Vitamin D Status during Pregnancy versus the Anthropometric Parameters of Two- and Four-Year-Olds: A Pilot Study
Abstract
1. Introduction
2. Material and Methods
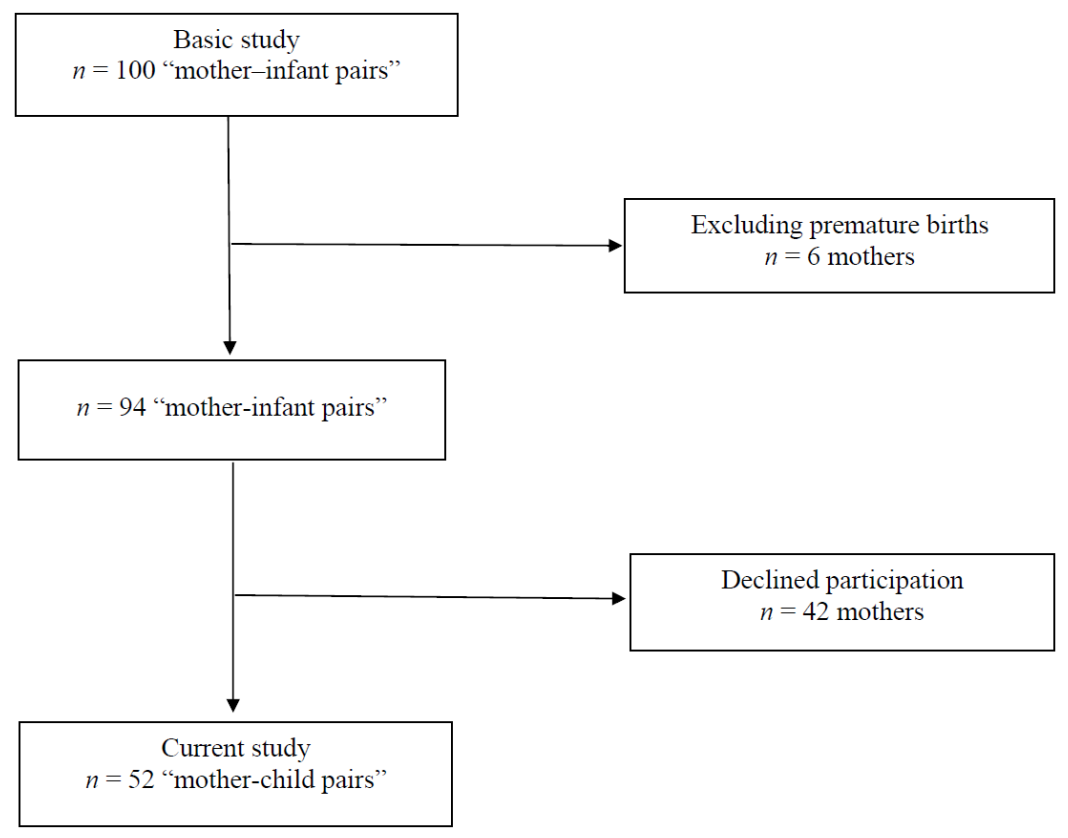
2.1. Study Design
2.2. Laboratory Analysis and Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Manios, Y.; Moschonis, G.; Lambrinou, C.P.; Tsoutsoulopoulou, K.; Binou, P.; Karachaliou, A.; Breidenassel, C.; Gonzalez-Gross, M.; Kiely, M.; Cashman, K.D. A systematic review of vitamin D status in southern European countries. Eur. J. Nutr. 2018, 57, 2001–2036. [Google Scholar] [CrossRef] [PubMed]
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid. Biochem. Mol. Biol. 2014, 144, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Płudowski, P.; Ducki, C.; Konstantynowicz, J.; Jaworski, M. Vitamin D status in Poland. Pol. Arch. Med. Wewn. 2016, 126, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Saraf, R.; Morton, S.M.B.; Camargo, C.A.; Gran, C.C. Global summary of maternal and newborn vitamin D status—A systematic review. Maternal and Child Nutrition 2016, 12, 647–668. [Google Scholar] [CrossRef]
- Holick, M.F.; Binkley, N.C.; Bischoff- Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Skowrońska-Jóźwiak, E.; Adamczewski, Z.; Tyszkiewicz, A.; Krawczyk-Rusiecka, K.; Lewandowski, K.; Lewinski, A. Assessment of adequacy of vitamin D supplementation during pregnancy. Ann. Agric. Environ. Med. 2014, 21, 198–200. [Google Scholar]
- Bartoszewicz, Z.; Kondracka, A.; Krasnodębska-Kiljańska, M.; Niedźwiedzka, B.; Popow, M.; Ambroziak, U.; Bednarczuk, T. Vitamin D insufficiency in healthy pregnant women living in Warsaw. Ginekol. Pol. 2013, 84, 363–367. [Google Scholar] [CrossRef]
- Wierzejska, R.; Jarosz, M.; Sawicki, W.; Bachanek, M.; Siuba-Strzelińska, M. Vitamin D concentration in maternal and umbilical cord blood by season. Int. J. Environ. Res. Public Health 2017, 14, 1121. [Google Scholar] [CrossRef]
- Domaracki, P.; Sadlecki, P.; Odrowąż-Sypniewska, G.; Dzikowska, E.; Walentowicz, P.; Siodmiak, J.; Grabiec, M.; Walentowicz-Sadlecka, M. Serum 25(OH) vitamin D levels in Polish women during pregnancies complicated by hypertensive disorders and gestational diabetes. Int. J. Mol. Sci. 2016, 17, 1574. [Google Scholar] [CrossRef]
- Itkonen, S.T.; Erkkola, M.; Lamberg-Allardt, C.J.E. Vitamin D fortification of fluid milk products and their contribution to vitamin D intake and vitamin D status in observational studies—A review. Nutrients 2018, 10, 1054. [Google Scholar] [CrossRef]
- Kunachowicz, H.; Przygoda, B.; Nadolna, I.; Iwanow, K. Food Composition Tables, 2nd ed.; PZWL: Warsaw, Poland, 2017; pp. 51–290. [Google Scholar]
- Rusińska, A.; Płudowski, P.; Walczak, M.; Borszewska-Kornacka, M.K.; Bossowski, A.; Chlebna-Sokół, D.; Czech-Kowalska, J.; Dobrzańska, A.; Franek, E.; Helwich, E.; et al. Vitamin D supplementation guidelines for Poland—A 2018 update. Standardy medyczne/Pediatria 2018, 15, 531–559. [Google Scholar] [CrossRef]
- Blumfield, M.L.; Hure, A.J.; Macdonald-Wicks, L.; Smith, R.; Collins, C.E. Micronutrient intakes during pregnancy in developed countries: Systematic review and meta-analysis. Nutr. Rev. 2013, 71, 118–132. [Google Scholar] [CrossRef]
- Wierzejska, R. Consumption of vitamin D and its sources in diet of pregnant women. Pol. J. Hum. Nutr. Metabol. 2018, 45, 172–180. [Google Scholar]
- Przygoda, B.; Wierzejska, R.; Matczuk, E.; Kłys, W.; Jarosz, M. Vitamins. In Nutrition Standards for the Population of Poland and Their Application; Jarosz, M., Rychlik, E., Stoś, K., Charzewska, J., Eds.; National Institute of Public Health—National Institute of Hygiene: Warsaw, Poland, 2020; pp. 171–272. [Google Scholar]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Dietary reference values for vitamin D. European Food Safety Authority. EFSA J. 2016, 14, 4547. [Google Scholar]
- Weker, H.; Barańska, M.; Riahi, A.; Strucińska, M.; Więch, M.; Rowicka, G.; Dyląg, H.; Klemarczyk, W.; Bzikowska, A.; Socha, P. Dietary patterns in toddlers with excess weight. The 2016 pitnuts study. Dev. Period Med. 2017, 21, 272–285. [Google Scholar]
- Merkiel, S.; Chalcarz, W. Preschool diets in children from Piła, Poland, require urgent intervention as implied by high risk of nutrient inadequacies. J. Health Popul. Nutr. 2016, 35, 11. [Google Scholar] [CrossRef]
- Kennel, K.A.; Drake, M.T.; Hurley, D.L. Vitamin D deficiency in adults: When to test and how to treat. Mayo Clin Proc. 2010, 85, 752–758. [Google Scholar] [CrossRef]
- Płudowski, P.; Karczmarewicz, E.; Bayer, M.; Carter, G.; Chlebna-Sokół, D.; Czech-Kowalska, J.; Dębski, R.; Decsi, T.; Dobrzańska, A.; Franek, E.; et al. Practical guidelines for the supplementation of vitamin D and the treatment of deficits in Central Europe—Recommended vitamin D intakes in the general population and groups at risk of vitamin D deficiency. Endokrynol. Pol. 2013, 64, 319–327. [Google Scholar] [CrossRef]
- Fang, K.; He, Y.; Mu, M.; Liu, K. Maternal vitamin D deficiency during pregnancy and low birth weight: A systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2021, 34, 1167–1173. [Google Scholar] [CrossRef]
- Pilz, S.; Zittermann, A.; Obeid, R.; Hahn, A.; Pludowski, P.; Trummer, C.; Lerchbaum, E.; Pérez-López, F.R.; Karras, S.N.; März, W. The role of vitamin D in fertility and during pregnancy and lactation: A review of clinical data. Int. J. Environ. Res. Public Health 2018, 15, 2241. [Google Scholar] [CrossRef]
- Moon, R.J.; Davies, J.H.; Cooper, C.; Harvey, N.C. Vitamin D, and maternal and child health. Calcif. Tissue Intern 2020, 106, 30–46. [Google Scholar] [CrossRef]
- Rostami, M.; Simbar, M.; Amiri, M.; Bidhendi-Yarandi, R.; Hosseinpanah, F.; Tehrani, F.R. The optimal cut-off point of vitamin D for pregnancy outcomes using a generalized additive model. Clin. Nutr. 2021, 40, 2145–2153. [Google Scholar] [CrossRef]
- Nobles, C.J.; Markenson, G.; Chasan-Taber, L. Early pregnancy vitamin D status and risk for adverse maternal and infant outcomes in a bi-ethnic cohort: The Behaviors Affecting Baby and You (B.A.B.Y.) study. Br. J. Nutr. 2015, 114, 2116–2128. [Google Scholar] [CrossRef]
- Eggemoen, Å.R.; Jenum, A.K.; Mdala, I.; Knutsen, K.V.; Lagerløv, P.; Sletner, L. Vitamin D levels during pregnancy and associations with birth weight and body composition of the newborn: A longitudinal multiethnic population-based study. Br. J. Nutr. 2017, 117, 985–993. [Google Scholar] [CrossRef]
- Aghajafari, F.; Nagulesapillai, T.; Ronksley, P.E.; Tough, S.C.; O’Beirne, M.; Rabi, D.M. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: Systematic review and meta-analysis of observational studies. BMJ 2013, 346, f1169. [Google Scholar] [CrossRef]
- Eckhardt, C.L.; Gernand, A.D.; Roth, D.E.; Bodnar, L.M. Maternal vitamin D status and infant anthropometry in a US multi-centre cohort study. Ann. Hum. Biol. 2015, 42, 215–222. [Google Scholar]
- Marco, N.D.; Kaufman, J.; Rodda, C.P. Shedding light on vitamin D status and its complexities during pregnancy, infancy and childhood: An Australian perspective. Int. J. Environ. Res. Public Health 2019, 16, 538. [Google Scholar] [CrossRef]
- Elsori, D.H.; Hammoud, M.S. Vitamin D deficiency in mothers, neonates and children. J. Steroid. Biochem. Mol. Biol. 2018, 175, 195–199. [Google Scholar] [CrossRef]
- Brustad, N.; Garland, J.; Thorsen, J.; Sevelsted, A.; Krakauer, M.; Vinding, R.K.; Stokholm, J.; Bønnelykke, K.; Bisgaard, H.; Chawes, B.L. Effect of high-dose vs standard-dose vitamin D supplementation in pregnancy on bone mineralization in offspring until age 6 years: A prespecified secondary analysis of a double-blinded, randomized clinical trial. JAMA Pediatr. 2020, 174, 1–9. [Google Scholar] [CrossRef]
- Bitew, Z.W.; Worku, T.; Alemu, A. Effects of vitamin D on neonatal sepsis: A systematic review and meta-analysis. Food Sci. Nutr. 2021, 9, 375–388. [Google Scholar] [CrossRef]
- Shor, D.B.; Barzel, J.; Tauber, E.; Amital, H. The effects of maternal vitamin D on neonatal growth parameters. Eur. J. Pediatr. 2015, 174, 1169–1174. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Yu, X.D.; Huang, L.S.; Chen, Q.; Ouyang, F.X.; Wang, X.; Zhang, J. Fetal vitamin D concentration and growth, adiposity and neurodevelopment during infancy. Eur. J. Clin. Nutr. 2018, 72, 1396–1403. [Google Scholar] [CrossRef] [PubMed]
- von Websky, K.; Hasan, A.A.; Reichetzeder, C.; Tsuprykov, O.; Hocher, B. Impact of vitamin D on pregnancy-related disorders and on offspring outcome. J. Steroid. Biochem. Mol. Biol. 2018, 180, 51–64. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.Q.; Qi, H.P.; Luo, Z.C.; Fraser, W.D. Maternal vitamin D status and pregnancy outcomes: A systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 2013, 26, 889–899. [Google Scholar] [CrossRef]
- Jiang, X.; Lu, J.; Zhang, Y.; Teng, H.; Pei, J.; Zhang, C.; Guo, B.; Yin, J. Association between maternal vitamin D status with pregnancy outcomes and offspring growth in a population of Wuxi, China. Asia Pac. J. Clin. Nutr. 2021, 30, 464–476. [Google Scholar]
- Craig, F.M.; Nick, S.; Kiely, M.; Specker, B.L.; Thacher, T.D.; Ozono, K.; Michigami, T.; Tiosano, D.; Mughal, M.Z.; Mäkitie, O.; et al. Global consensus recommendations on prevention and management of nutritional rickets. J. Clin. Endocrinol. Metab. 2016, 101, 394–415. [Google Scholar]
- Wierzejska, R.; Jarosz, M.; Klemińska-Nowak, M.; Tomaszewska, M.; Sawicki, W.; Bachanek, M.; Siuba-Strzelińska, M. Maternal and cord blood vitamin D status and anthropometric measurements in term newborns at birth. Front. Endocrinol. 2018, 9, 9. [Google Scholar] [CrossRef]
- Kiely, M.; O’Donovan, S.M.; Kenny, L.C.; Hourihane, J.O.; Irvine, A.D.; Murray, D.M. Vitamin D metabolite concentrations in umbilical cord blood serum and associations with clinical characteristics in large prospective mother-infant cohort in Ireland. J. Steroid. Biochem. Mol. Biol. 2017, 167, 162–168. [Google Scholar] [CrossRef]
- Treiber, M.; Mujezinovic, F.; Pecovnik Balon, B.; Gorenjak, M.; Maver, U.; Dovnik, A. Association between umbilical cord vitamin D levels and adverse neonatal outcomes. J. Intern. Med. Res. 2020, 48, 1–11. [Google Scholar] [CrossRef]
- Dovnik, A.; Mujezinović, F.; Treiber, M.; Pečovnik Balon, B.; Gorenjak, M.; Maver, U.; Takač, I. Seasonal variations of vitamin D concentrations in pregnant women and neonates in Slovenia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 181, 6–9. [Google Scholar] [CrossRef]
- Jacquemyn, Y.; Ajaji, M.; Karepouan, N. Vitamin D levels in maternal serum and umbilical cord blood in a multi-ethnic population in Antwerp, Belgium. Facts Views Vis. ObGyn. 2013, 5, 3–5. [Google Scholar]
- Morales, E.; Rodriguez, A.; Valvi, D.; Iñiguez, C.; Esplugues, A.; Vioque, J.; Marina, L.S.; Jiménez, A.; Espada, M.; Dehli, C.R.; et al. Deficit of vitamin D in pregnancy and growth and overweight in the offspring. Int. J. Obes. 2015, 39, 61–68. [Google Scholar] [CrossRef]
- van Eijsden, M.; Snijder, M.B.; Brouwer, I.; Vrijkotte, T.G.M. Maternal early-pregnancy vitamin D status in relation to linear growth at the age of 5–6 years: Results of the ABCD cohort. Eur. J. Clin. Nutr. 2013, 67, 972–977. [Google Scholar] [CrossRef][Green Version]
- Hauta-Alus, H.H.; Kajantie, E.; Holmlund-Suila, E.M.; Rosendahl, J.; Valkama, S.M.; Enlund-Cerullo, M.; Helve, O.M.; Hytinantti, T.K.; Viljakainen, H.; Andersson, S. High pregnancy, cord blood, and infant vitamin D concentrations may predict slower infant growth. J. Clin. Endocrinol. Metab. 2019, 104, 397–407. [Google Scholar] [CrossRef]
- Gould, J.F.; Anderson, A.J.; Yelland, L.N.; Smithers, L.G.; Skeaff, C.M.; Zhou, S.J.; Gibson, R.A.; Makrides, M. Association of cord blood vitamin D with early childhood growth and neurodevelopment. J. Paediatr. Child Health 2017, 53, 75–83. [Google Scholar] [CrossRef]
- Larsen, S.D.; Christensen, M.E.; Dalgård, C.; Lykkedegn, S.; Andersen, L.B.; Andersen, M.S.; Glintborg, D.; Christesen, H.T. Pregnancy or cord 25-hydroxyvitamin D is not associated with measures of body fat or adiposity in children from three months to three years of age. An Odense Child Cohort study. Clin. Nutr. 2020, 39, 1832–1839. [Google Scholar] [CrossRef]
- Roth, D.E.; Perumal, N.; Mahmud, A.A.; Baqui, A.H. Maternal vitamin D3 supplementation during the third trimester of pregnancy: Effects on infant growth in a longitudinal follow-up study in Bangladesh. J. Pediatr. 2013, 163, 1605–1611. [Google Scholar] [CrossRef]
- Bi, W.G.; Nuyt, A.M.; Weiler, H.; Leduc, L.; Santamaria, C.; Wei, S.Q. Association between vitamin D supplementation during pregnancy and offspring growth, morbidity, and mortality: A systematic review and meta-analysis. JAMA Pediatr. 2018, 172, 635–645. [Google Scholar] [CrossRef]
- WHO antenatal care recommendations for a positive pregnancy experience. In Nutritional Interventions Update: Vitamin D Supplements during Pregnancy; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/333562 (accessed on 15 October 2021).
- Zimmer, M.; Sieroszewski, P.; Oszukowski, P.; Huras, H.; Fuchs, T.; Pawłosek, A. Rekomendacje Polskiego Towarzystwa Ginekologów i Położników dotyczące suplementacji u kobiet ciężarnych. Ginekol. Perinatol. Prakt. 2020, 5, 170–181. (In Polish) [Google Scholar]
- Shakiba, M.; Iranmanesh, M.R. Vitamin D requirement in pregnancy to prevent deficiency in neonates: A randomized trial. Singap. Med. 2013, 54, 285–288. [Google Scholar] [CrossRef]
- Regulation of the Minister of Health of 24 September 2013 on guaranteed services in the field of primary health care. Pol. J. Laws 2013, 1248 (28 October 2013).
| Mothers: | |
| Number of women, n (%) | 52 (100) |
| Age (in years) mean ± SD | 30.2 ± 5.0 |
| Education, n (%) | |
| higher | 36 (69.3) |
| other | 16 (30.7) |
| Gravidity, n (%) | |
| primiparas | 24 (46.2) |
| multiparas | 28 (53.8) |
| Pre-pregnancy maternal BMI, mean ± SD | 23.1 ± 4.2 |
| Weight gain during pregnancy, n (%) | |
| low | 10 (19.2) |
| normal | 22 (42.3) |
| excessive | 20 (38.5) |
| Gestational diabetes, n (%) | 6 (11.5) |
| Smoking during pregnancy, n (%) | 8 (15.4) |
| Professionally active during pregnancy, n (%) | 31 (59.6) |
| Supplementation with vitamin/mineral preparations, n (%) | 51 (98.1) |
| Supplementation with single-component vitamin D preparations, n (%) | 7 (13.4) |
| Daily vitamin D consumption—from diet and supplements (µg) | |
| median (min-max) | 19.3 (1.2–73.7) |
| Daily calcium consumption—from milk and dairy products (mg) | |
| mean ± SD | 689 ± 455 |
| Daily caffeine consumption—from coffee, tea, and energy drinks (mg) median (min-max) | 50 (0–203) |
| Maternal serum vitamin D concentrations (ng/mL) mean ± SD | 18.3 ± 8.0 |
| Newborns: | |
| Gestational age (weeks) mean ± SD | 39.0 ± 1.9 |
| Sex of the newborn | |
| male, n (%) | 25 (48.1) |
| female, n (%) | 27 (51.9) |
| Neonatal weight (g) mean ± SD | 3512 ± 578 |
| Low birth weight (<2500 g), n (%) | 3 (5.8) |
| Macrosomia (>4000 g), n (%) | 11 (21.2) |
| Neonatal length (cm) mean ± SD | 55.6 ± 3.0 |
| Apgar score (points) mean ± SD | 9.9 ± 0.1 |
| Neonatal head circumference (cm) mean ± SD | 34.7 ± 1.5 |
| Neonatal chest circumference (cm) mean ± SD | 33.9 ± 2.3 |
| Cord blood vitamin D concentrations (ng/mL) mean ± SD | 25.4 ± 10.8 |
| Children at the age of 2: | |
| weight (kg) mean ± SD | 11.3 ± 1.1 |
| number of children with weight of <3 centile, n (%) | 2 (3.7) |
| number of children with weight of >90 centile, n (%) | 0 (0) |
| height (cm) mean ± SD | 89.5 ± 2.6 |
| number of children with height of <3 centile, n (%) | 0 (0) |
| number of children with height of >90 centile, n (%) | 15 (28.8) |
| Children at the age of 4: | |
| weight (kg) mean ± SD | 15.7 ± 1.3 |
| number of children with weight of <3 centile, n (%) | 2 (3.7) |
| number of children with weight of >90 centile, n (%) | 1 (1.9) |
| height (cm) mean ± SD | 103.5 ± 5.2 |
| number of children with height of <3 centile, n (%) | 3 (5.8) |
| number of children with height of >90 centile, n (%) | 7 (13.5) |
| Regression Beta Coefficient (SE) | 95% CI | p-Value | |
|---|---|---|---|
| Maternal serum vitamin D concentration | 0.07 (0.543) | −1.04; 1.17 | 0.8990 |
| Cord blood vitamin D concentration | −0.32 (0.552) | −1.44; 0.81 | 0.5682 |
| Neonatal weight | 0.00 (0.001) | −0.00; 0.00 | 0.2675 |
| Pre-pregnancy body mass index: | |||
| underweight | −0.06 (0.664) | −1.41; 1.29 | 0.9317 |
| overweight/obesity | 0.26 (0.732) | −1.23; 1.75 | 0.7280 |
| Low weight gain vs. normal gain | 0.07 (0.594) | −1.14; 1.28 | 0.9061 |
| Excessive weight gain vs. normal gain | −0.01 (0.626) | −1.28; 1.27 | 0.9893 |
| Gestational age | 0.62 (0.158) | −0.26; 0.39 | 0.6974 |
| Smoking | 0.45 (0.594) | −0.76; 1.66 | 0.4517 |
| Maternal age | 0.05 (0.420) | −0.80; 0.91 | 0.9000 |
| Gravidity | −0.53 (0.394) | −0.86; 0.75 | 0.8938 |
| Caffeine consumption | −0.01 (0.004) | −0.01; 0.00 | 0.1630 |
| Vitamin D consumption | 0.01 (0.001) | −0.01; 0.03 | 0.2033 |
| Calcium consumption | 0.00 (0.000) | −0.00; 0.00 | 0.8221 |
| Sex | 0.42 (0.419) | −0.43; 1.27 | 0.2297 |
| Regression Beta Coefficient (SE) | 95% CI | p-Value | |
|---|---|---|---|
| Maternal serum vitamin D concentration | 0.66 (1.279) | −1.95; 3.26 | 0.6115 |
| Cord blood vitamin D concentration | −0.72 (1.301) | −3.36; 1.94 | 0.5862 |
| Neonatal weight | 0.00 (0.001) | −0.00; 0.00 | 0.6790 |
| Pre-pregnancy body mass index: | |||
| underweight | −2.22 (1.563) | −5.41; 0.96 | 0.1655 |
| overweight/obesity | −1.94 (1.723) | −5.46; 1.57 | 0.2671 |
| Low weight gain vs. normal gain | 0.78 (1.398) | −2.05; 3.65 | 0.5727 |
| Excessive weight gain vs. normal gain | 1.42 (1.475) | −1.58; 4.42 | 0.3433 |
| Gestational age | 0.24 (0.373) | −0.52; 0.99 | 0.5283 |
| Smoking | −1.04 (1.399) | −3.89; 1.81 | 0.4615 |
| Maternal age | 0.03 (0.989) | −1.99; 2.04 | 0.9791 |
| Gravidity | −1.15 (0.929) | −3.04; 0.74 | 0.2244 |
| Gestational diabetes | −0.07 (1.522) | −3.17; 3.03 | 0.9630 |
| Caffeine consumption | −0.02 (0.009) | −0.04; 0.00 | 0.0901 |
| Vitamin D consumption | −0.01 (0.021) | −0.05; 0.03 | 0.6663 |
| Calcium consumption | −0.00 (0.001) | −0.00; 0.00 | 0.6150 |
| Sex | 1.17 (0.986) | −0.83; 3.18 | 0.2428 |
| Regression Beta Coefficient (SE) | 95% CI | p-Value | |
|---|---|---|---|
| Weight at the age of 2 | 0.76 (0.153) | 0.44; 1.07 | 0.0001 |
| Maternal serum vitamin D concentration | 0.58 (0.469) | −0.37; 1.54 | 0.2250 |
| Cord blood vitamin D concentration | 0.12 (0.480) | −0.86; 1.10 | 0.8017 |
| Neonatal weight | 0.00 (0.000) | −0.00; 0.00 | 0.5696 |
| Pre-pregnancy body mass index: | |||
| underweight | 0.75 (0.574) | −1.42; 1.92 | 0.1993 |
| overweight/obesity | 0.52 (0.634) | −0.77; 1.82 | 0.4155 |
| Low weight gain vs. normal gain | −0.91 (0.513) | −1.24; 0.86 | 0.7110 |
| Excessive weight gain vs. normal gain | −0.61 (0.542) | −1.71; 0.49 | 0.2703 |
| Gestational age | 0.02 (0.137) | −0.26; 0.31 | 08814 |
| Smoking | 0.29 (0.518) | −0.76; 1.35 | 0.5687 |
| Maternal age | −0.39 (0.363) | −1.13; 0.35 | 0.2870 |
| Gravidity | −0.03 (0.341) | −0.73; 0.66 | 09208 |
| Caffeine consumption | −0.02 (0.003) | −0.01; 0.00 | 0.4480 |
| Vitamin D consumption | 0.00 (0.007) | −0.01; 0.02 | 0.9105 |
| Calcium consumption | −0.00 (0.000) | −0.00; 0.00 | 0.3271 |
| Sex | −0.30 (0.367) | −1.05; 0.44 | 0.4107 |
| Regression Beta Coefficient (SE) | 95% CI | p-Value | |
|---|---|---|---|
| Height at the age of 2 | 0.47 (0.308) | –0.16; 1.10 | 0.1361 |
| Maternal serum vitamin D concentration | 3.75 (2.237) | –0.81; 8.32 | 0.1038 |
| Cord blood vitamin D concentration | 0.19 (2.279) | –4.45; 4.83 | 0.9333 |
| Neonatal weight | 0.00 (0.002) | –0.00; 0.01 | 0.0582 |
| Pre-pregnancy body mass index: | |||
| underweight | 2.73 (2.809) | –2.99; 8.46 | 0.3385 |
| overweight/obesity | 3.33 (3.063) | –2.91; 9.58 | 0.2850 |
| Low weight gain vs. normal gain | 1.85 (2.450) | –3.15; 6.84 | 0.4577 |
| Excessive weight gain vs. normal gain | –1.07 (2.607) | –6.39; 4.24 | 0.6831 |
| Gestational age | –0.71 (0.654) | –2.04; 0.63 | 0.2873 |
| Smoking | 0.55 (2.460) | –4.47; 5.57 | 0.8244 |
| Maternal age | –1.68 (1.725) | –5.20; 1.84 | 0.3379 |
| Gravidity | 1.06 (1.657) | –11.07; −0.24 | 0.5275 |
| Gestational diabetes | –5.66 (2.654) | –3.17; 3.03 | 0.4188 |
| Caffeine consumption | 0.00 (0.018) | –0.03; 0.04 | 0.7561 |
| Vitamin D consumption | –0.00 (0.036) | –0.08; 0.07 | 0.9343 |
| Calcium consumption | –0.00 (0.001) | –0.00; 0.00 | 0.6920 |
| Sex | –2.96 (1.756) | –6.54; 0.61 | 0.1029 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wierzejska, R.E.; Wojda, B.K. Vitamin D Status during Pregnancy versus the Anthropometric Parameters of Two- and Four-Year-Olds: A Pilot Study. Nutrients 2022, 14, 254. https://doi.org/10.3390/nu14020254
Wierzejska RE, Wojda BK. Vitamin D Status during Pregnancy versus the Anthropometric Parameters of Two- and Four-Year-Olds: A Pilot Study. Nutrients. 2022; 14(2):254. https://doi.org/10.3390/nu14020254
Chicago/Turabian StyleWierzejska, Regina Ewa, and Barbara Katarzyna Wojda. 2022. "Vitamin D Status during Pregnancy versus the Anthropometric Parameters of Two- and Four-Year-Olds: A Pilot Study" Nutrients 14, no. 2: 254. https://doi.org/10.3390/nu14020254
APA StyleWierzejska, R. E., & Wojda, B. K. (2022). Vitamin D Status during Pregnancy versus the Anthropometric Parameters of Two- and Four-Year-Olds: A Pilot Study. Nutrients, 14(2), 254. https://doi.org/10.3390/nu14020254






