SMOFlipid Impact on Growth and Neonatal Morbidities in Very Preterm Infants
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Follow-Up
2.4. Study Outcome
2.5. Definitions
2.5.1. Nutrition Protocol
2.5.2. Growth Anthropometry
2.5.3. Preterm Neonatal Morbidities
2.6. Statistical Analysis
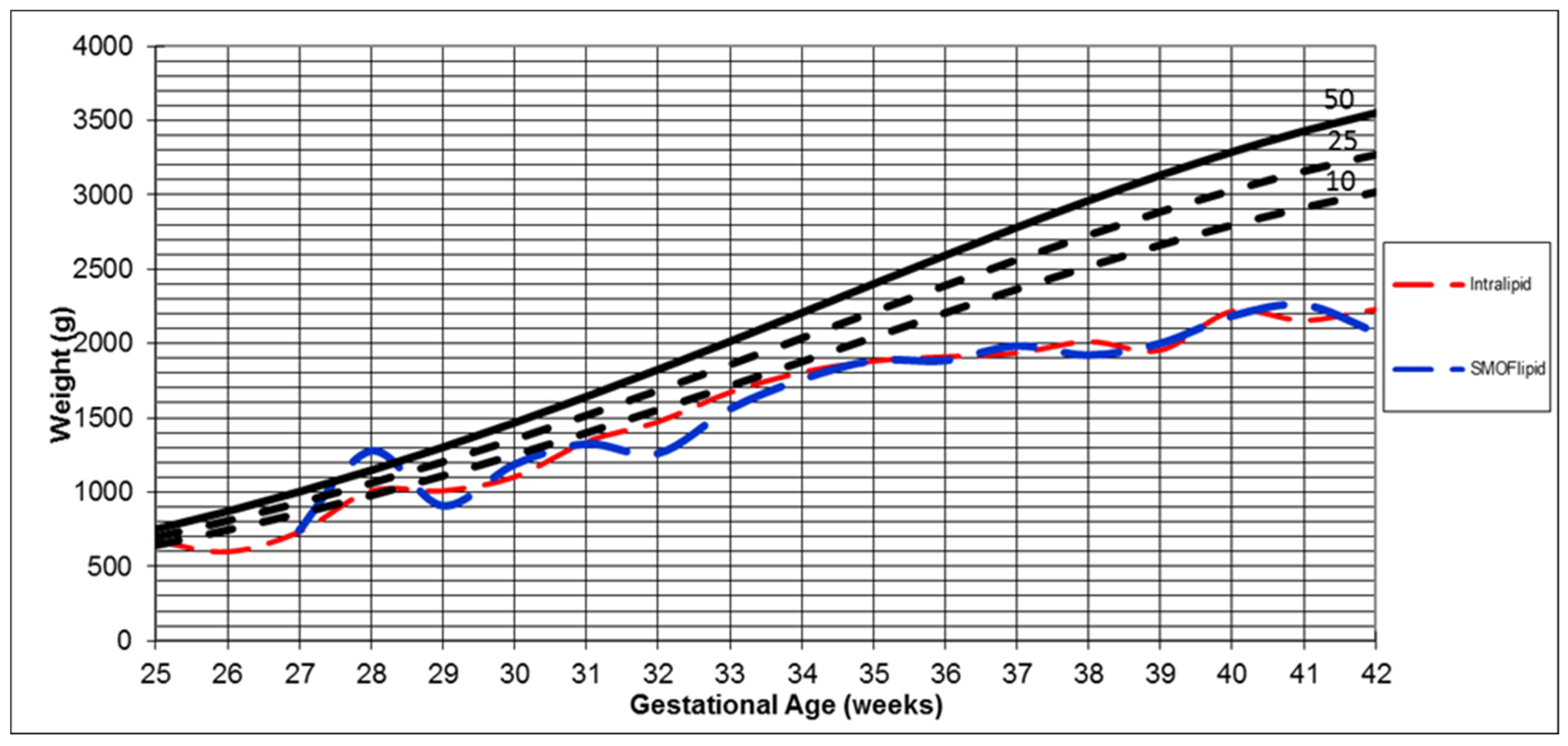
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heird, W.C.; Driscoll, J.M.; Schullinger, J.N.; Grebin, B.; Winters, R.W. Intravenous alimentation in pediatric patients. J. Pediatr. 1972, 80, 351–372. [Google Scholar] [CrossRef]
- Christensen, R.D.; Henry, E.; Kiehn, T.I.; Street, J.L. Pattern of daily weights among low birth weight neonates in the neonatal intensive care unit: Data from a multihospital health-care system. J. Perinatol. 2005, 26, 37–43. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Embleton, N.D.; Simmer, K. Practice of Parenteral Nutrition in VLBW and ELBW Infants. Nutr. Care Preterm Infants 2014, 110, 177–189. [Google Scholar]
- Salas-Salvadó, J.; Molina, J.; Figueras, J.; Massó, J.; Martí-Henneberg, C.; Jimenez, R. Effect of the Quality of Infused Energy on Substrate Utilization in the Newborn Receiving Total Parenteral Nutrition. Pediatr. Res. 1993, 33, 112–117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lapillonne, A.; Mis, N.F.; Goulet, O.; van den Akker, C.H.V.D.; Wu, J.; Koletzko, B.; Braegger, C.; Bronsky, J.; Cai, W.; Campoy, C.; et al. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Lipids. Clin. Nutr. 2018, 37, 2324–2336. [Google Scholar] [CrossRef] [PubMed]
- Rangel, S.J.; Calkins, C.M.; Cowles, R.A.; Barnhart, D.C.; Huang, E.Y.; Abdullah, F.; Arca, M.J.; Teitelbaum, D.H. Parenteral nutrition–associated cholestasis: An American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J. Pediatr. Surg. 2012, 47, 225–240. [Google Scholar] [CrossRef]
- Lacaille, F.; Gupte, G.; Colomb, V.; D’Antiga, L.; Hartman, C.; Hojsak, I.; Kolacek, S.; Puntis, J.; Shamir, R. Intestinal failure-associated liver disease: A position paper of the ESPGHAN Working Group of intestinal failure and intestinal transplantation. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 272–283. [Google Scholar] [CrossRef]
- Calder, P.C.; Adolph, M.; Deutz, N.E.; Grau, T.; Innes, J.K.; Klek, S.; Lev, S.; Mayer, K.; Michael-Titus, A.T.; Pradelli, L.; et al. Lipids in the intensive care unit: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2018, 37, 1–18. [Google Scholar] [CrossRef]
- Waitzberg, D.L.; Torrinhas, R.S.; Jacintho, T.M. New Parenteral Lipid Emulsions for Clinical Use. J. Parenter. Enter. Nutr. 2006, 30, 351–367. [Google Scholar] [CrossRef]
- Xu, X.-T.; Huang, H.; Tian, M.-X.; Hu, R.-C.; Dai, Z.; Jin, X. A four-oil intravenous lipid emulsion improves markers of liver function, triglyceride levels and shortens length of hospital stay in adults: A systematic review and meta-analysis. Nutr. Res. 2021, 92, 1–11. [Google Scholar] [CrossRef]
- Osowska, S.; Kunecki, M.; Sobocki, J.; Tokarczyk, J.; Majewska, K.; Omidi, M.; Radkowski, M.; Fisk, H.L.; Calder, P.C. Effect of changing the lipid component of home parenteral nutrition in adults. Clin. Nutr. 2018, 38, 1355–1361. [Google Scholar] [CrossRef]
- Ho, B.E.; Chan, S.C.; Faino, A.V.; Mortensen, M.; Williamson, N.; Javid, P.J.; Horslen, S.P.; Wendel, D. Evaluation of SMOFlipid in pediatric intestinal-failure patients and its effects on essential fatty acid levels. J. Parenter. Enter. Nutr. 2021, 45, 546–552. [Google Scholar] [CrossRef]
- Goulet, O.; Antébi, H.; Wolf, C.; Talbotec, C.; Alcindor, L.G.; Corriol, O.; Lamor, M.; Colomb-Jung, V. A new intravenous fat emulsion containing soybean oil, medium-chain triglycerides, olive oil, and fish oil: A single-center, double-blind randomized study on efficacy and safety in pediatric patients receiving home parenteral nutrition. J. Parenter. Enter. Nutr. 2010, 34, 485–495. [Google Scholar] [CrossRef]
- Ozkan, H.; Köksal, N.; Dorum, B.A.; Kocael, F.; Ozarda, Y.; Bozyigit, C.; Doğan, P.; Varal, I.G.; Bagci, O. New-generation fish oil and olive oil lipid for prevention of oxidative damage in preterm infants: Single center clinical trial at university hospital in Turkey. Pediatr. Int. 2019, 61, 388–392. [Google Scholar] [CrossRef]
- Ndiaye, A.B.; Mohamed, I.; Pronovost, E.; Angoa, G.; Piedboeuf, B.; Lemyre, B.; Afifi, J.; Qureshi, M.; Sériès, T.; Guillot, M.; et al. Use of SMOF lipid emulsion in very preterm infants does not affect the incidence of bronchopulmonary dysplasia–free survival. J. Parenter. Enter. Nutr. 2022. [Google Scholar] [CrossRef]
- Najm, S.; Löfqvist, C.; Hellgren, G.; Engström, E.; Lundgren, P.; Hård, A.-L.; Lapillonne, A.; Sävman, K.; Nilsson, A.K.; Andersson, M.X.; et al. Effects of a lipid emulsion containing fish oil on polyunsaturated fatty acid profiles, growth and morbidities in extremely premature infants: A randomized controlled trial. Clin. Nutr. ESPEN 2017, 20, 17–23. [Google Scholar] [CrossRef]
- Belza, C.; Wales, J.C.; Courtney-Martin, G.; Silva, N.; Avitzur, Y.; Wales, P.W. An Observational Study of Smoflipid vs Intralipid on the Evolution of Intestinal Failure–Associated Liver Disease in Infants With Intestinal Failure. J. Parenter. Enter. Nutr. 2019, 44, 688–696. [Google Scholar] [CrossRef]
- Vlaardingerbroek, H.; Vermeulen, M.; Carnielli, V.P.; Vaz, F.; Akker, C.V.D.; van Goudoever, J.B. Growth and Fatty Acid Profiles of VLBW Infants Receiving a Multicomponent Lipid Emulsion From Birth. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 417–427. [Google Scholar] [CrossRef]
- Rayyan, M.; Devlieger, H.; Jochum, F.; Allegaert, K. Short-term use of parenteral nutrition with a lipid emulsion containing a mixture of soybean oil, olive oil, medium-chain triglycerides, and fish oil: A randomized double-blind study in preterm infants. J. Parenter. Enter. Nutr. 2012, 36, 81S–94S. [Google Scholar] [CrossRef]
- Hill, N.S.; Cormack, B.E.; Little, B.S.; Bloomfield, F.H. Growth and Clinical Outcome in Very Low-Birth-Weight Infants After the Introduction of a Multicomponent Intravenous Lipid Emulsion. J. Parenter. Enter. Nutr. 2020, 44, 1318–1327. [Google Scholar] [CrossRef]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef]
- Papile, L.-A.; Burstein, J.; Burstein, R.; Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1500 gm. J. Pediatr. 1978, 92, 529–534. [Google Scholar] [CrossRef]
- Walsh, M.C.; Wilson-Costello, D.; Zadell, A.; Newman, N.; Fanaroff, A. Safety, Reliability, and Validity of a Physiologic Definition of Bronchopulmonary Dysplasia. J. Perinatol. 2003, 23, 451–456. [Google Scholar] [CrossRef]
- Bell, M.J.; Ternberg, J.L.; Feigin, R.D.; Keating, J.P.; Marshall, R.; Barton, L.; Brotherton, T. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 1978, 187, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Speer, C.P. Late-onset neonatal sepsis: Recent developments. Arch. Dis. Child. Fetal Neonatal Ed. 2015, 100, F257e63. [Google Scholar] [CrossRef] [PubMed]
- International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch. Ophthalmol. 2005, 123, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Ronald, E.; Kleinman, F.R.G. American Academy of Pediatrics Committee on Nutrition, American Academy of Pediatrics. 2014. Available online: https://www.ncbi.nlm.nih.gov/nlmcatalog/101653189 (accessed on 15 July 2022).
- Tomsits, E.; Pataki, M.; Tölgyesi, A.; Fekete, G.; Rischak, K.; Szollár, L. Safety and efficacy of a lipid emulsion containing a mixture of soybean oil, medium-chain triglycerides, olive oil, and fish oil: A randomised, double-blind clinical trial in preterm infants requiring parenteral nutrition. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Ryan, A.S.; Montalto, M.B.; Groh-Wargo, S.; Mimouni, F.; Sentipal-Walerius, J.; Doyle, J.; Siegman, J.S.; Thomas, A.J. Effect of DHA-containing formula on growth of preterm infants to 59 weeks postmenstrual age. Am. J. Hum. Biol. 1999, 11, 457–467. [Google Scholar] [CrossRef]
- Carlson, S.E.; Werkman, S.H.; Tolley, E.A. Effect of long-chain n-3 fatty acid supplementation on visual acuity and growth of preterm infants with and without bronchopulmonary dysplasia. Am. J. Clin. Nutr. 1996, 63, 687–697. [Google Scholar] [CrossRef]
- Koletzko, B.; Carlson, S.E.; van Goudoever, J.B. Should infant formula provide both Omega-3 DHA and Omega-6 arachidonic acid? Ann. Nutr. Metab. 2015, 66, 137–138. [Google Scholar] [CrossRef]
- Martinez, M. Tissue levels of polyunsaturated fatty acids during early human development. J. Pediatr. 1992, 120, S129–S138. [Google Scholar] [CrossRef]
- Guillot, M.; Synnes, A.; Pronovost, E.; Qureshi, M.; Daboval, T.; Caouette, G.; Olivier, F.; Bartholomew, J.; Mohamed, I.; Massé, E.; et al. Maternal High-Dose DHA Supplementation and Neurodevelopment at 18–22 Months of Preterm Children. Pediatrics 2022, 150, e2021055819. [Google Scholar] [CrossRef]
- Vlaardingerbroek, H.; Veldhorst, M.A.B.; Spronk, S.; Akker, C.V.D.; van Goudoever, J.B. Parenteral lipid administration to very-low-birth-weight infants—Early introduction of lipids and use of new lipid emulsions: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2012, 96, 255–268. [Google Scholar] [CrossRef]
- Krohn, K.; Koletzko, B. Parenteral lipid emulsions in paediatrics. Curr. Opin. Clin. Nutr. Metab. Care 2006, 9, 319–323. [Google Scholar] [CrossRef]
- Wanten, G.J. Parenteral lipids in nutritional support and immune modulation. Clin. Nutr. Suppl. 2009, 4, 13–17. [Google Scholar] [CrossRef]
- Hsieh, A.T.; Anthony, J.C.; Diersen-Schade, D.A.; Rumsey, S.C.; Lawrence, P.; Li, C.; Nathanielsz, P.W.; Brenna, J.T. The Influence of Moderate and High Dietary Long Chain Polyunsaturated Fatty Acids (LCPUFA) on Baboon Neonate Tissue Fatty Acids. Pediatr. Res. 2007, 61, 537–545. [Google Scholar] [CrossRef]
- Martin, C.R.; DaSilva, D.A.; Cluette-Brown, J.E.; DiMonda, C.; Hamill, A.; Bhutta, A.Q.; Coronel, E.; Wilschanski, M.; Stephens, A.J.; Driscoll, D.F.; et al. Decreased Postnatal Docosahexaenoic and Arachidonic Acid Blood Levels in Premature Infants are Associated with Neonatal Morbidities. J. Pediatr. 2011, 159, 743–749.e2. [Google Scholar] [CrossRef]
- Ma, L.; Li, N.; Liu, X.; Shaw, L.; Calzi, S.L.; Grant, M.B.; Neu, J. Arginyl-glutamine dipeptide or docosahexaenoic acid attenuate hyperoxia-induced lung injury in neonatal mice. Nutrition 2012, 28, 1186–1191. [Google Scholar] [CrossRef]
- Velten, M.; Britt, R.D., Jr.; Heyob, K.M.; Tipple, T.E.; Rogers, L.K. Maternal dietary docosahexaenoic acid supplementation attenuates fetal growth restriction and enhances pulmonary function in a newborn mouse model of perinatal inflammation. J. Nutr. 2014, 144, 258–266. [Google Scholar] [CrossRef]
- Rogers, L.K.; Valentine, C.J.; Pennell, M.; Velten, M.; Britt, R.D.; Dingess, K.; Zhao, X.; Welty, S.E.; Tipple, T.E. Maternal Docosahexaenoic Acid Supplementation Decreases Lung Inflammation in Hyperoxia-Exposed Newborn Mice. J. Nutr. 2010, 141, 214–222. [Google Scholar] [CrossRef]
- Blanco, P.G.; Freedman, S.D.; Lopez, M.C.; Ollero, M.; Comen, E.; Laposata, M.; Alvarez, J.G. Oral docosahexaenoic acid given to pregnant mice increases the amount of surfactant in lung and amniotic fluid in preterm fetuses. Am. J. Obstet. Gynecol. 2004, 190, 1369–1374. [Google Scholar] [CrossRef]
- Manley, B.J.; Makrides, M.; Collins, C.T.; McPhee, A.J.; Gibson, R.A.; Ryan, P.; Sullivan, T.R.; Davis, P.G.; DINO Steering Committee. High-Dose Docosahexaenoic Acid Supplementation of Preterm Infants: Respiratory and Allergy Outcomes. Pediatrics 2011, 128, e71–e77. [Google Scholar] [CrossRef]
- Collins, C.T.; Makrides, M.; McPhee, A.J.; Sullivan, T.R.; Davis, P.G.; Thio, M.; Simmer, K.; Rajadurai, V.S.; Travadi, J.; Berry, M.J.; et al. Docosahexaenoic Acid and Bronchopulmonary Dysplasia in Preterm Infants. N. Engl. J. Med. 2017, 376, 1245–1255. [Google Scholar] [CrossRef]
- Marc, I.; Piedboeuf, B.; Lacaze-Masmonteil, T.; Fraser, W.; Mâsse, B.; Mohamed, I.; Qureshi, M.; Afifi, J.; Lemyre, B.; Caouette, G.; et al. Effect of maternal docosahexaenoic acid supplementation on bronchopulmonary dysplasia-free survival in breastfed preterm infants: A randomized clinical trial. JAMA 2020, 324, 157–167. [Google Scholar] [CrossRef]
- Wang, Q.; Zhou, B.; Cui, Q.; Chen, C. Omega-3 Long-chain Polyunsaturated Fatty Acids for Bronchopulmonary Dysplasia: A Meta-analysis. Pediatrics 2019, 144, e20190181. [Google Scholar] [CrossRef]
- Tanaka, K.; Tanaka, S.; Shah, N.; Ota, E.; Namba, F. Docosahexaenoic acid and bronchopulmonary dysplasia in preterm infants: A systematic review and meta-analysis. J. Matern. Fetal. Neonatal. Med. 2022, 35, 1730–1738. [Google Scholar] [CrossRef]
- Alshaikh, B. SMOFlipid and Incidence of BPD in Preterm Infants. 2022. Available online: https://clinicaltrialsgov/ct2/show/NCT04078906 (accessed on 15 July 2022).
- Vayalthrikkovil, S.; Bashir, R.A.; Rabi, Y.; Amin, H.; Spence, J.-M.; Robertson, H.L.; Lodha, A. Parenteral Fish-Oil Lipid Emulsions in the Prevention of Severe Retinopathy of Prematurity: A Systematic Review and Meta-Analysis. Am. J. Perinatol. 2017, 34, 705–715. [Google Scholar] [CrossRef]

| Variable | N | Intralipid (n = 620) | SMOFlipid (n = 238) | p Value |
|---|---|---|---|---|
| Gestational age (weeks), median (IQR) | 858 | 29 (27.0–30.8) | 29 (27.0–31.0) | 0.12 |
| Birth weight (grams), (IQR) | 858 | 1100 (875–1344) | 1100 (870–1310) | 0.40 |
| Length (cm), median (IQR) | 858 | 37 (34–39) | 37 (33–39) | 0.4 |
| Head circumference (cm), (IQR) | 858 | 26 (24–28) | 27 (24–28) | 0.25 |
| Small for gestational age, n (%) | 858 | 38 (6.1) | 22 (9.2) | 0.13 |
| 1 min Apgar score, median (IQR) | 858 | 5 (3–6) | 6 (4–7) | 0.006 * |
| 5 min Apgar score, median (IQR) | 858 | 7 (6–8) | 7 (7–8) | <0.001 * |
| Male, n (%) | 858 | 320 (51.6) | 126 (52.7) | 0.82 |
| Antenatal steroid treatment, n (%) | 858 | 329 (53.1) | 130 (54.4) | 0.76 |
| Gestational diabetes mellitus, n (%) | 858 | 27 (4.4) | 14 (5.9) | 0.37 |
| Maternal hypertension, n (%) | 858 | 146 (23.5) | 62 (25.9) | 0.48 |
| Preterm rupture of membrane, n (%) | 858 | 77 (12.4) | 18 (8) | 0.08 |
| Cesarean section, n (%) | 858 | 251 (40.5) | 169 (70.7) | <0.001 * |
| Inotropes (dopamine, dobutamine, epinephrine, milrinone), n (%) | 858 | 237 (38.2) | 104 (43.5) | 0.16 |
| Hydrocortisone, n (%) | 858 | 124 (20) | 53 (22.2) | 0.51 |
| Omeprazole, n (%) | 858 | 66 (10.6) | 19 (7.9) | 0.25 |
| Noninvasive respiratory support, n (%) | 858 | 519 (83.7) | 207 (86.6) | 0.34 |
| Respiratory distress syndrome required surfactant, n (%) | 858 | 380 (61.3) | 174 (72.8) | 0.001 * |
| Mechanical ventilation, n (%) | 858 | 426 (68.7) | 187 (78.2) | 0.005 * |
| Patent ductus arteriosus required treatment, n (%) | 858 | 49 (7.9) | 25 (10.5) | 0.23 |
| Peripherally inserted central catheter (PICC), n (%) | 858 | 196 (31.6) | 100 (41.8) | 0.005 * |
| Corrected gestational age at discharge | 661 | 36 (34-38) | 36 (33-38) | 0.55 |
| Variable | N | Intralipid (n = 620) | SMOFlipid (n = 238) | p Value |
|---|---|---|---|---|
| Parenteral nutrition | ||||
| Duration of parenteral nutrition (days), median (IQR) | 858 | 16 (8–32) | 13 (7–26) | 0.14 |
| Duration of parenteral lipid (days), median (IQR) | 858 | 7 (5–7) | 7 (5–7) | 0.07 |
| Average parenteral lipid intake (g/kg/day), median (IQR) | 858 | 2 (1.6–2.4) | 2.2 (1.8–2.6) | <0.001 * |
| Average parenteral protein intake (g/kg/day), median (IQR) | 858 | 3.8 (3.6–4) | 4 (3.9–4) | <0.001 * |
| Average parenteral carbohydrate intake (mg/kg/min), median (IQR) | 858 | 8.5 (7.9–9.2) | 8.2 (7.2–8.7) | <0.001 * |
| Average parenteral calorie intake (kcal/kg/day), median (IQR) | 858 | 76.42 (68.74–82.06) | 75.48 (68.11–80.85) | 0.15 |
| Average parenteral lipid intake in the 1st 7 days (g/kg/day), median (IQR) | 858 | 1.8 (1.4–2.3) | 2.2 (1.8–2.6) | <0.001 * |
| Average parenteral protein intake in the 1st 7 days (g/kg/day), median (IQR) | 858 | 4 (3.6–4) | 4 (4–4) | <0.001 * |
| Average parenteral carbohydrate intake in the 1st 7 days (mg/kg/min), median (IQR) | 858 | 8.2 (7.5–8.8) | 7.6 (6.8–8.2) | <0.001 * |
| Average parenteral calorie intake in the 1st 7 days (kcal/kg/day), median (IQR) | 858 | 73.03 (61.57–79.93) | 73.85 (65.12–79.71) | 0.56 |
| Enteral nutrition | ||||
| Age of starting feeding (days), median (IQR) | 858 | 3 (1–5) | 3 (1–5.25) | 0.15 |
| Received expressed breastmilk, n (%) | 858 | 304 (49) | 155 (64.9) | <0.001 * |
| High calorie formula (1 kcal/mL), n (%) | 858 | 54 (8.7) | 20 (8.4) | 0.89 |
| Feeding interruption #, n (%) | 858 | 85 (13.7) | 33 (13.8) | 1.0 |
| Variable | N | Intralipid (n = 620) | SMOFlipid (n = 238) | p Value |
|---|---|---|---|---|
| Growth anthropometrics | ||||
| Δ Weight z-score, median (IQR) | 858 | −1.2 (−2.26–−0.31) | −1.70 (−3.01–−0.57) | <0.001 * |
| Weight gain velocity (g/kg/day), median (IQR) | 858 | 6.2 (3.6–8) | 5.8 (2–7.7) | 0.02 * |
| Weight at discharge # (g), median (IQR) | 858 | 1820 (1402.5–1967.5) | 1780 (1190–2000) | 0.10 |
| Weight at discharge # z-score, median (IQR) | 858 | −1.72 (−2.76–−1.07) | −1.94 (−2.86–−1.29) | 0.02 * |
| HC at discharge # (g), median (IQR) | 858 | 32 (31–34) | 33 (32–35) | 0.55 |
| HC at discharge # z-score, median (IQR) | 858 | −1.2 (−1.82–−0.44) | −1.3 (−2.01–−65) | 0.24 |
| Δ HC z-score, median (IQR) | 858 | −1.02 (−1.69–−0.39) | −1.1 (−1.82–−0.53) | 0.19 |
| Neonatal morbidities and mortality | ||||
| Bronchopulmonary dysplasia, n (%) | 582 | 209 (47.9) | 44 (30.1) | <0.001 * |
| Late onset of sepsis (culture-proven), n (%) | 858 | 227 (36.6) | 122 (51) | <0.001 * |
| Retinopathy of prematurity stage ≥ 2, n (%) | 575 | 43 (10.3) | 11 (7.1) | 0.27 |
| Any intraventricular hemorrhage, n (%) | 858 | 223 (36) | 76 (31.8) | 0.26 |
| Severe intraventricular hemorrhage, n (%) | 858 | 108 (17.4) | 36 (15.1) | 0.48 |
| Necrotizing enterocolitis (stage ≥ 2), n (%): Medical management Surgical management | 858 | 171 (27.6) 39 (6.3) | 52 (21.8) 14 (5.9) | 0.08 0.88 |
| Spontaneous intestinal perforation, n (%) | 858 | 5 (0.8) | 5 (2.1) | 0.15 |
| Length of hospital stay, median (IQR) | 858 | 41 (23–64) | 38 (16–64) | 0.06 |
| Mortality, n (%) | 858 | 134 (21.6) | 63 (26.5) | 0.15 |
| Unadjusted 95% CI | Adjusted 95% CI | |
|---|---|---|
| Δ Weight z-score (MD) | −0.48 (−0.75, −0.20) | −0.67 (−0.96, −0.39) |
| Weight at discharge z-score # (MD) | 2.07 (−9.08, 13.22) | −0.96 (−13.37, 11.46) |
| Bronchopulmonary dysplasia (RR) | 0.63 (0.48, 0.82) | 0.61 (0.46, 0.80) |
| Late-onset sepsis (RR) | 1.40 (1.19, 1.65) | 1.44 (1.22, 1.69) |
| Retinopathy of prematurity stage ≥ 2 (RR) | 0.69 (0.37, 1.31) | 0.43 (0.15–1.22) |
| Severe intraventricular hemorrhage (RR) | 0.87 (0.61–1.22) | 0.82 (0.55–1.22) |
| Necrotizing enterocolitis (RR) | 0.76 (0.59–0.97) | 0.78 (0.59–1.01) |
| Length of hospital stay (RR) | −6.59 (−13.0, 0.21) | −3.09 (−8.18, 2.00) |
| Mortality (RR) | 1.23 (0.95–1.59) | 1.21 (0.9–1.64) |
| Variable | Mean Confidence Interval | Mean Difference Confidence Interval | p Value | Interaction p Value | |
|---|---|---|---|---|---|
| Intralipid | SMOFlipid | Sex | |||
| Δ Weight z-score | 0.001 * | ||||
| Male | −1.13 (−1.33–−0.93) | −1.96 (−2.30–−1.64) | 0.84 (0.46–1.22) | <0.001 * | |
| Female | −1.78 (−1.99–−1.56) | −1.85 (−2.19–−1.53) | 0.08 (−0.31−0.47) | 0.823 | |
| Weight at discharge # (g) | 1757.78 (1705.42–1810.13) | 1668.57 (1586.53–1750.62) | 89.21 (−9.18–187.59) | 0.07 | 0.74 |
| Weight at discharge z-score # | 0.91 (−4.77–6.59) | 2.98 (−7.31–13.27) | −2.07 (−13.8–−9.08) | 0.72 | 0.77 |
| Weight gain velocity (g/kg/day) | 5.91 (5.07–6.75) | 4.63 (3.94–5.31) | 1.29 (−0.15–2.72) | 0.08 | 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asfour, S.S.; Alshaikh, B.; AlMahmoud, L.; Sumaily, H.H.; Alodhaidan, N.A.; Alkhourmi, M.; Abahussain, H.A.; Khalil, T.M.; Albeshri, B.A.; Alhamidi, A.A.; et al. SMOFlipid Impact on Growth and Neonatal Morbidities in Very Preterm Infants. Nutrients 2022, 14, 3952. https://doi.org/10.3390/nu14193952
Asfour SS, Alshaikh B, AlMahmoud L, Sumaily HH, Alodhaidan NA, Alkhourmi M, Abahussain HA, Khalil TM, Albeshri BA, Alhamidi AA, et al. SMOFlipid Impact on Growth and Neonatal Morbidities in Very Preterm Infants. Nutrients. 2022; 14(19):3952. https://doi.org/10.3390/nu14193952
Chicago/Turabian StyleAsfour, Suzan S., Belal Alshaikh, Latifah AlMahmoud, Haider H. Sumaily, Nabeel A. Alodhaidan, Mousa Alkhourmi, Hissah A. Abahussain, Thanaa M. Khalil, Bushra A. Albeshri, Aroub A. Alhamidi, and et al. 2022. "SMOFlipid Impact on Growth and Neonatal Morbidities in Very Preterm Infants" Nutrients 14, no. 19: 3952. https://doi.org/10.3390/nu14193952
APA StyleAsfour, S. S., Alshaikh, B., AlMahmoud, L., Sumaily, H. H., Alodhaidan, N. A., Alkhourmi, M., Abahussain, H. A., Khalil, T. M., Albeshri, B. A., Alhamidi, A. A., Al-Anazi, M. R., Asfour, R. S., & Al-Mouqdad, M. M. (2022). SMOFlipid Impact on Growth and Neonatal Morbidities in Very Preterm Infants. Nutrients, 14(19), 3952. https://doi.org/10.3390/nu14193952







