Prevalence of and Risk Factors for Iron Deficiency in Twin and Singleton Newborns
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
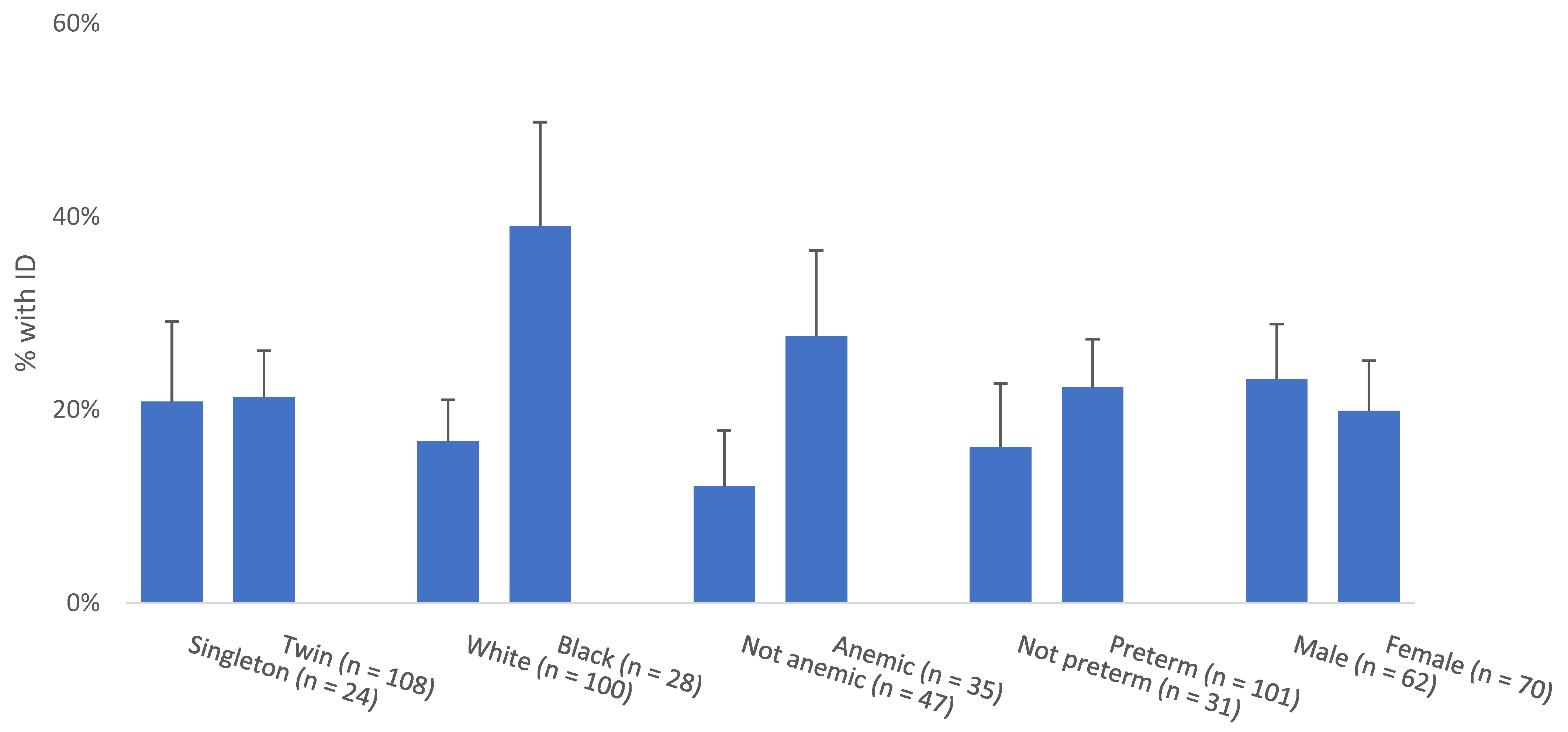
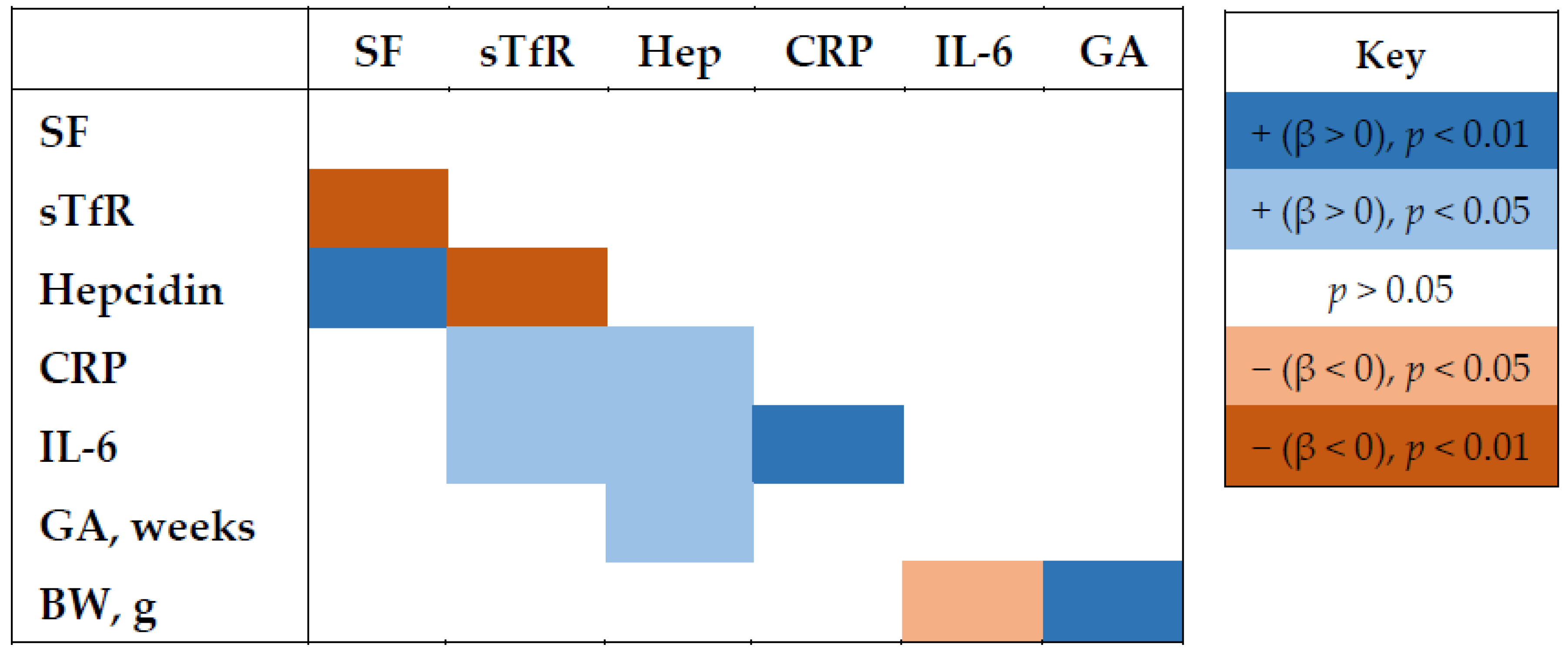
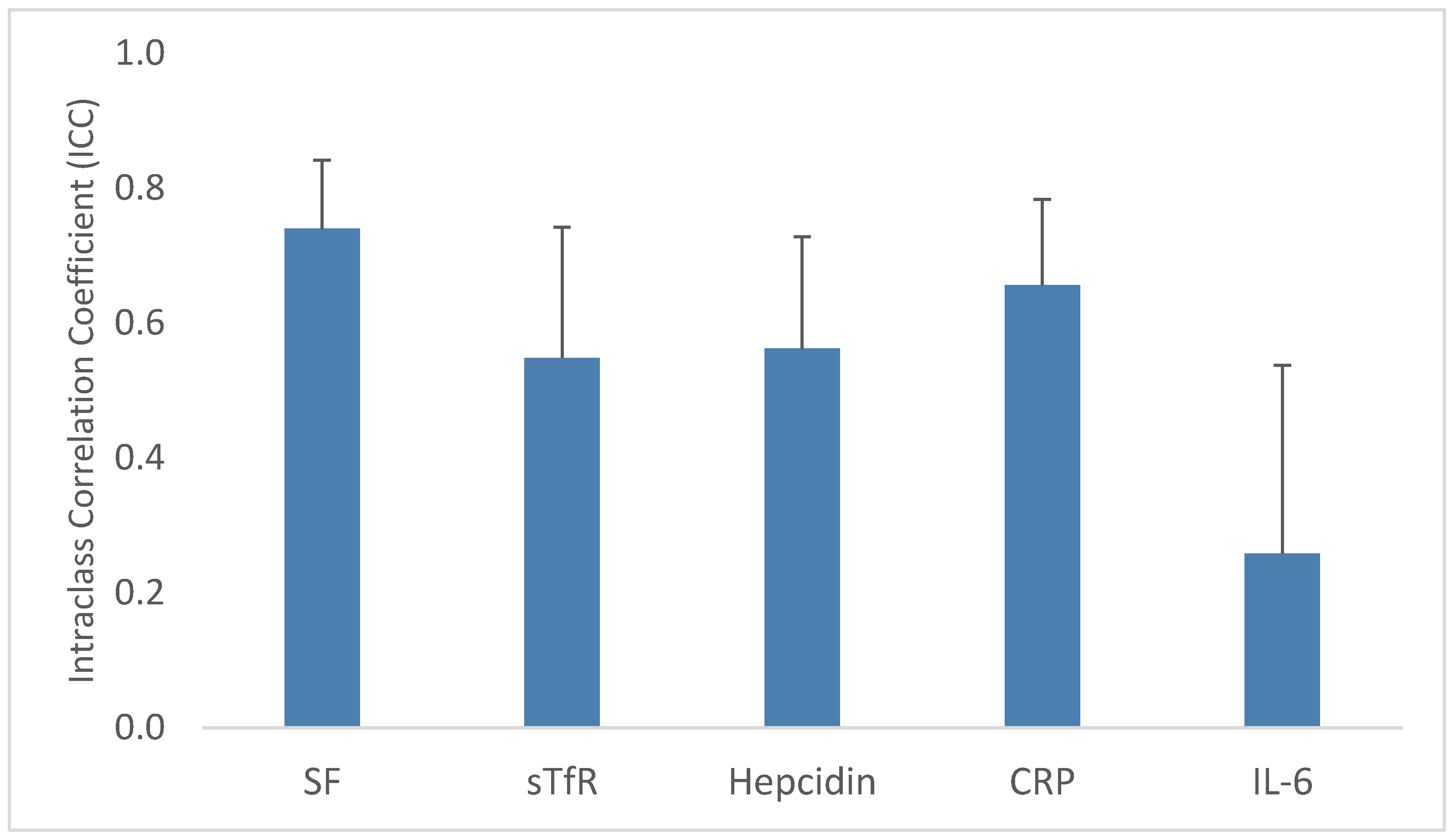
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Black, M.M.; Walker, S.P.; Fernald, L.C.H.; Andersen, C.T.; DiGirolamo, A.M.; Lu, C.; McCoy, D.C.; Fink, G.; Shawar, Y.R.; Shiffman, J.; et al. Early childhood development coming of age: Science through the life course. Lancet 2017, 389, 77–90. [Google Scholar] [CrossRef]
- Kassebaum, N.J. The global burden of anemia. Hematol./Oncol. Clin. N. Am. 2016, 30, 247–308. [Google Scholar] [CrossRef] [PubMed]
- Black, M.M.; Quigg, A.M.; Hurley, K.M.; Pepper, M.R. Iron deficiency and iron-deficiency anemia in the first two years of life: Strategies to prevent loss of developmental potential. Nutr. Rev. 2011, 69 (Suppl. 1), S64–S70. [Google Scholar] [CrossRef]
- Gupta, P.M.; Hamner, H.C.; Suchdev, P.S.; Flores-Ayala, R.; Mei, Z. Iron status of toddlers, nonpregnant females, and pregnant females in the United States. Am. J. Clin. Nutr. 2017, 106, 1640S–1646S. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.D.; Greer, F.R.; Committee on Nutrition. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics 2010, 126, 1040–1050. [Google Scholar] [CrossRef]
- Siddappa, A.M.; Georgieff, M.K.; Wewerka, S.; Worwa, C.; Nelson, C.A.; Deregnier, R.A. Iron deficiency alters auditory recognition memory in newborn infants of diabetic mothers. Pediatr. Res. 2004, 55, 1034–1041. [Google Scholar] [CrossRef]
- Mercer, J.S.; Erickson-Owens, D.A.; Deoni, S.C.L.; Dean, D.C., 3rd; Collins, J.; Parker, A.B.; Wang, M.; Joelson, S.; Mercer, E.N.; Padbury, J.F. Effects of delayed cord clamping on 4-month ferritin levels, Brain myelin content, and neurodevelopment: A randomized controlled trial. J. Pediatr. 2018, 203, 266–272.e262. [Google Scholar] [CrossRef]
- Lubach, G.R.; Coe, C.L. Preconception maternal iron status is a risk factor for iron deficiency in infant rhesus monkeys (Macaca mulatta). J. Nutr. 2006, 136, 2345–2349. [Google Scholar] [CrossRef][Green Version]
- Golub, M.S.; Hogrefe, C.E.; Tarantal, A.F.; Germann, S.L.; Beard, J.L.; Georgieff, M.K.; Calatroni, A.; Lozoff, B. Diet-induced iron deficiency anemia and pregnancy outcome in rhesus monkeys. Am. J. Clin. Nutr. 2006, 83, 647–656. [Google Scholar] [CrossRef][Green Version]
- Siddappa, A.M.; Rao, R.; Long, J.D.; Widness, J.A.; Georgieff, M.K. The assessment of newborn iron stores at birth: A review of the literature and standards for ferritin concentrations. Neonatology 2007, 92, 73–82. [Google Scholar] [CrossRef]
- Coe, C.L.; Lubach, G.R.; Shirtcliff, E.A. Maternal stress during pregnancy predisposes for iron deficiency in infant monkeys impacting innate immunity. Pediatr. Res. 2007, 61, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Osterman, M.J.K.; Hamilton, B.E.; Martin, J.A.; Driscoll, A.K.; Valenzuela, C.P. Births: Final Data for 2020; US Department of Health and Human Services Centers for Disease Control and Prevention: Atlanta, GA, USA, 2022.
- Goodnight, W.; Newman, R. Optimal nutrition for improved twin pregnancy outcome. Obstet. Gynecol. 2009, 114, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Ru, Y.; Pressman, E.K.; Cooper, E.M.; Guillet, R.; Katzman, P.J.; Kent, T.R.; Bacak, S.J.; O’Brien, K.O. Iron deficiency and anemia are prevalent in women with multiple gestations. Am. J. Clin. Nutr. 2016, 104, 1052–1060. [Google Scholar] [CrossRef]
- Sutcliffe, A.G.; Derom, C. Follow-up of twins: Health, behaviour, speech, language outcomes and implications for parents. Early Hum. Dev. 2006, 82, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Wierzejska, R.E. Review of Dietary Recommendations for Twin Pregnancy: Does Nutrition Science Keep Up with the Growing Incidence of Multiple Gestations? Nutrients 2022, 14, 1143. [Google Scholar] [CrossRef] [PubMed]
- Brotanek, J.M.; Halterman, J.S.; Auinger, P.; Flores, G.; Weitzman, M. Iron Deficiency, Prolonged Bottle-Feeding, and Racial/Ethnic Disparities in Young Children. JAMA Pediatr. 2005, 159, 1038–1042. [Google Scholar] [CrossRef]
- Le, C.H.H. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003–2012). PLoS ONE 2016, 11, e0166635. [Google Scholar] [CrossRef]
- Cepeda-Lopez, A.C.; Osendarp, S.J.; Melse-Boonstra, A.; Aeberli, I.; Gonzalez-Salazar, F.; Feskens, E.; Villalpando, S.; Zimmermann, M.B. Sharply higher rates of iron deficiency in obese Mexican women and children are predicted by obesity-related inflammation rather than by differences in dietary iron intake. Am. J. Clin. Nutr. 2011, 93, 975–983. [Google Scholar] [CrossRef]
- Cepeda-Lopez, A.C.; Aeberli, I.; Zimmermann, M.B. Does obesity increase risk for iron deficiency? A review of the literature and the potential mechanisms. Int. J. Vitam. Nutr. Res. 2010, 80, 263–270. [Google Scholar] [CrossRef]
- Ramakrishnan, U.; Frith-Terhune, A.; Cogswell, M.; Kettel Khan, L. Dietary intake does not account for differences in low iron stores among Mexican American and non-Hispanic white women: Third National Health and Nutrition Examination Survey, 1988–1994. J. Nutr. 2002, 132, 996–1001. [Google Scholar] [CrossRef]
- Burris, H.H.; Lorch, S.A.; Kirpalani, H.; Pursley, D.M.; Elovitz, M.A.; Clougherty, J.E. Racial disparities in preterm birth in USA: A biosensor of physical and social environmental exposures. Arch. Dis. Child 2019, 104, 931. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, S.P.; Scardo, J.A.; Hayes, E.; Abuhamad, A.Z.; Berghella, V. Twins: Prevalence, problems, and preterm births. Am. J. Obs. Gynecol. 2010, 203, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Khoury, M.J.; Erickson, J.D. Maternal factors in dizygotic twinning: Evidence from interracial crosses. Ann. Hum. Biol. 1983, 10, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Ru, Y.; Pressman, E.K.; Guillet, R.; Katzman, P.J.; Vermeylen, F.; O’Brien, K.O. Umbilical cord hepcidin concentrations are positively associated with the variance in iron status among multiple birth neonates. J. Nutr. 2018, 148, 1716–1722. [Google Scholar] [CrossRef]
- Pfeiffer, C.M.; Looker, A.C. Laboratory methodologies for indicators of iron status: Strengths, limitations, and analytical challenges. Am. J. Clin. Nutr. 2017, 106, 1606S–1614S. [Google Scholar] [CrossRef]
- Ganz, T.; Nemeth, E. Hepcidin and iron homeostasis. Biochim. Biophys. Acta 2012, 1823, 1434–1443. [Google Scholar] [CrossRef]
- Suchdev, P.S.; Williams, A.M.; Mei, Z.; Flores-Ayala, R.; Pasricha, S.R.; Rogers, L.M.; Namaste, S.M. Assessment of iron status in settings of inflammation: Challenges and potential approaches. Am. J. Clin. Nutr. 2017, 106, 1626S–1633S. [Google Scholar] [CrossRef]
- Tamura, T.; Goldenberg, R.L.; Hou, J.; Johnston, K.E.; Cliver, S.P.; Ramey, S.L.; Nelson, K.G. Cord serum ferritin concentrations and mental and psychomotor development of children at five years of age. J. Pediatr. 2002, 140, 165–170. [Google Scholar] [CrossRef]
- Lee, S.; Guillet, R.; Cooper, E.M.; Westerman, M.; Orlando, M.; Kent, T.; Pressman, E.; O’Brien, K.O. Prevalence of anemia and associations between neonatal iron status, hepcidin, and maternal iron status among neonates born to pregnant adolescents. Pediatr. Res. 2016, 79, 42–48. [Google Scholar] [CrossRef]
- Buhimschi, C.S.; Bhandari, V.; Dulay, A.T.; Nayeri, U.A.; Abdel-Razeq, S.S.; Pettker, C.M.; Thung, S.; Zhao, G.; Han, Y.W.; Bizzarro, M.; et al. Proteomics mapping of cord blood identifies haptoglobin “switch-on” pattern as biomarker of early-onset neonatal sepsis in preterm newborns. PLoS ONE 2011, 6, e26111. [Google Scholar] [CrossRef]
- Nayeri, U.A.; Buhimschi, C.S.; Zhao, G.; Buhimschi, I.A.; Bhandari, V. Components of the antepartum, intrapartum, and postpartum exposome impact on distinct short-term adverse neonatal outcomes of premature infants: A prospective cohort study. PLoS ONE 2018, 13, e0207298. [Google Scholar] [CrossRef] [PubMed]
- Namaste, S.M.; Rohner, F.; Huang, J.; Bhushan, N.L.; Flores-Ayala, R.; Kupka, R.; Mei, Z.; Rawat, R.; Williams, A.M.; Raiten, D.J.; et al. Adjusting ferritin concentrations for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am. J. Clin. Nutr. 2017, 106, 359S–371S. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Anemia in Pregnancy: ACOG Practice Bulletin, Number 233. Obstet. Gynecol. 2021, 138, e55–e64. [Google Scholar] [CrossRef] [PubMed]
- MacQueen, B.C.; Christensen, R.D.; Baer, V.L.; Ward, D.M.; Snow, G.L. Screening umbilical cord blood for congenital Iron deficiency. Blood Cells Mol. Dis. 2019, 77, 95–100. [Google Scholar] [CrossRef]
- MacQueen, B.C.; Christensen, R.D.; Ward, D.M.; Bennett, S.T.; O’Brien, E.A.; Sheffield, M.J.; Baer, V.L.; Snow, G.L.; Weaver Lewis, K.A.; Fleming, R.E.; et al. The iron status at birth of neonates with risk factors for developing iron deficiency: A pilot study. J. Perinatol. 2017, 37, 436–440. [Google Scholar] [CrossRef][Green Version]
- Shao, J.; Richards, B.; Kaciroti, N.; Zhu, B.; Clark, K.M.; Lozoff, B. Contribution of iron status at birth to infant iron status at 9 months: Data from a prospective maternal-infant birth cohort in China. Eur. J. Clin. Nutr. 2021, 75, 364–372. [Google Scholar] [CrossRef]
- East, P.; Delker, E.; Lozoff, B.; Delva, J.; Castillo, M.; Gahagan, S. Associations among infant iron deficiency, childhood emotion and attention regulation, and adolescent problem behaviors. Child Dev. 2018, 89, 593–608. [Google Scholar] [CrossRef]
- Doom, J.R.; Richards, B.; Caballero, G.; Delva, J.; Gahagan, S.; Lozoff, B. Infant Iron Deficiency and Iron Supplementation Predict Adolescent Internalizing, Externalizing, and Social Problems. J. Pediatr. 2018, 195, 199–205.e192. [Google Scholar] [CrossRef]
- Geng, F.; Mai, X.; Zhan, J.; Xu, L.; Zhao, Z.; Georgieff, M.; Shao, J.; Lozoff, B. Impact of Fetal-Neonatal Iron Deficiency on Recognition Memory at 2 Months of Age. J. Pediatr. 2015, 167, 1226–1232. [Google Scholar] [CrossRef]
- Lozoff, B.; Clark, K.M.; Jing, Y.; Armony-Sivan, R.; Angelilli, M.L.; Jacobson, S.W. Dose-response relationships between iron deficiency with or without anemia and infant social-emotional behavior. J. Pediatr. 2008, 152, 696–702. [Google Scholar] [CrossRef]
- Algarín, C.; Peirano, P.; Garrido, M.; Pizarro, F.; Lozoff, B. Iron deficiency anemia in infancy: Long-lasting effects on auditory and visual system functioning. Pediatr. Res. 2003, 53, 217. [Google Scholar] [CrossRef] [PubMed]
- Lozoff, B.; Jimenez, E.; Hagen, J.; Mollen, E.; Wolf, A.W. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics 2000, 105, e51. [Google Scholar] [CrossRef] [PubMed]
- Lozoff, B. Iron deficiency and child development. Food Nutr. Bull. 2007, 28, S560–S571. [Google Scholar] [CrossRef]
- Ru, Y.; Pressman, E.K.; Guillet, R.; Katzman, P.J.; Bacak, S.J.; O’Brien, K.O. Predictors of anemia and iron status at birth in neonates born to women carrying multiple fetuses. Pediatr. Res. 2018, 84, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Butwick, A.J.; McDonnell, N. Antepartum and postpartum anemia: A narrative review. Int. J. Obs. Anesth. 2021, 47, 102985. [Google Scholar] [CrossRef] [PubMed]
- Breymann, C. Iron Deficiency Anemia in Pregnancy. Semin. Hematol. 2015, 52, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Mei, Z.; Cogswell, M.E.; Looker, A.C.; Pfeiffer, C.M.; Cusick, S.E.; Lacher, D.A.; Grummer-Strawn, L.M. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am. J. Clin. Nutr. 2011, 93, 1312–1320. [Google Scholar] [CrossRef]
- O’Brien, K.O.; Ru, Y. Iron status of North American pregnant women: An update on longitudinal data and gaps in knowledge from the United States and Canada. Am. J. Clin. Nutr. 2017, 106, 1647S–1654S. [Google Scholar] [CrossRef]
| Characteristic | Twin Pregnancies | Singleton Pregnancies | p-Value 1 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean | SD | n | % | Mean | SD | ||
| Maternal and Pregnancy | |||||||||
| Race | 54 | 24 | 0.253 | ||||||
| White | 42 | 77.8 | 16 | 66.7 | |||||
| Black | 10 | 18.5 | 8 | 33.3 | |||||
| Other | 2 | 3.7 | 0 | 0.0 | |||||
| Hispanic ethnicity | 54 | 24 | 0.340 | ||||||
| No | 52 | 96.3 | 24 | 100 | |||||
| Yes | 2 | 3.7 | 0 | 0 | |||||
| Maternal age, year | 54 | 28.9 | 6.1 | 24 | 27.9 | 6.4 | 0.497 | ||
| Gravidity | 54 | 24 | 0.023 | ||||||
| 1 | 26 | 48.1 | 5 | 20.8 | |||||
| 2+ | 28 | 51.9 | 19 | 79.2 | |||||
| Parity | 54 | 24 | 0.096 | ||||||
| 0 | 29 | 53.7 | 8 | 33.3 | |||||
| 1+ | 25 | 46.3 | 16 | 66.7 | |||||
| BMI | 33 | 35.7 | 8.2 | 12 | 37.8 | 8.2 | 0.457 | ||
| Anemia (Hb <11 g/dL) | 35 | 12 | 0.207 | ||||||
| No | 19 | 54.3 | 9 | 75.0 | |||||
| Yes | 16 | 45.7 | 3 | 25.0 | |||||
| Preeclampsia | 54 | 24 | 0.766 | ||||||
| No | 40 | 74.1 | 17 | 70.8 | |||||
| Yes | 14 | 25.9 | 7 | 29.2 | |||||
| Gestational and/or chronic hypertension | 54 | 24 | 0.143 | ||||||
| No | 52 | 96.3 | 21 | 87.5 | |||||
| Yes | 2 | 3.7 | 3 | 12.5 | |||||
| Twin type | 54 | ||||||||
| Di-di | 47 | 87.0 | |||||||
| Mono-di | 7 | 13.0 | |||||||
| Gestational age (GA), weeks | 54 | 34.9 | 2.2 | 24 | 35.2 | 2.9 | 0.529 | ||
| Preterm (GA <37 weeks) | 54 | 24 | 0.510 | ||||||
| No | 12 | 22.2 | 7 | 29.2 | |||||
| Yes | 42 | 77.8 | 17 | 70.8 | |||||
| Delivery context | 54 | 24 | 0.753 | ||||||
| Term delivery | 12 | 22.2 | 7 | 29.2 | |||||
| Spontaneous PTB | 20 | 37.0 | 9 | 37.5 | |||||
| Provider-initiated PTB | 22 | 40.7 | 8 | 33.3 | |||||
| Delivery type | 54 | 24 | 0.441 | ||||||
| Vaginal | 23 | 42.6 | 8 | 33.3 | |||||
| C-section | 31 | 57.4 | 16 | 66.7 | |||||
| Neonatal | |||||||||
| Birth weight (BW), g | 108 | 2239.1 | 477.6 | 24 | 2639.0 | 749.7 | 0.001 | ||
| LBW (BW <2500 g) | 108 | 24 | 0.045 | ||||||
| No | 39 | 36.1 | 14 | 58.3 | |||||
| Yes | 69 | 63.9 | 10 | 41.7 | |||||
| VLBW (BW <1500 g) | 108 | 24 | 0.887 | ||||||
| No | 98 | 90.7 | 22 | 91.7 | |||||
| Yes | 10 | 9.3 | 2 | 8.3 | |||||
| Sample type | 108 | 24 | 0.409 | ||||||
| Serum | 105 | 97.2 | 24 | 100 | |||||
| Plasma | 3 | 2.8 | 0 | 0 | |||||
| Biomarker | Twins | Singletons | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | Mean | SE | n | % | Mean | SE | |
| SF, ng/mL | 108 | 176.33 | 15.36 | 24 | 158.46 | 22.44 | ||
| ID (SF <76 ng/mL) | 23 | 21.3 | 5 | 20.8 | ||||
| sTfR, ng/mL | 108 | 2501.55 | 98.98 | 24 | 3527.85 | 404.99 | ||
| Hepcidin, ng/mL | 108 | 14.95 | 1.65 | 24 | 13.68 | 2.44 | ||
| CRP, ng/ml | 108 | 116.46 | 46.14 | 24 | 66.74 | 12.75 | ||
| Elevated (CRP ≥95th %ile) | 6 | 5.6 | 1 | 4.2 | ||||
| IL-6, pg/mL | 107 | 13.58 | 7.22 | 24 | 2.96 | 0.87 | ||
| Elevated (IL-6 ≥100 pg/mL) | 3 | 2.8 | 0 | 0 | ||||
| Characteristic | Β 1 | 95% CI |
|---|---|---|
| Race | ||
| White | ||
| Black | −0.53 | (−0.94, −0.12) |
| Other | 0.21 | (−0.84, 1.27) |
| Twin status | ||
| Singleton | ||
| Twin | 0.05 | (−0.33, 0.44) |
| Preterm (<37 weeks) | ||
| No | ||
| Yes | −0.54 | (−0.94, −0.15) |
| Sex | ||
| Male | ||
| Female | 0.32 | (0.11, 0.52) |
| Percent of Intrauterine Variability Explained | |||
|---|---|---|---|
| SF | sTfR | Hepcidin | |
| Hepcidin | 24.5 | 11.6 | |
| CRP | 0.2 | −1.1 | −6.6 |
| IL-6 | 1.8 | −1.3 | −3.2 |
| Birth weight | −0.6 | 0.5 | 3.2 |
| Infant sex | −2.7 | −1.2 | −4.2 |
| Maternal race | 5.0 | 5.3 | 1.1 |
| Maternal anemia | 12.2 | −2.5 | −1.1 |
| Maternal BMI | 9.8 | −6.3 | 0.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campbell, R.K.; Buhimschi, C.S.; Zhao, G.; Dela Rosa, C.; Stetson, B.T.; Backes, C.H.; Buhimschi, I.A. Prevalence of and Risk Factors for Iron Deficiency in Twin and Singleton Newborns. Nutrients 2022, 14, 3854. https://doi.org/10.3390/nu14183854
Campbell RK, Buhimschi CS, Zhao G, Dela Rosa C, Stetson BT, Backes CH, Buhimschi IA. Prevalence of and Risk Factors for Iron Deficiency in Twin and Singleton Newborns. Nutrients. 2022; 14(18):3854. https://doi.org/10.3390/nu14183854
Chicago/Turabian StyleCampbell, Rebecca K., Catalin S. Buhimschi, Guomao Zhao, Cielo Dela Rosa, Bethany T. Stetson, Carl H. Backes, and Irina A. Buhimschi. 2022. "Prevalence of and Risk Factors for Iron Deficiency in Twin and Singleton Newborns" Nutrients 14, no. 18: 3854. https://doi.org/10.3390/nu14183854
APA StyleCampbell, R. K., Buhimschi, C. S., Zhao, G., Dela Rosa, C., Stetson, B. T., Backes, C. H., & Buhimschi, I. A. (2022). Prevalence of and Risk Factors for Iron Deficiency in Twin and Singleton Newborns. Nutrients, 14(18), 3854. https://doi.org/10.3390/nu14183854






