The Diet Quality of Food-Insecure Australian Adults—A Nationally Representative Cross-Sectional Analysis
Abstract
1. Introduction
2. Materials and Methods
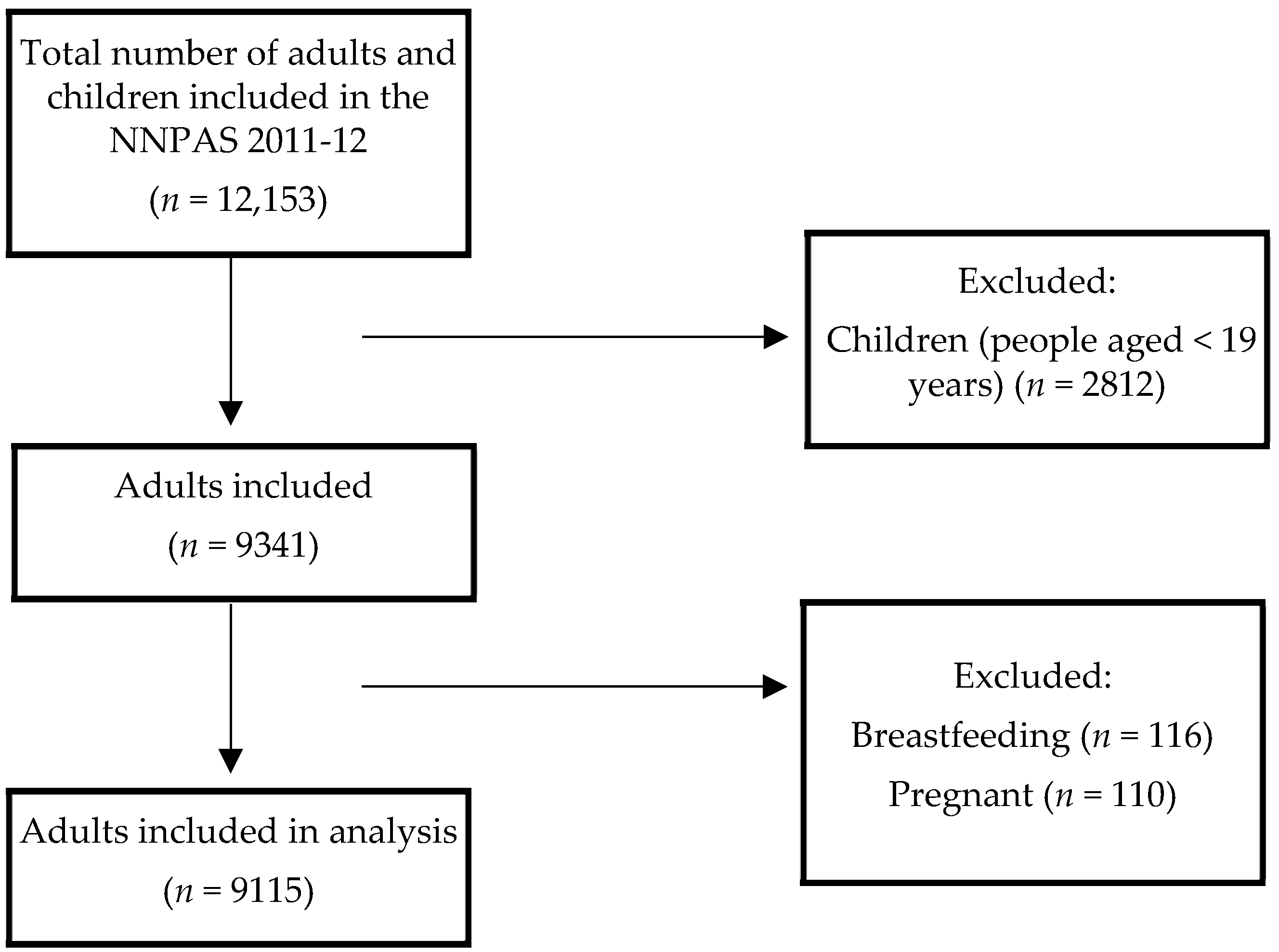
2.1. Study Design and Participants
2.2. Procedures
2.2.1. Food Security
2.2.2. Dietary Intake
2.2.3. Diet Quality
2.2.4. Sociodemographic and Health Characteristics
2.3. Analysis
2.4. General Procedure
3. Results
3.1. Socio-Demographic and Health Characteristics of Australian Adults by Food Security Status
3.2. Diet Quality Assessment Using the Dietary Guidelines Index (DGI)
3.3. Energy and Nutrient Intakes by Food Security Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- High Level Panel of Experts (HLPE). Impacts of COVID-19 on Food Security and Nutrition: Developing Effective Policy Responses to Address the Hunger and Malnutrition Pandemic Rome. 2020. Available online: http://www.fao.org/3/cb1000en/cb1000en.pdf (accessed on 3 August 2021).
- Food and Agriculture Organziation (FAO). The State of Food Insecurity in the World 2001 Rome: United Nations. 2001. Available online: https://www.fao.org/3/y1500e/y1500e00.htm (accessed on 15 August 2022).
- Food and Agriculture Organization (FAO). State of Food Security and Nutrition in the World—Table A1.1 Geneva: United Nations 2020. Available online: https://www.fao.org/3/ca9692en/online/ca9692en.html#chapter-a1_1 (accessed on 2 March 2022).
- Hanson, K.L.; Connor, L.M. Food insecurity and dietary quality in US adults and children: A systematic review. Am. J. Clin. Nutr. 2014, 100, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.W.; Tester, J.M. The Association between Food Insecurity and Diet Quality Varies by Race/Ethnicity: An Analysis of National Health and Nutrition Examination Survey 2011–2014 Results. J. Acad. Nutr. Diet. 2019, 119, 1676–1686. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.W.; Epel, E.S.; Ritchie, L.D.; Crawford, P.B.; Laraia, B.A. Food Insecurity Is Inversely Associated with Diet Quality of Lower-Income Adults. J. Acad. Nutr. Diet. 2014, 114, 1943–1953.e2. [Google Scholar] [CrossRef] [PubMed]
- Vaudin, A.; Moshfegh, A.; Sahyoun, N. Measuring Food Insecurity in Older Adults Using both Physical and Economic Food Access, NHANES 2013-18. J. Nutr. 2022, 152, 1953–1962. [Google Scholar] [CrossRef] [PubMed]
- Bocquier, A.; Vieux, F.; Lioret, S.; Dubuisson, C.; Caillavet, F.; Darmon, N. Socio-economic characteristics, living conditions and diet quality are associated with food insecurity in France. Public Health Nutr. 2015, 18, 2952–2961. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics (ABS). 4363.0.55.001—Australian Health Survey: Users’ Guide, 2011–2013; Australian Bureau of Statistics (ABS): Canberra, Australia, 2015.
- Machado, P.P.; Steele, E.M.; Levy, R.B.; Sui, Z.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ Open 2019, 9, e029544. [Google Scholar] [CrossRef] [PubMed]
- Marchese, L.; Livingstone, K.M.; Woods, J.L.; Wingrove, K.; Machado, P. Ultra-processed food consumption, socio-demographics and diet quality in Australian adults. Public Health Nutr. 2022, 25, 94–104. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics (ABS). 4727.0.55.005—Australian Aboriginal and Torres Strait Islander Health Survey: Nutrition Results—Food and Nutrients, 2012–2013; Australian Bureau of Statistics (ABS): Canberra, Australia, 2015. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/PrimaryMainFeatures/4727.0.55.005?OpenDocument (accessed on 24 May 2022).
- Food Standards Australia New Zealand (FSANZ). AUSNUT 2011–2013 Food Composition Database; FSANZ: Canberra, Australia, 2014. Available online: https://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/Pages/default.aspx (accessed on 24 May 2022).
- Thorpe, M.G.; Milte, C.M.; Crawford, D.; McNaughton, S.A. A Revised Australian Dietary Guideline Index and Its Association with Key Sociodemographic Factors, Health Behaviors and Body Mass Index in Peri-Retirement Aged Adults. Nutrients 2016, 8, 160. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16 College Station; StataCorp LLC: College Station, TX, USA, 2019; Available online: https://www.stata.com (accessed on 5 July 2022).
- Gamba, R.; Leung, C.W.; Guendelman, S.; Lahiff, M.; Laraia, B.A. Household Food Insecurity Is Not Associated with Overall Diet Quality Among Pregnant Women in NHANES 1999–2008. Matern. Child Health J. 2016, 20, 2348–2356. [Google Scholar] [CrossRef]
- Jia, J.; Fung, V.; Meigs, J.B.; Thorndike, A.N. Food Insecurity, Dietary Quality, and Health Care Utilization in Lower-Income Adults: A Cross-Sectional Study. J. Acad. Nutr. Diet. 2021, 121, 2177–2186. [Google Scholar] [CrossRef]
- Lachat, C.; Hawwash, D.; Ocké, M.C.; Berg, C.; Forsum, E.; Hörnell, A.; Larsson, C.L.; Sonestedt, E.; Wirfält, E.; Åkesson, A.; et al. Strengthening the Reporting of Observational Studies in Epidemiology-Nutritional Epidemiology (STROBE-nut): An Extension of the STROBE Statement. PLoS Med. 2016, 13, e1002036. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics (ABS). Australian Burden of Disease Study 2015: Dietary Risk Factors; ABS: Canberra, Australia, 2020. Available online: https://www.aihw.gov.au/reports/burden-of-disease/interactive-data-risk-factor-burden/contents/dietary-risk-factors (accessed on 20 July 2022).
- Booth, S.; Begley, A.; Mackintosh, B.; Kerr, D.A.; Jancey, J.; Caraher, M.; Whelan, J.; Pollard, C.M. Gratitude, resignation and the desire for dignity: Lived experience of food charity recipients and their recommendations for improvement, Perth, Western Australia. Public Health Nutr. 2018, 21, 2831–2841. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, R.; Lawrence, M.; Caraher, M. Kitchens and pantries—Helping or hindering? The perspectives of emergency food users in Victoria, Australia. J. Hunger. Environ. Nutr. 2017, 12, 26–45. [Google Scholar] [CrossRef]
- McKenzie, H.J.; McKay, F.H. Food as a discretionary item: The impact of welfare payment changes on low-income single mother’s food choices and strategies. J. Poverty Soc. Justice 2017, 25, 35–48. [Google Scholar] [CrossRef]
- Ramsey, R.; Giskes, K.; Turrell, G.; Gallegos, D. Food insecurity among adults residing in disadvantaged urban areas: Potential health and dietary consequences. Public Health Nutr. 2012, 15, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Elsahoryi, N.; Al-Sayyed, H.; Odeh, M.; McGrattan, A.; Hammad, F. Effect of COVID-19 on food security: A cross-sectional survey. Clin. Nutr. ESPEN 2020, 40, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.K.; Lammert, L.J.; Beverly, E.A. Food Insecurity and its Impact on Body Weight, Type 2 Diabetes, Cardiovascular Disease, and Mental Health. Curr. Cardiovasc. Risk Rep. 2021, 15, 15. [Google Scholar] [CrossRef]
- Vercammen, K.A.; Moran, A.J.; McClain, A.C.; Thorndike, A.N.; Fulay, A.P.; Rimm, E.B. Food Security and 10-Year Cardiovascular Disease Risk Among U.S. Adults. Am. J. Prev. Med. 2019, 56, 689–697. [Google Scholar] [CrossRef]
- Browne, N.T.; Cuda, S.E. Nutritional and activity recommendations for the child with normal weight, overweight, and obesity with consideration of food insecurity: An Obesity Medical Association (OMA) Clinical Practice Statement 2022. Obes. Pillars 2022, 2, 100012. [Google Scholar] [CrossRef]
- Temple, J.B.; Booth, S.; Pollard, C.M. Social Assistance Payments and Food Insecurity inAustralia: Evidence from the HouseholdExpenditure Survey. Int. J. Environ. Res. Public Health 2019, 16, 455. [Google Scholar] [CrossRef]
- Landrigan, T.J.; Kerr, D.A.; Dhaliwal, S.S.; Savage, V.; Pollard, C.M. Removing the Australian tax exemption on healthy food adds food stress to families vulnerable to poor nutrition. Aust. N. Z. J. Public Health 2017, 41, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.J.; Kane, S.; Ramsey, R.; Good, E.; Dick, M. Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia. BMC Public Health 2016, 16, 315. [Google Scholar] [CrossRef] [PubMed]
- Carey, R.; Caraher, M.; Lawrence, M.; Friel, S. Opportunities and challenges in developing a whole-of-government national food and nutrition policy: Lessons from Australia’s National Food Plan. Public Health Nutr. 2016, 19, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Public Health Association of Australia, Heart Foundation, Dietitians Australia, Red Cross, Indigenous Allied Health Australia, Victorian Aboriginal Community Controlled Health Organisation. Joint Policy Statement on: Food Security for Aboriginal & Torres Strait Islander Peoples. Canberra. 2019. Available online: https://www.phaa.net.au/documents/item/3824 (accessed on 10 September 2022).
- McKechnie, R.; Turrell, G.; Giskes, K.; Gallegos, D. Single-item measure of food insecurity used in the National Health Survey may underestimate prevalence in Australia. Aust. N. Z. J. Public Health 2018, 42, 389–395. [Google Scholar] [CrossRef]
- Beacom, E.; Furey, S.; Hollywood, L.; Humphreys, P. Investigating food insecurity measurement globally to inform practice locally: A rapid evidence review. Crit. Rev. Food Sci. Nutr. 2021, 61, 3319–3339. [Google Scholar] [CrossRef]
- Bastian, A.; Parks, C.; McKay, F.H.; van der Pligt, P.; Yaroch, A.; McNaughton, S.A.; Lindberg, R. Development of a Comprehensive Household Food Security Tool for Families with Young Children and/or Pregnant Women in High Income Countries. Int. J. Environ. Res. Public Health 2022, 19, 10543. [Google Scholar] [CrossRef]
- Subar, A.F.; Freedman, L.S.; Tooze, J.A.; Kirkpatrick, S.I.; Boushey, C.; Neuhouser, M.L.; Thompson, F.E.; Potischman, N.; Guenther, P.M.; Tarasuk, V.; et al. Addressing Current Criticism Regarding the Value of Self-Report Dietary Data. J Nutr. 2015, 145, 2639–2645. [Google Scholar] [CrossRef]
- Freedman, L.S.; Commins, J.M.; Moler, J.E.; Willett, W.; Tinker, L.F.; Subar, A.F.; Spiegelman, D.; Rhodes, D.; Potischman, N.; Neuhouser, M.L.; et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am. J. Epidemiol. 2015, 181, 473–487. [Google Scholar] [CrossRef]
| Characteristic | Food-Secure (95.6%) | Food-Insecure (4.4%) | p Value ^ | |
|---|---|---|---|---|
| Age, mean | Years | 46.9 (46.8, 47.1) | 39.9 (38.8, 41.6) | <0.001 |
| Sex, % | Male Female | 51.1 (50.7, 51.5) 48.9 (48.5, 49.3) | 38.4 (32.5, 44.8) 61.6 (55.2, 67.5) | <0.001 |
| Equivilised household income, % # | Below the poverty line Above the poverty line | 18.1 (17.0, 19.2) 81.9 (80.8, 83.0) | 44.7 (37.7, 51.7) 55.3 (48.3, 62.3) | <0.001 |
| Country of birth, % * | Australia English speaking Non-English speaking | 68.6 (66.9, 70.3) 11.7 (10.8, 12.6) 19.7 (18.1, 21.4) | 74.4 (67.7, 80.2) 10.0 (5.7, 17.0) 15.6 (10.5, 22.5) | 0.33 |
| Location, % ± | Major city Inner regional Outer regional/remote | 71.7 (70.5, 73.0) 19.0 (17.3, 20.8) 9.3 (7.8, 11.0) | 66.0 (59.6, 71.7) 24.0 (18.6, 30.3) 10.1 (6.8, 14.6) | 0.11 |
| Labour status, % | Employed Unemployed Not in labour force | 67.7 (66.3, 69.1) 2.3 (1.9, 2.9) 30.0 (28.8, 31.2) | 49.7 (42.7, 56.7) 9.4 (5.5, 15.6) 40.9 (34.4, 47.8) | <0.001 |
| Marital status, % | Married Not married | 60.1 (58.9, 61.3) 39.9 (38.7, 41.1) | 33.8 (27.0) 66.2 (58.7, 73.0) | <0.001 |
| Educational obtainment, % ^^ | Low Medium High | 25.4 (24.2, 26.5) 49.2 (47.6, 50.8) 25.5 (24.1, 26.9) | 37.9 (31.0, 45.4) 47.9 (40.3, 55.6) 14.2 (9.5, 20.7) | <0.001 |
| Body Mass Index, % ## | Underweight Normal weight Overweight Obese | 2.2 (1.7, 2.7) 34.0 (32.6, 35.4) 36.6 (35.1, 38.1) 27.2 (25.9, 28.6) | 2.9 (0.4, 5.4) 35.6 (28.8, 42.4) 27.5 (21.0, 33.9) 33.9 (27.5, 40.4) | 0.06 |
| Smoking status, % ** | Current smoker Ex-smoker Never smoked | 16.8 (15.7, 17.9) 31.4 (30.1, 32.8) 51.8 (50.3, 53.2) | 50.3 (42.6, 58.0) 23.8 (18.2, 30.5) 25.9 (20.8, 31.8) | <0.001 |
| DGI Component Mean Scores * | Food-Secure | Food-Insecure | Model 1—Group Differences (Minimally Adjusted) a | |
|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | B (95% CI) | p Value | |
| 1. Food variety | 2.3 (2.3, 2.3) | 1.6 (1.5, 1.8) | −0.54 (−0.72, −0.36) | <0.005 |
| 2. Fruit | 5.0 (4.9, 5.1) | 3.8 (3.1, 4.5) | −1.06 (−1.69, −0.43) | 0.001 |
| 3. Vegetables | 4.4 (4.3, 4.5) | 3.7 (3.2, 4.2) | −0.62 (−1.09, −0.15) | 0.010 |
| 4. Cereal (total) serves per day | 2.8 (2.8, 2.9) | 2.4 (2.2, 2.7) | −0.26 (−0.50, −0.03) | 0.026 |
| mostly wholegrain | 1.5 (1.4, 1.5) | 1.0 (0.8, 1.2) | −0.31 (−0.57, −0.05) | 0.021 |
| 5. Meat and alternatives (total) serves per day | 3.0 (2.9, 3.0) | 2.6 (2.3, 2.9) | −0.28 (−0.55, −0.01) | 0.045 |
| mostly lean | 4.5 (4.4, 4.5) | 4.5 (4.3, 4.6) | 0.01 (−0.18, 0.19) | 0.95 |
| 6. Dairy and alternatives (total) | 4.7 (4.6, 4.8) | 4.6 (4.1, 5.1) | −0.32 (−0.80, 0.16) | 0.19 |
| 7. Fluid intake (total) serves per day | 3.8 (3.7, 3.8) | 3.9 (3.6, 4.1) | −0.02 (−0.21, 0.18) | 0.87 |
| mostly water | 4.3 (4.3, 4.4) | 4.4 (4.2, 4.6) | −0.01 (−0.20, 0.17) | 0.90 |
| 8. Limit discretionary foods | 3.3 (3.1, 3.4) | 3.5 (2.8, 4.2) | 0.21 (−0.42, 0.84) | 0.51 |
| 9. Limit saturated fat mostly trimmed meat | 4.4 (4.4, 4.5) | 4.2 (3.9, 4.5) | −0.22 (−0.47, 0.03) | 0.08 |
| mostly low-fat milk | 3.8 (3.7, 3.9) | 3.7 (3.4, 4.0) | −0.02 (−0.33, 0.29) | 0.91 |
| 10. Moderate unsaturated fat | 8.2 (8.0, 8.3) | 8.7 (8.1, 9.3) | 0.60 (0.10, 1.09) | 0.018 |
| 11. Limit added salt during cooking | 2.6 (2.5, 2.6) | 2.5 (2.1, 2.8) | −0.02 (−0.34, 0.29) | 0.88 |
| at the table | 3.3 (3.2, 3.4) | 2.8 (2.5, 3.2) | −0.58 (−0.89, −0.27) | <0.001 |
| 12. Limit extra sugars | 6.6 (6.4, 6.7) | 6.5 (5.9, 7.0) | 0.13 (−0.49, 0.76) | 0.68 |
| 13. Limit alcohol | 8.5 (8.4, 8.6) | 8.5 (8.1, 9.0) | −0.20 (−0.71, 0.31) | 0.45 |
| TOTAL DGI SCORE | 76.8 (76.3, 77.3) | 72.8 (70.5, 75.2) | −3.52 (−5.57, −1.46) | 0.001 |
| Energy/Nutrient Mean | Food-Secure | Food-Insecure | Model 1—Group Differences (Minimally Adjusted) a | |
|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | B (95% CI) | p Value | |
| Energy intake (kJ/day) | 8694 (8589, 8800) | 8147 (7622, 8672) | −474.2 (−943.3, −5.1) | 0.048 |
| Protein intake (%E/day) | 18.5 (18.3, 18.6) | 17.2 (16.3, 18.1) | −1.24 (−2.09, −0.39) | 0.004 |
| Total fat (%E/day) | 30.9 (30.6, 31.1) | 30.0 (28.5, 31.4) | −1.13 (−2.42, 0.17) | 0.09 |
| Saturated fat intake (%E/day) | 12.1 (11.9, 12.2) | 12.1 (11.4, 12.8) | −0.01 (−0.74, 0.72) | 0.97 |
| Trans fat intake (%E/day) | 0.5 (0.6, 0.6) | 0.6 (0.5, 0.6) | 0.01 (−0.05, 0.07) | 0.81 |
| Mono-unsaturated fat intake (%E/day) | 11.8 (11.7, 12.0) | 11.2 (10.5, 11.9) | −0.73 (−1.37, −0.09) | 0.026 |
| Poly-unsaturated fat intake (%E/day) | 4.8 (4.7, 4.9) | 4.6 (4.2, 5.0) | −0.29 (−0.66, 0.08) | 0.13 |
| Carbohydrate intake (%E/day) | 43.3 (43.0, 43.6) | 45.6 (44.0, 47.2) | 2.03 (0.65, 3.41) | 0.004 |
| Total sugars intake (%E/day) | 19.0 (18.8, 19.3) | 21.8 (19.8, 23.8) | 2.55 (0.90, 4.21) | 0.003 |
| Fibre intake (g/MJ) | 23.0 (22.6, 23.4) | 20.1 (18.3, 21.8) | −2.29 (−3.81, −0.77) | 0.003 |
| Sodium intake (mg/MJ) | 2443 (2407, 2479) | 2321 (2152, 2490) | −136.7 (−321.6, 48.2) | 0.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lindberg, R.; McNaughton, S.A.; Abbott, G.; Pollard, C.M.; Yaroch, A.L.; Livingstone, K.M. The Diet Quality of Food-Insecure Australian Adults—A Nationally Representative Cross-Sectional Analysis. Nutrients 2022, 14, 4133. https://doi.org/10.3390/nu14194133
Lindberg R, McNaughton SA, Abbott G, Pollard CM, Yaroch AL, Livingstone KM. The Diet Quality of Food-Insecure Australian Adults—A Nationally Representative Cross-Sectional Analysis. Nutrients. 2022; 14(19):4133. https://doi.org/10.3390/nu14194133
Chicago/Turabian StyleLindberg, Rebecca, Sarah A. McNaughton, Gavin Abbott, Christina M. Pollard, Amy L. Yaroch, and Katherine M. Livingstone. 2022. "The Diet Quality of Food-Insecure Australian Adults—A Nationally Representative Cross-Sectional Analysis" Nutrients 14, no. 19: 4133. https://doi.org/10.3390/nu14194133
APA StyleLindberg, R., McNaughton, S. A., Abbott, G., Pollard, C. M., Yaroch, A. L., & Livingstone, K. M. (2022). The Diet Quality of Food-Insecure Australian Adults—A Nationally Representative Cross-Sectional Analysis. Nutrients, 14(19), 4133. https://doi.org/10.3390/nu14194133









