Validating a Nutrition Ranking System for Food Pantries Using the Healthy Eating Index-2015
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. HER Guideline Measures
2.3. Healthy Eating Index (HEI) Measures
2.4. Data Analysis
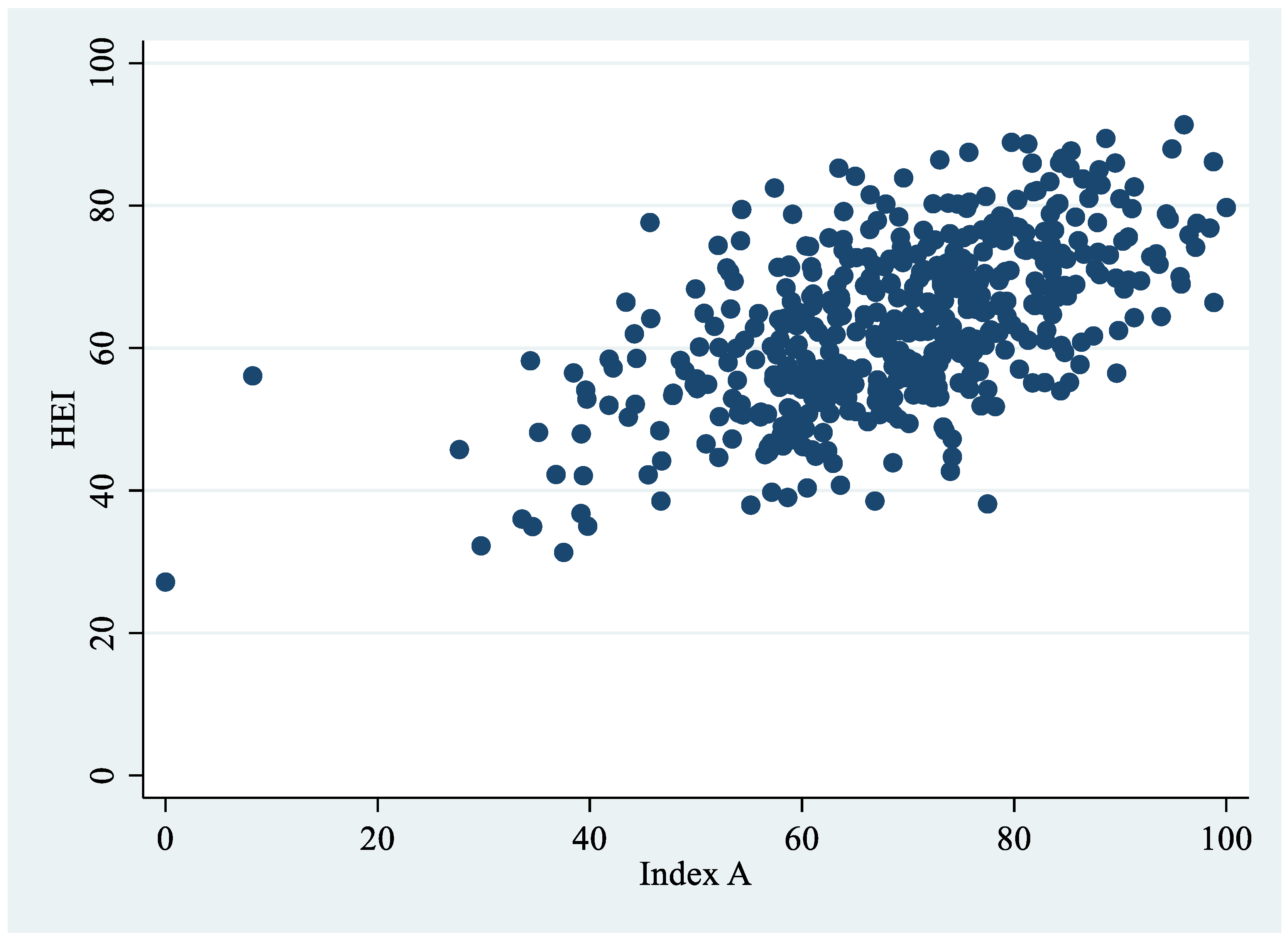
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martin, K.S. Reinventing Food Banks and Pantries: New Tools to End Hunger; Island Press: Washington, DC, USA, 2021. [Google Scholar]
- Schwartz, M.B.; Seligman, H.K. The Unrealized Health-Promoting Potential of a National Network of Food Pantries. J. Hunger Environ. Nutr. 2019, 14, 1–3. [Google Scholar] [CrossRef]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Statistical Supplement to Household Food Security in the United States in 2020. Available online: http://www.ers.usda.gov/publications/pub-details/?pubid=102071 (accessed on 29 April 2022).
- U.S. Department of Agriculture, Economic Research Service. Food Security in the U.S.—Survey Tools. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/#six (accessed on 28 March 2022).
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Social Determinants of Health—Healthy People 2030. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 16 December 2021).
- Rush, T.J.; Ng, V.; Irwin, J.D.; Stitt, L.W.; He, M. Food insecurity and dietary intake of immigrant food bank users. Can. J. Diet. Pract. Res. Publ. Dietit. 2007, 68, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Duffy, P.; Zizza, C.; Jacoby, J.; Tayie, F.A. Diet Quality is Low among Female Food Pantry Clients in Eastern Alabama. J. Nutr. Educ. Behav. 2009, 41, 414–419. [Google Scholar] [CrossRef]
- Starkey, L.J.; Kuhnlein, H.V.; Gray-Donald, K. Food bank users: Sociodemographic and nutritional characteristics. Can. Med. Assoc. J. 1998, 158, 1143–1149. [Google Scholar]
- Gundersen, C.; Ziliak, J.P. Food Insecurity and Health Outcomes. Health Aff. Proj. Hope 2015, 34, 1830–1839. [Google Scholar] [CrossRef]
- Leung, C.W.; Kullgren, J.T.; Malani, P.N.; Singer, D.C.; Kirch, M.; Solway, E.; Wolfson, J.A. Food insecurity is associated with multiple chronic conditions and physical health status among older US adults. Prev. Med. Rep. 2020, 20, 101211. [Google Scholar] [CrossRef] [PubMed]
- Gregory, C.A.; Coleman-Jensen, A. Food Insecurity, Chronic Disease, and Health Among Working-Age Adults; US Department of Agriculture, Economic Research Service: Washington, DC, USA, 2017. Available online: https://www.ers.usda.gov/webdocs/publications/84467/err-235.pdf?v=8785.3 (accessed on 28 March 2022).
- Laraia, B.A. Food insecurity and chronic disease. Adv. Nutr. Bethesda Md. 2013, 4, 203–212. [Google Scholar] [CrossRef]
- Dinour, L.M.; Bergen, D.; Yeh, M.-C. The Food Insecurity–Obesity Paradox: A Review of the Literature and the Role Food Stamps May Play. J. Am. Diet. Assoc. 2007, 107, 1952–1961. [Google Scholar] [CrossRef]
- Franklin, B.; Jones, A.; Love, D.; Puckett, S.; Macklin, J.; White-Means, S. Exploring mediators of food insecurity and obesity: A review of recent literature. J. Community Health 2012, 37, 253–264. [Google Scholar] [CrossRef]
- Seligman, H.K.; Laraia, B.A.; Kushel, M.B. Food Insecurity Is Associated with Chronic Disease among Low-Income NHANES Participants. J. Nutr. 2010, 140, 304–310. [Google Scholar] [CrossRef]
- Seligman, H.K.; Bindman, A.B.; Vittinghoff, E.; Kanaya, A.M.; Kushel, M.B. Food insecurity is associated with diabetes mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J. Gen. Intern. Med. 2007, 22, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Caspi, C.E.; Canterbury, M.; Carlson, S.; Bain, J.; Bohen, L.; Grannon, K.; Peterson, H.; Kottke, T. A behavioural economics approach to improving healthy food selection among food pantry clients. Public Health Nutr. 2019, 22, 2303–2313. [Google Scholar] [CrossRef] [PubMed]
- Wright, B.N.; Tooze, J.A.; Bailey, R.L.; Liu, Y.; Rivera, R.L.; McCormack, L.; Stluka, S.; Franzen-Castle, L.; Henne, B.; Mehrle, D.; et al. Dietary Quality and Usual Intake of Underconsumed Nutrients and Related Food Groups Differ by Food Security Status for Rural, Midwestern Food Pantry Clients. J. Acad. Nutr. Diet. 2020, 120, 1457–1468. [Google Scholar] [CrossRef] [PubMed]
- Algert, S.J.; Reibel, M.; Renvall, M.J. Barriers to Participation in the Food Stamp Program Among Food Pantry Clients in Los Angeles. Am. J. Public Health 2006, 96, 807–809. [Google Scholar] [CrossRef]
- Eicher-Miller, H.A. A review of the food security, diet and health outcomes of food pantry clients and the potential for their improvement through food pantry interventions in the United States. Physiol. Behav. 2020, 220, 112871. [Google Scholar] [CrossRef]
- Long, C.R.; Rowland, B.; McElfish, P.A. Intervention to Improve Access to Fresh Fruits and Vegetables among Arkansas Food Pantry Clients. Prev. Chronic Dis. 2019, 16, E09. [Google Scholar] [CrossRef]
- Seligman, H.K.; Lyles, C.R.; Marshall, M.B.; Prendergast, K.; Smith, M.C.; Headings, A.; Bradshaw, G.; Rosenmoss, S.; Waxman, E. A pilot food bank intervention featuring diabetes-appropriate food improved glycemic control among clients in three states. Health Aff. Proj. Hope 2015, 34, 1956–1963. [Google Scholar] [CrossRef]
- How to Help Your Neighbors This Summer|Feeding America. Available online: https://www.feedingamerica.org/hunger-blog/help-your-neighbors-summer (accessed on 23 June 2022).
- Liu, Y.; Desmond, N.E.; Wright, B.N.; Bailey, R.L.; Dong, T.; Craig, B.A.; Eicher-Miller, H.A. Nutritional contributions of food pantries and other sources to the diets of rural, Midwestern food pantry users in the USA. Br. J. Nutr. 2020, 125, 891–901. [Google Scholar] [CrossRef]
- Wright, B.N.; Bailey, R.L.; Craig, B.A.; Mattes, R.D.; McCormack, L.; Stluka, S.; Franzen-Castle, L.; Henne, B.; Mehrle, D.; Remley, D.; et al. Daily Dietary Intake Patterns Improve after Visiting a Food Pantry among Food-Insecure Rural Midwestern Adults. Nutrients 2018, 10, 583. [Google Scholar] [CrossRef]
- Caspi, C.E. Needs and Preferences Among Food Pantry Clients. Prev. Chronic Dis. 2021, 18, E29. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, Y.; Remley, D.T.; Eicher-Miller, H.A. Frequency of Food Pantry Use Is Associated with Diet Quality among Indiana Food Pantry Clients. J. Acad. Nutr. Diet. 2019, 119, 1703–1712. [Google Scholar] [CrossRef] [PubMed]
- Caspi, C.E.; Davey, C.; Barsness, C.B.; Wolfson, J.; Peterson, H.; Pratt, R.J. Applying the Healthy Eating Index-2015 in a Sample of Choice-Based Minnesota Food Pantries to Test Associations between Food Pantry Inventory, Client Food Selection, and Client Diet. J. Acad. Nutr. Diet. 2021, 121, 2242–2250. [Google Scholar] [CrossRef] [PubMed]
- Byker Shanks, C. Promoting Food Pantry Environments that Encourage Nutritious Eating Behaviors. J. Acad. Nutr. Diet. 2017, 117, 523–525. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.B.; Levi, R.; Lott, M.; Arm, K.; Seligman, H. Healthy Eating Research Nutrition Guidelines for the Charitable Food System. Healthy Eating Research; 2020. Available online: https://healthyeatingresearch.org/ (accessed on 28 March 2022).
- Feldman, M.; Schwartz, M.B. A Tipping Point: Leveraging Opportunities to Improve the Nutritional Quality of Food Bank Inventory; Mazon: A Jewish Response to Hunger. 2018. Available online: https://mazon.org/wp-content/uploads/MAZON-Report-TippingPoint.pdf (accessed on 28 March 2022).
- Anderson, E.; Wei, R.; Liu, B.; Plummer, R.; Kelahan, H.; Tamez, M.; Marrero, A.; Bhupathiraju, S.; Mattei, J. Improving Healthy Food Choices in Low-Income Settings in the United States Using Behavioral Economic-Based Adaptations to Choice Architecture. Front. Nutr. 2021, 8, 734991. [Google Scholar] [CrossRef] [PubMed]
- Nanney, M.S.; Grannon, K.Y.; Cureton, C.; Hoolihan, C.; Janowiec, M.; Wang, Q.; Warren, C.; King, R.P. Application of the Healthy Eating Index-2010 to the hunger relief system. Public Health Nutr. 2016, 19, 2906–2914. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Reedy, J.; Lerman, J.L.; Krebs-Smith, S.M.; Kirkpatrick, S.I.; Pannucci, T.E.; Wilson, M.M.; Subar, A.F.; Kahle, L.L.; Tooze, J.A. Evaluation of the Healthy Eating Index-2015. J. Acad. Nutr. Diet. 2018, 118, 1622–1633. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; 2020. Available online: https://DietaryGuidelines.gov/ (accessed on 28 July 2022).
- Byker Shanks, C.; Webber, E.; Larison, L.; Wytcherley, B. The translational implications of applying multiple measures to evaluate the nutrient quality of the food supply: A case study of two food pantries in Montana. Transl. Behav. Med. 2020, 10, 1367–1381. [Google Scholar] [CrossRef]
- King, R.P.; Warren, C.; Cureton, C.; Hoolihan, C.; Grannon, K.Y.; Nanney, M.S. How Healthy Is Hunger Relief Food? Am. J. Agric. Econ. 2016, 98, 533–548. [Google Scholar] [CrossRef]
- Caspi, C.E.; Grannon, K.Y.; Wang, Q.; Nanney, M.S.; King, R.P. Refining and implementing the Food Assortment Scoring Tool (FAST) in food pantries. Public Health Nutr. 2018, 21, 2548–2557. [Google Scholar] [CrossRef]
- Feeding America. Feeding America’s Foods to Encourage Background. Available online: http://hungerandhealth.feedingamerica.org/wp-content/uploads/legacy/mp/files/tool_and_resources/files/f2e-background-detail.v1.pdf (accessed on 30 June 2022).
- Seidel, M.; Laquatra, I.; Woods, M.; Sharrard, J. Applying a Nutrient-Rich Foods Index Algorithm to Address Nutrient Content of Food Bank Food. J. Acad. Nutr. Diet. 2015, 115, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.S.; Wolff, M.; Callahan, K.; Schwartz, M.B. Supporting Wellness at Pantries: Development of a Nutrition Stoplight System for Food Banks and Food Pantries. J. Acad. Nutr. Diet. 2019, 119, 553–559. [Google Scholar] [CrossRef] [PubMed]
- SWAP: Overview of a Stoplight Nutrition System for Food Banks and Food Pantries. Hunger and Health. Available online: https://hungerandhealth.feedingamerica.org/resource/swap-development-stoplight-nutrition-system-food-banks-food-pantries/ (accessed on 24 June 2022).
- Hesse, M.; Peachy, A.; Wang, D. The Development and Implementation of Nourish to Rank and Track the Nutritional Quality of Food Bank Foods. In Proceedings of the Food and Nutirtion Conference & Expo, Virtual, 19 October 2021. [Google Scholar]
- Casey, P.H.; Goolsby, S.L.; Lensing, S.Y.; Perloff, B.P.; Bogle, M.L. The use of telephone interview methodology to obtain 24-hour dietary recalls. J. Am. Diet. Assoc. 1999, 99, 1406–1411. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 13 January 2016).
- Ahrens, A.; Hansen, C.B.; Schaffer, M.E. lassopack: Model selection and prediction with regularized regression in Stata. Stata J. 2020, 20, 176–235. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Meyer, G.J.; Finn, S.E.; Eyde, L.D.; Kay, G.G.; Moreland, K.L.; Dies, R.R.; Eisman, E.J.; Kubiszyn, T.W.; Reed, G.M. Psychological testing and psychological assessment: A review of evidence and issues. Am. Psychol. 2001, 56, 128–165. [Google Scholar] [CrossRef] [PubMed]
- Nanney, M.S.; Kratchmer, L. Healthy F.O.O.D. in Food Shelves. Presented at the Minnesota Food Access Summit, Duluth, MN, USA, October 2015. [Google Scholar]
- Martin, K.; Xu, R.; Schwartz, M.B. Food pantries select healthier foods after nutrition information is available on their food bank’s ordering platform. Public Health Nutr. 2020, 24, 5066–5073. [Google Scholar] [CrossRef] [PubMed]
- Feeding America. The Impact of the Coronavirus on Food Insecurity in 2020 & 2021. Available online: https://www.feedingamerica.org/sites/default/files/2021-03/National%20Projections%20Brief_3.9.2021_0.pdf (accessed on 17 June 2021).
- Kinney, S.; Simon, C.; Caspi, C.; Schwartz, M. Under Pressure: Prioritizing Healthy Hunger Relief during the COVID-19 Pandemic. Available online: https://uconnruddcenter.org/wp-content/uploads/sites/2909/2021/03/PHA-Report-January-2021.pdf (accessed on 21 June 2021).

| Tier-Ranked Variables | Model 1
(Ridge Regression) | Model 2
(Cross-Validation) | Model 3
(Linear Regression) |
|---|---|---|---|
| % Green | 0.185 | 0.257 | 0.270 |
| % Red | −0.217 | −0.269 | −0.278 |
| Constant | 59.23 | 57.13 | 56.72 |
| Sample | Sample Size | Index A | Index B | Index C |
|---|---|---|---|---|
| 1 | 101 | 0.4863 | 0.4865 | 0.4866 |
| 2 | 100 | 0.5998 | 0.5997 | 0.5997 |
| 3 | 101 | 0.6452 | 0.6444 | 0.6441 |
| 4 | 100 | 0.5641 | 0.5642 | 0.5642 |
| 5 | 101 | 0.6274 | 0.6276 | 0.6276 |
| Mean | 0.5846 | 0.5845 | 0.5844 | |
| SD | 0.0629 | 0.0626 | 0.0625 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gombi-Vaca, M.F.; Xu, R.; Schwartz, M.; Battista Hesse, M.; Martin, K.; Caspi, C.E. Validating a Nutrition Ranking System for Food Pantries Using the Healthy Eating Index-2015. Nutrients 2022, 14, 3899. https://doi.org/10.3390/nu14193899
Gombi-Vaca MF, Xu R, Schwartz M, Battista Hesse M, Martin K, Caspi CE. Validating a Nutrition Ranking System for Food Pantries Using the Healthy Eating Index-2015. Nutrients. 2022; 14(19):3899. https://doi.org/10.3390/nu14193899
Chicago/Turabian StyleGombi-Vaca, Maria Fernanda, Ran Xu, Marlene Schwartz, Michelle Battista Hesse, Katie Martin, and Caitlin E. Caspi. 2022. "Validating a Nutrition Ranking System for Food Pantries Using the Healthy Eating Index-2015" Nutrients 14, no. 19: 3899. https://doi.org/10.3390/nu14193899
APA StyleGombi-Vaca, M. F., Xu, R., Schwartz, M., Battista Hesse, M., Martin, K., & Caspi, C. E. (2022). Validating a Nutrition Ranking System for Food Pantries Using the Healthy Eating Index-2015. Nutrients, 14(19), 3899. https://doi.org/10.3390/nu14193899






