodáček, I.; Šuba, J.; Ďuračková, Z. Emulsified omega-3 fatty-acids modulate the symptoms of depressive disorder in children and adolescents: A pilot study. Child Adolesc. Psychiatry Ment. Health 2017, 11, 30. [Google Scholar] [CrossRef] [PubMed]
- Gabbay, V.; Freed, R.D.; Alonso, C.M.; Senger, S.; Stadterman, J.; Davison, B.A.; Klein, R.G. A Double-Blind Placebo-Controlled Trial of Omega-3 Fatty Acids as a Monotherapy for Adolescent Depression. J. Clin. Psychiatry 2018, 79, 17m11596. [Google Scholar] [CrossRef]
- van der Wurff, I.S.M.; von Schacky, C.; Bergeland, T.; Leontjevas, R.; Zeegers, M.P.; Kirschner, P.A.; de Groot, R.H.M. Exploring the association between whole blood Omega-3 Index, DHA, EPA, DHA, AA and n-6 DPA, and depression and self-esteem in adolescents of lower general secondary education. Eur. J. Nutr. 2019, 58, 1429–1439. [Google Scholar] [CrossRef]
- Katrenčíková, B.; Vaváková, M.; Waczulíková, I.; Oravec, S.; Garaiova, I.; Nagyová, Z.; Hlaváčová, N.; Ďuračková, Z.; Trebatická, J. Lipid Profile, Lipoprotein Subfractions, and Fluidity of Membranes in Children and Adolescents with Depressive Disorder: Effect of Omega-3 Fatty Acids in a Double-Blind Randomized Controlled Study. Biomolecules 2020, 10, 1427. [Google Scholar] [CrossRef]
- Trebatická, J.; Hradečná, Z.; Surovcová, A.; Katrenčíková, B.; Gushina, I.; Waczulíková, I.; Sušienková, K.; Garaiova, I.; Šuba, J.; Ďuračková, Z. Omega-3 fatty-acids modulate symptoms of depressive disorder, serum levels of omega-3 fatty acids and omega-6/omega-3 ratio in children. A randomized, double-blind and controlled trial. Psychiatry Res. 2020, 287, 112911. [Google Scholar] [CrossRef]
- Paduchová, Z.; Katrenčíková, B.; Vaváková, M.; Laubertová, L.; Nagyová, Z.; Garaiova, I.; Ďuračková, Z.; Trebatická, J. The Effect of Omega-3 Fatty Acids on Thromboxane, Brain-Derived Neurotrophic Factor, Homocysteine, and Vitamin D in Depressive Children and Adolescents: Randomized Controlled Trial. Nutrients 2021, 13, 1095. [Google Scholar] [CrossRef]
- Islam, M.R.; Ali, S.; Karmoker, J.R.; Kadir, M.F.; Ahmed, M.U.; Nahar, Z.; Islam, S.M.A.; Islam, M.S.; Hasnat, A.; Islam, S. Evaluation of serum amino acids and non-enzymatic antioxidants in drug-naïve first-episode major depressive disorder. BMC Psychiatry 2020, 20, 333. [Google Scholar] [CrossRef] [PubMed]
- Geng, C.; Shaikh, A.S.; Han, W.; Chen, D.; Guo, Y.; Jiang, P. Vitamin D and depression: Mechanisms, determination and application. Asia. Pac. J. Clin. Nutr. 2019, 28, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.H.; Chiou, H.Y.; Chen, Y.H. Associations between serum homocysteine levels and anxiety and depression among children and adolescents in Taiwan. Sci. Rep. 2017, 7, 8330. [Google Scholar] [CrossRef] [PubMed]
- Yosaee, S.; Clark, C.C.T.; Keshtkaran, Z.; Ashourpour, M.; Keshani, P.; Soltani, S. Zinc in depression: From development to treatment: A comparative/dose response meta-analysis of observational studies and randomized controlled trials. Gen. Hosp. Psychiatry 2022, 74, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, A.; Khorasanchi, Z.; Sadeghnia, H.R.; Tayefi, M.; Avan, A.; Ferns, G.A.; Bahrami-Taghanaki, H.; Ghayour-Mobarhan, M. Depression in adolescent girls: Relationship to serum vitamins a and E, immune response to heat shock protein 27 and systemic inflammation. J. Affect. Disord. 2019, 252, 68–73. [Google Scholar] [CrossRef]
- Bahrami, A.; Mazloum, S.R.; Maghsoudi, S.; Soleimani, D.; Khayyatzadeh, S.S.; Arekhi, S.; Arya, A.; Mirmoosavi, S.J.; Ferns, G.A.; Bahrami-Taghanaki, H.; et al. High Dose Vitamin D Supplementation Is Associated with a Reduction in Depression Score Among Adolescent Girls: A Nine-Week Follow-Up Study. J. Diet. Suppl. 2018, 15, 173–182. [Google Scholar] [CrossRef]
- Libuda, L.; Timmesfeld, N.; Antel, J.; Hirtz, R.; Bauer, J.; Führer, D.; Zwanziger, D.; Öztürk, D.; Langenbach, G.; Hahn, D.; et al. Effect of vitamin D deficiency on depressive symptoms in child and adolescent psychiatric patients: Results of a randomized controlled trial. Eur. J. Nutr. 2020, 59, 3415–3424. [Google Scholar] [CrossRef]
- Esnafoglu, E.; Ozturan, D.D. The relationship of severity of depression with homocysteine, folate, vitamin B12, and vitamin D levels in children and adolescents. Child Adolesc. Ment. Health. 2020, 25, 249–255. [Google Scholar] [CrossRef]
- Al-Sabah, R.; Al-Taiar, A.; Shaban, L.; Albatineh, A.N.; Sharaf Alddin, R.; Durgampudi, P.K. Vitamin D level in relation to depression symptoms during adolescence. Child. Adolesc. Psychiatry Ment. Health 2022, 16, 53. [Google Scholar] [CrossRef]
- Tahmasebi, K.; Amani, R.; Nazari, Z.; Ahmadi, K.; Moazzen, S.; Mostafavi, S.A. Association of Mood Disorders with Serum Zinc Concentrations in Adolescent Female Students. Biol. Trace Elem. Res. 2017, 178, 180–188. [Google Scholar] [CrossRef]
- Gonoodi, K.; Moslem, A.; Ahmadnezhad, M.; Darroudi, S.; Mazloum, Z.; Tayefi, M.; Tabatabaeizadeh, S.A.; Eslami, S.; Shafiee, M.; Khashayarmanesh, Z.; et al. Relationship of Dietary and Serum Zinc with Depression Score in Iranian Adolescent Girls. Biol. Trace Elem. Res. 2018, 186, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Hoepner, C.T.; McIntyre, R.S.; Papakostas, G.I. Impact of Supplementation and Nutritional Interventions on Pathogenic Processes of Mood Disorders: A Review of the Evidence. Nutrients 2021, 13, 767. [Google Scholar] [CrossRef] [PubMed]
- Rainka, M.; Aladeen, T.; Westphal, E.; Meaney, J.; Gengo, F.; Greger, J.; Capote, H. L-Methylfolate Calcium Supplementation in Adolescents and Children: A Retrospective Analysis. J. Psychiatr. Pract. 2019, 25, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Nery, F.G.; Tallman, M.J.; Cecil, K.M.; Blom, T.J.; Patino, L.R.; Adler, C.M.; DelBello, M.P. N-acetylcysteine for depression and glutamate changes in the left prefrontal cortex in adolescents and young adults at risk for bipolar disorder: A pilot study. Early Interv. Psychiatry 2022, 16, 195–199. [Google Scholar] [CrossRef]
- Cullen, K.R.; Klimes-Dougan, B.; Westlund Schreiner, M.; Carstedt, P.; Marka, N.; Nelson, K.; Miller, M.J.; Reigstad, K.; Westervelt, A.; Gunlicks-Stoessel, M.; et al. N-Acetylcysteine for Nonsuicidal Self-Injurious Behavior in Adolescents: An Open-Label Pilot Study. J. Child Adolesc. Psychopharmacol. 2018, 28, 136–144. [Google Scholar] [CrossRef]
- Ligezka, A.N.; Sonmez, A.I.; Corral-Frias, M.P.; Golebiowski, R.; Lynch, B.; Croarkin, P.E.; Romanowicz, M. A systematic review of microbiome changes and impact of probiotic supplementation in children and adolescents with neuropsychiatric disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 108, 110187. [Google Scholar] [CrossRef]
- Saccarello, A.; Montarsolo, P.; Massardo, I.; Picciotto, R.; Pedemonte, A.; Castagnaro, R.; Brasesco, P.C.; Guida, V.; Piccom, P.; Fioravanti, P.; et al. Oral Administration of S-Adenosylmethionine (SAMe) and Lactobacillus Plantarum HEAL9 Improves the Mild-To-Moderate Symptoms of Depression: A Randomized, Double-Blind, Placebo-Controlled Study. Prim. Care Companion. CNS Disord. 2020, 22, 19m02578. [Google Scholar] [CrossRef]
- Murray, E.; Sharma, R.; Smith, K.B.; Mar, K.D.; Barve, R.; Lukasik, M.; Pirwani, A.F.; Malette-Guyon, E.; Lamba, S.; Thomas, B.J.; et al. Probiotic consumption during puberty mitigates LPS-induced immune responses and protects against stress-induced depression- and anxiety-like behaviors in adulthood in a sex-specific manner. Brain Behav. Immun. 2019, 81, 198–212. [Google Scholar] [CrossRef]
- Simkin, D.R. Microbiome and Mental Health, Specifically as It Relates to Adolescents. Curr. Psychiatry Rep. 2019, 21, 93. [Google Scholar] [CrossRef]
| Authors | Year of Publication | Part of the Mediterranean Diet | Age and Size of the Study Group | Results and Conclusions |
|---|---|---|---|---|
| Hong et al. [83] | 2017 | Vegetables, fruits | n = 65,212 Age: 12–18 years (mean age = 15.1 years, SD = 0.02) | Healthy eating behavior (regular consumption of fruit, vegetables, breakfast and milk) was negatively associated with perceived symptoms of stress and depression. |
| Winpenny et al. [58] | 2018 | Vegetables, fruits, and fish | n = 603 Age: 14 years (study enrollment) and 17 years (follow-up) | There were no significant associations between diet quality (MD), fruit and vegetable or fish consumption, and depression symptoms at 14 and depressive symptoms at 17, corrected for baseline depression symptoms. |
| Oddy et al. [60] | 2018 | Fruits, vegetables, fish, whole grains | n = 843 Age: 14 years (study enrollment) and 17 years (follow-up) | A diet rich in fruits, vegetables, fish and whole grains was inversely correlated with BMI and inflammation at 17 years of age (p < 0.05). The Western nutritional pattern is indirectly associated with an increased risk of developing depression symptoms in adolescents through the biological pathways of obesity. and inflammation, and a “healthy” diet appears to be protective in these pathways. |
| Hoare et al. [84] | 2018 | Vegetables, fruits | n = 3696 Age: 16 years (study enrollment) and 29 years (follow-up) | Fruit consumption was cross-sectionally associated with a lower probability of developing depression in adolescence in both men and women, both before and after controlling the covariates. Vegetable consumption among women was cross-sectionally associated with a decreased probability of developing depression in adolescence. Those who never experienced depression were the largest consumers of fruits and vegetables during adolescence. |
| Ferrer-Cascales et al. [85] | 2018 | Breakfast, cereal products, dairy products | n = 527 Age: 12–17 years (mean age = 14.30 years, SD = 1.52) | A high-quality breakfast, characterized by the consumption of grain products and dairy products, was associated with lower levels of perceived stress and depressive symptoms in adolescents. People who skipped breakfast showed lower levels of stress and depression than breakfast eaters who ate a low-quality or very low-quality breakfast. |
| Zhu et al. [86] | 2019 | Breakfast | n = 10 174 Mean age: 19.76 years, SD = 0.86 | Skipping breakfast was associated with an increased risk of depressive symptoms. and these relationships did not change after adjusting for many potentially confounding variables. Eating breakfast is crucial to reducing the incidence of depressive symptoms. |
| Khayyatzadeh et al. [87] | 2019 | Vegetables, fruits, fish, dairy products | n = 670 teenage girls Age: 12–18 years (mean age = 14.5 years, SD = 1.5) | The high consumption of fruits, vegetables, fish, and dairy products was associated with a lower incidence of depressive symptoms. However, no significant links have been found between traditional and Western eating patterns as a result of depression. |
| Tanaka et al. [88] | 2019 | Vegetables | n = 858 Mean age: 15.49 years, SD = 1.78) | Regular consumption of green and yellow vegetables reduces the symptoms of depression in adolescents. Eating vegetables in these colors can be crucial for the mental health of adolescents. |
| Khayyatzadeh et al. [89] | 2021 | Fiber | n = 988 teenage girls Age: 12–18 years (mean age: 14.5 years, SD = 1.52 and 1.54) | The consumption of soluble and insoluble dietary fiber was much higher in healthy adolescents compared to people with symptoms of depression (p < 0.001). There was a significant inverse relationship between dietary antioxidant intake and depression symptoms among Iranian teenagers. |
| Gao et al. [90] | 2021 | Breakfast | n = 1017 Mean age: 19 years, SD = 18.19 | Teenagers who skipped breakfast more than once a week had an increased risk of developing depressive symptoms compared to those who ate breakfast every day. Eating snacks between meals, desserts, and sugary beverages was significantly related to depression in univariate analyzes. |
| Cao et al. [91] | 2022 | Breakfast | n = 3967 Age: 11–19 | Lifestyle is associated with the risk of developing depressive symptoms, including skipping breakfast in both girls and boys. |
| Sangouni et al. [92] | 2022 | Breakfast | n = 933 teenage girls Age: 12–18 years | There was a significant difference between the depression score categories for main meal consumption (p < 0.001) and regular meal consumption (p < 0.001). There was no significant relationship between breakfast consumption and the depression score (p = 0.007), snack consumption (p = 0.002), and consumption of fried foods (p > 0.05). |
| Authors | Year of Publication | Age and Size of the Study Group | Results and Conclusions |
|---|---|---|---|
| Macronutrients: | |||
| Khanna et al. [95] | 2020 | n = 546 Age: 13–15 years, SD = 0.5 | Low consumption of protein-rich foods such as milk and legumes was significantly associated with higher mean depression scores. Stronger relationships have been observed with milk protein consumption, especially during breakfast meals. |
| Farhadnejad et al. [96] | 2020 | n = 263 teenage girls Age: 15–18 years (mean age: 16.20 years, SD = 0.97) | Participants with depression had lower protein intakes (% energy) and a higher proportion of carbohydrates in the diet (p < 0.05) compared to people without depression. |
| Authors | Year of Publication | Age and Size of the Study Group | Results and Conclusions |
|---|---|---|---|
| Fatty Acids: | |||
| Trebatická et al. [99] | 2017 | n = 35 Age: 11–17 (mean age: 15.5 years, SD = 1.5) n = 17 omega-3 group, n = 18 omega-6 group) | Significant decreases in depression scores were observed in the 35 patients who completed the 12-week intervention after the 12-week intervention only in the Omega-3 group (p = 0.034). Fish oil (57.2% EPA and 42.8% DHA) may be an effective supplement to standard antidepressant therapy. in the treatment of depressive disorders in adolescents. |
| Gabbay et al. [100] | 2018 | n = 48 Age: 12–19 years (n = 21—omega-3 group, n = 27—placebo group) | A 10-week randomized, placebo-controlled study of omega-3 fatty acids in adolescents with severe depression (MDD) did not show improvement in response to omega-3 fatty acids (final dose = 3.6 g/day, EPA to DHA ratio 2:1) compared to placebo for the severity of depression, anhedonia, irritability, and suicidal tendency. |
| van Wurff et al. [101] | 2020 | n = 257 Age: 13–15 years (mean age: 14.11 years, SD = 0.55) | No evidence was found to link DHA, EPA and the omega-3 index (O3I) to depression in adolescents. One possible explanation for the lack of association in the present study could be that the design of this study was participant selection. with O3I ≤ 5%. |
| Katrenčíková et al. [102] | 2020 | n = 78 (58 depressed patients aged 15.6 ± 1.6 years, 20 healthy people aged 14.8 ± 2.4 years) | Supplementation with omega-3 fatty acids increased non-atherogenic HDL subfractions. HDL-CH and its subfractions, but not LDL-CH, may play a role in the pathophysiology of depressive disorders. |
| Trebatická et al. [103] | 2020 | n = 58 Age: 11–17 (mean age: 15.7 years, SD = 1.6) (n = 29 omega-6, n = 29 omega-3) | An emulsion of fish oil rich in omega-3 acids can be an effective supplement to standard antidepressant therapy in the treatment of depressive disorders in adolescents. |
| Paduchová et al. [104] | 2021 | n = 58 Mean age: 15.6 years, SD = 1.6 | There was a significant positive correlation between the severity of depression or the omega-6/omega-3 FA ratio and plasma thromboxane B and a negative correlation with brain-derived neurotrophic factor (BDNF). Children and adolescents with depressive disorders had higher levels of thromboxane B and decreased vitamin D levels compared to healthy controls. Supplementation with omega-3 FA in conjunction with standard antidepressant therapy may have a beneficial effect on thromboxane levels. However, the positive effect of omega-3 FA supplementation on BDNF levels was observed only in patients with depression. |
| Authors | Year of Publication | Age and Size of the Study Group | Results and Conclusions |
|---|---|---|---|
| Antioxidant Vitamins (A, C, E): | |||
| Bahrami et al. [109] | 2019 | n = 563 teenage girls Age: 12–18 years (mean age 14.5 years, SD = 1.5) | There were no differences between people with high and low depression scores with respect to vitamins A, E, and their corrected lipid levels (p > 0.05). |
| Farhadnejad et al. [96] | 2020 | n = 263 teenage girls Age: 15–18 years (mean age 16.20 years, SD = 0.97) | Higher β-carotene consumption of -carotene was associated with a lower incidence of depression, anxiety, and stress. Vitamin C consumption was not associated with the risk of depression and anxiety stress and stress. A higher vitamin E intake was associated with a lower risk of stress. |
| Khayyatzadeh et al. [89] | 2021 | n = 988 teenage girls Age: 12–18 years (mean age: 14.5 years, SD = 1.52) | People with no or minimal depression symptoms had a significantly higher intake of α-carotene (p = 0.01), β-carotene (p = 0.006), lutein (p = 0.03) and vitamin C (p = 0.04) in compared to people with mild to severe symptoms of depression. Higher dietary intakes of vitamin C, but not vitamin E, were associated with fewer symptoms of depression among adolescents. |
| Vitamin D: | |||
| Bahrami et al. [110] | 2018 | n = 988 Mean age: 14.56 years, SD = 1.53 | Vitamin D capsules (50,000 IU of D3/1 time per week for 9 weeks) showed a significant reduction in the total depression score of BDII (p = 0.001). A high dose of vitamin D once a week can be useful in alleviating symptoms of depression. |
| Libuda et al. [111] | 2020 | n = 113 Age: 11.0–18.9 years (n = 56 vitamin D supplementation, n = 57 placebo group) | Vitamin D supplementation (2640 IU of vitamin D once a day) in children and adolescents who suffered from depression with vitamin D deficiency did not result in a significant reduction in self-reported depression symptoms, but a significant reduction in parent-reported depressive symptoms after 4 weeks of stationary or daily treatment compared to placebo. |
| Esnafoglu et al. [112] | 2020 | n = 89 with a mean age of 15.08, SD = 1.46 with depressive disorders, n = 43, mean age control group 14.41 years, SD = 2.32 | Vitamin D levels were significantly lower in the group of teens with depressive disorders (p < 0.001). Lower vitamin D levels have been shown to play a role in the pathogenesis of depression in adolescents. It is recommended that clinicians test vitamin D levels in adolescents with depression. |
| Al-Sabah et al. [113] | 2022 | n = 704 Age: 11–16 years Mean age: 12.25 years, SD = 0.8 | There was no significant correlation between serum 25(OH)D concentration and the result of depression symptoms measured with the Pediatric Depression Inventory (CDI). |
| Vitamins of group B: | |||
| Esnafoglu et al. [112] | 2020 | n = 89 with a mean age of 15.08, SD = 1.46 with depressive disorders, n = 43, mean age control group 14.41 years, SD = 2.32 | There were no significant differences between the groups in terms of folate levels (p = 0.052). The depressed group had extremely low vitamin B12 levels compared to the control group (p < 0.001). Low vitamin B12 levels and elevated homocysteine levels may play a role in the pathogenesis of depression in adolescents. |
| Minerals: | |||
| Zinc: | |||
| Tahmasebi et al. [114] | 2017 | n = 100 Age: 15–20 years (mean age: 17.9 years, SD = 1.2) | Each 10 μg/dL increase in serum zinc resulted in a 0.3 and 0.01 decrease in depression and anxiety scores, respectively (p < 0.05). Serum zinc levels were inversely correlated with mood disorders, including depression and anxiety in adolescents. |
| Gonoodi et al. [115] | 2018 | n = 408 Age: 12–18 years (mean age: 15.2 years, SD = 1.5) | Dietary zinc consumption (7.04 ± 4.28 mg/day) was significantly lower among those with mild or severe symptoms of depression than among those with no or minimal symptoms of depression (8.06 ± 3.03 mg/day). Dietary zinc consumption was inversely correlated with the depression score (r = 0.133, p = 0.008). Dietary zinc consumption, but not serum zinc concentration, was inversely related to depressive symptoms. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zielińska, M.; Łuszczki, E.; Michońska, I.; Dereń, K. The Mediterranean Diet and the Western Diet in Adolescent Depression-Current Reports. Nutrients 2022, 14, 4390. https://doi.org/10.3390/nu14204390
Zielińska M, Łuszczki E, Michońska I, Dereń K. The Mediterranean Diet and the Western Diet in Adolescent Depression-Current Reports. Nutrients. 2022; 14(20):4390. https://doi.org/10.3390/nu14204390
Chicago/Turabian StyleZielińska, Magdalena, Edyta Łuszczki, Izabela Michońska, and Katarzyna Dereń. 2022. "The Mediterranean Diet and the Western Diet in Adolescent Depression-Current Reports" Nutrients 14, no. 20: 4390. https://doi.org/10.3390/nu14204390
APA StyleZielińska, M., Łuszczki, E., Michońska, I., & Dereń, K. (2022). The Mediterranean Diet and the Western Diet in Adolescent Depression-Current Reports. Nutrients, 14(20), 4390. https://doi.org/10.3390/nu14204390







