Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018
Abstract
1. Introduction
2. Materials and Methods
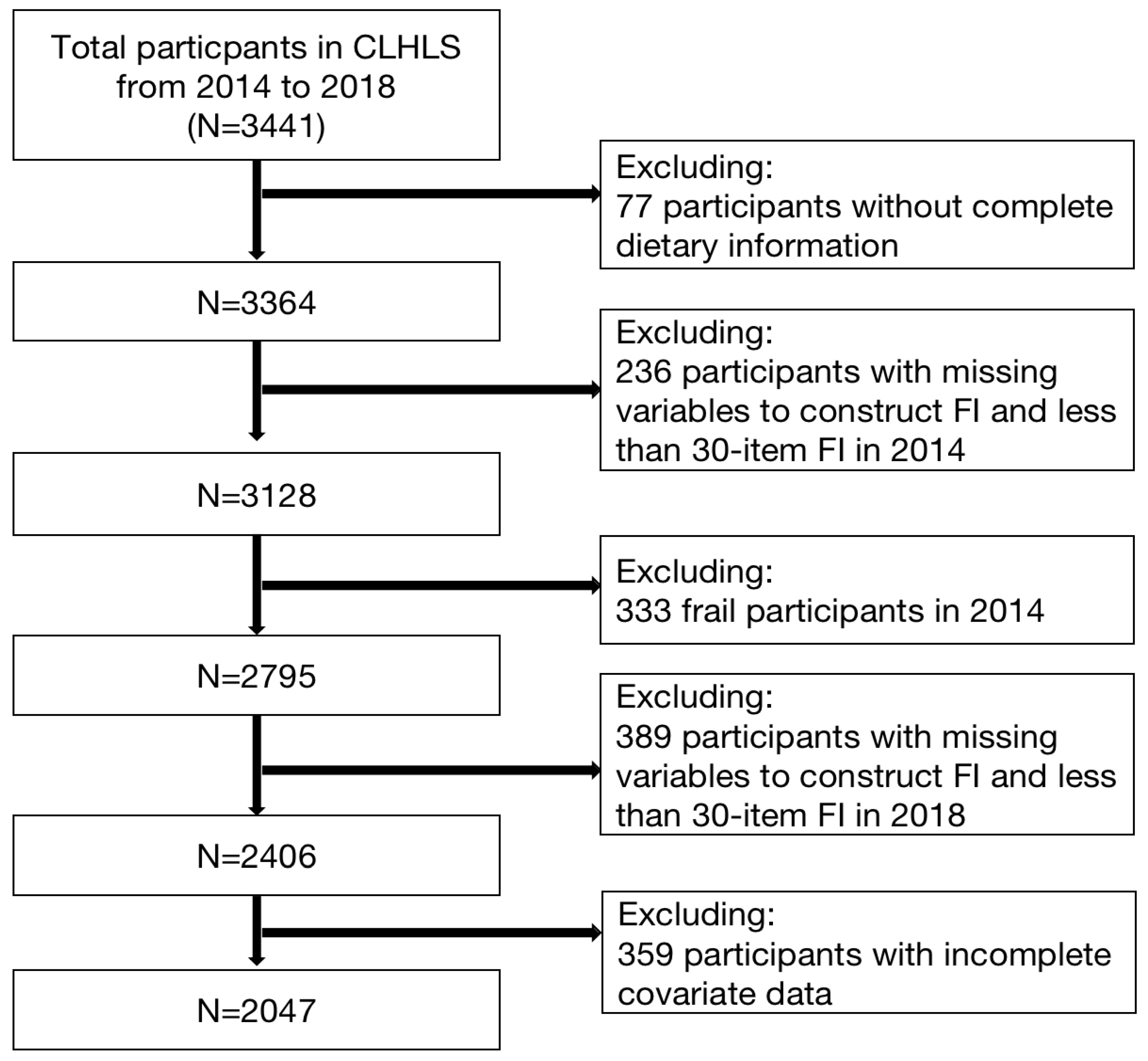
2.1. Data Collection and Population
2.2. Food Variety Measurement
2.3. Dietary Pattern Measurement
2.4. Frailty Index
2.5. Covariates
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 21 June 2022).
- Available online: http://www.gov.cn/xinwen/2018-07/19/content_5307839.htm (accessed on 21 June 2022).
- Wong, A.; Wouterse, B.; Slobbe, L.C.J.; Boshuizen, H.C.; Polder, J.J. Medical Innovation and Age-Specific Trends in Health Care Utilization: Findings and Implications. Soc. Sci. Med. 2012, 74, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in Elderly People. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Ewing, S.K.; Cawthon, P.M.; Fink, H.A.; Taylor, B.C.; Cauley, J.A.; Dam, T.-T.; Marshall, L.M.; Orwoll, E.S.; Cummings, S.R.; et al. A Comparison of Frailty Indexes for the Prediction of Falls, Disability, Fractures, and Mortality in Older Men. J. Am. Geriatr. Soc. 2009, 57, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.-Y.; Liu, X.; Xue, Q.-L.; Chen, S.; Wu, C. The Association between Frailty and Healthcare Expenditure among Chinese Older Adults. J. Am. Med. Dir. Assoc. 2020, 21, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Puts, M.T.E.; Toubasi, S.; Andrew, M.K.; Ashe, M.C.; Ploeg, J.; Atkinson, E.; Ayala, A.P.; Roy, A.; Rodríguez Monforte, M.; Bergman, H.; et al. Interventions to Prevent or Reduce the Level of Frailty in Community-Dwelling Older Adults: A Scoping Review of the Literature and International Policies. Age Ageing 2017, 46, 383–392. [Google Scholar] [CrossRef]
- Dent, E.; Martin, F.C.; Bergman, H.; Woo, J.; Romero-Ortuno, R.; Walston, J.D. Management of Frailty: Opportunities, Challenges, and Future Directions. Lancet 2019, 394, 1376–1386. [Google Scholar] [CrossRef]
- Vetrano, D.L.; Triolo, F.; Maggi, S.; Malley, R.; Jackson, T.A.; Poscia, A.; Bernabei, R.; Ferrucci, L.; Fratiglioni, L. Fostering Healthy Aging: The Interdependency of Infections, Immunity and Frailty. Ageing Res. Rev. 2021, 69, 101351. [Google Scholar] [CrossRef]
- Jennings, A.; Berendsen, A.M.; de Groot, L.C.P.G.M.; Feskens, E.J.M.; Brzozowska, A.; Sicinska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugère, C.; et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef]
- Iuliano, S.; Poon, S.; Robbins, J.; Bui, M.; Wang, X.; De Groot, L.; Van Loan, M.; Zadeh, A.G.; Nguyen, T.; Seeman, E. Effect of Dietary Sources of Calcium and Protein on Hip Fractures and Falls in Older Adults in Residential Care: Cluster Randomised Controlled Trial. BMJ 2021, 375, n2364. [Google Scholar] [CrossRef]
- Lin, C.-C.; Shih, M.-H.; Chen, C.-D.; Yeh, S.-L. Effects of Adequate Dietary Protein with Whey Protein, Leucine, and Vitamin D Supplementation on Sarcopenia in Older Adults: An Open-Label, Parallel-Group Study. Clin. Nutr. 2021, 40, 1323–1329. [Google Scholar] [CrossRef]
- Nakazaki, E.; Mah, E.; Sanoshy, K.; Citrolo, D.; Watanabe, F. Citicoline and Memory Function in Healthy Older Adults: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. J. Nutr. 2021, 151, 2153–2160. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Diet Collaborators. Health Effects of Dietary Risks in 195 Countries, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, A. Dietary Diversity and Healthy Aging: A Prospective Study. Nutrients 2021, 13, 1787. [Google Scholar] [CrossRef] [PubMed]
- Yokoro, M.; Otaki, N.; Yano, M.; Tani, M.; Tanino, N.; Fukuo, K. Associations between Dietary Variety and Frailty in Community-Dwelling Older People Who Live Alone: Gender Differences. J. Frailty Aging 2022. [Google Scholar] [CrossRef]
- Kim, J.; Yang, S.; Kim, H.; Chang, E.; Kim, Y. Association Between Frailty and Dietary Diversity in Korean Elderly: Based on the 2018 Korean National Health and Nutrition Examination Survey. Curr. Dev. Nutr. 2021, 5, 1050. [Google Scholar] [CrossRef]
- Hayakawa, M.; Motokawa, K.; Mikami, Y.; Yamamoto, K.; Shirobe, M.; Edahiro, A.; Iwasaki, M.; Ohara, Y.; Watanabe, Y.; Kawai, H.; et al. Low Dietary Variety and Diabetes Mellitus Are Associated with Frailty among Community-Dwelling Older Japanese Adults: A Cross-Sectional Study. Nutrients 2021, 13, 641. [Google Scholar] [CrossRef] [PubMed]
- Otaki, N.; Yano, M.; Yokoro, M.; Tanino, N.; Fukuo, K. Relationship Between Dietary Variety and Frailty in Older Japanese Women During the Period of Restriction on Outings Due to COVID-19. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2021, 76, e256–e262. [Google Scholar] [CrossRef]
- Motokawa, K.; Watanabe, Y.; Edahiro, A.; Shirobe, M.; Murakami, M.; Kera, T.; Kawai, H.; Obuchi, S.; Fujiwara, Y.; Ihara, K.; et al. Frailty Severity and Dietary Variety in Japanese Older Persons: A Cross-Sectional Study. J. Nutr. Health Aging 2018, 22, 451–456. [Google Scholar] [CrossRef]
- Huang, W.-C.; Huang, Y.-C.; Lee, M.-S.; Chang, H.-Y.; Doong, J.-Y. Frailty Severity and Cognitive Impairment Associated with Dietary Diversity in Older Adults in Taiwan. Nutrients 2021, 13, 418. [Google Scholar] [CrossRef]
- Yeung, S.S.Y.; Zhu, Z.L.Y.; Chan, R.S.M.; Kwok, T.; Woo, J. Prospective Analysis of Fruit and Vegetable Variety on Health Outcomes in Community-Dwelling Chinese Older Adults. J. Nutr. Health Aging 2021, 25, 735–741. [Google Scholar] [CrossRef]
- Rahi, B.; Ajana, S.; Tabue-Teguo, M.; Dartigues, J.-F.; Peres, K.; Feart, C. High Adherence to a Mediterranean Diet and Lower Risk of Frailty among French Older Adults Community-Dwellers: Results from the Three-City-Bordeaux Study. Clin. Nutr. 2018, 37, 1293–1298. [Google Scholar] [CrossRef] [PubMed]
- de Haas, S.C.M.; de Jonge, E.A.L.; Voortman, T.; Graaff, J.S.; Franco, O.H.; Ikram, M.A.; Rivadeneira, F.; Kiefte-de Jong, J.C.; Schoufour, J.D. Dietary Patterns and Changes in Frailty Status: The Rotterdam Study. Eur. J. Nutr. 2018, 57, 2365–2375. [Google Scholar] [CrossRef] [PubMed]
- León-Muñoz, L.M.; García-Esquinas, E.; López-García, E.; Banegas, J.R.; Rodríguez-Artalejo, F. Major Dietary Patterns and Risk of Frailty in Older Adults: A Prospective Cohort Study. BMC Med. 2015, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.; Leung, J.; Woo, J. Dietary Patterns and Risk of Frailty in Chinese Community-Dwelling Older People in Hong Kong: A Prospective Cohort Study. Nutrients 2015, 7, 7070–7084. [Google Scholar] [CrossRef] [PubMed]
- Lo, Y.-L.; Hsieh, Y.-T.; Hsu, L.-L.; Chuang, S.-Y.; Chang, H.-Y.; Hsu, C.-C.; Chen, C.-Y.; Pan, W.-H. Dietary Pattern Associated with Frailty: Results from Nutrition and Health Survey in Taiwan. J. Am. Geriatr. Soc. 2017, 65, 2009–2015. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, Y.; Wu, H.; He, G.; Li, S.; Chen, B. Association between Dietary Patterns and Frailty Prevalence in Shanghai Suburban Elders: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 10852. [Google Scholar] [CrossRef]
- Theou, O.; Rockwood, K. Comparison and Clinical Applications of the Frailty Phenotype and Frailty Index Approaches. Interdiscip. Top. Gerontol. Geriatr. 2015, 41, 74–84. [Google Scholar] [CrossRef]
- Mitnitski, A.B.; Mogilner, A.J.; Rockwood, K. Accumulation of Deficits as a Proxy Measure of Aging. ScientificWorldJournal 2001, 1, 323–336. [Google Scholar] [CrossRef]
- Gu, D.; Dupre, M.E.; Sautter, J.; Zhu, H.; Liu, Y.; Yi, Z. Frailty and Mortality among Chinese at Advanced Ages. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2009, 64, 279–289. [Google Scholar] [CrossRef]
- Gu, D.; Feng, Q. Frailty Still Matters to Health and Survival in Centenarians: The Case of China. BMC Geriatr. 2015, 15, 159. [Google Scholar] [CrossRef]
- Aihemaitijiang, S.; Zhang, L.; Ye, C.; Halimulati, M.; Huang, X.; Wang, R.; Zhang, Z. Long-Term High Dietary Diversity Maintains Good Physical Function in Chinese Elderly: A Cohort Study Based on CLHLS from 2011 to 2018. Nutrients 2022, 14, 1730. [Google Scholar] [CrossRef] [PubMed]
- Searle, S.D.; Mitnitski, A.; Gahbauer, E.A.; Gill, T.M.; Rockwood, K. A Standard Procedure for Creating a Frailty Index. BMC Geriatr. 2008, 8, 24. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.; Song, X.; Mitnitski, A.; Rockwood, K. A Limit to Frailty in Very Old, Community-Dwelling People: A Secondary Analysis of the Chinese Longitudinal Health and Longevity Study. Age Ageing 2013, 42, 372–377. [Google Scholar] [CrossRef]
- Song, Y.; Deng, Y.; Li, J.; Hao, B.; Cai, Y.; Chen, J.; Shi, H.; Xu, W. Associations of Falls and Severe Falls with Blood Pressure and Frailty among Chinese Community-Dwelling Oldest Olds: The Chinese Longitudinal Health and Longevity Study. Aging 2021, 13, 16527–16540. [Google Scholar] [CrossRef] [PubMed]
- Claesson, M.J.; Jeffery, I.B.; Conde, S.; Power, S.E.; O’Connor, E.M.; Cusack, S.; Harris, H.M.B.; Coakley, M.; Lakshminarayanan, B.; O’Sullivan, O.; et al. Gut Microbiota Composition Correlates with Diet and Health in the Elderly. Nature 2012, 488, 178–184. [Google Scholar] [CrossRef]
- Kim, S.; Jazwinski, S.M. The Gut Microbiota and Healthy Aging: A Mini-Review. Gerontology 2018, 64, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Stubbs, B.; Noale, M.; Solmi, M.; Rizzoli, R.; Vaona, A.; Demurtas, J.; Crepaldi, G.; Maggi, S. Adherence to a Mediterranean Diet Is Associated with Lower Incidence of Frailty: A Longitudinal Cohort Study. Clin. Nutr. 2018, 37, 1492–1497. [Google Scholar] [CrossRef]
- Talegawkar, S.A.; Bandinelli, S.; Bandeen-Roche, K.; Chen, P.; Milaneschi, Y.; Tanaka, T.; Semba, R.D.; Guralnik, J.M.; Ferrucci, L. A Higher Adherence to a Mediterranean-Style Diet Is Inversely Associated with the Development of Frailty in Community-Dwelling Elderly Men and Women. J. Nutr. 2012, 142, 2161–2166. [Google Scholar] [CrossRef]
- Bollwein, J.; Diekmann, R.; Kaiser, M.J.; Bauer, J.M.; Uter, W.; Sieber, C.C.; Volkert, D. Dietary Quality Is Related to Frailty in Community-Dwelling Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 483–489. [Google Scholar] [CrossRef]
- Ward, R.E.; Orkaby, A.R.; Chen, J.; Hshieh, T.T.; Driver, J.A.; Gaziano, J.M.; Djousse, L. Association between Diet Quality and Frailty Prevalence in the Physicians’ Health Study. J. Am. Geriatr. Soc. 2020, 68, 770–776. [Google Scholar] [CrossRef]
- Ocké, M.C. Evaluation of Methodologies for Assessing the Overall Diet: Dietary Quality Scores and Dietary Pattern Analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Mulero, J.; Zafrilla, P.; Martinez-Cacha, A. Oxidative Stress, Frailty and Cognitive Decline. J. Nutr. Health Aging 2011, 15, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, R.R.; Miller, S.L.; Miller, K.B. Optimal Protein Intake in the Elderly. Clin. Nutr. 2008, 27, 675–684. [Google Scholar] [CrossRef]
- Beasley, J.M.; LaCroix, A.Z.; Neuhouser, M.L.; Huang, Y.; Tinker, L.; Woods, N.; Michael, Y.; Curb, J.D.; Prentice, R.L. Protein Intake and Incident Frailty in the Women’s Health Initiative Observational Study. J. Am. Geriatr. Soc. 2010, 58, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Ghosh, M.; Ganguli, A. Mitogenic Response and Probiotic Characteristics of Lactic Acid Bacteria Isolated from Indigenously Pickled Vegetables and Fermented Beverages. World J. Microbiol. Biotechnol. 2012, 28, 703–711. [Google Scholar] [CrossRef]
- Laclaustra, M.; Rodriguez-Artalejo, F.; Guallar-Castillon, P.; Banegas, J.R.; Graciani, A.; Garcia-Esquinas, E.; Ordovas, J.; Lopez-Garcia, E. Prospective Association between Added Sugars and Frailty in Older Adults. Am. J. Clin. Nutr. 2018, 107, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Struijk, E.A.; Rodríguez-Artalejo, F.; Fung, T.T.; Willett, W.C.; Hu, F.B.; Lopez-Garcia, E. Sweetened Beverages and Risk of Frailty among Older Women in the Nurses’ Health Study: A Cohort Study. PLoS Med. 2020, 17, e1003453. [Google Scholar] [CrossRef]
- Hsieh, T.-J.; Su, S.-C.; Chen, C.-W.; Kang, Y.-W.; Hu, M.-H.; Hsu, L.-L.; Wu, S.-Y.; Chen, L.; Chang, H.-Y.; Chuang, S.-Y.; et al. Individualized Home-Based Exercise and Nutrition Interventions Improve Frailty in Older Adults: A Randomized Controlled Trial. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 119. [Google Scholar] [CrossRef]
- Roschel, H.; Hayashi, A.P.; Fernandes, A.L.; Jambassi-Filho, J.C.; Hevia-Larraín, V.; de Capitani, M.; Santana, D.A.; Gonçalves, L.S.; de Sá-Pinto, A.L.; Lima, F.R.; et al. Supplement-Based Nutritional Strategies to Tackle Frailty: A Multifactorial, Double-Blind, Randomized Placebo-Controlled Trial. Clin. Nutr. 2021, 40, 4849–4858. [Google Scholar] [CrossRef]
- Zuniga, K.E.; Parma, D.L.; Muñoz, E.; Spaniol, M.; Wargovich, M.; Ramirez, A.G. Dietary Intervention among Breast Cancer Survivors Increased Adherence to a Mediterranean-Style, Anti-Inflammatory Dietary Pattern: The Rx for Better Breast Health Randomized Controlled Trial. Breast Cancer Res. Treat. 2019, 173, 145–154. [Google Scholar] [CrossRef]
- Razavi, A.C.; Sapin, A.; Monlezun, D.J.; McCormack, I.G.; Latoff, A.; Pedroza, K.; McCullough, C.; Sarris, L.; Schlag, E.; Dyer, A.; et al. Effect of Culinary Education Curriculum on Mediterranean Diet Adherence and Food Cost Savings in Families: A Randomised Controlled Trial. Public Health Nutr. 2021, 24, 2297–2303. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Food Variety Score < 7 | Food Variety Score ≥ 7 | p |
|---|---|---|---|
| n (%) | 871 (42.55%) | 1176 (57.45%) | <0.001 |
| Gender | <0.001 | ||
| Male | 505 (52.31) | 554 (47.69) | |
| Female | 366 (62.96) | 622 (37.04) | |
| Age | <0.01 | ||
| ≥60 and <75 | 300 (52.63) | 270 (47.37) | |
| ≥75 to <85 | 507 (57.74) | 371 (42.26) | |
| ≥85 | 369 (61.60) | 230 (38.40) | |
| Marital status | <0.001 | ||
| Married or partnered | 571 (52.19) | 532 (47.81) | |
| Unmarried or others | 605 (63.48) | 348 (36.52) | |
| Region of residence | <0.01 | ||
| Urban community | 446 (53.80) | 383 (46.20) | |
| Rural village | 730 (59.93) | 488 (40.07) | |
| Family income | <0.001 | ||
| Quintile 1 (lowest) | 358 (66.54) | 180 (33.46) | |
| Quintile 2 | 331 (57.77) | 242 (42.23) | |
| Quintile 3 | 236 (56.87) | 179 (42.13) | |
| Quintile 4 (highest) | 251 (48.18) | 270 (51.82) | |
| Living conditions | <0.001 | ||
| Alone | 294 (54.99) | 149 (45.01) | |
| Not alone | 882 (66.37) | 722 (33.63) | |
| BMI | <0.001 | ||
| Underweight | 178 (67.17) | 87 (32.83) | |
| Normal | 685 (58.55) | 485 (41.45) | |
| Overweight | 238 (50.42) | 234 (49.58) | |
| Obese | 75 (53.57) | 65 (46.43) | |
| Smoking status | 0.06 | ||
| Current | 222 (53.62) | 192 (46.38) | |
| Former | 132 (53.88) | 113 (46.12) | |
| Never | 822 (59.22) | 566 (40.78) | |
| Alcohol consumption status | <0.001 | ||
| Current | 222 (53.62) | 192 (46.38) | |
| Former | 132 (53.88) | 113 (46.12) | |
| Never | 822 (59.22) | 566 (40.78) | |
| Exercise | <0.001 | ||
| Yes | 314 (47.50) | 347 (52.50) | |
| No | 862 (62.19) | 524 (37.81) | |
| Vitamins intake | <0.001 | ||
| Often | 57 (32.20) | 120 (67.80) | |
| Not often | 1119 (59.84) | 751 (40.16) |
| Food Variety Score | Crude Model | Adjusted Model 1 | Adjusted Model 2 |
| <7 | 1 (reference) | 1 (reference) | 1 (reference) |
| ≥7 | 0.78 (0.59–1.02) | 0.80 (0.60–1.07) | 0.81 (0.61–1.08) |
| Food Variety Change | Crude Model | Adjusted Model 1 | Adjusted Model 2 |
| Maintained low variety | 1 (reference) | 1 (reference) | 1 (reference) |
| Variety gets declined | 0.88 (0.63–1.24) | 0.93 (0.66–1.33) | 0.93 (0.65–1.33) |
| Variety gets increased | 0.77 (0.52–1.15) | 0.84 (0.55–1.26) | 0.83 (0.55–1.26) |
| Maintained high variety | 0.58 (0.40–0.85) | 0.60 (0.40–0.89) | 0.59 (0.39–0.90) |
| Dietary Patterns | Crude Model | Adjusted Model 1 | Adjusted Model 2 |
|---|---|---|---|
| Milk–nut–mushroom or algae pattern | |||
| Q1 | 1 (reference) | 1 (reference) | 1 (reference) |
| Q2 | 0.98 (0.68–1.40) | 1.05 (0.72–1.52) | 1.04 (0.72–1.52) |
| Q3 | 0.75 (0.52–1.10) | 0.80 (0.54–1.19) | 0.80 (0.53–1.19) |
| Q4 | 0.92 (0.64–1.32) | 0.96 (0.66–1.42) | 0.96 (0.64–1.43) |
| Egg–bean–pickle–sugar pattern | |||
| Q1 | 1 (reference) | 1 (reference) | 1 (reference) |
| Q2 | 0.90 (0.63–1.29) | 0.87 (0.61–1.26) | 0.87 (0.60–1.25) |
| Q3 | 0.77 (0.54–1.11) | 0.79 (0.54–1.15) | 0.79 (0.54–1.15) |
| Q4 | 0.64 (0.44–0.96) | 0.61 (0.41–0.90) | 0.60 (0.41–0.90) |
| Fruit–vegetable–meat–fish pattern | |||
| Q1 | 1 (reference) | 1 (reference) | 1 (reference) |
| Q2 | 0.66 (0.46–0.94) | 0.70 (0.48–1.02) | 0.71 (0.49–1.03) |
| Q3 | 0.58 (0.40–0.84) | 0.58 (0.39–0.85) | 0.58 (0.39–0.85) |
| Q4 | 0.64 (0.45–0.92) | 0.62 (0.42–0.92) | 0.63 (0.43–0.93) |
| tea pattern | |||
| Q1 | 1 (reference) | 1 (reference) | 1 (reference) |
| Q2 | 0.83 (0.58–1.19) | 0.88 (0.60–1.27) | 0.88 (0.60–1.27) |
| Q3 | 0.77 (0.54–1.11) | 0.89 (0.61–1.30) | 0.90 (0.61–1.31) |
| Q4 | 0.72 (0.49–1.04) | 0.93 (0.62–1.37) | 0.93 (0.62–1.38) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Wang, Q.; Hao, W.; Zhu, D. Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018. Nutrients 2022, 14, 4279. https://doi.org/10.3390/nu14204279
Zhang J, Wang Q, Hao W, Zhu D. Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018. Nutrients. 2022; 14(20):4279. https://doi.org/10.3390/nu14204279
Chicago/Turabian StyleZhang, Jiajun, Qi Wang, Wenting Hao, and Dongshan Zhu. 2022. "Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018" Nutrients 14, no. 20: 4279. https://doi.org/10.3390/nu14204279
APA StyleZhang, J., Wang, Q., Hao, W., & Zhu, D. (2022). Long-Term Food Variety and Dietary Patterns Are Associated with Frailty among Chinese Older Adults: A Cohort Study Based on CLHLS from 2014 to 2018. Nutrients, 14(20), 4279. https://doi.org/10.3390/nu14204279





