Assessment of Mediterranean Diet Adherence and Lifestyle Change during COVID-19 National Lockdown in Tunisian Adult Population
Abstract
1. Introduction
2. Subjects and Methods
2.1. Selection of Participants and Study Design
2.2. Questionnaire Design
2.3. Data Collection
2.4. Statistical Analyses
3. Results
3.1. Participant Characteristics
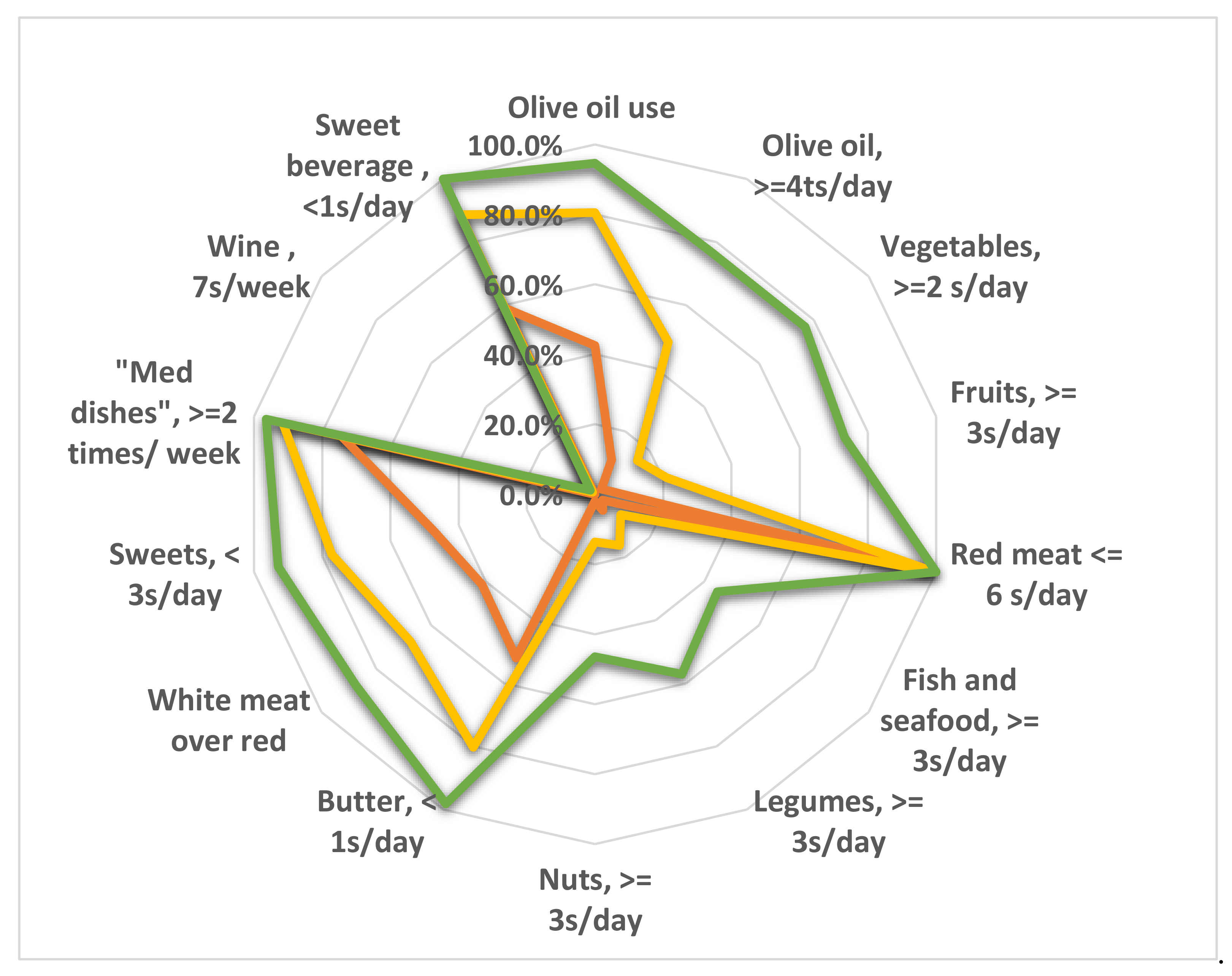
3.2. MD Adherence
3.3. Lifestyle Habits
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Questionnaire
| Questions | Answers |
|---|---|
| 1. How old are you? | Age in years |
| 2. Sex | Man/woman |
| 3. Nationality | Tunisian/other |
| 4. Place of residence (governorate) | governorate |
| 5. Instruction level | No schooling/primary schooling/secondary schooling/University graduate |
| 6. Occupational status | Unemployed/housewife/student/worker/intermediate executive/upper executive/retiree |
| 7. Number of people in the household | Number |
| 8. What type of housing does the household have? | Housing type |
| 9. Do you have electricity? | Yes/No |
| 10. What is the source of drinking water for the family members? | Source of drinking water |
| 11. Your status with regard to housing? | Owner/in ownership/renter/free accommodation with friends or relatives or company accommodation |
| 12. How many rooms (for sleeping) do you have in your home? | Number of rooms |
| 13. Do you have a refrigerator? | Yes/No |
| 14. Do you have a washing machine? | Yes/No |
| 15. Do you have a dishwasher? | Yes/No |
| 16. Do you have a satellite dish? | Yes/No |
| 17. Do you have internet access? | Yes/No |
| 18. Do you have a television? | Yes/No |
| 19. Do you have a central heating system? | Yes/No |
| 20. Do you have an air conditioner? | Yes/No |
| 21. Do you have a mobile phone? | Yes/No |
| 22. Do you have a car? | Yes/No |
| 23. Do you have a computer? | Yes/No |
| Questions | Answers |
|---|---|
| 1. Enter your weight (kg) as accurately as possible. | Weight in kg |
| 2. Enter your height (cm) as accurately as possible. | Height in cm |
| 3. Do you suffer from any chronic illness? If yes, quote, otherwise write No. | Yes/No |
| 4. Do you follow a special diet? If yes, specify, otherwise write No. | Yes/No |
| 5. Did you contract COVID-19? | No/Yes, tested positive with mild form of the disease/Yes, tested positive with severe form of the disease/suspected positive/contact case |
| 6. Have you experienced family death due to COVID-19? | Yes/No |
| 7. Have you had a vaccine against COVID-19? | Yes/No |
| Questions | Answers |
|---|---|
| 1. Is olive oil the main culinary fat used? | Yes/No |
| 2. How many teaspoons of olive oil do you consume per day (including that used for frying, salads, eating out, etc.)? | 4 or more/2 or 3/1 or less |
| 3. How many portions of vegetables (cooked and raw potatoes and beans are not included) do you eat per day? (One portion = half a large plate) | 3 or more/1 or 2/less than 1 |
| 4. How many servings of fresh fruit do you consume per day? (Serving size = one unit of medium-sized fruit, one large cup of sliced fruit, one slice of medium-sized melon/watermelon, or one cup of fresh juice) | 3 or more/1 or 2/less than 1 |
| 5. How many servings of red meat (veal, beef, mutton)/hamburgers/other meat products (salami, merguez, sausage…) do you consume per day? (One serving = 100 to 150 g = one quarter to half of a meal dish) | 1 or less/2 to 4/5 to 6/7 or more |
| 6. How many portions of butter, margarine or cream do you consume per day? (One portion = 12 g = one dessert spoon for butter and margarine, 2 tablespoons for cream) | Less than 1/one/more than 1 |
| 7. How much sugary drinks (industrial juices)/carbonated drinks/sodas do you consume per day? (One serving equals 330 mL) | Less than 1/1 or more |
| 8. How many glasses/cups of wine do you consume per week? | More than 14 glasses (more than 2 glasses per day)/7 to 14 glasses (1 or 2 glasses per day)/2 to 6 glasses (sometimes but not every day)/one glass or less (occasionally)/none |
| 9. How many portions of legumes (lentils, beans, chickpeas, peas…) do you consume per week? (One portion = 150 g = one dish or glass) | 3 or more/1 to 2/less than 1 |
| 10. How many portions of fish and seafood do you eat per week? (One portion = 100 to 150 g = a quarter to half of a meal dish) | 3 or more/1 to 2/less than 1 |
| 11. How many times a week do you consume industrial (not homemade) desserts/confectionery/pastries? (Including cakes, biscuits, ice cream, etc.) | Less than 1/1 to 2/3 or more |
| 12. How many servings of nuts (unsalted) do you consume per week? (Including unsalted peanuts, almonds, hazelnuts, walnuts, etc. One serving = 30 g = one handful) | 3 or more/1 to 2/less than 1 |
| 13. Do you prefer to consume chicken, turkey, or rabbit meat, or a vegetarian protein source, rather than red meat or derived products? | Yes/No |
| 14. How many times a week do you eat dishes cooked with tomatoes or tomato sauce, onion and/or garlic and olive oil? | Twice or more/once or less |
| Questions | Answers |
|---|---|
| 1. How many portions of pasta, rice, or other cereals including Oriental and Western pastries do you consume per day? | None/half portion/1 portion/2 portions/more than 2 portions |
| 2. How many servings of whole meal, cracked wheat, cooked wheat, and corn bread do you eat per day? (1 average serving = 80 g or 2 slices) | None/half portion/1 portion/2 portions/more than 2 portions |
| 3. How many servings of milk or yoghurt do you consume per day (1 serving = 150 mL in a cup or 125 g in a pot)? | None/half portion/1 portion/2 portions/more than 2 portions |
| 4. How many servings of cheese or dairy products do you consume per week (1 serving of dairy product = 100 g; 1 serving of ripened cheese = 50 g)? | None/half portion/1 portion/2 portions/more than 2 portions |
| 5. How many eggs do you consume per week? | None/1 egg/2 eggs/4 eggs/more than 4 eggs |
| 6. How much water did you drink per day during the third wave of the pandemic? | Less than 1 L/1 to 2 L/more than 2 L |
| Questions | Answers |
|---|---|
| 1. Did you smoke before COVID-19 (cigarettes, cigars, electronic cigarettes)? | No/Yes, fewer than 5 cigarettes/Yes, between 5 and 10 cigarettes/Yes, more than 10 cigarettes |
| 2. Do you currently smoke? | No/Yes, fewer than 5 cigarettes/Yes, between 5 and 10 cigarettes/Yes, more than 10 cigarettes |
| 3. Your sleeping habits before COVID-19? | Less than 7 h per night/7 h to 9 h per night/More than 9 h per night |
| 4. Your sleeping habits at present? | Less than 7 h per night/7 h to 9 h per night/More than 9 h per night |
| 5. Did you play any sport before COVID-19? | No/gymnastics, yoga, dance, aerobics/walking/swimming/football, basketball, volley, tennis/martial arts |
| 6. Do you currently play sports at home? | No/Yes, training without weights/Yes, weight training at home/yoga/treadmill/postural gymnastics/others |
| 7. How many times did you play sports during COVID-19? | I didn’t play sports/1 to 2 times per week/3 to 4 times per week/more than 4 times per week |
References
- World Health Organization. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(COVID-2019)-and-the-virus-that-causes-it (accessed on 3 August 2022).
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 3 August 2022).
- Atlas Magazine. Available online: https://www.atlas-mag.net/en/article/COVID-19-tunisia-records-highest-mortality-rate-in-africa (accessed on 3 August 2022).
- Ruktanonchai, N.W.; Floyd, J.; Lai, S.; Ruktanonchai, C.W.; Sadilek, A.; Rente-Lourenco, P.; Steele, J.J.S. Assessing the impact of coordinated COVID-19 exit strategies across Europe. Science 2020, 369, 1465–1470. [Google Scholar] [CrossRef] [PubMed]
- Turki, S.; Bouzekri, K.; Trabelsi, T.; EL Ati, J. Impact of COVID-19 lockdown on food habits, appetite and body weight in Tunisian adults. J. Nutr. Sci. 2022, 11, E60. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef] [PubMed]
- Saulle, R.; La Torre, G. The Mediterranean Diet, recognized by UNESCO as a cultural heritage of humanity. Ital. J. Pub. Health 2012, 7, 414–415. [Google Scholar]
- D’Innocenzo, S.; Biagi, C.; Lanari, M.J.N. Obesity and the Mediterranean diet: A review of evidence of the role and sustainability of the Mediterranean diet. Nutrients 2019, 11, 1306. [Google Scholar] [CrossRef] [PubMed]
- Romagnolo, D.F.; Selmin, O.I. Mediterranean Diet and Prevention of Chronic Diseases. Nutr. Today 2017, 52, 208–222. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, M.L.; García-Vigara, A.; Hidalgo-Mora, J.J.; García-Pérez, M.; Tarín, J.; Cano, A. Mediterranean diet and health: A systematic review of epidemiological studies and intervention trials. Maturitas 2020, 136, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health benefits of the Mediterranean diet: Metabolic and molecular mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Fíto, M.; Marrugat, J.; Covas, M.; Schröder, H. Investigators, RAH Adherence to the Mediterranean diet is associated with better mental and physical health. Br. J. Nut. 2009, 101, 1821–1827. [Google Scholar] [CrossRef]
- Greene, M.W.; Roberts, A.P.; Frugé, A.D. Negative association between Mediterranean diet adherence and COVID-19 cases and related deaths in Spain and 25 OECD countries: An ecological study. Front. Nutr. 2021, 8, 74. [Google Scholar] [CrossRef]
- Da Silva, R.; Bach-Faig, A.; Quintana, B.R.; Buckland, G.; de Almeida, M.D.V.; Serra-Majem, L.J. Worldwide variation of adherence to the Mediterranean diet, in 1961–1965 and 2000–2003. Pub. Health Nut. 2009, 12, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide adherence to Mediterranean diet between 1960 and 2011. Eur J Clin Nutr. 2019, 72 (Suppl. 1), 83–91. [Google Scholar] [CrossRef] [PubMed]
- Della Valle, P.G.; Mosconi, G.; Nucci, D.; Vigezzi, G.P.; Gentile, L.; Gianfredi, V.; Bonaccio, M.; Gianfagna, F.; Signorelli, C.; Iacoviello, L.; et al. Adherence to the Mediterranean Diet during the COVID-19 national lockdowns: A systematic review of observational studies. Acta Bio-Med. Atenei Parm. 2021, 92, e2021440. [Google Scholar]
- Worldometer. Available online: https://www.worldometers.info/world-population/tunisia-population/ (accessed on 3 August 2022).
- Checkmarket. Available online: https://fr.checkmarket.com/calculateur-taille-echantillon/#sample-size-margin-oferrorcalculator:%20entre%202000%20et%205400%20selon%20le%20sc%C3%A9nario%20en%207 (accessed on 23 April 2021).
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A Short Screener Is Valid for Assessing Mediterranean Diet Adherence among Older Spanish Men and Women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 14.0; StataCorp LLC: College Station, TX, USA, 2015. [Google Scholar]
- Medianet E-Business Digital Strategy. Available online: https://www.medianet.tn/fr/actualites/detail/profils-des-utilisateurs-des-reseaux-sociaux-en-tunisie-/all/1 (accessed on 11 August 2022).
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.J.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Sánchez, E.; Ramírez-Vargas, G.; Avellaneda-López, Y.; Orellana-Pecino, J.I.; García-Marín, E.; Díaz-Jimenez, J. Eating Habits and Physical Activity of the Spanish Population during the COVID-19 Pandemic Period. Nutrients 2020, 12, 2826. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López, M.D. Changes in Dietary Behaviours during the COVID-19 Outbreak Confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef]
- Giacalone, D.; Frøst, M.B.; Rodríguez-Pérez, C.J. Reported changes in dietary habits during the COVID-19 lockdown in the Danish population: The Danish COVIDiet study. Front. Nutr. 2020, 7, 294. [Google Scholar] [CrossRef]
- García-Conesa, M.-T.; Philippou, E.; Pafilas, C.; Massaro, M.; Quarta, S.; Andrade, V.; Dimitrova, D.J.N. Exploring the validity of the 14-item mediterranean diet adherence screener (Medas): A cross-national study in seven european countries around the mediterranean region. Nutrients 2020, 12, 2960. [Google Scholar] [CrossRef]
- Belhedi, A. Les Disparités Régionales en Tunisie. Défis et Enjeux. 2019. Available online: https://www.researchgate.net/publication/331384640_Les_disparites_regionales_en_Tunisie_Defis_et_enjeux#fullTextFileContent (accessed on 11 August 2022).
- Deconinck, K.; Avery, E.; Jackson, L.A.J.E. Food supply chains and COVID-19: Impacts and policy lessons. Eurochoices 2020, 19, 34–39. [Google Scholar] [CrossRef]
- ElKadhi, Z.; Elsabbagh, D.; Frija, A.; Lakoud, T.; Wiebelt, M.; Breisinger, C. The Impact of COVID-19 on Tunisia’s Economy, Agri-Food System, and Households; MENA Policy Note 5; International Food Policy Research Institute (IFPRI): Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- FAO. The Impact of COVID-19 on Fisheries and Aquaculture Food Systems, Possible Responses: Information Paper, November 2020; FAO: Rome, Italy, 2021. [Google Scholar] [CrossRef]
- Mahjoub, A.J.T.F. Pandémie COVID-19 en Tunisie: Les Inégalités, les Vulnérabilités à la Pauvreté et au Chômage. Forum Tunisien Pour les Droits Economiques et Sociaux. 2020. Available online: http://ftdes.net/rapports/COVID-AZ19.pdf (accessed on 11 August 2022).
- INS. Suivi de L’impact Socio-économique du COVID-19 sur les Ménages Tunisiens. Available online: http://www.ins.tn/sites/default/files/publication/pdf/Enq%20covid%20menages%20%20octobre%20202.pdf. (accessed on 11 August 2022).
- El Ati, J.; Traissac, P.; Doggui, R.; Verger, E.; Alouane, L.; Ben Gharbia, H.; Kefi, F.; TURKI, S.; Bahrini, A.; Dop, M.C. Towards the enhancement of the Mediterranean diet in the Mediterranean region. FAO 2019, unpublished work. [Google Scholar]
- National Institute of Statistics. Consumption and Living Standards. [Consommation et Niveau de Vie, in French]. Statistiques Tunisie. 2016. Available online: http://www.ins.nat.tn/sites/default/files/publication/pdf/Bulletin%20-cons-2016-fr2-2.pdf (accessed on 11 August 2022).
- Tong, T.Y.; Imamura, F.; Monsivais, P.; Brage, S.; Griffin, S.J.; Wareham, N.J.; Forouhi, N.G. Dietary cost associated with adherence to the Mediterranean diet, and its variation by socio-economic factors in the UK Fenland Study. Br. J. Nutr. 2018, 119, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Perez-Araluce, R.; Martinez-Gonzalez, M.; Fernández-Lázaro, C.; Bes-Rastrollo, M.; Gea, A.; Carlos, S.J.C.N. Mediterranean diet and the risk of COVID-19 in the ‘Seguimiento Universidad de Navarra’cohort. Clin. Nutr. 2021, ahead of print. [Google Scholar] [CrossRef]
- Calder, P.C.; Carr, A.C.; Gombart, A.F.; & Eggersdorfer, M.J.N. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients 2020, 12, 1181. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; the Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Gillies, C.L.; Singh, R.; Singh, A.; Chudasama, Y.; Coles, B.; Seidu, S.; Zaccardi, F.; Davies, M.J.; Khunti, K. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: A systematic review and meta-analysis. Diabetes Obes Metab. 2022, 22, 1915–1924. [Google Scholar] [CrossRef] [PubMed]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2022, 323, 1775–1776. [Google Scholar] [CrossRef]
- Yang, H.; Ma, J. How the COVID-19 pandemic impacts tobacco addiction: Changes in smoking behavior and associations with well-being. Addict. Behav. 2021, 119, 106917. [Google Scholar] [CrossRef]
- Bommele, J.; Hopman, P.; Walters, B.H.; Geboers, C.; Croes, E.; Fong, G.T.; Quah, A.; Willemsen, M. The double-edged relationship between COVID-19 stress and smoking: Implications for smoking cessation. Tob. Induc. Dis. 2020, 18, 63. [Google Scholar] [CrossRef]
- Fenollar-Cortés, J.; Jiménez, Ó.; Ruiz-García, A.; Resurrección, D.M. Gender differences in psychological impact of the confinement during the COVID-19 outbreak in Spain: A longitudinal study. Front. Psychol. 2021, 12, 682860. [Google Scholar] [CrossRef]
- Ingram, J.; Maciejewski, G.; Hand, C.J. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front. Psychol. 2020, 11, 588604. [Google Scholar] [CrossRef] [PubMed]
- Laberge, L.; Petit, D.; Simard, C.; Vitaro, F.; Tremblay, R.E.; Montplaisir, J. Development of sleep patterns in early adolescence. J. Sleep Res. 2001, 10, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Abouzid, M.; El-Sherif, D.M.; Eltewacy, N.K.; Dahman, N.B.H.; Okasha, S.A.; Ghozy, S.; Islam, S.M.S. Influence of COVID-19 on lifestyle behaviors in the Middle East and North Africa Region: A survey of 5896 individuals. J. Transl. Med. 2021, 19, 129. [Google Scholar] [CrossRef] [PubMed]
- López-Valenciano, A.; Suárez-Iglesias, D.; Sanchez-Lastra, M.A.; Ayán, C.J. Impact of COVID-19 pandemic on university students’ physical activity levels: An early systematic review. Front. Psychol. 2021, 11, 624567. [Google Scholar] [CrossRef]
- López-Bueno, R.; Calatayud, J.; Andersen, L.L.; Balsalobre-Fernández, C.; Casaña, J.; Casajús, J.A.; López-Sánchez, G.F.J.S. Immediate impact of the COVID-19 confinement on physical activity levels in Spanish adults. Sustainability 2020, 12, 5708. [Google Scholar] [CrossRef]
- Goethals, L.; Barth, N.; Guyot, J.; Hupin, D.; Celarier, T.; Bongue, B. Impact of Home Quarantine on Physical Activity among Older Adults Living at Home during the COVID-19 Pandemic: Qualitative Interview Study. JMIR Aging 2020, 3, e19007. [Google Scholar] [CrossRef]
| Total Population n (%) 1 | Women n (%) | Men n (%) | |
|---|---|---|---|
| 1082 (100.0) | 804 (74.3) | 278 (25.7) | |
| Location | p = 0.1922 | ||
| Greater Tunis | 482 (44.6) | 350 (43.5) | 132 (47.5) |
| Northeast | 154 (14.2) | 120 (14.9) | 34 (12.2) |
| Northwest | 93 (8.6) | 72 (9.0) | 21 (7.5) |
| Center-east | 195 (18.0) | 151 (18.8) | 44 (15.8) |
| Center-west | 44 (4.1) | 31 (3.9) | 13 (4.7) |
| Southeast | 90 (8.3) | 67 (8.3) | 23 (8.3) |
| Southwest | 24 (2.2) | 13 (1.6) | 11 (4.0) |
| Age category | p < 0.00012 | ||
| Young adult (20–25 years) | 339 (31.3) | 277 (34.4) | 62 (22.3) |
| Adults (25–60 years) | 691 (63.9) | 503 (62.6) | 188 (67.6) |
| Elderly (60 years and over) | 52 (4.8) | 24 (2.9) | 28 (10.1) |
| Education | p < 0.00012 | ||
| Not graduated | 4 (0.4) | 1 (0.1) | 3 (1.1) |
| Primary school graduation | 9 (0.8) | 6 (0.7) | 3 (1.1) |
| Secondary school graduation | 76 (7.0) | 37 (4.6) | 39 (14.0) |
| University graduation | 993 (91.8) | 760 (94.5) | 233 (83.8) |
| Occupational status | p < 0.00012 | ||
| Unemployed or housewife | 145 (13.4) | 131 (16.3) | 14 (0.5) |
| Student | 423 (39.1) | 346 (43.0) | 77 (27.7) |
| Worker | 71 (6.6) | 40 (5.0) | 31 (11.1) |
| Intermediate executive | 132 (12.2) | 84 (10.4) | 48 (17.3) |
| Upper executive | 272 (25.1) | 186 (23.1) | 86 (30.9) |
| Retiree | 39 (3.6) | 17 (2.1) | 39 (7.9) |
| Household size (n = 1059) 3 | p = 0.1082 | ||
| Living alone | 29 (2.7) | 17 (2.1) | 12 (4.3) |
| Small family (≤4 members) | 798 (73.8) | 604 (75.1) | 194 (69.8) |
| Large family (>4 members) | 232 (21.4) | 171 (21.3) | 61 (21.9) |
| Unspecified | 23 (2.1) | 12 (1.5) | 11 (4.0) |
| Household welfare proxy (n = 1059) 3 | p = 0.142 | ||
| Lower tertile | 351 (32.5) | 267 (33.2) | 84 (30.2) |
| Middle tertile | 353 (32.6) | 251 (31.2) | 102 (36.7) |
| Upper tertile | 355 (32.8) | 274 (34.0) | 81 (29.1) |
| Not declared | 23 (2.1) | 12 (1.4) | 11 (3.9) |
| Total Population n (%) 2 | Women n (%) | Men n (%) | ||||
|---|---|---|---|---|---|---|
| 1082 (100) | 804 (74.3) | 278 (25.7) | ||||
| Age (years) 1 | 32.5 | 12.0 | 31.1 | 10.8 | 36.5 | 14.2 |
| Weight (kg) 1 | 71.1 | 15.2 | 67.8 | 13.9 | 80.5 | 14.8 |
| Height (m) 1 | 1.68 | 0.08 | 1.64 | 0.06 | 1.77 | 0.06 |
| BMI (kg/m2) 1 | 25.1 | 4.9 | 25.0 | 5.0 | 25.4 | 4.4 |
| Nutritional status 2 | p = 0.20 3 | |||||
| Underweight | 60 (5.5) | 50 (6.2) | 10 (3.6) | |||
| Normal weight | 528 (48.8) | 396 (49.2) | 132 (47.5) | |||
| Preobese | 337 (31.1) | 241 (30.0) | 96 (34.5) | |||
| Obese | 157 (14.5) | 117 (14.6) | 40 (14.4) | |||
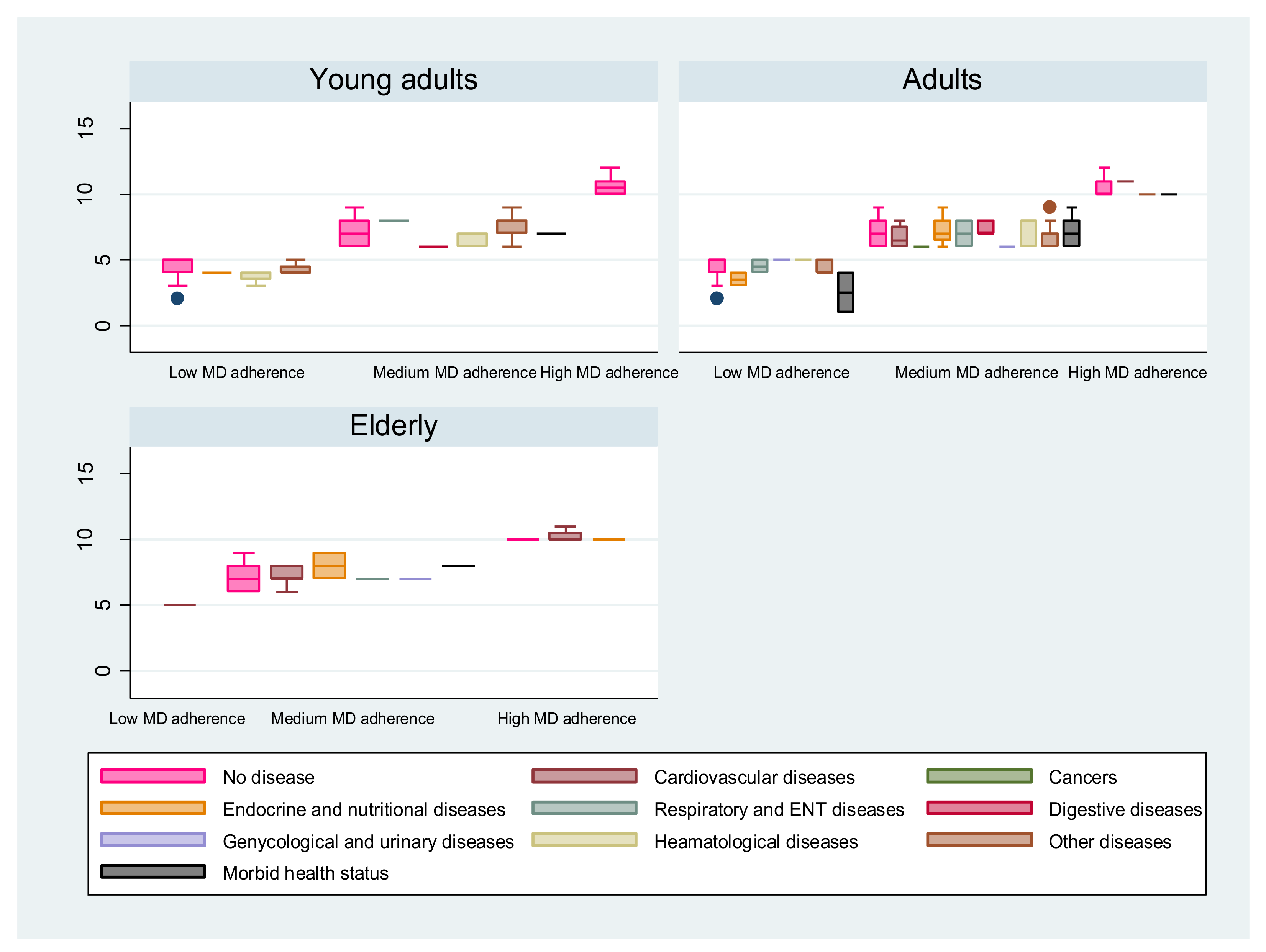
| History of chronic diseases (number of diseases) 2 | p = 0.203 | |||||
| No chronic disease | 852 (78.7) | 632 (78.6) | 220 (79.1) | |||
| One disease | 195 (18.0) | 143 (17.8) | 52 (18.7) | |||
| Multiple diseases | 35 (3.2) | 29 (3.6) | 6 (2.1) | |||
| History of chronic diseases (type of diseases) 2 | p = 0.0023 | |||||
| Cardiovascular diseases | 25 (10.9) | 14 (8.1) | 11 (19.0) | |||
| Endocrine, nutritional, or metabolic diseases | 56 (24.3) | 37 (21.5) | 19 (32.7) | |||
| Respiratory and ENT diseases | 14 (6.1) | 8 (4.6) | 6 (10.3) | |||
| Digestive diseases | 13 (5.7) | 12 (7.0) | 1 (1.7) | |||
| Hematological diseases | 26 (11.3) | 26 (15.1) | 0 (0.0) | |||
| Genecology, urinary and kidney diseases | 9 (3.9) | 5 (2.9) | 4 (6.8) | |||
| Cancer | 2 (0.9) | 2 (1.2) | 0 (0.0) | |||
| Other diseases | 50 (21.7) | 39 (22.7) | 11 (19.0) | |||
| Morbid health status (more than 3 diseases) | 35 (15.2) | 29 (16.9) | 6 (10.3) | |||
| Diet 2 | p = 0.0043 | |||||
| Spontaneous feeding with no diet | 960 (88.7) | 713 (88.7) | 247 (88.8) | |||
| Healthy diet | 23 (2.1) | 15 (3.2) | 8 (1.4) | |||
| Weight-loss diet | 34 (3.1) | 29 (3.6) | 5 (1.8) | |||
| Reduced sugar/salt diet | 20 (1.8) | 8 (1.0) | 12 (4.3) | |||
| Therapeutic diet | 13 (1.2) | 11 (1.4) | 2 (0.7) | |||
| Vegetarian diet | 2 (0.2) | 2 (0.2) | 0 (0.0) | |||
| Not specified | 30 (2.8) | 26 (3.2) | 4 (1.4) | |||
| Incidence of COVID-192 | p = 0.553 | |||||
| Not exposed | 734 (67.8) | 539 (67.0) | 195 (70.1) | |||
| Suspected infection | 168 (15.5) | 132 (16.4) | 36 (12.9) | |||
| Mid-form infection | 167 (15.4) | 124 (15.4) | 43 (15.5) | |||
| Severe form infection | 13 (1.2) | 9 (1.1) | 4 (1.4) | |||
| Occurrence of family death due to COVID-19 2 | p = 0.903 | |||||
| No | 886 (81.9) | 659 (82.0) | 227 (81.6) | |||
| Yes | 196 (18.1) | 145 (18.0) | 51 (18.4) | |||
| Vaccination against COVID-192 | p = 0.143 | |||||
| No | 847 (78.3) | 638 (79.3) | 209 (75.2) | |||
| Yes | 235 (21.7) | 166 (20.7) | 69 (24.8) | |||
| Item | MEDAS Score 1 | Proportion of MD Adherents n (%) 2 | ||
|---|---|---|---|---|
| Low Adherence | Medium Adherence | High Adherence | ||
| Total population (n = 1082) | 6.6 ± 1.07 7 [6-8] | 256 (23.7) | 770 (71.2) | 56 (5.2) |
| Sex (n = 806) 4 | Mann–Whitney test p = 0.24 3 | Chi-squared test p = 0.433 3 | ||
| Women | 6.6 ± 1.7 7 [6-8] | 145 (24.7) | 409 (69.8) | 32 (5.5) |
| Men | 6.5 ± 1.6 6 [6-7] | 50 (22.7) | 162 (73.6) | 8 (3.6) |
| Location (n = 806) 4 | Kruskal–Wallis test p = 0.028 3 | Chi-squared test p = 0.098 3 | ||
| Greater Tunis | 6.5 ± 1.7 6 [5-8] | 89 (25.2) | 249 (70.5) | 15 (4.2) |
| Northeast | 6.5 ± 1.9 6 [5-8] | 36 (28.8) | 83 (66.4) | 6 (4.8) |
| Northwest | 6.41 ± 1.4 6 [6-7] | 13 (19.4) | 53 (79.1) | 1 (1.5) |
| Center-east | 7.1 ± 1.8 7 [6-8] | 24 (17.5) | 99 (72.3) | 14 (10.2) |
| Center-west | 6.3 ± 1.5 7 [5-7] | 10 (27.8) | 26 (72.2) | 0 (0) |
| Southeast | 6.6 ± 1.5 7 [5-8] | 17 (25.7) | 47 (71.2) | 2 (3) |
| Southwest | 6.5 ± 1.8 6 [5-8] | 6 (27.3) | 14 (63.6) | 2 (9) |
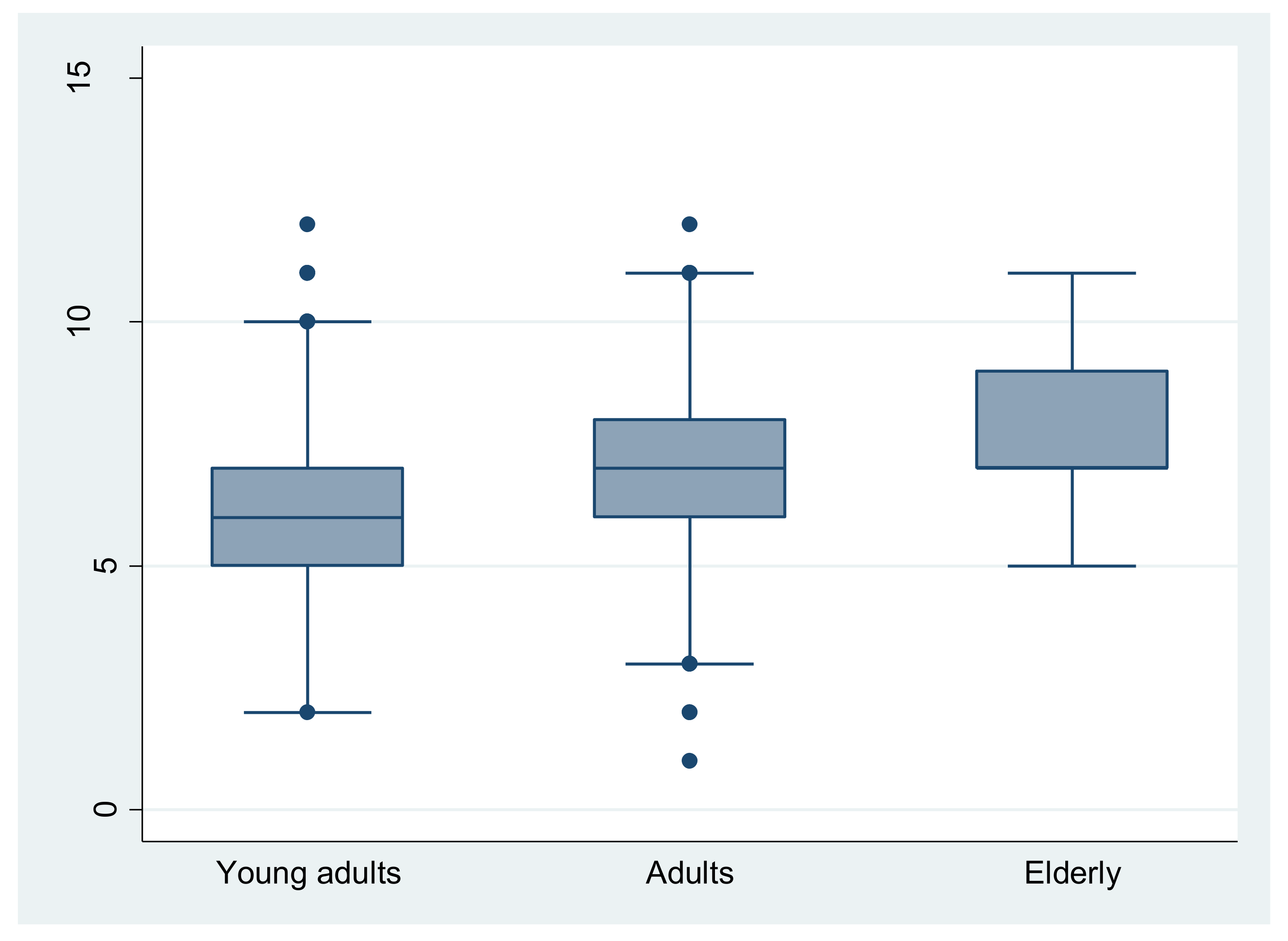
| Age category (n = 806) 4 | Kruskal–Wallis test p < 0.001 3 Spearman test (r = 0.15, p < 0.001) 3 | Chi-squared test p < 0.001 3 | ||
| Young adults (20–25 years) | 6.3 ± 1.7 6 [5-7] | 81 (30.6%) | 176 (66.4) | 8 (3) |
| Adults (25–60 years) | 6.7 ± 1.7 7 [6-8] | 113 (22.4%) | 366 (72.5) | 26 (5.1) |
| Elderly (over 60 years) | 7.7 ± 1.8 7 [7-9] | 1 (2.8%) | 29 (80.5) | 6 (16.6) |
| Education (n = 806) 4 | Kruskal–Wallis test p = 0.22 3 | Chi-squared test p = 0.768 3 | ||
| Not graduated | 7.7 ± 0.9 7.5 [7-8.5] | 0 (0) | 4 (100) | 0 (0) |
| Primary school graduation | 7.5 [5.5-8] | 2 (25) | 6 (75) | 0 (0) |
| Secondary school graduation | 6.3 ± 1.4 6 [6-7] | 12 (24.4) | 36 (73.5) | 1 (2) |
| University graduation | 6.6 ± 1.7 7 [6-8] | 181 (24.2) | 525 (70.5) | 39 (5.2) |
| Occupational status (n = 806) 4 | Kruskal–Wallis test (p = 0.015) 3 Spearman test (r = 0.11, p = 0.017) 3 | Chi-squared test p = 0.798 3 | ||
| Unemployed/housewife | 6.5 ± 1.5 6.5 [5-8] | 26 (26.5) | 70 (71.4) | 2 (2) |
| Student | 6.4 ± 1.8 6 [5-8] | 94 (29.3) | 213 (66.3) | 14 (4.3) |
| Worker | 6.3 ± 1.3 6 [6-7] | 14 (24.6) | 43 (75.4) | 0 (0) |
| Intermediate executive | 6.4 ± 1.5 6 [6-7] | 24 (24.7) | 71 (73.1) | 2 (2) |
| Upper executive | 7 ± 1.8 [6-8] | 36 (17.1) | 154 (73.3) | 20 (9.5) |
| Retiree | 7.4 ± 1.5 7 [7-8] | 1 (4.3) | 20 (86.9) | 2 (8.7) |
| Household size (n = 788) 5 | Kruskal–Wallis test p = 0.2 3 | Chi-squared test p = 0.079 3 | ||
| Living alone | 6.3 ± 1.1 6 [6-7] | 4 (21) | 15 (79) | 0 (0) |
| Small family (≤4 members) | 6.7 ± 1.7 6 [6-8] | 128 (21.6) | 433 (73) | 32 (5.4) |
| Large family (>4 members) | 6.4 ± 1.8 6.5 [6-8] | 55 (31.2) | 32 (64.8) | 7 (4) |
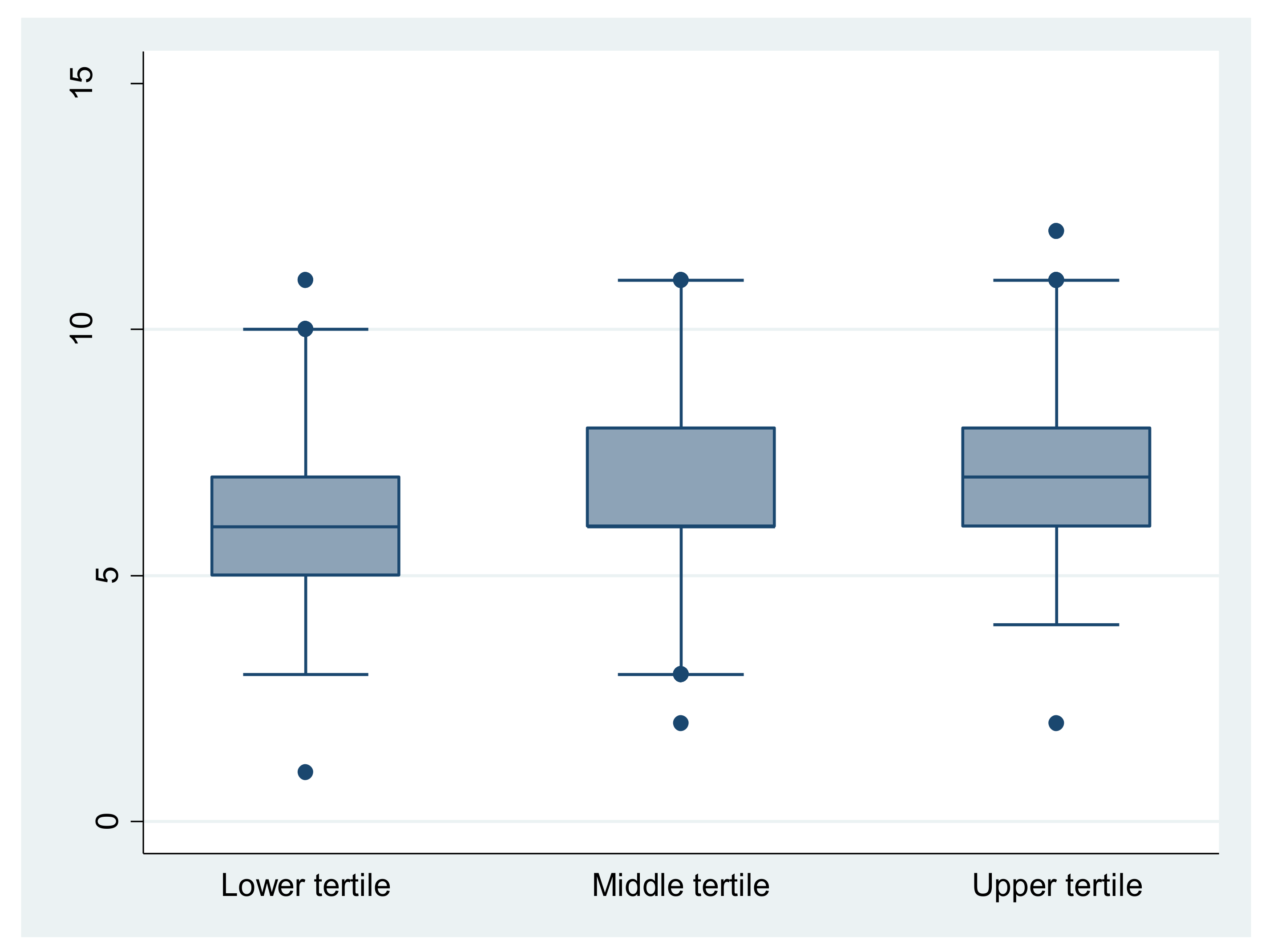
| Household welfare proxy (n = 788) 5 | Kruskal–Wallis test p < 0.001 3 Spearman test (r = 0.214, p <0.001) 3 | Chi-squared test p < 0.001 3 | ||
| Lower tertile | 6.17 ± 1.64 6 [5-7] | 87 (33.1) | 168 (63.9) | 8 (3) |
| Middle tertile | 6.55 ± 1.7 6 [6-8] | 66 (23.6) | 201 (71.8) | 13 (4.6) |
| Upper tertile | 7.11 ± 1.62 7 [6-8] | 34 (13.9) | 193 (78.8) | 18 (7.3) |
| Smoking Pre-COVID-19 | Smoking during COVID-19 | |
|---|---|---|
| Nonsmoking | 878 (81.2) 1 | 901 (83.2) |
| <5 cigarettes/day | 49 (4.5) | 37 (3.4) |
| 5–10 cigarettes/day | 44 (4.0) | 48 (4.4) |
| >10 cigarettes/day | 111 (10.2) | 96 (8.8) |
| Sleeping habits pre-COVID-19 | Sleeping habits during COVID-19 | |
| <7 h/night | 338 (31.2) 1 | 421 (38.9) |
| 7–9 h/night | 573 (53) | 499 (46.1) |
| >9 h/night | 171 (15.8) | 162 (15) |
| Sport Practiced Pre-COVID-19 | |
|---|---|
| None | 505 (46.7) 1 |
| Gym, yoga, dance, or aerobics | 105 (9.7) |
| Walking | 293 (27.1) |
| Swimming | 7 (0.6) |
| Football, basketball, volleyball, or tennis | 50 (4.6) |
| Martial arts | 14 (1.3) |
| Two activities | 95 (8.8) |
| Three activities or more | 13 (1.2) |
| Sport practiced during COVID-19 | |
| None | 810 (74.9) 1 |
| Gym, yoga, dance or aerobics | 22 (2) |
| Weightless training | 111(10) |
| Weight training at home | 33(3) |
| Treadmill | 16 (1.5) |
| Others | 52(4.8) |
| Two activities | 32(3) |
| Three activities or more | 6 (0.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turki, S.; Bouzekri, K.; Trabelsi, T.; El Ati, J. Assessment of Mediterranean Diet Adherence and Lifestyle Change during COVID-19 National Lockdown in Tunisian Adult Population. Nutrients 2022, 14, 4151. https://doi.org/10.3390/nu14194151
Turki S, Bouzekri K, Trabelsi T, El Ati J. Assessment of Mediterranean Diet Adherence and Lifestyle Change during COVID-19 National Lockdown in Tunisian Adult Population. Nutrients. 2022; 14(19):4151. https://doi.org/10.3390/nu14194151
Chicago/Turabian StyleTurki, Saoussen, Khaoula Bouzekri, Tarek Trabelsi, and Jalila El Ati. 2022. "Assessment of Mediterranean Diet Adherence and Lifestyle Change during COVID-19 National Lockdown in Tunisian Adult Population" Nutrients 14, no. 19: 4151. https://doi.org/10.3390/nu14194151
APA StyleTurki, S., Bouzekri, K., Trabelsi, T., & El Ati, J. (2022). Assessment of Mediterranean Diet Adherence and Lifestyle Change during COVID-19 National Lockdown in Tunisian Adult Population. Nutrients, 14(19), 4151. https://doi.org/10.3390/nu14194151







