Dietary Sodium and Potassium Intake: Data from the Mexican National Health and Nutrition Survey 2016
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Estimating Total Na and K Intake
2.3. Food Classification Based on NOVA Processing Level
2.4. Sociodemographic Characteristics and Socio-Economic Status
2.5. Anthropometry
2.6. Adult Sample
2.7. Ethical Considerations
2.8. Statistical Analysis
3. Results
3.1. Food Groups That Contribute to Sodium and Potassium Intake
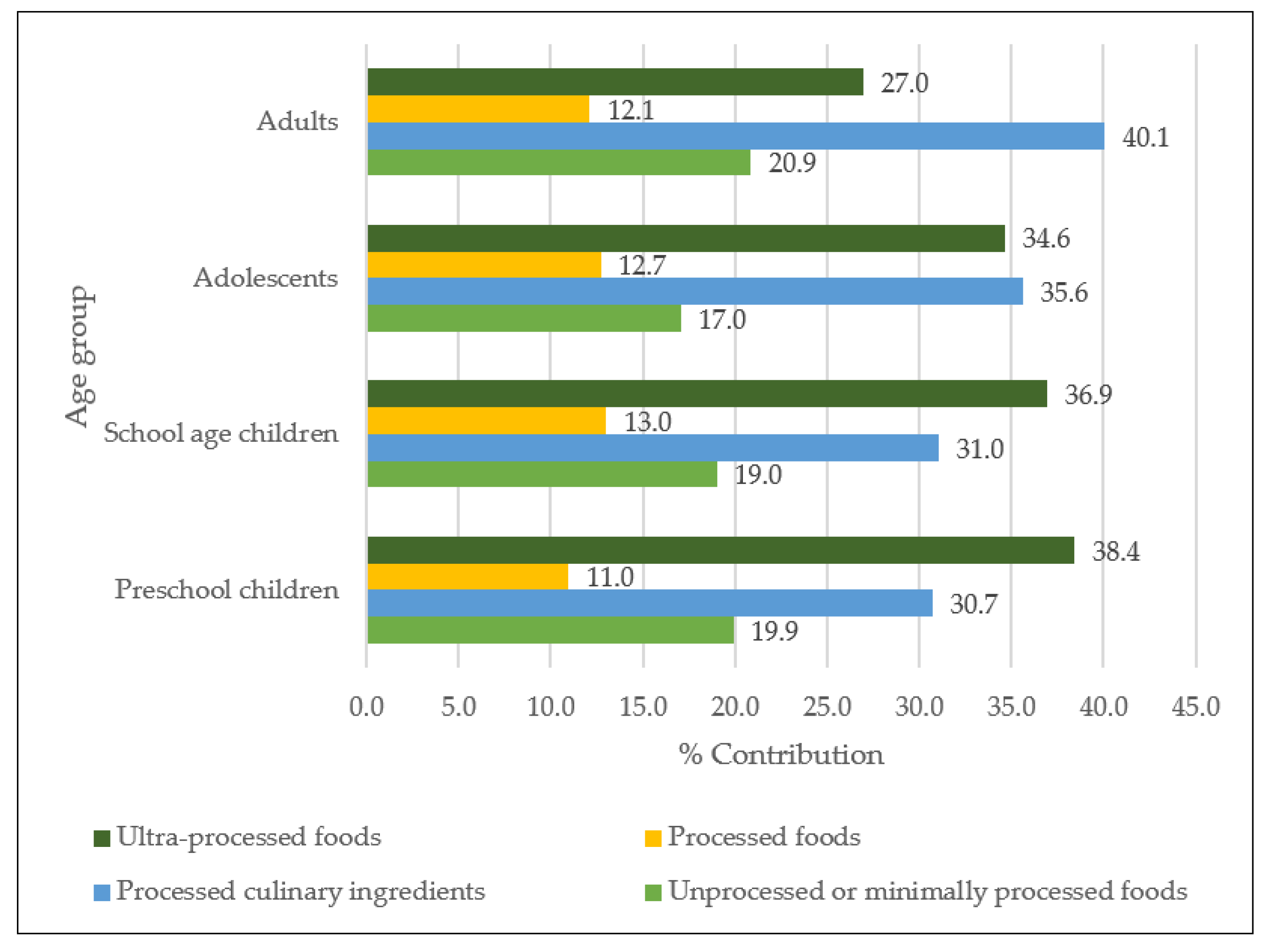
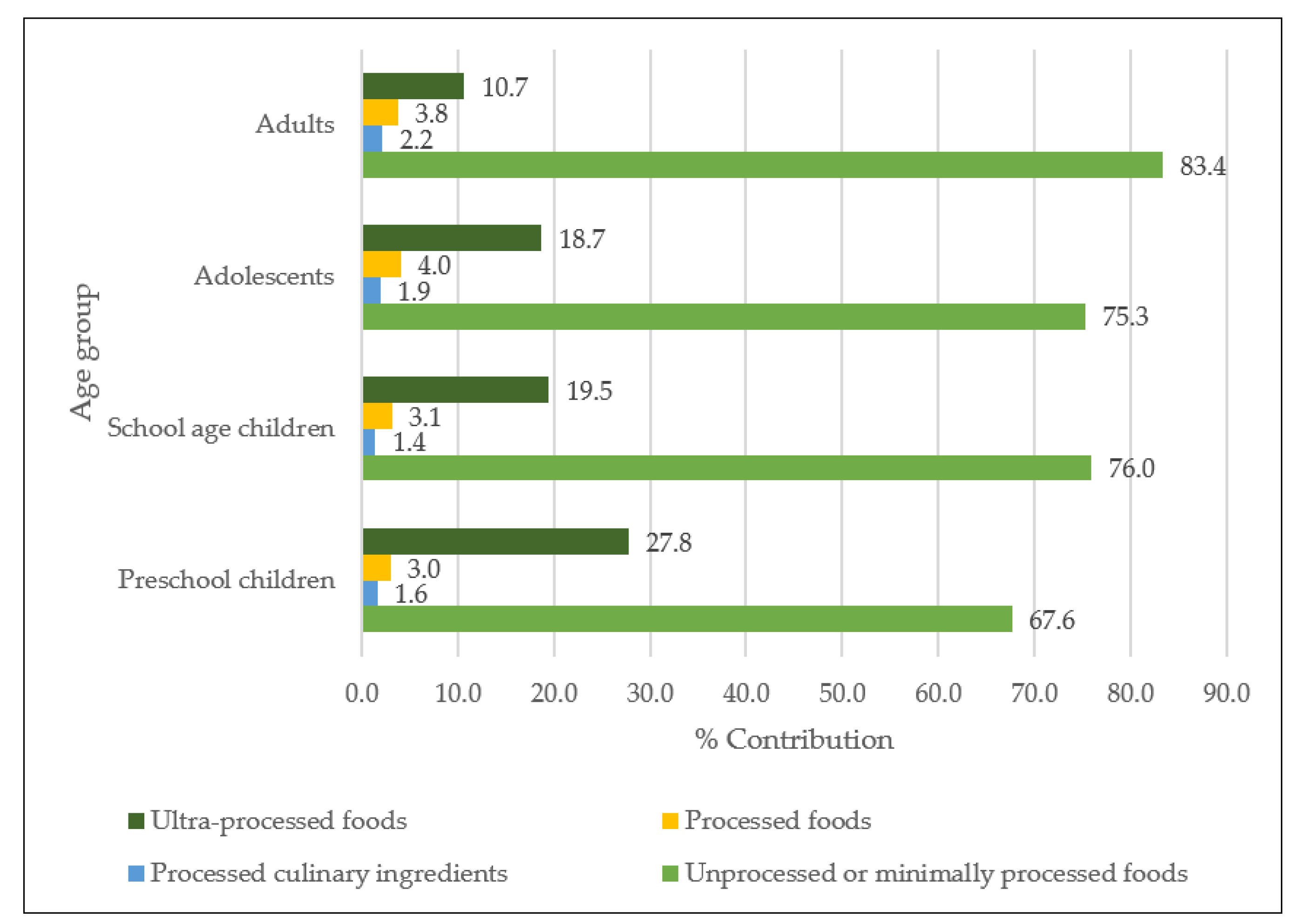
3.2. Contribution of Na and K According to the NOVA Classification
3.3. Na and K Intake: Health Risk
3.4. Na and K Intake: Nutrition Status and Clinical Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- IOM (Institute of Medicine). Dietary Reference Intakes for Water, Potassium, Sodium, Chloride and Sulfate; The National Academies Press: Washington, DC, USA, 2005; ISBN 0309091586. [Google Scholar]
- Pirahanchi, Y.; Jessu, R.; Aeddula, N.R. Physiology, Sodium Potassium Pump; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Grillo, A.; Salvi, L.; Coruzzi, P.; Salvi, P.; Parati, G. Sodium intake and hypertension. Nutrients 2019, 11, 1970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jr, R.C.M.; Schmidlin, O.; Frassetto, L.A.; Sebastian, A.; Morris, R.C.; Schmidlin, O.; Frassetto, L.A.; Sebastian, A. Relationship and Interaction between Sodium and Potassium Relationship and Interaction between Sodium and. J. Am. Coll. Nutr. 2013, 25 (Suppl. 3), 37–41. [Google Scholar] [CrossRef]
- Newberry, S.J.; Chung, M.; Anderson, C.A.M.; Chen, C.; Fu, Z.; Tang, A.; Zhao, N.; Booth, M.; Marks, J.; Hollands, S.; et al. Sodium and Potassium Intake: Effects on Chronic Disease Outcomes and Risks [Internet]; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2018. [Google Scholar]
- National Academies of Sciences Engineering and Medicine. Dietary Reference Intakes for Sodium and Potassium; The National AcademiesThe National Academies Press: Washington, DC, USA, 2019; ISBN 978-0-309-48834-1. [Google Scholar]
- OMS (Organización Mundial de la Salud). Ingesta de Sodio en Adultos y Niños; Organización Mundial de la Salud: Geneva, Switzerland, 2013. [Google Scholar]
- Mozaffarian, D.; Fahimi, S.; Singh, G.M.; Micha, R.; Khatibzadeh, S.; Engell, R.E.; Lim, S.; Danaei, G.; Ezzati, M.; Powles, J. Global Sodium Consumption and Death from Cardiovascular Causes. N. Engl. J. Med. 2014, 371, 624–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vega-Vega, O.; Fonseca-Correa, J.I.; Mendoza-De la Garza, A.; Rincón-Pedrero, R.; Espinosa-Cuevas, A.; Baeza-Arias, Y.; Dary, O.; Herrero-Bervera, B.; Nieves-Anaya, I.; Correa-Rotter, R. Contemporary dietary intake: Too much sodium, not enough potassium, yet sufficient iodine: The SALMEX cohort results. Nutrients 2018, 10, 816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madriz, K.; Ramos, E.; Blanco-Metzler, A.; Saavedra, L.; Nilson, E.; Tiscornia, V. Policy Brief: El Desafío de Reducir el Consumo de sal/Sodio en la Dieta de la Población Latinoamericana; Tres Ríos, Costa Rica, 2020. [Google Scholar]
- Marrón-Ponce, J.A.; Tolentino-Mayo, L.; Hernández-F, M.; Batis, C. Trends in ultra-processed food purchases from 1984 to 2016 in Mexican households. Nutrients 2019, 11, 45. [Google Scholar] [CrossRef] [Green Version]
- Arcand, J.; Blanco-Metzler, A.; Aguilar, K.B.; L’abbe, M.R.; Legetic, B. Sodium levels in packaged foods sold in 14 latin american and Caribbean countries: A food label analysis. Nutrients 2018, 11, 369. [Google Scholar] [CrossRef] [Green Version]
- OMS (Organización Mundial de la Salud). Ingesta de Potasio en Adultos y Niños; Organización Mundial de la Salud: Geneva, Switzerland, 2013; pp. 1–7. [Google Scholar]
- He, F.J.; MacGregor, G.A. Beneficial effects of potassium on human health. Physiol. Plant 2008, 133, 725–735. [Google Scholar] [CrossRef]
- Vallejo, M.; Colín-Ramírez, E.; Mancía, S.R.; Rosado, R.C.; Madero, M.; Vázquez, O.I.; Vargas-Barrón, J. Assessment of Sodium and Potassium Intake by 24 h Urinary Excretion in a Healthy Mexican Cohort. Arch. Med. Res. 2017, 48, 195–202. [Google Scholar] [CrossRef]
- Organización Panamerica de la Salud. SHAKE Menos sal, más Salud. Guía Técnica Para Reducir el Consumo de sal; Organización Panamerica de la Salud: Washington, DC, USA, 2018. [Google Scholar]
- Cook, N.R.; Obarzanek, E.; Cutler, J.A.; Buring, J.E.; Rexrode, K.M.; Kumanyika, S.K.; Appel, L.J.; Whelton, P.K. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: The Trials of Hypertension Prevention follow-up study. Arch. Intern. Med. 2009, 169, 32–40. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; O’Leary, N.; Yin, L.; Liu, X.; Swaminathan, S.; Khatib, R.; Rosengren, A.; et al. Joint association of urinary sodium and potassium excretion with cardiovascular events and mortality: Prospective cohort study. BMJ 2019, 364, l772. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.F.; Mony, P.; Devanath, A.; et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef] [Green Version]
- Colin-Ramirez, E.; Espinosa-Cuevas, Á.; Miranda-Alatriste, P.V.; Tovar-Villegas, V.I.; Arcand, J.; Correa-Rotter, R. Food sources of sodium intake in an adult mexican population: A sub-analysis of the SALMEX study. Nutrients 2017, 9, 810. [Google Scholar] [CrossRef] [Green Version]
- Romero-Martínez, M.; Shamah-Levy, T.; Cuevas-Nasu, L.; Méndez Gómez-Humarán, I.; Gaona-Pineda, E.; Gómez-Acosta, L.; Rivera-Dommarco, J. Diseño metodológico de la Encuesta Nacional de Salud y Nutrición de Medio Camino 2016. Salud Publica Mex 2017, 59, 299–305. [Google Scholar] [CrossRef] [Green Version]
- Blanton, C.A.; Moshfegh, A.J.; Baer, D.J.; Kretsch, M.J. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J. Nutr. 2006, 136, 2594–2599. [Google Scholar] [CrossRef]
- Ramírez-Silva, I.; Rodríguez-Ramírez, S.; Barragán-Vázquez, S.; Castellanos-Gutiérrez, A.; Reyes-García, A.; Martínez-Piña, A.; Pedroza-Tobías, A. Prevalence of inadequate intake of vitamins and minerals in the Mexican population correcting by nutrient retention factors, Ensanut 2016. Salud Publica Mex. 2020, 62, 521–531. [Google Scholar] [CrossRef]
- Ramírez Silva, I.; Barragán-Vázquez, S.; Rodríguez-Ramírez, S.; Rivera-Dommarco, J.A.; Mejía-Rodríguez, F.; Barquera-Cervera, S.; Tolentino, L.; Al, E. Base de Alimentos de México (BAM): Compilación de la Composición de los Alimentos Frecuentemente Consumidos en el País; Versión 18.1.1; Morelos, México, 2020. [Google Scholar]
- Organización Mundial de la Salud. Alimentos y Bebidas Ultraprocesados en América Latina: Tendencias, Efecto Sobre la Obesidad e Implicaciones para las Políticas Públicas; World Health Organization: Geneva, Switzerland, 2015; ISBN 9789275718643. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Levy, R.; Moubarac, J.-C.; Jaime, P.; Martins, A.P.; Canella, D.; Louzada, M.; Parra, D. NOVA. The Star Shines Bright (Food Classification. Public Health). World Nutr. 2016, 7, 28–38. [Google Scholar]
- Marrón-Ponce, J.A.; Flores, M.; Cediel, G.; Monteiro, C.A.; Batis, C. Associations between Consumption of Ultra-Processed Foods and Intake of Nutrients Related to Chronic Non-Communicable Diseases in Mexico. J. Acad. Nutr. Diet. 2019, 119, 1852–1865. [Google Scholar] [CrossRef] [PubMed]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Chap 6. Construction of Body Mass Index- for-Age Standards; World Health Organization: Washington, DC, USA, 2000. [Google Scholar]
- World Health Organization (WHO). Physical Status: The Use and Interpretation of Anthropometry; World Health Organization: Geneva, Switerland, 1993. [Google Scholar]
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charleston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwartz, J.E.; Townsend, R.R.; et al. Measurement of Blood Pressure in Humans: A Scientific Statement from the American Heart Association. Hypertension 2019, 3, e35–e66. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alcaraz, C.; Shamah-Levy, T.; Romero-Martínez, M.; Sepúlveda-Amor, J.; Aguilar-Salinas, C.A.; Rivera-Dommarco, J.; Kershenobich-Stalnikowitz, D.; Hernández-Ávila, M.; Barquera, S. Submuestra para el análisis de enfermedades crónicas con biomarcadores, Encuesta Nacional de Salud y Nutrición 2016. Salud Publica Mex. 2020, 62, 504–510. [Google Scholar] [CrossRef]
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020, 43, 14–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. Centers for Disease Control and Prevention Cholesterol. Available online: https://www.cdc.gov/cholesterol/cholesterol_screening.htm (accessed on 26 December 2021).
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Carrillo-Larco, R.M.; Bernabe-Ortiz, A. Sodium and Salt Consumption in Latin America and the Caribbean: A Systematic-Review and Meta-Analysis of Population-Based Studies and Surveys. Nutrients 2020, 12, 556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powles, J.; Fahimi, S.; Micha, R.; Khatibzadeh, S.; Shi, P.; Ezzati, M.; Engell, R.E.; Lim, S.S.; Danaei, G.; Mozaffarian, D. Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013, 3, e003733. [Google Scholar] [CrossRef] [Green Version]
- Kumssa, D.B.; Joy, E.J.M.; Broadley, M.R. Global Trends (1961–2017) in Human Dietary Potassium Supplies. Nutrients 2021, 13, 1369. [Google Scholar] [CrossRef] [PubMed]
- Pereira, T.S.S.; Cade, N.V.; Mill, J.G.; Sichieri, R.; Molina, M.D.C.B. Use of the Method of Triads in the Validation of Sodium and Potassium Intake in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). PLoS ONE 2016, 11, e0169085. [Google Scholar] [CrossRef]
- Popkin, B.M.; Lu, B.; Zhai, F. Understanding the nutrition transition: Measuring rapid dietary changes in transitional countries. Public Health Nutr. 2002, 5, 947–953. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M. The Nutrition Transition: An Overview of World Patterns of Change. Nutr. Rev. 2004, 62, S140–S143. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [Green Version]
- García-chávez, C.G.; Monterrubio-flores, E.; Ramírez-silva, I.; Aburto, T.C.; Pedraza, L.S.; Rivera-dommarco, J. Contribución de los alimentos a la ingesta total de energía en la dieta de los mexicanos mayores de cinco años. Salud Publica Mex. 2020, 62, 166–180. [Google Scholar] [CrossRef]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Andrews, K.G.; Engell, R.E.; Mozaffarian, D. Global, regional and national consumption of major food groups in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open 2015, 5, e008705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Insitute for Health Metrics and Evaluation (IHME). Global Burden Disease Compare Data Visualization; IHME: Seattle, WA, USA, 2019. [Google Scholar]
- Moubarac, J.-C.; Batal, M.; Louzada, M.L.; Martinez Steele, E.; Monteiro, C.A. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017, 108, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Machado, P.P.; Steele, E.M.; Levy, R.B.; Sui, Z.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ Open 2019, 9, e029544. [Google Scholar] [CrossRef] [Green Version]
- Schnabel, L.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Srour, B.; Hercberg, S.; Buscail, C.; Julia, C. Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-aged Adults in France. JAMA Intern. Med. 2019, 179, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Cuadrado-Soto, E.; Peral-Suarez, Á.; Aparicio, A.; Perea, J.M.; Ortega, R.M.; López-Sobaler, A.M. Sources of Dietary Sodium in Food and Beverages Consumed by Spanish Schoolchildren between 7 and 11 Years Old by the Degree of Processing and the Nutritional Profile. Nutrients 2018, 10, 1880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rauber, F.; da Costa Louzada, M.L.; Steele, E.M.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-Processed Food Consumption and Chronic Non-Communicable Diseases-Related Dietary Nutrient Profile in the UK (2008–2014). Nutrients 2018, 10, 587. [Google Scholar] [CrossRef] [Green Version]
- Koyama, T.; Yoshiike, N. Association between Parent and Child Dietary Sodium and Potassium Intakes: Aomori Prefectural Health and Nutrition Survey, 2016. Nutrients 2019, 11, 1414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merkiel, S.; Chalcarz, W. Preschool diets in children from Piła, Poland, require urgent intervention as implied by high risk of nutrient inadequacies. J. Health. Popul. Nutr. 2016, 35, 11. [Google Scholar] [CrossRef] [Green Version]
- O’Halloran, S.A.; Grimes, C.A.; Lacy, K.E.; Campbell, K.J.; Nowson, C.A. Dietary intake and sources of potassium and the relationship to dietary sodium in a sample of Australian pre-school children. Nutrients 2016, 8, 496. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez-Ramírez, S.; Muñoz-Espinosa, A.; Rivera, J.A.; González-Castell, D.; González de Cosío, T. Mexican Children under 2 Years of Age Consume Food Groups High in Energy and Low in Micronutrients. J. Nutr. 2016, 146, 1916S–1923S. [Google Scholar] [CrossRef] [Green Version]
- Farapti, F.; Sulistyowati, M.; Artanti, K.D.; Setyaningtyas, S.W.; Sumarmi, S.; Mulyana, B. Highlighting of Urinary Sodium and Potassium among Indonesian Schoolchildren Aged 9–12 Years: The Contribution of School Food. J. Nutr. Metab. 2019, 2019, 1028672. [Google Scholar] [CrossRef]
- López-Sobaler, A.M.; Aparicio, A.; González-Rodríguez, L.G.; Cuadrado-Soto, E.; Rubio, J.; Marcos, V.; Sanchidrián, R.; Santos, S.; Pérez-Farinós, N.; Dal Re, M.Á.; et al. Adequacy of Usual Vitamin and Mineral Intake in Spanish Children and Adolescents: ENALIA Study. Nutrients 2017, 9, 131. [Google Scholar] [CrossRef] [Green Version]
- Saeid, N.; Elmzibri, M.; Hamrani, A.; Latifa, Q.; Belghiti, H.; El Berri, H.; Benjeddou, K.; Bouziani, A.; Benkirane, H.; Taboz, Y.; et al. Assessment of Sodium and Potassium Intakes in Children Aged 6 to 18 Years by 24 h Urinary Excretion in City of Rabat, Morocco. J. Nutr. Metab. 2018, 2018, 8687192. [Google Scholar] [CrossRef] [PubMed]
- Grimes, C.A.; Riddell, L.J.; Campbell, K.J.; Beckford, K.; Baxter, J.R.; He, F.J.; Nowson, C.A. Dietary intake and sources of sodium and potassium among Australian schoolchildren: Results from the cross-sectional Salt and Other Nutrients in Children (SONIC) study. BMJ Open 2017, 7, e016639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonçalves, C.; Abreu, S.; Padrão, P.; Pinho, O.; Graça, P.; Breda, J.; Santos, R.; Moreira, P. Sodium and potassium urinary excretion and dietary intake: A cross-sectional analysis in adolescents. Food Nutr. Res. 2016, 60, 29442. [Google Scholar] [CrossRef] [Green Version]
- Yu, A.Y.L.; López-Olmedo, N.; Popkin, B.M. Analysis of dietary trends in Chinese adolescents from 1991 to 2011. Asia Pac. J. Clin. Nutr. 2018, 27, 1106–1119. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, C.E.; Nicklas, T.A.; Fulgoni, V.L. 3rd Food Sources of Energy and Nutrients of Public Health Concern and Nutrients to Limit with a Focus on Milk and other Dairy Foods in Children 2 to 18 Years of Age: National Health and Nutrition Examination Survey, 2011–2014. Nutrients 2018, 10, 1050. [Google Scholar] [CrossRef] [Green Version]
- Zárate-Ortiz, A.G.; Melse-Boonstra, A.; Rodríguez-Ramírez, S.; Hernández-Cordero, S.; Feskens, E.J.M. Dietary Patterns and the Double Burden of Malnutrition in Mexican Adolescents: Results from ENSANUT-2006. Nutrients 2019, 11, 2753. [Google Scholar] [CrossRef] [Green Version]
- Huang, L.; Wang, H.; Wang, Z.; Wang, Y.; Zhang, B.; Ding, G. Associations of dietary sodium, potassium, and sodium to potassium ratio with blood pressure— regional disparities in China. Nutrients 2020, 12, 366. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.; McFann, K.; Chonchol, M.; Kendrick, J. Dietary sodium and potassium intake is not associated with elevated blood pressure in US adults with no prior history of hypertension. J. Clin. Hypertens. 2014, 16, 418–423. [Google Scholar] [CrossRef] [Green Version]
- Bolton, K.A.; Trieu, K.; Woodward, M.; Nowson, C.; Webster, J.; Dunford, E.K.; Bolam, B.; Grimes, C. Dietary Intake and Sources of Potassium in a Cross-Sectional Study of Australian Adults. Nutrients 2019, 11, 2996. [Google Scholar] [CrossRef] [Green Version]
- Fang, K.; He, Y.; Fang, Y.; Lian, Y. Dietary Sodium Intake and Food Sources Among Chinese Adults: Data from the CNNHS 2010-2012. Nutrients 2020, 12, 453. [Google Scholar] [CrossRef] [Green Version]
- Graudal, N.A.; Hubeck-Graudal, T.; Jurgens, G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst. Rev. 2017, 2017, CD004022. [Google Scholar] [CrossRef]
- Thuesen, B.H.; Toft, U.; Buhelt, L.P.; Linneberg, A.; Friedrich, N.; Nauck, M.; Wallaschofski, H.; Jørgensen, T. Estimated daily salt intake in relation to blood pressure and blood lipids: The role of obesity. Eur. J. Prev. Cardiol. 2015, 22, 1567–1574. [Google Scholar] [CrossRef]
- McLean, R.M. Measuring population sodium intake: A review of methods. Nutrients 2014, 6, 4651–4662. [Google Scholar] [CrossRef]
- Campos-Nonato, I.; Hernández-Barrera, L.; Oviedo-Solís, C.; Ramírez-Villalobos, D.; Hernández, B.; Barquera, S. Epidemiología de la hipertensión arterial en adultos mexicanos: Diagnóstico, control y tendencias. Ensanut 2020. Salud Publica Mex 2021, 63, 692–704. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization; IHME: University of Washington, Seattle, WA, USA, 2019; Available online: https://vizhub.healthdata.org/gbd-compare/ (accessed on 21 December 2021).
- Vega-Solano, J.; Blanco-Metzler, A.; Madriz-Morales, K.; Fernandes-Nilson, E.A.; Labonté, M.E. Impact of salt intake reduction on CVD mortality in Costa Rica: A scenario modelling study. PLoS ONE 2021, 16, e0245388. [Google Scholar] [CrossRef]
- Nilson, E.A.F.; Metlzer, A.B.; Labonté, M.-E.; Jaime, P.C. Modelling the effect of compliance with WHO salt recommendations on cardiovascular disease mortality and costs in Brazil. PLoS ONE 2020, 15, e0235514. [Google Scholar] [CrossRef]
- Shamah-Levy, T.; Cuevas-Nasu, L.; Gaona-Pineda, E.; Gómez-Acosta, L.M.; Morales-Rúan, M.D.C.; Hernández-Ávila, M.; Rivera-Dommarco, J.Á. Sobrepeso y obesidad en niños y adolescentes en México, actualización de la Encuesta Nacional de Salud y Nutrición de Medio Camino 2016. Salud Publica Mex. 2018, 60, 244–253. [Google Scholar] [CrossRef] [Green Version]
- Barquera, S.; Hernández-Barrera, L.; Trejo-Valdivia, B. Obesidad en México, prevalencia y tendencias en adultos. Ensanut 2018-19. Salud Publica Mex. 2020, 62, 682–692. [Google Scholar] [CrossRef]
| Preschool Children | School-Age Children | Adolescents | Adults | |||||
|---|---|---|---|---|---|---|---|---|
| n = 528 | N = 8,584,831 | n = 1095 | N = 16,144,480 | n = 1240 | N = 23,988,992 | n = 1356 | N = 87,921,191 | |
| Mean (SE) | 95%CI | Mean (SE) | 95%CI | Mean (SE) | 95%CI | Mean (SE) | 95%CI | |
| Total (n = 4219; N = 136,639,494) | ||||||||
| Sodium intake (mg/day) | 1512.2 ± 68.6 | (1377.1, 1647.2) | 2843.8 ± 236.1 | (2379.0, 3308.6) | 3743.2 ± 304.2 | (3144.4, 4341.9) | 3132.3 ± 171.9 | (2794.0, 3470.7) |
| Potassium intake (mg/day) | 1615.7 ± 68.6 | (1480.6, 1750.7) | 2255.7 ± 136.5 | (1986.9, 2524.5) | 2966.6 ± 180.3 | (2611.7, 3321.5) | 3400.6 ± 273.5 | (2862.1, 3939.0) |
| Na-K ratio | 1.1 ± 0.1 | (0.9, 1.2) | 1.4 ± 0.1 | (1.1, 1.7) | 1.3 ± 0.0 | (1.3, 1.4) | 1.1 ± 0.0 | (1.0, 1.2) |
| Sex | ||||||||
| Women (n = 2312; N = 72,673,426) | ||||||||
| Sodium intake (mg/day) | 1494.8 ± 95.6 | (1306.7, 1682.9) | 2817.2 ± 425.6 | (1979.5, 3655.0) | 3286.6 ± 240.2 | (2813.8, 3759.5) | 2927.9 ± 217.2 | (2500.3, 3355.5) |
| Potassium intake (mg/day) | 1594.4 ± 93.0 | (1411.3, 1777.6) | 2052.2 ± 77.6 | (1899.4, 2205.1) | 2560.6 ± 138.5 | (2288.0, 2833.1) | 3250.5 ± 427.4 | (2409.1, 4091.9) |
| Na-K ratio | 1.0 ± 0.1 | (0.9, 1.1) | 1.6 ± 0.3 | (1.0, 2.2) | 1.4 ± 0.1 | (1.2, 1.5) | 1.1 ± 0.1 | (1.0, 1.2) |
| Men (n = 1907; N = 63,966,069) | ||||||||
| Sodium intake (mg/day) | 1528.6 ± 109.7 | (1312.5, 1744.6) | 2867.2 ± 253.4 | (2368.3, 3366.1) | 4236.6 ± 567.5 | (3119.5, 5353.7) | 3383.7 ± 257.2 | (2877.3, 3890.1) |
| Potassium intake (mg/day) | 1635.8 ± 96.6 | (1445.6, 1826.0) | 2434.6 ± 236.4 | (1969.2, 2900.0) | 3405.5 ± 329.3 | (2757.1, 4053.9) | 3585.0 ± 325.7 | (2943.7, 4226.3) |
| Na-K ratio | 1.1 ± 0.1 | (0.9, 1.4) | 1.3 ± 0.1 | (1.2, 1.4) | 1.3 ± 0.1 | (1.2, 1.5) | 1.1 ± 0.1 | (1.0, 1.2) |
| Area of residence | ||||||||
| Rural (n = 2227; N = 37,106,754) | ||||||||
| Sodium intake (mg/day) | 1439.1 ± 107.6 | (1225.8, 1652.3) | 2515.5 ± 243.5 | (2032.9, 2998.1) | 3498.7 ± 202.9 | (3096.6, 3900.8) | 3133.7 ± 375.8 | (2389.0, 3878.5) |
| Potassium intake (mg/day) | 1552.4 ± 100.4 | (1353.5, 1751.3) | 2193.2 ± 125.1 | (1945.2, 2441.1) | 2817.7 ± 135.3 | (2549.5, 3085.9) | 3626.9 ± 452.4 | (2730.3, 4523.5) |
| Na/-K ratio | 1.0 ± 0.1 | (0.9, 1.1) | 1.3 ± 0.1 | (1.1, 1.5) | 1.3 ± 0.1 | (1.2, 1.4) | 1.0 ± 0.1 | (0.9, 1.2) |
| Urban (n = 1992; N = 99,532,740) | ||||||||
| Sodium intake (mg/day) | 1538.7 ± 84.6 | (1371.7, 1705.7) | 2978.9 ± 317.6 | (2352.0, 3605.9) | 3824.4 ± 398.5 | (3037.9, 4610.9) | 3131.8 ± 189.5 | (2757.7, 3505.9) |
| Potassium intake (mg/day) | 1638.7 ± 85.9 | (1469.0, 1808.3) | 2281.4 ± 185.6 | (1915.1, 2647.7) | 3016.1 ± 233.3 | (2555.6, 3476.6) | 3314.9 ± 337.7 | (2648.4, 3981.5) |
| Na-K ratio | 1.1 ± 0.1 | (0.9, 1.3) | 1.5 ± 0.2 | (1.1, 1.9) | 1.4 ± 0.1 | (1.2, 1.5) | 1.1 ± 0.1 | (1.0, 1.2) |
| Socioeconomic tertile | ||||||||
| Low (n = 1464; N = 31,441,350) | ||||||||
| Sodium intake (mg/day) | 1388.4 ± 112.4 | (1166.7, 1610.2) | 2368.8 ± 201.1 | (1972.1, 2765.5) | 2896.1 ± 144.7 | (2610.7, 3181.6) | 2854.5 ± 278.6 | (2304.9, 3404.2) |
| Potassium intake (mg/day) | 1483.7 ± 101.0 | (1284.4, 1683.0) | 2163.3 ± 250.4 | (1669.3, 2657.3) | 2701.7 ± 134.7 | (2436.1, 2967.4) | 3283.7 ± 261.1 | (2768.6, 3798.8) |
| Na-K ratio | 1.0 ± 0.1 | (0.9, 1.2) | 1.3 ± 0.1 | (1.1, 1.4) | 1.2 ± 0.0 | (1.1, 1.3) | 1.0 ± 0.1 | (0.8, 1.1) |
| Medium (n = 1516; N = 40,785,812) | ||||||||
| Sodium intake (mg/day) | 1448.3 ± 108.6 | (1234.3, 1662.2) | 2958.1 ± 574.0 | (1827.6, 4088.7) | 4324.4 ± 772.5 | (2802.8, 5846.0) | 3264.8 ± 379.6 | (2517.0, 4012.6) |
| Potassium intake (mg/day) | 1637.2 ± 118.2 | (1404.3, 1870.1) | 1982.8 ± 116.5 | (1753.3, 2212.4) | 3423.6 ± 445.3 | (2546.4, 4300.8) | 3450.6 ± 486.4 | (2492.6, 4408.7) |
| Na-K ratio | 1.1 ± 0.2 | (0.8, 1.4) | 1.7 ± 0.4 | (0.9, 2.5) | 1.3 ± 0.1 | (1.1, 1.5) | 1.2 ± 0.1 | (1.0, 1.3) |
| High (n = 1239; N = 64,412,333) | ||||||||
| Sodium intake (mg/day) | 1684.5 ± 126.3 | (1435.7, 1933.3) | 3053.3 ± 313.5 | (2435.7, 3670.9) | 3707.6 ± 271.0 | (3173.6, 4241.5) | 3186.0 ± 216.4 | (2759.6, 3612.4) |
| Potassium intake (mg/day) | 1692.7 ± 123.8 | (1448.7, 1936.6) | 2546.4 ± 264.9 | (2024.6, 3068.3) | 2745.9 ± 132.0 | (2485.8, 3005.9) | 3426.1 ± 463.0 | (2513.8, 4338.4) |
| Na-K ratio | 1.1 ± 0.1 | (1.0, 1.3) | 1.3 ± 0.1 | (1.1, 1.4) | 1.5 ± 0.1 | (1.3, 1.6) | 1.1 ± 0.1 | (1.0, 1.3) |
| Body Mass Index a | ||||||||
| Normal (n = 2277; N = 49,562,419) | ||||||||
| Sodium intake (mg/day) | 1477.9 ± 70.7 | (1338.6, 1617.1) | 2533.5 ± 327.7 | (1888.3, 3178.7) | 2894.7 ± 121.6 | (2655.2, 3134.1) | 2898.6 ± 234.6 | (2436.6, 3360.5) |
| Potassium intake (mg/day) | 1576.3 ± 73.3 | (1431.9, 1720.6) | 1878.3 ± 77.0 | (1726.8, 2029.9) | 2380.0 ± 93.7 | (2195.5, 2564.5) | 3072.9 ± 285.5 | (2510.8, 3635.0) |
| Na-K ratio | 1.1 ± 0.1 | (0.9, 1.2) | 1.5 ± 0.2 | (1.1, 1.9) | 1.4 ± 0.1 | (1.2, 1.5) | 1.1 ± 0.1 | (0.9, 1.3) |
| Overweight (n = 949; N = 35,937,427) | ||||||||
| Sodium intake (mg/day) | 1097.8 ± 128.3 | (845.2, 1350.4) | 2376.3 ± 139.2 | (2102.2, 2650.4) | 2856.8 ± 138.7 | (2583.6, 3129.9) | 3110.9 ± 318.0 | (2484.5, 3737.3) |
| Potassium intake (mg/day) | 1064.5 ± 153.1 | (762.9, 1366.1) | 2103.3 ± 106.4 | (1893.7, 2312.9) | 2188.1 ± 108.7 | (1973.9, 2402.2) | 3163.4 ± 400.8 | (2374.1, 3952.7) |
| Na-K ratio | 1.1 ± 0.1 | (0.8, 1.3) | 1.2 ± 0.1 | (1.1, 1.4) | 1.4 ± 0.1 | (1.3, 1.5) | 1.1 ± 0.1 | (1.0, 1.3) |
| Obesity (n = 840 N = 42,639,888) | ||||||||
| Sodium intake (mg/day) | 2194.8 ± 254.5 | (1693.5, 2696.2) | 2720.2 ± 224.5 | (2277.9, 3162.5) | 3359.6 ± 375.0 | (2620.7, 4098.4) | 3287.1 ± 257.1 | (2780.5, 3793.6) |
| Potassium intake (mg/day) | 2102.1 ± 131.4 | (1843.1, 2361.0) | 2095.6 ± 168.8 | (1763.1, 2428.1) | 2653.8 ± 252.6 | (2156.2, 3151.5) | 3786.6 ± 511.3 | (2779.3, 4793.9) |
| Na-K ratio | 1.1 ± 0.2 | (0.8, 1.5) | 1.5 ± 0.1 | (1.2, 1.7) | 1.3 ± 0.2 | (1.0, 1.6) | 1.0 ± 0.1 | (0.9, 1.2) |
| Preschool Children | School-Age Children | Adolescents | Adults | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sodium | ||||||||||||
| Ranking | Food Groups | mg/day | % Contribution | Food Groups | mg/day | % Contribution | Food Groups | mg/day | % Contribution | Food Groups | mg/day | % Contribution |
| 1 | Salt | 399.3 ± 41.3 | 26.8 ± 1.5 | Salt | 1016.9 ± 216.2 | 28.1 ± 1.2 | Salt | 1186.2 ± 133.7 | 32.2 ± 2.3 | Salt | 1153.5 ± 104.7 | 36.5 ± 1.5 |
| 2 | Cereals | 253.6 ± 38.7 | 13.4 ± 1.6 | Cereals | 458.1 ± 43.3 | 16.0 ± 1.2 | Cereals | 641.7 ± 117.0 | 13.6 ± 1.4 | Cereals | 448.5 ± 60.5 | 12.5 ± 1.1 |
| 3 | Dairy | 196.8 ± 12.3 | 16.1 ± 1.3 | Dairy | 228.8 ± 20.0 | 10.2 ± 0.6 | Dairy | 287.1 ± 44.3 | 8.4 ± 1.0 | Red meat | 197.3 ± 40.6 | 5.9 ± 0.9 |
| 4 | Processed meats | 148.1 ± 28.1 | 7.6 ± 1.2 | Processed meats | 237.1 ± 34.7 | 7.9 ± 0.8 | Processed meats | 268.7 ± 43.5 | 6.6 ± 0.9 | Dairy | 184.0 ± 16.9 | 6.7 ± 0.5 |
| 5 | Seasonings | 76.6 ± 20.1 | 4.4 ± 1.0 | Salty snacks | 116.9 ± 19.3 | 4.1 ± 0.4 | Salty snacks | 172.3 ± 34.4 | 4.0 ± 0.6 | Processed meats | 178.6 ± 31.6 | 4.5 ± 0.6 |
| 6 | Eggs | 42.7 ± 3.7 | 3.3 ± 0.3 | Red meat | 105.4 ± 17.0 | 3.6 ± 0.5 | Red meat | 159.0 ± 31.8 | 4.7 ± 1.2 | Seasonings | 125.0 ± 44.2 | 3.5 ± 1.0 |
| 7 | Salty snacks | 45.5 ± 15.4 | 2.3 ± 0.6 | Seasonings | 104.1 ± 30.2 | 2.7 ± 0.5 | Seasonings | 89.02 ± 19.1 | 2.5 ± 0.4 | Corn tortilla | 95.5 ± 8.6 | 4.4 ± 0.4 |
| 8 | Red meat | 27.8 ± 8.4 | 1.7 ± 0.4 | Corn tortilla | 52.2 ± 4.8 | 2.9 ± 0.2 | Corn tortilla | 87.6 ± 9.4 | 3.5 ± 0.3 | Eggs | 68.0 ± 8.9 | 2.9 ± 0.4 |
| 9 | Cereal-based sweets | 26.1 ± 6.1 | 1.8 ± 0.4 | Eggs | 51.6 ± 4.2 | 2.9 ± 0.3 | Sweet bakery bread | 80.3 ± 14.6 | 3.2 ± 0.6 | Sweet bakery bread | 63.4 ± 8.4 | 2.9 ± 0.4 |
| 10 | Non-cereal-based sweets | 26.5 ± 4.6 | 1.8 ± 0.2 | R-to-E Cereals | 51.1 ± 11.0 | 2.7 ± 0.4 | Eggs | 77.7 ± 9.1 | 2.7 ± 0.3 | Cereals based sweets | 60.3 ± 18.1 | 1.9 ± 0.6 |
| Potassium | ||||||||||||
| Ranking | Food groups | mg/day | % Contribution | Food groups | mg/day | % Contribution | Food groups | mg/day | % Contribution | Food groups | mg/day | % Contribution |
| 1 | Dairy | 396.7 ± 32.3 | 23.7 ± 1.7 | Vegetables | 350.3 ± 42.5 | 13.5 ± 0.9 | Fruits | 414.5 ± 67.7 | 11.7 ± 1.2 | Vegetables | 701.6 ± 124.8 | 17.7 ± 1.2 |
| 2 | Fruits | 260.7 ± 28.5 | 14.7 ± 1.2 | Dairy | 324.2 ± 29.1 | 15.6 ± 0.9 | Vegetables | 385.7 ± 46.7 | 13.2 ± 1.1 | Fruits | 467.0 ± 74.2 | 12.3 ± 0.8 |
| 3 | Vegetables | 168.7 ± 19.1 | 9.8 ± 0.8 | Fruits | 278.5 ± 22.3 | 12.1 ± 0.8 | Corn tortilla | 363.3 ± 38.9 | 13.8 ± 0.9 | Corn tortilla | 401.4 ± 35.7 | 13.9 ± 1.0 |
| 4 | Yogurt and milk-based drinks | 101.4 ± 14.5 | 5.9 ± 0.8 | Corn tortilla | 215.9 ± 19.9 | 10.8 ± 0.6 | Dairy | 360.4 ± 48.4 | 11.5 ± 0.9 | Legumes | 302.6 ± 38.1 | 9.3 ± 0.9 |
| 5 | Corn tortilla | 89.3 ± 9.1 | 6.4 ± 0.6 | Legumes | 149.8 ± 18.0 | 6.7 ± 0.5 | Legumes | 273.6 40.6 | 8.2 ± 0.8 | Dairy | 233.2 ± 26.6 | 7.9 ± 0.6 |
| 6 | Legumes | 81.4 ± 10.9 | 5.3 ± 0.6 | Root vegetables | 134.2 ± 34.1 | 4.2 ± 0.6 | Red meat | 161.4 ± 20.8 | 5.7 ± 0.4 | Root vegetables | 198.6 ± 47.8 | 4.5 ± 0.6 |
| 7 | SSBs carbonated | 75.6 ± 11.5 | 4.8 ± 0.8 | Red meat | 101.6 ± 11.7 | 4.8 ± 0.6 | Cereals | 100.2 ± 11.3 | 4.0 ± 0.4 | Red meat | 172.0 ± 24.3 | 5.9 ± 0.5 |
| 8 | Root vegetables | 59.4 ± 13.7 | 3.0 ± 0.5 | Cereals | 88.2 ± 6.7 | 4.5 ± 0.2 | Salty snacks | 98.2 ± 19.0 | 3.1 ± 0.5 | Cereals | 138.9 ± 27.7 | 4.2 ± 0.4 |
| 9 | Cereals | 55.8 ± 7.3 | 4.3 ± 0.5 | Yogurt and milk-based drinks | 82.1 ± 14.9 | 3.0 ± 0.4 | Poultry | 95.4 ± 23.7 | 3.4 ± 0.7 | Coffee and tea | 134.0 ± 36.9 | 3.5 ± 0.4 |
| 10 | Poultry | 45.2 ± 6.2 | 3.0 ± 0.4 | Poultry | 79.7 ± 11.4 | 3.3 ± 0.3 | Root vegetables | 88.7 ± 16.01 | 2.9 ± 0.4 | Poultry | 120.8 ± 21.1 | 4.2 ± 0.5 |
| Preschool Children | School-Age Children | Adolescents | Adults | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High Na | Insufficient K | Na-K | High Na | Insufficient K | Na-K | High Na | Insufficient K | Na-K | High Na | Insufficient K | Na-K | |
| Total (n = 4219; N = 136,639,494) | ||||||||||||
| Age | 73.6 (66.9, 79.4) | 73.3 (66.2, 79.4) | 41.5 (34.6, 48.8) | 82.1 (78.1, 85.6) | 67.1 (61.5, 72.3) | 61.1 (56.3, 65.8) | 81.6 (76.3, 85.9) | 58.0 (49.1, 66.3) | 62.5 (52.6, 71.5) | 64.1 (57.1, 70.5) | 65.6 (56.7, 73.5) | 45.7 (38.6, 53.0) |
| Sex | ||||||||||||
| Women | 74.8 (67.0, 81.2) | 71.9 (61.6, 80.2) | 44.8 (35.3, 54.7) | 80.9 (75.4, 85.4) | 66.8 (59.8, 73.2) | 59.5 (53.3, 65.5) | 79.4 (70.5, 86.2) | 62.1 (49.5, 73.3) | 60.5 (44.2, 74.7) | 60.9 (51.0, 70.0) | 69.7 (55.0, 81.3) | 45.1 (35.0, 55.6) |
| Men | 72.5 (61.9, 81.1) | 74.7 (64.5, 82.8) | 38.4 (28.6, 49.2) | 83.2 (77.0, 88.0) | 67.4 (59.0, 74.9) | 62.6 (54.8, 69.7) | 84.0 (76.8, 89.3) | 53.5 (42.0, 64.7) | 64.8 (52.6, 75.3) | 68.0 (58.6, 76.1) | 60.4 (49.5, 70.4) | 46.4 (37.3, 55.8) |
| Area of residence | ||||||||||||
| Rural | 71.8 (63.3, 79.0) | 80.5 (72.8, 86.5) | 40.3 (31.4, 49.9) | 75.6 (69.9, 80.5) | 67.1 (59.7, 73.8) | 52.5 (46.0, 58.9) | 79.3 (73.5, 84.1) | 54.0 (45.6, 62.2) | 60.2 (53.7, 66.4) | 65.6 (56.1, 74.0) | 61.5 (47.9, 73.6) | 37.8 (27.7, 49.1) |
| Urban | 74.3 (65.49,81.5) | 70.7 (61.4, 78.6) | 41.9 (33.1, 51.3) | 84.8 (79.5, 89.0) | 67.1 (59.7, 73.8) | 64.7 (58.5, 70.4) | 82.4 (75.5, 87.7) | 59.3 (47.8, 69.8) | 63.3 (50.0, 74.8) | 63.5 (54.5, 71.6) | 67.1 (55.8, 76.7) | 48.7 (39.6, 57.8) |
| Region | ||||||||||||
| North | 73.2 (58.7, 84.1) | 70.8 (50.9, 85.1) | 55.4 (38.6, 71.0) | 81.4 (71.0, 88.6) | 75.4 (59.3, 86.6) | 67.1 (56.8, 76.0) | 89.5 (78.1, 95.3) | 76.9 (52.2, 91.0) | 58.2 (26.5, 84.3) | 70.8 (53.5, 83.6) | 52.4 (30.3, 73.6) | 45.8 (26.7, 66.2) |
| Center | 70.4 (55.9, 81.7) | 69.2 (55.7, 80.0) | 39.1 (26.9, 53.0) | 85.0 (79.2,89.4) | 64.7 (55.3, 73.0) | 65.8 (57.1, 73.6) | 81.2 (72.2, 87.7) | 47.9 (36.4, 59.5) | 67.0 (55.2, 77.0) | 71.3 (62.2, 78.9) | 68.4 (55.4, 79.0) | 47.2 (37.0, 57.7) |
| Mexico City and State of Mexico | 78.3 (63.1, 88.4) | 70.2 (49.5, 85.0) | 43.2 (26.0, 62.1) | 88.5 (76.1, 94.9) | 70.5 (56.9, 81.3) | 70.5 (59.0, 79.8) | 72.3 (56.8, 83.9) | 67.9 (55.4, 78.2) | 75.3 (57.6, 87.3) | 58.8 (44.7, 71.7) | 77.0 (64.5, 86.1) | 60.3 (46.5, 72.6) |
| South | 75.4 (65.6, 83.1) | 81.1 (71.5, 88.0) | 35.2 (26.1, 45.6) | 77.2 (68.9, 83.8) | 63.3 (53.4, 72.2) | 49.3 (40.8, 57.7) | 80.9 (73.5, 86.5) | 53.2 (41.1, 64.9) | 54.5 (42.7, 65.7) | 55.3 (42.0, 67.8) | 66.8 (52.3, 78.6) | 38.4 (27.3, 50.8) |
| Socioeconomic status | ||||||||||||
| Low | 70.5 (60.5, 78.9) | 82.0 (71.2, 89.4) | 38.0 (28.2, 49.0) | 75.7 (68.8, 81.5) | 71.2 (61.7, 79.2) | 58.8 (50.7, 66.5) | 75.2 (67.1, 81.9) | 61.7 (51.3, 71.2) | 58.1 (49.2, 66.6) | 49.5 (35.6, 63.5) | 64.4 (50.8,76.0) | 37.3 (26.3, 49.9) |
| Medium | 71.4 (59.0, 81.3) | 74.3 (62.4, 83.5) | 39.2 (27.3, 52.5) | 81.0 (73.9, 86.6) | 72.0 (64.4, 78.5) | 59.2 (51.1, 66.9) | 83.7 (75.7, 89.5) | 52.2 (38.6, 65.5) | 63.2 (48.3, 76.0) | 64.1 (53.0, 73.8) | 63.4 (48.0, 76.5) | 48.5 (35.8, 61.4) |
| High | 78.7 (66.1, 87.5) | 65.4 (51.7, 76.9) | 47.0 (34.2, 60.1) | 87.2 (79.9, 92.1) | 60.4 (49.9, 70.0) | 64.2 (55.6, 72.0) | 83.1 (73.0, 89.9) | 60.6 (45.2, 74.1) | 64.1 (44.4, 80.0) | 70.6 (60.7, 78.9) | 67.2 (52.0, 79.5) | 47.9 (36.8, 59.2) |
| Body mass indexa (kg/m2) | ||||||||||||
| Normal | 72.3 (65.1, 78.5) | 74.9 (67.0, 81.4) | 41.8 (34.3, 49.7) | 78.5 (72.8, 83.3) | 76.5 (70.8, 81.4) | 59.1 (53.2, 64.8) | 68.1 (61.0, 74.5) | 69.0 (62.8, 74.5) | 60.3 (52.3, 67.8) | 60.8 (47.6, 72.6) | 70.8 (57.1,81.6) | 45.4 (33.7, 57.8) |
| Overweight | 71.2 (29.6, 93.6) | 97.9 (90.3, 99.6) | 41.6 (14.0, 75.7) | 84.7 (75.4, 90.9) | 60.3 (48.7, 70.8) | 60.2 (48.4, 70.9) | 82.4 (75.8, 87.5) | 75.7 (65.5, 83.6) | 70.1 (60.6, 78.1) | 61.7 (51.5, 71.0) | 73.0 (59.7, 83.1) | 47.9 (37.9, 58.1) |
| Obesity | 100 | 40.3 (11.0, 78.8) | 68.4 (28.8, 92.1) | 88.0 (80.0, 93.1) | 66.6 (49.4, 80.2) | 61.5 (48.1, 73.3) | 86.8 (72.7, 94.2) | 81.5 (58.1, 93.3) | 50.6 (19.4, 81.3) | 68.0 (56.7, 77.4) | 56.4 (41.7, 70.0) | 44.0 (32.0, 56.8) |
| Sodium Intake Quartiles (mg/day) | n | First | Second | Third | Fourth | p | ||||
| Mean | 95%CI | Mean | 95%CI | Mean | 95%CI | Mean | 95%CI | |||
| 1356 | 801.8 | (761.9, 841.7) | 1578.93 | (1517.6, 1649.2) | 2438.4 | (2381.6, 2494.9) | 5049.6 | (4579.4, 5519.8) | - | |
| BMI (kg/m2) a | 1294 | 28.7 | (27.2, 30.2) | 28.5 | (27.2, 29.8) | 28.7 | (27.0, 30.3) | 28.2 | (27.1, 29.4) | 0.966 |
| Waist circumference (cm). Women | 554 | 96.4 | (91.4, 101.3) | 93.5 | (88.9, 98.2) | 94.2 | (90.2, 98.2) | 94.1 | (90.8, 97.4) | 0.853 |
| Men | 356 | 98.562 | (89.8, 107.3) | 95.0 | (90.9, 99.1) | 98.1 | (93.8, 102.5) | 97.3753 | (92.0, 102.8) | 0.749 |
| SBP (mm Hg) | 901 | 123.2 | (119.7, 126.8) | 128.3 | (119.6, 136.9) | 120.5 | (117.1, 123.9) | 122.1 | (117.2, 127.0) | 0.373 |
| DBP (mm Hg) | 901 | 73.7 | (71.3, 76.2) | 76.4 | (73.1, 79.7) | 73.4 | (70.9, 75.8) | 72.1 | (69.6, 74.6) | 0.259 |
| eGFR (mL/min/1.73 m2) | 922 | 116.6 | (110.6, 122.5) | 113.7 | (107.4, 120.1) | 123.3 | (108.2, 138.4) | 112.4 | (108.3, 116.5) | 0.486 |
| Glucose (mg/dL) | 922 | 107.4 | (101.4, 113.4) | 115.8 | (96.0, 135.5) | 109.9 | (98.0, 121.7) | 101.0 | (95.9, 106.0) | 0.185 |
| Cholesterol (mg/dL) b | 922 | 202.5 | (189.0, 216.0) | 193.5 | (178.4, 208.6) | 184.4 | (172.8, 196.1) | 181.4 | (173.6, 189.1) | 0.058 |
| HDL-c (mg/dL) c | 922 | 40.8 | (38.1, 43.6) | 35.7 | (31.6 39.8) | 38.9 | (35.2, 42.6) | 35.5 | (33.2, 37.8) | 0.026 |
| LDL-c (mg/dL) d | 865 | 123.6 | (110.1, 137) | 115.3 | (108.3, 122.3) | 111.9 | (102.3, 121.4) | 106.6 | (98.8, 114.3) | 0.156 |
| TG (mg/dL), mean (95%CI) e | 922 | 197.8 | (176.3, 219.3) | 361.5 | (79.9, 643.1) | 218.8 | (153.4, 284.3) | 220.5 | (170.3, 270.6) | 0.547 |
| Diabetes f (%) | ||||||||||
| Prediabetes | 926 | 24.6 | (17.4, 33.6) | 27.79 | (15.0, 45.6) | 32.92 | (21.7, 46.6) | 28.46 | (16.5, 44.6) | 0.548 |
| Previous diagnosis | 12.31 | (7.9, 18.8) | 8.107 | (4.6, 13.8) | 7.305 | (4.2, 12.4) | 6.175 | (3.3, 11.2) | ||
| Survey finding | 9.9 | (3.7, 24.2) | 15.3 | (3.7, 46.4) | 9.1 | (2.4, 28.6) | 3.7 | (1.3, 9.9) | ||
| High blood pressure g (%) | ||||||||||
| Normal | 901 | 43.6 | (31.3, 56.8) | 32.0 | (20.3, 46.5) | 42.3 | (29.7, 56.0) | 46.8 | (33.2, 60.9) | 0.213 |
| Elevated | 11.5 | (6.7, 19.2) | 11.8 | (4.9, 25.7) | 18.3 | (8.6, 34.9) | 15.3 | (8.4, 26.4) | ||
| Stage 1 | 23.7 | (13.3, 38.6) | 20.8 | (9.6, 39.4) | 21.7 | (11.1, 38.0) | 9.8 | (5.5, 17.0) | ||
| Stage 2 | 7.9 | (4.5, 13.5) | 25.6 | (10.4, 50.6) | 8.4 | (4.6, 15.0) | 11.4 | (4.4, 26.5) | ||
| Previous diagnosis | 13.2 | (8.7, 19.6) | 9.7 | (5.6, 16.3) | 9.3 | (4.5, 18.3) | 16.7 | (8.0, 31.6) | ||
| Coronary heart disease (%) | 926 | 0.7 | (0.1, 3.4) | 1.5 | (0.6, 4.2) | 1.9 | (0.6, 5.7) | 4.1 | (0.7, 21.7) | 0.385 |
| Cerebro-vascular disease (%) | 916 | 0.0 | 0.5 | (0.1, 3.3) | 0.1 | (0.0, 1.1) | 0.9 | (0.1, 6.0) | 0.580 | |
| Smoking (%) | ||||||||||
| Never | 926 | 43.2 | (32.0, 55.1) | 65.8 | (51.5, 77.8) | 54.9 | (40.8, 68.2) | 31.8 | (21.3, 44.5) | 0.002 |
| Current smoker | 20.1 | (11.4, 33.1) | 6.4 | (3.6, 11.1) | 13.7 | (7.0, 25.2) | 30.9 | (18.4, 46.9) | ||
| Ex-smoker | 36.7 | (26.2, 48.7) | 27.8 | (17.4, 41.3) | 31.4 | (20.2, 45.3) | 37.3 | (24.8, 51.8) | ||
| Potassium intake quartiles (mg/day) | n | First | Second | Third | Fourth | p | ||||
| Mean | 95%CI | Mean | 95%CI | Mean | 95%CI | Mean | 95%CI | |||
| 1356 | 965.4 | (921.1, 1009.7) | 1552.2 | (1510.6, 1593.7) | 2210.9 | (2166.5, 2255.5) | 5039.5 | (4338.9, 5740.1) | - | |
| BMI (kg/m2) a | 1294 | 28.3 | (27.1, 29.5) | 27.4 | (26.4, 28.5) | 29.4 | (28.2, 30.6) | 28.6 | (27.3, 29.9) | 0.096 |
| Waist circumference (cm). Women | 554 | 98.2 | (93.5, 102.9) | 93.6 | (89.4, 97.7) | 96.6 | (93.0, 100.3) | 92.1 | (88.9, 95.4) | 0.143 |
| Men | 356 | 91.4 | (87.5, 95.3) | 95.7 | (91.3, 100.0) | 98.4 | (94.8, 102.1) | 98.2 | (93.4, 103.1) | 0.056 |
| SBP (mm Hg) | 901 | 122.0 | (117.8, 126.2) | 122.4 | (116.8, 127.9) | 122.3 | (119.6, 125.0) | 123.7 | (118.6, 128.8) | 0.959 |
| DBP (mm Hg) | 901 | 73.9 | (70.6, 77.2) | 74.5 | (71.7, 77.2) | 74.4 | (72.1, 76.7) | 72.8 | (70.5, 75.2) | 0.758 |
| eGFR (mL/min/1.73 m2) | 922 | 115.2 | (112.0, 118.4) | 117.6 | (110.4, 124.7) | 118.0 | (113.1, 122.8) | 115.3 | (107.2, 123.4) | 0.819 |
| Glucose (mg/dL) | 922 | 118.0 | (98.0, 138.0) | 102.0 | (97.1, 106.9) | 105.9 | (99.2, 112.6) | 106.7 | (97.5, 115.9) | 0.289 |
| Cholesterol (mg/dL) b | 922 | 181.8 | (172.1, 191.6) | 187.9 | (176.9, 198.8) | 198.7 | (187.8, 209.5) | 184.1 | (174.7, 193.6) | 0.112 |
| HDL-c (mg/dL), c | 922 | 41.6 | (39.3, 43.9) | 39.9 | (33.3, 46.5) | 40.1 | (37.7, 42.4) | 34.3 | (32.4, 36.1) | 0.000 |
| LDL-c (mg/dL) d | 865 | 104.9 | (95.7, 114.1) | 112.7 | (104.2, 121.2) | 123.5 | (113.5, 133.5) | 108.7 | (101.4, 115.9) | 0.036 |
| TG (mg/dL), mean (95%CI) e | 922 | 225.6 | (145.9, 305.2) | 224.9 | (113.0, 336.9) | 235.3 | (160.9, 309.8) | 258.7 | (145.3, 372.1) | 0.969 |
| Diabetes f (%) | ||||||||||
| Prediabetes | 926 | 24.7 | (14.8, 38.3) | 29.3 | (16.8, 46.0) | 24.8 | (14.9, 38.4) | 31.5 | (20.4, 45.2) | 0.505 |
| Previous diagnosis | 9.2 | (5.3, 15.5) | 9.8 | (5.8, 16.0) | 12.3 | (7.5, 19.5) | 5.0 | (2.8, 8.9) | ||
| Survey finding | 17.8 | (4.5, 50.0) | 5.4 | (2.5, 11.4) | 5.2 | (1.5, 16.9) | 8.0 | (2.6, 22.2) | ||
| High blood pressure g (%) | ||||||||||
| Normal | 901 | 47.4 | (31.5, 63.9) | 41.3 | (28.0, 56.2) | 36.1 | (25.8, 47.9) | 43.4 | (31.2, 56.4) | 0.754 |
| Elevated | 10.1 | (4.9, 19.6) | 9.4 | (5.0, 16.8) | 20.3 | (10.4, 35.8) | 15.9 | (8.7, 27.5) | ||
| Stage 1 | 24.5 | (9.3, 50.6) | 22.9 | (11.8, 39.8) | 19.3 | (10.6, 32.4) | 12.7 | (7.6, 20.6) | ||
| Stage 2 | 8.9 | (4.2, 18.1) | 12.7 | (5.1, 28.2) | 11.0 | (5.9, 19.5) | 14.8 | (6.5, 30.1) | ||
| Previous diagnosis | 9.1 | (5.1, 15.6) | 13.7 | (8.1, 22.3) | 13.3 | (7.9, 21.6) | 13.2 | (6.3, 25.6) | ||
| Coronary heart disease (%) | 926 | 1.0 | (0.3, 3.5) | 0.7 | (0.1, 4.6) | 3.2 | (1.2, 7.9) | 3.2 | (0.6, 16.8) | 0.496 |
| Cerebro-vascular disease (%) | 916 | 0.7 | (0.1, 5.3) | 0.0 | 0 | 0.2 | (0.0, 1.6) | 0.7 | (0.1, 4.6) | 0.699 |
| Smoking (%) | 926 | |||||||||
| Never | 58.2 | (42.3, 72.5) | 50.8 | (36.7, 64.7) | 45.4 | (33.7, 57.7) | 42.5 | (30.7, 55.2) | 0.691 | |
| Current smoker | 17.8 | (8.9, 32.2) | 20.2 | (10.8, 34.5) | 22.4 | (12.9, 36.0) | 19.6 | (10.3, 34.0) | ||
| Ex-smoker | 24.1 | (15.5, 35.4) | 29.1 | (19.6, 40.8) | 32.2 | (22.1, 44.2) | 37.9 | (26.7, 50.7) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vargas-Meza, J.; Cervantes-Armenta, M.A.; Campos-Nonato, I.; Nieto, C.; Marrón-Ponce, J.A.; Barquera, S.; Flores-Aldana, M.; Rodríguez-Ramírez, S. Dietary Sodium and Potassium Intake: Data from the Mexican National Health and Nutrition Survey 2016. Nutrients 2022, 14, 281. https://doi.org/10.3390/nu14020281
Vargas-Meza J, Cervantes-Armenta MA, Campos-Nonato I, Nieto C, Marrón-Ponce JA, Barquera S, Flores-Aldana M, Rodríguez-Ramírez S. Dietary Sodium and Potassium Intake: Data from the Mexican National Health and Nutrition Survey 2016. Nutrients. 2022; 14(2):281. https://doi.org/10.3390/nu14020281
Chicago/Turabian StyleVargas-Meza, Jorge, Manuel A. Cervantes-Armenta, Ismael Campos-Nonato, Claudia Nieto, Joaquín Alejandro Marrón-Ponce, Simón Barquera, Mario Flores-Aldana, and Sonia Rodríguez-Ramírez. 2022. "Dietary Sodium and Potassium Intake: Data from the Mexican National Health and Nutrition Survey 2016" Nutrients 14, no. 2: 281. https://doi.org/10.3390/nu14020281
APA StyleVargas-Meza, J., Cervantes-Armenta, M. A., Campos-Nonato, I., Nieto, C., Marrón-Ponce, J. A., Barquera, S., Flores-Aldana, M., & Rodríguez-Ramírez, S. (2022). Dietary Sodium and Potassium Intake: Data from the Mexican National Health and Nutrition Survey 2016. Nutrients, 14(2), 281. https://doi.org/10.3390/nu14020281







