Association between Milk Intake and All-Cause Mortality among Chinese Adults: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
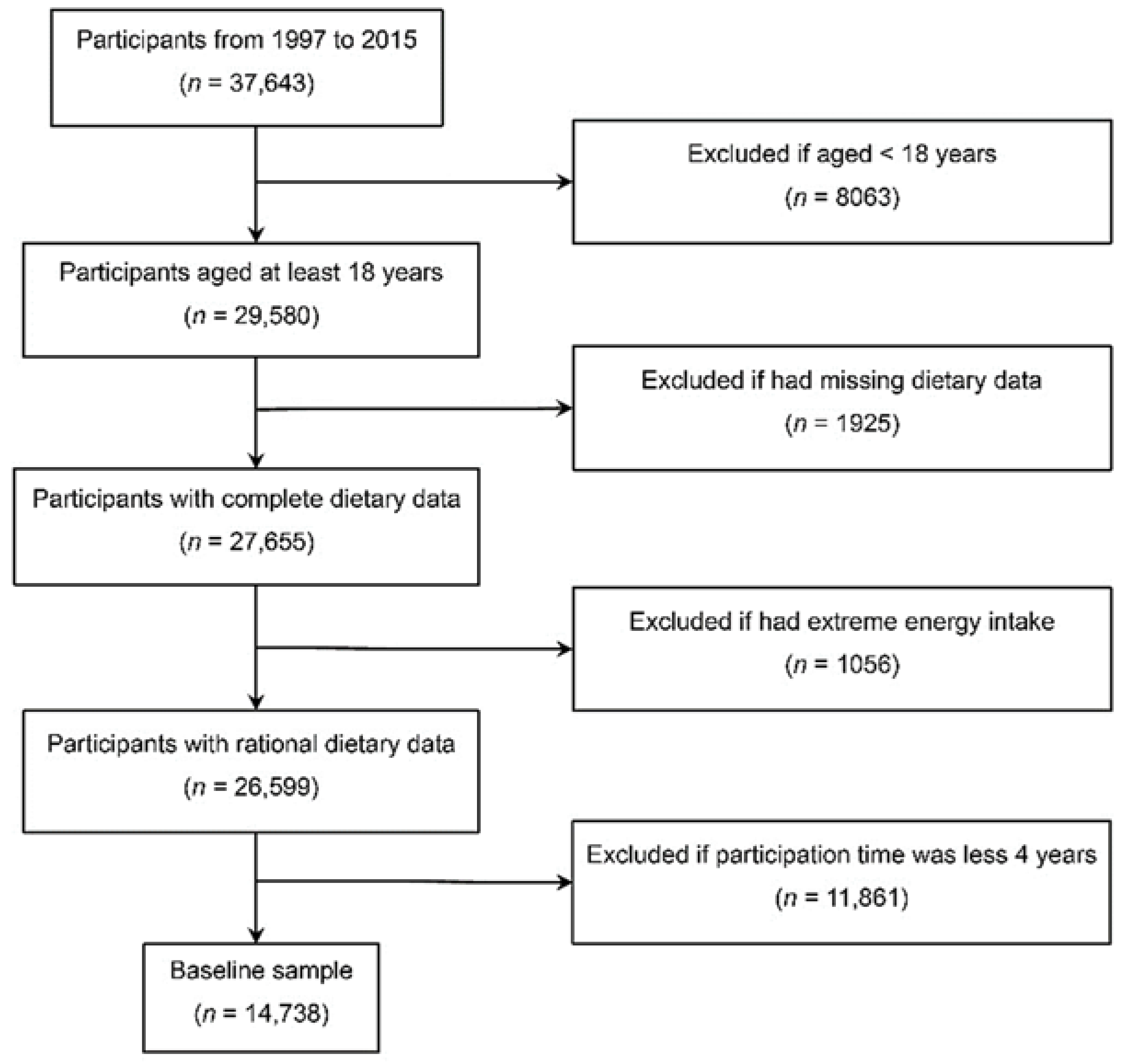
2.1. Study Population
2.2. Data Collection
2.3. Assessment of Outcome
2.4. Definition of Covariates
2.5. Statistical Analyses
3. Results
3.1. Sociodemographic Characteristics of Participants
3.2. Dietary Intake Characteristics of Participants
3.3. Association between Milk Intake and All-Cause Mortality
3.3.1. Overall Population
3.3.2. Stratified Analyses
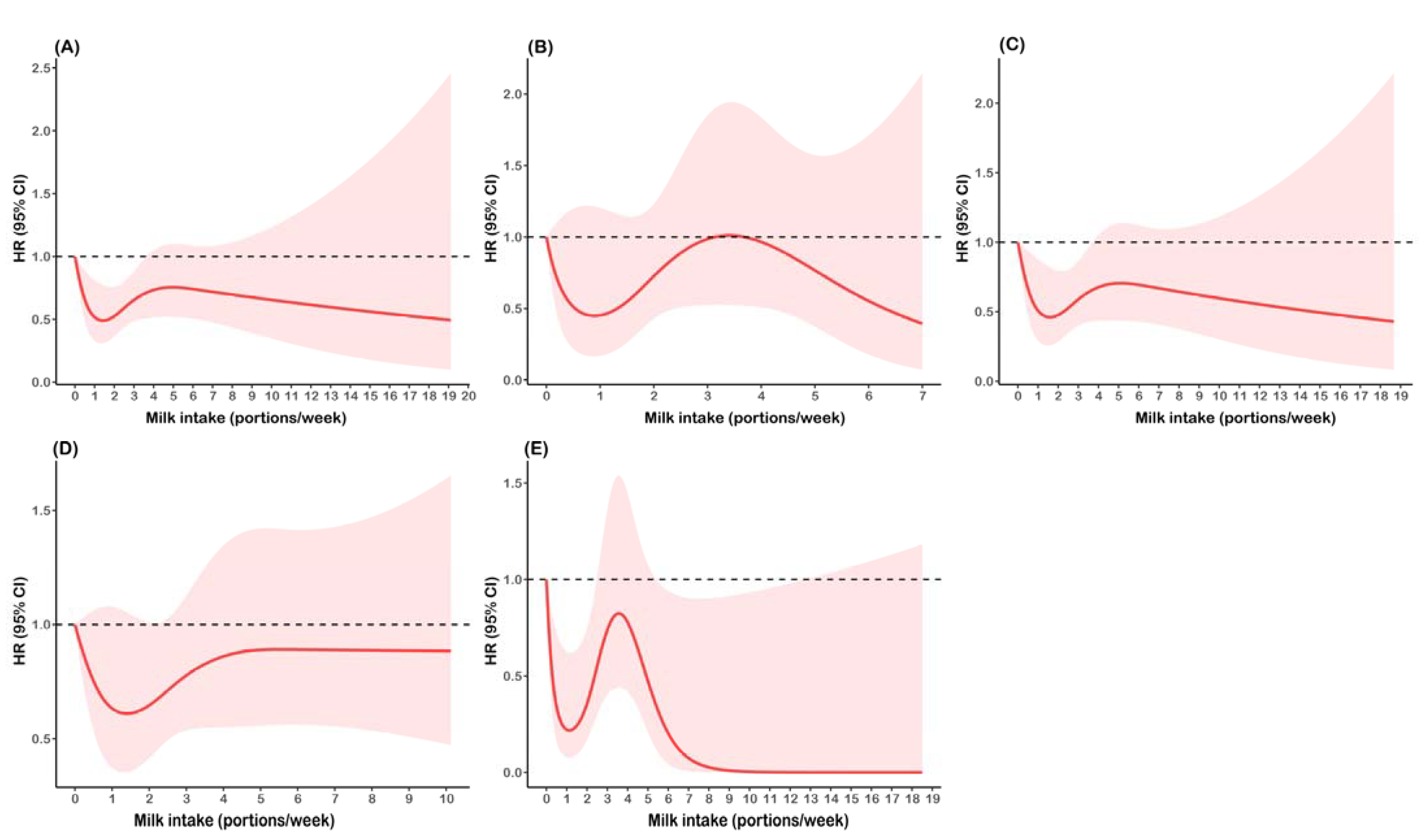
3.4. Nonlinear Relationship between Milk Intake and All-Cause Mortality
3.5. Sensitivity Analyses
4. Discussion
4.1. Insufficient Intake of Milk among Chinese Adults
4.2. Role of Milk in Health
4.3. Association between Milk and All-Cause Mortality for Different Dietary Qualities
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Drewnowski, A.; Victor, F., III. Nutrient Profiling of Foods: Creating a Nutrient-Rich Food Index. Nutr. Rev. 2008, 66, 23–39. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. Available online: https://www.dietaryguidelines.gov/ (accessed on 27 June 2021).
- Chinese Nutrition Society. Chinese Dietary Guideline 2016, 1st ed.; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- Austialian Government. Australian Dietary Guidelines. Available online: https://www.eatforhealth.gov.au/guidelines/australian-dietary-guidelines-1-5 (accessed on 27 June 2021).
- Talaei, M.; Pan, A.; Yuan, J.M.; Koh, W.P. Dairy Intake and Risk of Type 2 Diabetes. Clin. Nutr. 2018, 37, 712–718. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yatsuya, H.; Lin, Y.; Sasakabe, T.; Kawai, S.; Kikuchi, S.; Iso, H.; Tamakoshi, A. Milk Intake and Stroke Mortality in the Japan Collaborative Cohort Study-a Bayesian Survival Analysis. Nutrients 2020, 12, 2743. [Google Scholar] [CrossRef]
- Farvid, M.S.; Malekshah, A.F.; Pourshams, A.; Poustchi, H.; Sepanlou, S.G.; Sharafkhah, M.; Khoshnia, M.; Farvid, M.; Abnet, C.C.; Kamangar, F.; et al. Dairy Food Intake and All-Cause, Cardiovascular Disease, and Cancer Mortality: The Golestan Cohort Study. Am. J. Epidemiol. 2017, 185, 697–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Um, C.Y.; Judd, S.E.; Flanders, W.D.; Fedirko, V.; Bostick, R.M. Associations of Calcium and Dairy Products with All-Cause and Cause-Specific Mortality in the Reasons for Geographic and Racial Differences in Stroke (Regards) Prospective Cohort Study. Nutr. Cancer 2017, 69, 1185–1195. [Google Scholar] [CrossRef] [PubMed]
- Mullie, P.; Pizot, C.; Autier, P. Daily Milk Consumption and All-Cause Mortality, Coronary Heart Disease and Stroke: A Systematic Review and Meta-Analysis of Observational Cohort Studies. BMC Public Health 2016, 16, 1236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, B.H. Dairy and Cardiovascular Disease: A Review of Recent Observational Research. Curr. Nutr. Rep. 2014, 3, 130–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, W.; Chen, H.; Niu, Y.; Wu, H.; Xia, D.; Wu, Y. Dairy Products Intake and Cancer Mortality Risk: A Meta-Analysis of 11 Population-Based Cohort Studies. Nutr. J. 2016, 15, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Um, C.Y.; Prizment, A.; Hong, C.P.; Lazovich, D.; Bostick, R.M. Associations of Calcium and Dairy Product Intakes with All-Cause, All-Cancer, Colorectal Cancer and Chd Mortality among Older Women in the Iowa Women’s Health Study. Br. J. Nutr. 2019, 121, 1188–1200. [Google Scholar] [CrossRef]
- Goldbohm, R.A.; Chorus, A.M.; Garre, F.G.; Schouten, L.J.; van den Brandt, P.A. Dairy Consumption and 10-Y Total and Cardiovascular Mortality: A Prospective Cohort Study in the Netherlands. Am. J. Clin. Nutr. 2011, 93, 615–627. [Google Scholar] [CrossRef] [Green Version]
- Van Aerde, M.A.; Soedamah-Muthu, S.S.; Geleijnse, J.M.; Snijder, M.B.; Nijpels, G.; Stehouwer, C.D.; Dekker, J.M. Dairy Intake in Relation to Cardiovascular Disease Mortality and All-Cause Mortality: The Hoorn Study. Eur. J. Nutr. 2013, 52, 609–616. [Google Scholar] [CrossRef] [Green Version]
- Michaelsson, K.; Wolk, A.; Langenskiold, S.; Basu, S.; Lemming, E.W.; Melhus, H.; Byberg, L. Milk Intake and Risk of Mortality and Fractures in Women and Men: Cohort Studies. BMJ 2014, 349, g6015. [Google Scholar] [CrossRef] [Green Version]
- Willett, W.C.; Ludwig, D.S. Milk and Health. N. Engl. J. Med. 2020, 382, 644–654. [Google Scholar] [CrossRef]
- Dehghan, M.; Mente, A.; Rangarajan, S.; Sheridan, P.; Mohan, V.; Iqbal, R.; Gupta, R.; Lear, S.; Wentzel-Viljoen, E.; Avezum, A.; et al. Association of Dairy Intake with Cardiovascular Disease and Mortality in 21 Countries from Five Continents (Pure): A Prospective Cohort Study. Lancet 2018, 392, 2288–2297. [Google Scholar] [CrossRef]
- Wang, Y.; Jia, X.; Du, W.; Wang, Z.; Wang, H.; Zhang, B. Dairy Consumption Characteristics among Chinese Adult Residents from 1989 to 2011. Wei Sheng Yan Jiu J. Hyg. Res. 2017, 46, 409–433. [Google Scholar]
- He, Y.; Yang, X.; Xia, J.; Zhao, L.; Yang, Y. Consumption of Meat and Dairy Products in China: A Review. Proc. Nutr. Soc. 2016, 75, 385–391. [Google Scholar] [CrossRef] [Green Version]
- Chinese Nutrition Society. Chinese Dietary Reference Intakes, 1st ed.; Sciences Press: Beijing, China, 2013. [Google Scholar]
- Wang, X.J.; Jiang, C.Q.; Zhang, W.S.; Zhu, F.; Jin, Y.L.; Woo, J.; Cheng, K.K.; Lam, T.H.; Xu, L. Milk Consumption and Risk of Mortality from All-Cause, Cardiovascular Disease and Cancer in Older People. Clin. Nutr. 2020, 39, 3442–3451. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.Y.; Liu, F.C.; Yang, X.L.; Li, J.X.; Cao, J.; Lu, X.F.; Huang, J.F.; Li, Y.; Chen, J.C.; Zhao, L.C.; et al. Association of Cardiovascular Diseases with Milk Intake among General Chinese Adults. Chin. Med. J. 2020, 133, 1144–1154. [Google Scholar] [CrossRef]
- Na, X.; Zhu, Z.; Chen, Y.; He, H.; Zhou, G.; Zhou, J.; Zhang, T.; Zhuang, G.; Liu, A. Leisure-Time Physical Activity and Milk Intake Synergistically Reduce the Risk of Pathoglycemia: A Cross-Sectional Study in Adults in Beijing, China. Asia Pac. J. Clin. Nutr. 2020, 29, 183–191. [Google Scholar]
- University of North Carolina; Chinese Center for Disease Control and Prevention. China Health and Nutrition Survey. Available online: https://www.cpc.unc.edu/projects/china (accessed on 27 June 2021).
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey—Monitoring and Understanding Socio-Economic and Health Change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.X.; Wang, G.Y.; Pan, X.C. China Food Composition; Peking University Medical Press: Beijing, China, 2002; p. 329. [Google Scholar]
- Ershow, A.G.; Wong-Chen, K. Chinese Food Composition Tables an Annotated Translation of the 1981 Edition Published by the Institute of Nutrition and Food Hygiene, Chinese Academy of Preventive Medicine, Beijing. J. Food Compos. Anal. 1990, 3, 191–434. [Google Scholar] [CrossRef]
- Chen, C.; Lu, F.C. The Guidelines for Prevention and Control of Overweight and Obesity in Chinese Adults. Biomed. Environ. Sci. 2004, 17, 1–36. [Google Scholar] [PubMed]
- Kurth, T.; Walker, A.M.; Glynn, R.J.; Chan, K.; Gaziano, J.M.; Berger, K.; Robins, J.M. Results of Multivariable Logistic Regression, Propensity Matching, Propensity Adjustment, and Propensity-Based Weighting under Conditions of Nonuniform Effect. Am. J. Epidemiol. 2006, 163, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Haug, A.; Høstmark, A.T.; Harstad, O.M. Bovine Milk in Human Nutrition—A Review. Lipids Health Dis. 2007, 6, 25. [Google Scholar] [CrossRef] [Green Version]
- Fulgoni, V.L., III; Keast, D.R.; Auestad, N.; Quann, E.E. Nutrients from Dairy Foods Are Difficult to Replace in Diets of Americans: Food Pattern Modeling and an Analyses of the National Health and Nutrition Examination Survey 2003–2006. Nutr. Res. 2011, 31, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Dougkas, A.; Minihane, A.M.; Givens, D.I.; Reynolds, C.K.; Yaqoob, P. Differential Effects of Dairy Snacks on Appetite, but Not Overall Energy Intake. Br. J. Nutr. 2012, 108, 2274–2285. [Google Scholar] [CrossRef]
- Bendtsen, L.Q.; Blædel, T.; Holm, J.B.; Lorenzen, J.K.; Mark, A.B.; Kiilerich, P.; Kristiansen, K.; Astrup, A.; Larsen, L.H. High Intake of Dairy During Energy Restriction Does Not Affect Energy Balance or the Intestinal Microflora Compared with Low Dairy Intake in Overweight Individuals in a Randomized Controlled Trial. Appl. Physiol. Nutr. Metab. 2018, 43, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zemel, M.B.; Donnelly, J.E.; Smith, B.K.; Sullivan, D.K.; Richards, J.; Morgan-Hanusa, D.; Mayo, M.S.; Sun, X.; Cook-Wiens, G.; Bailey, B.W.; et al. Effects of Dairy Intake on Weight Maintenance. Nutr. Metab. 2008, 5, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polzonetti, V.; Pucciarelli, S.; Vincenzetti, S.; Polidori, P. Dietary Intake of Vitamin D from Dairy Products Reduces the Risk of Osteoporosis. Nutrients 2020, 12, 1743. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Jung, J.H.; Kim, M.S.; Lee, H.J. High Dairy Products Intake Reduces Osteoporosis Risk in Korean Postmenopausal Women: A 4 Year Follow-up Study. Nutr. Res. Pract. 2018, 12, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Eelderink, C.; Rietsema, S.; van Vliet, I.M.Y.; Loef, L.C.; Boer, T.; Koehorst, M.; Nolte, I.M.; Westerhuis, R.; Singh-Povel, C.M.; Geurts, J.M.W.; et al. The Effect of High Compared with Low Dairy Consumption on Glucose Metabolism, Insulin Sensitivity, and Metabolic Flexibility in Overweight Adults: A Randomized Crossover Trial. Am. J. Clin. Nutr. 2019, 109, 1555–1568. [Google Scholar] [CrossRef] [PubMed]
- Agriculture and Horticulture Development Board. Change in Uk Consumer Preferences Show Need for More Cheese. Available online: https://ahdb.org.uk/news/change-in-UK-consumer-preferences-for-more-cheese (accessed on 2 July 2021).
- Ding, M.; Li, J.; Qi, L.; Ellervik, C.; Zhang, X.; Manson, J.E.; Stampfer, M.; Chavarro, J.E.; Rexrode, K.M.; Kraft, P.; et al. Associations of Dairy Intake with Risk of Mortality in Women and Men: Three Prospective Cohort Studies. BMJ 2019, 367, l6204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Downer, M.K.; Batista, J.L.; Mucci, L.A.; Stampfer, M.J.; Epstein, M.M.; Håkansson, N.; Wolk, A.; Johansson, J.E.; Andrén, O.; Fall, K.; et al. Dairy Intake in Relation to Prostate Cancer Survival. Int. J. Cancer 2017, 140, 2060–2069. [Google Scholar] [CrossRef]
- Dong, J.Y.; Zhang, L.; He, K.; Qin, L.Q. Dairy Consumption and Risk of Breast Cancer: A Meta-Analysis of Prospective Cohort Studies. Breast Cancer Res. Treat. 2011, 127, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Rosenblatt, D.A.N.; Chan, D.S.; Vieira, A.R.; Vieira, R.; Greenwood, D.C.; Vatten, L.J.; Norat, T. Dairy Products, Calcium, and Prostate Cancer Risk: A Systematic Review and Meta-Analysis of Cohort Studies. Am. J. Clin. Nutr. 2015, 101, 87–117. [Google Scholar] [CrossRef] [Green Version]
- Bermejo, L.M.; López-Plaza, B.; Santurino, C.; Cavero-Redondo, I.; Gómez-Candela, C. Milk and Dairy Product Consumption and Bladder Cancer Risk: A Systematic Review and Meta-Analysis of Observational Studies. Adv. Nutr. 2019, 10, S224–S238. [Google Scholar] [CrossRef]
- Harrison, S.; Lennon, R.; Holly, J.; Higgins, J.; Gardner, M.; Perks, C.; Gaunt, T.; Tan, V.; Borwick, C.; Emmet, P.; et al. Does Milk Intake Promote Prostate Cancer Initiation or Progression Via Effects on Insulin-Like Growth Factors (Igfs)? A Systematic Review and Meta-Analysis. Cancer Causes Control. 2017, 28, 497–528. [Google Scholar] [CrossRef] [Green Version]
- Nakanishi, A.; Homma, E.; Osaki, T.; Sho, R.; Souri, M.; Sato, H.; Watanabe, M.; Ishizawa, K.; Ueno, Y.; Kayama, T.; et al. Association between Milk and Yogurt Intake and Mortality: A Community-Based Cohort Study (Yamagata Study). BMC Nutr. 2021, 7, 1–7. [Google Scholar] [CrossRef]
- Wang, C.; Yatsuya, H.; Tamakoshi, K.; Iso, H.; Tamakoshi, A. Milk Drinking and Mortality: Findings from the Japan Collaborative Cohort Study. J. Epidemiol. 2015, 25, 66–73. [Google Scholar] [CrossRef] [Green Version]
- Park, S.-J.; Park, J.; Song, H.J.; Lee, C.-H.; Lee, H.-J. Association between Dairy Product Intake and Hypertriglyceridemia in Korean Adults. Nutr. Res. Pract. 2020, 14, 152. [Google Scholar] [CrossRef]
- Shin, W.K.; Lee, H.W.; Shin, A.; Lee, J.K.; Kang, D. Milk Consumption Decreases Risk for Breast Cancer in Korean Women under 50 Years of Age: Results from the Health Examinees Study. Nutrients 2019, 12, 32. [Google Scholar] [CrossRef] [Green Version]
- Bian, S.; Hu, J.; Zhang, K.; Wang, Y.; Yu, M.; Ma, J. Dairy Product Consumption and Risk of Hip Fracture: A Systematic Review and Meta-Analysis. BMC Public Health 2018, 18, 165. [Google Scholar] [CrossRef] [Green Version]
- Saito, A.; Okada, E.; Tarui, I.; Matsumoto, M.; Takimoto, H. The Association between Milk and Dairy Products Consumption and Nutrient Intake Adequacy among Japanese Adults: Analysis of the 2016 National Health and Nutrition Survey. Nutrients 2019, 11, 2361. [Google Scholar] [CrossRef] [Green Version]
- Tsugane, S. Why Has Japan Become the World’s Most Long-Lived Country: Insights from a Food and Nutrition Perspective. Eur. J. Clin. Nutr. 2020, 75, 921–928. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, A.; Wu, W.; Ren, Z.; Yang, C.; Wang, P.; Zhang, Y. Beneficial Effect of Dietary Diversity on the Risk of Disability in Activities of Daily Living in Adults: A Prospective Cohort Study. Nutrients 2020, 12, 3263. [Google Scholar] [CrossRef]
- Yin, Z.; Fei, Z.; Qiu, C.; Brasher, M.S.; Kraus, V.B.; Zhao, W.; Shi, X.; Zeng, Y. Dietary Diversity and Cognitive Function among Elderly People: A Population-Based Study. J. Nutr. Health Aging 2017, 21, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liang, D.; Zhao, A. Dietary Diversity and the Risk of Fracture in Adults: A Prospective Study. Nutrients 2020, 12, 3655. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, A.; Wu, W.; Yang, C.; Ren, Z.; Wang, M.; Wang, P.; Zhang, Y. Dietary Diversity Is Associated with Memory Status in Chinese Adults: A Prospective Study. Front. Aging Neurosci. 2020, 21, 580760. [Google Scholar] [CrossRef] [PubMed]
- Leosdottir, M.; Nilsson, P.; Nilsson, J.A.; Månsson, H.; Berglund, G. The Association between Total Energy Intake and Early Mortality: Data from the Malmö Diet and Cancer Study. J. Intern. Med. 2004, 256, 499–509. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef] [PubMed]
- Todd, J.E. Changes in Consumption of Food Away from Home and Intakes of Energy and Other Nutrients among Us Working-Age Adults, 2005–2014. Public Health Nutr. 2017, 20, 3238–3246. [Google Scholar] [CrossRef] [Green Version]
- Yun, S.; Kim, H.J.; Oh, K. Trends in Energy Intake among Korean Adults, 1998–2015: Results from the Korea National Health and Nutrition Examination Survey. Nutr. Res. Pract. 2017, 11, 147. [Google Scholar] [CrossRef] [Green Version]
| No Consumption | 0.1–2 Portions/Week | >2 Portions/Week | p | ||
|---|---|---|---|---|---|
| (N = 11,975) | (N = 1341) | (N = 1422) | |||
| Age, M (P25, P75) | 42.0 (32.0, 54.0) | 44.0 (34.0, 57.0) | 50.0 (36.0, 61.0) | <0.001 | |
| Sex, n (%) | 0.123 | ||||
| Male | 5604 (46.8) | 614 (45.8) | 626 (44.0) | ||
| Female | 6371 (53.2) | 727 (54.2) | 796 (56.0) | ||
| Education, n (%) | <0.001 | ||||
| Junior high school or below | 6404 (53.5) | 466 (34.8) | 516 (36.3) | ||
| Senior high school or vocational school | 1574 (13.1) | 313 (23.3) | 305 (21.4) | ||
| University or above | 722 (6.03) | 259 (19.3) | 270 (19.0) | ||
| Unknown | 3275 (27.3) | 303 (22.6) | 331 (23.3) | ||
| Place of residence, n (%) | <0.001 | ||||
| Eastern China | 4340 (36.2) | 791 (59.0) | 950 (66.8) | ||
| Central China | 4487 (37.5) | 342 (25.5) | 289 (20.3) | ||
| Western China | 3148 (26.3) | 208 (15.5) | 183 (12.9) | ||
| Individual annual income, yuan, n (%) | <0.001 | ||||
| <30,000 | 6974 (58.2) | 732 (54.6) | 752 (52.9) | ||
| 30,000–59,999 | 3535 (29.5) | 435 (32.4) | 496 (34.9) | ||
| ≥60,000 | 1466 (12.2) | 174 (13.0) | 174 (12.2) | ||
| Smoke status, n (%) | <0.001 | ||||
| Never | 5347 (44.7) | 738 (55.0) | 770 (54.1) | ||
| Former smoker | 333 (2.78) | 45 (3.36) | 60 (4.22) | ||
| Current smoker | 2070 (17.3) | 205 (15.3) | 206 (14.5) | ||
| Unknown | 4225 (35.3) | 353 (26.3) | 386 (27.1) | ||
| Alcohol intake, times/week, n (%) | <0.001 | ||||
| Never | 5162 (43.1) | 655 (48.8) | 696 (48.9) | ||
| <1 | 888 (7.42) | 140 (10.4) | 123 (8.65) | ||
| ≥1 | 1665 (13.9) | 189 (14.1) | 211 (14.8) | ||
| Unknown | 4260 (35.6) | 357 (26.6) | 392 (27.6) | ||
| Physical activity, MET-hour/week, M (P25, P75) | 125 (57.0, 199) | 109 (56.0, 167) | 96.1 (49.0, 158) | <0.001 | |
| BMI, kg/m2, n (%) | <0.001 | ||||
| <18.5 | 354 (2.96) | 34 (2.54) | 45 (3.16) | ||
| 18.5–23.9 | 8222 (68.7) | 860 (64.1) | 879 (61.8) | ||
| 24.0–27.9 | 2482 (20.7) | 323 (24.1) | 376 (26.4) | ||
| ≥28.0 | 917 (7.66) | 124 (9.25) | 122 (8.58) | ||
| Chronic disease history, n (%) | <0.001 | ||||
| No | 10,741 (89.7) | 1154 (86.1) | 1153 (81.1) | ||
| Yes | 1234 (10.3) | 187 (13.9) | 269 (18.9) | ||
| No Consumption | 0.1–2 Portions/Week | >2 Portions/Week | p | ||
|---|---|---|---|---|---|
| (N = 11,975) | (N = 1341) | (N = 1422) | |||
| Dietary diversity score, M (P25, P75) | 3.00 (2.61, 3.67) | 4.00 (3.33, 4.67) | 4.38 (3.75, 5.17) | <0.001 | |
| Energy intake, kcal/day, M (P25, P75) | 2057.07 (1723.43, 2400.67) | 1983.93 (1663.95, 2297.24) | 1996.05 (1678.69, 2293.63) | <0.001 | |
| Vegetables intake, g/day, M (P25, P75) | 208 (144, 282) | 186 (127, 250) | 192 (133, 261) | <0.001 | |
| Fruits intake, g/day, M (P25, P75) | 0.00 (0.00, 100) | 83.3 (0.00, 150) | 100 (33.3, 168) | <0.001 | |
| Red meat intake, g/day, M (P25, P75) | 1.33 (0.00, 20.0) | 9.33 (0.00, 33.3) | 7.32 (0.00, 33.3) | <0.001 | |
| Milk intake at baseline, potions/week, n (%) | <0.001 | ||||
| 0 | 11,975 (100) | 307 (22.9) | 179 (12.6) | ||
| 0.1–2 | 0 (0) | 933 (69.6) | 243 (17.1) | ||
| ≥3 | 0 (0) | 101 (7.5) | 1000 (70.3) | ||
| No Consumption | 0.1–2 Portions/Week | >2 Portions/Week | |
|---|---|---|---|
| Overall population | |||
| Incidence (no. of deaths/1000 person-years) | 4.30 | 2.53 | 3.35 |
| Unadjusted Model | 1.00 (Reference) | 0.63 (0.44, 0.90) * | 0.81 (0.60, 1.10) |
| Model 1 | 1.00 (Reference) | 0.57 (0.39, 0.81) ** | 0.73 (0.54, 1.00) * |
| Model 2 | 1.00 (Reference) | 0.55 (0.38, 0.79) ** | 0.74 (0.38, 1.43) |
| IPTW Model | 1.00 (Reference) | 0.63 (0.44, 0.90) * | 0.81 (0.60, 1.10) |
| Low dietary diversity | |||
| Incidence (no. of deaths/1000 person-years) | 4.99 | 4.05 | 4.73 |
| Unadjusted Model | 1.00 (Reference) | 0.78 (0.46, 1.33) | 0.92 (0.49, 1.73) |
| Model 1 | 1.00 (Reference) | 0.76 (0.44, 1.29) | 0.67 (0.36, 1.25) |
| Model 2 | 1.00 (Reference) | 0.76 (0.45, 1.31) | 0.66 (0.35, 1.24) |
| IPTW Model | 1.00 (Reference) | 0.78 (0.46, 1.33) | 0.92 (0.49, 1.73) |
| High dietary diversity | |||
| Incidence (no. of deaths/1000 person-years) | 2.99 | 1.95 | 3.10 |
| Unadjusted Model | 1.00 (Reference) | 0.65 (0.40, 1.07) | 0.97 (0.67, 1.40) |
| Model 1 | 1.00 (Reference) | 0.50 (0.30, 0.82) ** | 0.69 (0.47, 1.02) |
| Model 2 | 1.00 (Reference) | 0.51 (0.31, 0.84) ** | 0.71 (0.48, 1.05) |
| IPTW Model | 1.00 (Reference) | 0.65 (0.40, 1.06) | 0.96 (0.66, 1.39) |
| Low energy intake | |||
| Incidence (no. of deaths/1000 person-years) | 5.79 | 4.12 | 4.57 |
| Unadjusted Model | 1.00 (Reference) | 0.78 (0.52, 1.17) | 0.80 (0.56, 1.16) |
| Model 1 | 1.00 (Reference) | 0.72 (0.47, 1.10) | 0.83 (0.57, 1.21) |
| Model 2 | 1.00 (Reference) | 0.75 (0.48, 1.14) | 0.80 (0.53, 1.19) |
| IPTW Model | 1.00 (Reference) | 0.78 (0.52, 1.17) | 0.80 (0.56, 1.17) |
| High energy intake | |||
| Incidence (no. of deaths/1000 person-years) | 3.20 | 1.06 | 2.16 |
| Unadjusted Model | 1.00 (Reference) | 0.35 (0.16, 0.74) ** | 0.72 (0.43, 1.21) |
| Model 1 | 1.00 (Reference) | 0.32 (0.15, 0.68) ** | 0.61 (0.36, 1.05) |
| Model 2 | 1.00 (Reference) | 0.31 (0.14, 0.67) ** | 0.60 (0.35, 1.04) |
| IPTW Model | 1.00 (Reference) | 0.35 (0.16, 0.74) ** | 0.72 (0.43, 1.21) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Na, X.; Lan, H.; Wang, Y.; Tan, Y.; Zhang, J.; Zhao, A. Association between Milk Intake and All-Cause Mortality among Chinese Adults: A Prospective Study. Nutrients 2022, 14, 292. https://doi.org/10.3390/nu14020292
Na X, Lan H, Wang Y, Tan Y, Zhang J, Zhao A. Association between Milk Intake and All-Cause Mortality among Chinese Adults: A Prospective Study. Nutrients. 2022; 14(2):292. https://doi.org/10.3390/nu14020292
Chicago/Turabian StyleNa, Xiaona, Hanglian Lan, Yu Wang, Yuefeng Tan, Jian Zhang, and Ai Zhao. 2022. "Association between Milk Intake and All-Cause Mortality among Chinese Adults: A Prospective Study" Nutrients 14, no. 2: 292. https://doi.org/10.3390/nu14020292
APA StyleNa, X., Lan, H., Wang, Y., Tan, Y., Zhang, J., & Zhao, A. (2022). Association between Milk Intake and All-Cause Mortality among Chinese Adults: A Prospective Study. Nutrients, 14(2), 292. https://doi.org/10.3390/nu14020292






