Clinical Status, Nutritional Behavior, and Lifestyle, and Determinants of Community Well-Being of Patients from the Perspective of Physicians: A Cross-Sectional Study of Young Older Adults, Nonagenarians, and Centenarians in Salerno and Province, Italy
Abstract
1. Introduction
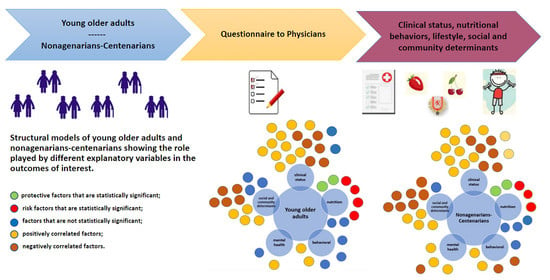
2. Materials and Methods
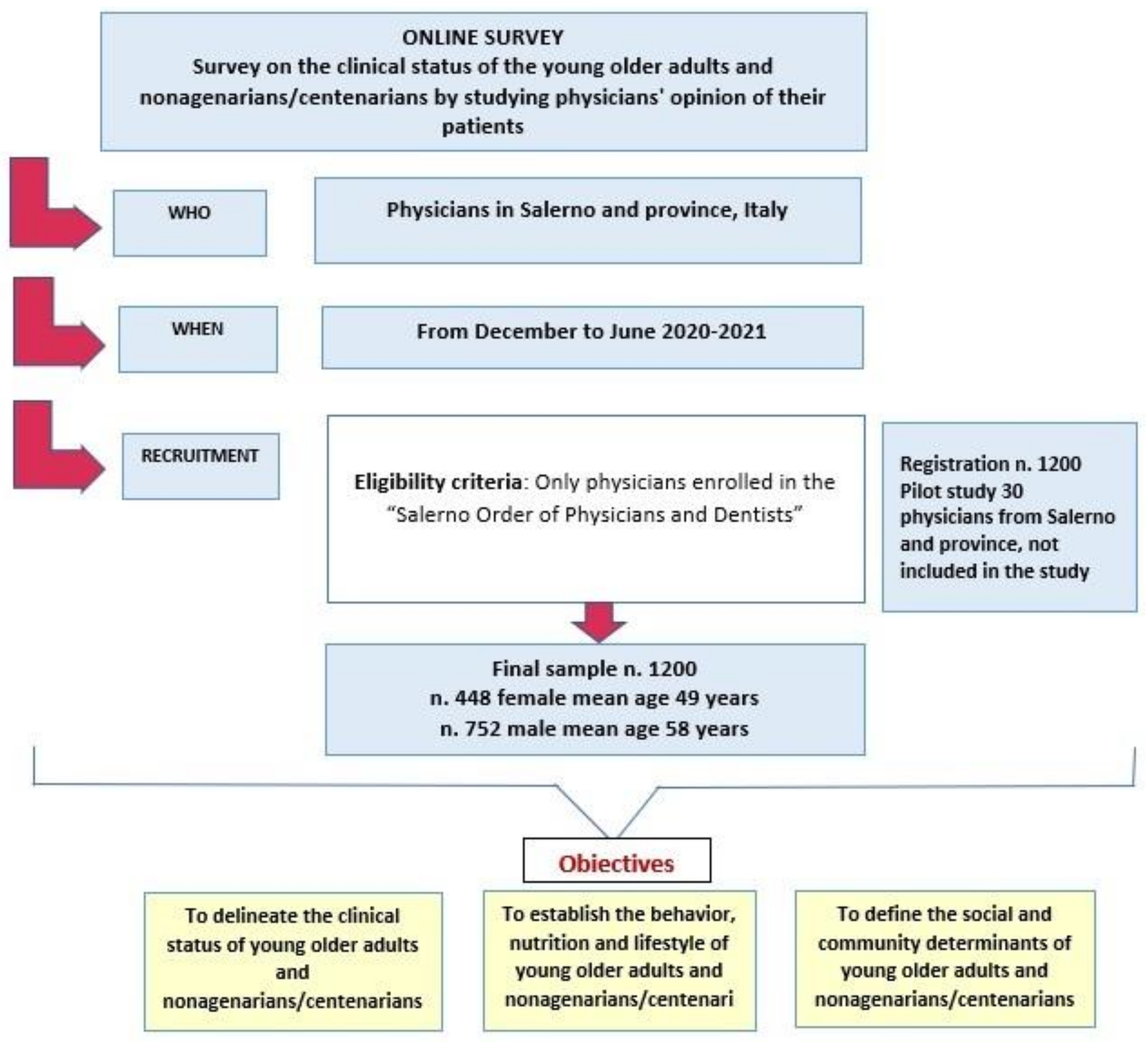
2.1. Study Design and Sampling
2.2. Data Collection Procedure
2.3. Data Collection Instrument
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Data of Physicians Who Participated in the Survey
3.2. Physician’s Assessment of the Clinical Status of the Young Older Adults and the Nonagenarians/Centenarians
3.3. Physician’s Assessment of Behavioral, Lifestyle, and Nutritional Factors of the Young Older Adults and the Nonagenarians/Centenarians
3.4. Physician’s Assessment of the Social and Community Determinants of the Young Older Adults and the Nonagenarians/Centenarians
3.5. Physician’s Assessment of the Organization of the Health Care System
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WPP. World Population Prospects 2019, United Nations, Department of Economic and Social Affairs, Population Division 2019. Available online: https://population.un.org/wpp/Download/Probabilistic/Population/ (accessed on 15 March 2022).
- Antonini, F.M. Elogio della vecchiaia: Centenari 1990. LR Med. Prat. 1990, 326, 1–3. [Google Scholar]
- Magnolfi, S.; Noferi, I.; Petruzzi, E.; Pinzani, P.; Malentacchi, F.; Pazzagli, M.; Antonini, F.; Marchionni, N. Centenarians in Tuscany: The role of the environmental factors. Arch. Gerontol. Geriatr. 2008, 48, 263–266. [Google Scholar] [CrossRef]
- Vaupel, J.W.; Carey, J.R.; Christensen, K.; Johnson, T.E.; Yashin, A.I.; Holm, N.V.; Iachine, I.A.; Kannisto, V.; Khazaeli, A.A.; Liedo, P.; et al. Biodemographic Trajectories of Longevity. Science 1998, 280, 855–860. [Google Scholar] [CrossRef]
- Fries, J.F. Aging, natural death, and the compression of morbidity. N. Engl. J. Med. 1980, 303, 130–135. [Google Scholar] [CrossRef]
- Barbi, E.; Caselli, G.; Vallin, J. Hétérogénéité des générations et âge extrême de le vie. Population 2003, 1, 45–67. [Google Scholar] [CrossRef]
- Puca, A. A caccia dei geni della longevità. Le Scienze 2004, 426, 42–47. [Google Scholar]
- Candore, G.; Modica, M.A.; Lio, D.; Colonna-Romano, G.; Listì, F.; Grimaldi, M.P.; Russo, M.; Triolo, G.; Accardo-Palumbo, A.; Cuccia, M.C.; et al. Pathogenesis of autoimmune diseases associated with 8.1 ancestral haplotype: A genetically determined defect of C4 influences immunological parameters of healthy carriers of the haplotype. Biomed. Pharmacother. 2003, 57, 274–277. [Google Scholar] [CrossRef]
- Capri, M.; Salvioli, S.; Sevini, F.; Valensin, S.; Celani, L. The Genetics of Human Longevity. Ann. N. Y. Acad. Sci. 2006, 1067, 252–263. [Google Scholar] [CrossRef]
- Scola, L.; Lio, D.; Candore, G.; Forte, G.I.; Crivello, A.; Colonna-Romano, G.; Pes, M.G.; Carru, C.; Ferrucci, L.; Deiana, L.; et al. Analysis of HLA-DRB1, DQA1, DQB1 haplotypes in Sardinian centenarians. Exp. Gerontol. 2008, 43, 114–118. [Google Scholar] [CrossRef][Green Version]
- Brown-Borg, H.M.; Rakoczy, S.G. Glutathione metabolism in long-living Ames dwarf mice. Exp. Gerontol. 2005, 40, 115–120. [Google Scholar] [CrossRef]
- Uthus, E.O.; Brown-Borg, H.M. Methionine flux to transsulfuration is enhanced in the long living Ames dwarf mouse. Mech. Ageing Dev. 2006, 127, 444–450. [Google Scholar] [CrossRef]
- Seshadri, S.; Beiser, A.; Selhub, J.; Jacques, P.F.; Rosenberg, I.H.; D’Agostino, R.B.; Wilson, P.W.; Wolf, P.A. Plasma homocysteine as a risk factor for dementia and Alzheimer’s disease. N. Engl. J. Med. 2002, 346, 476–483. [Google Scholar] [CrossRef]
- Almeida, O.P.; Alfonso, H.; Yeap, B.B.; Hankey, G.; Flicker, L. Complaints of difficulty to fall asleep increase the risk of depression in later life: The health in men study. J. Affect. Disord. 2011, 134, 208–216. [Google Scholar] [CrossRef]
- Wijsman, C.A.; Van Heemst, D.; Rozing, M.P.; Slagboom, P.E.; Beekman, M.; De Craen, A.J.M.; Maier, A.B.; Westendorp, R.G.J.; Blom, H.J.; Mooijaart, S.P. Homocysteine and Familial Longevity: The Leiden Longevity Study. PLoS ONE 2011, 6, e17543. [Google Scholar] [CrossRef]
- Wijsman, C.A.; Rozing, M.P.; Streefland, T.C.M.; le Cessie, S.; Mooijaart, S.P.; Slagboom, P.E.; Westendorp, R.G.J.; Pijl, H.; van Heemst, D.; On behalf of the Leiden Longevity Study Group. Familial longevity is marked by enhanced insulin sensitivity. Aging Cell 2011, 10, 114–121. [Google Scholar] [CrossRef]
- Smetannikova, M.A.; Beliavskaia, V.A.; Smetannikova, N.A.; Savkin, I.V.; Denisova, D.V.; Ustinov, S.N.; Maksimov, V.N.; Shabalin, A.V.; Bolotnova, T.V.; Voevoda, M.I. Functional polymorphism of p53 and CCR5 genes in the long-lived of the Siberian region. Vestnik Rossiiskoi Akademii Meditsinskikh Nauk 2004, 11, 25–28. (In Russian) [Google Scholar]
- van Heemst, D.; Mooijaart, S.P.; Beekman, M.; Schreuder, J.; de Craen, A.J.; Brandt, B.W.; Slagboom, P.E.; Westendorp, R.G. Variation in the human TP53 gene affects old age survival and cancer mortality. Exp. Gerontol. 2005, 40, 11–15. [Google Scholar] [CrossRef]
- Orsted, D.D.; Bojesen, S.E.; Tybjaerg-Hansen, A.; Nordestgaard, B.G. Tumor suppressor p53 Arg-72 Pro polymorphism and longevity, cancer survival, and risk of cancer in the general population. J. Exp. Med. 2007, 204, 1295–1301. [Google Scholar] [CrossRef]
- Feng, Z.; Lin, M.; Wu, R. The regulation of aging and longevity: A new and complex role of p53. Genes Cancer 2011, 2, 443–452. [Google Scholar] [CrossRef]
- Vecchione, C.; Villa, F.; Carrizzo, A.; Spinelli, C.C.; Damato, A.; Ambrosio, M.; Ferrario, A.; Madonna, M.; Uccellatore, A.; Lupini, S.; et al. A rare genetic variant of BPIFB4 predisposes to high blood pressure via impairment of nitric oxide signaling. Nat. Sci. Rep. 2019, 7, 9706. [Google Scholar] [CrossRef]
- Puca, A.A.; Carrizzo, A.; Spinelli, C.; Damato, A.; Ambrosio, M.; Villa, F.; Ferrario, A.; Maciag, A.; Fornai, F.; Lenzi, P.; et al. Single systemic transfer of a human gene associated with exceptional longevity halts the progression of atherosclerosis and inflammation in ApoE knockout mice through a CXCR4-mediated mechanism. Eur. Heart J. 2019, 41, 2487–2497. [Google Scholar] [CrossRef]
- Bocquet-Appel, J.P.; Jacobi, L. Familial trasmission of longevity. Ann. Hum. Biol. 1990, 17, 81–95. [Google Scholar] [CrossRef]
- Herskind, A.M.; McGue, M.; Holm, N.V.; Sorensen, T.I.; Harvald, B.; Vaupel, J.W. The heritability of human longevity, a population-based study of 2872 Danish twins pairs born 1870–1900. Hum. Genet. 1996, 97, 319–323. [Google Scholar] [CrossRef]
- Gavrilov, L.A.; Gavrilova, N.S.; Olshansky, S.J.; Carnes, B.A. Genealogical Data and the Biodemography of Human Longevity. Soc. Biol. 2002, 49, 160–173. [Google Scholar] [CrossRef]
- Gavrilova, N.; Gavrilov, L.A. Data resources for studies on family clustering of human longevity. Demogr. Res. 1999, 1, 4. [Google Scholar] [CrossRef]
- Mitchell, B.D.; Hsueh, W.C.; King, T.M.; Pollin, T.I.; Sorkin, J.; Agarwala, R.; SchaÈffer, A.A.; Shuldiner, A.R. Heritability of life span in the Old Order Amish. Am. J. Med. Genet. 2001, 102, 346–352. [Google Scholar] [CrossRef]
- Hjelmborg, J.V.; Iachine, I.; Skytthe, A.; Vaupel, J.W.; McGue, M.; Koskenvuo, M.; Kaprio, J.; Pedersen, N.L.; Christensen, K. Genetic influence on human lifespan and longevity. Hum. Genet. 2006, 119, 312–321. [Google Scholar] [CrossRef]
- Sebastiani, P.; Perls, T.T. The genetics of extreme longevity: Lessons from the new England centenarian study. Front. Genet. 2012, 3, 277. [Google Scholar] [CrossRef]
- Ruby, J.G.; Wright, K.M.; Rand, K.A.; Kermany, A.; Noto, K.; Curtis, D.; Varner, N.; Garrigan, D.; Slinkov, D.; Dorfman, I.; et al. Estimates of the Heritability of Human Longevity Are Substantially Inflated due to Assortative Mating. Genetics 2018, 210, 1109–1124. [Google Scholar] [CrossRef]
- Kane, A.E.; Sinclair, D.A. Epigenetic changes during aging and their reprogramming potential. Crit. Rev. Biochem. Mol. Biol. 2019, 54, 61–83. [Google Scholar] [CrossRef]
- Benayoun, B.A.; Pollina, E.A.; Brunet, A. Epigenetic regulation of ageing: Linking environmental inputs to genomic stability. Nat. Rev. Mol. Cell Biol. 2015, 16, 593–610. [Google Scholar] [CrossRef]
- Brian, J.M.; Willcox, B.J.; Donlon, T.A. Genetic and epigenetic regulation of human aging and longevity. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 1718–1744. [Google Scholar]
- Aliberti, S.M.; De Caro, F.; Funk, R.H.W.; Schiavo, L.; Gonnella, J.; Boccia, G.; Capunzo, M. Extreme Longevity: Analysis of the Direct or Indirect Influence of Environmental Factors on Old, Nonagenarians, and Centenarians in Cilento, Italy. Int. J. Environ. Res. Public Health 2022, 19, 1589. [Google Scholar] [CrossRef]
- Darviri, C.; Demakakos, P.; Tigani, X.; Charizani, F.; Tsiou, C. Psychosocial dimensions of exceptional longevity: A qualitative exploration of centenarians’ experiences, personality, and Life strategies. Int. J. Aging Hum. Dev. 2009, 69, 101–118. [Google Scholar] [CrossRef]
- Scelzo, A.; Di Somma, S.; Antonini, P.; Montross, L.P.; Schork, N.; Brenner, D.; Jeste, D.V. Mixed-methods quantitative–qualitative study of 29 nonagenarians and centenarians in rural Southern Italy: Focus on positive psychological traits. Int. Psychogeriatr. 2017, 30, 31–38. [Google Scholar] [CrossRef]
- Pizza, V.; Antonini, P.; Marino, R.; D’Arena, G.; Lucibello, S.G.; Rizzo, M.; Brenner, D.A.; Jeste, D.V.; Di Somma, S. Cognitive Health of Nonagenarians in Southern Italy: A Descriptive Analysis from a Cross-Sectional, Home-Based Pilot Study of Exceptional Longevity. Medicina 2020, 56, 218. [Google Scholar] [CrossRef]
- Franceschi, C.; Motta, L.; Motta, M.; Malaguarnera, M.; Capri, M.; Vasto, S.; Candore, G.; Caruso, C.; IMUSCE. The extreme longevity: The state of the art in Italy. Exp. Gerontol. 2008, 43, 45–52. [Google Scholar] [CrossRef]
- Fara, G.M. Nutrition between sustainability and quality. Ann. Ig. 2015, 27, 693–704. [Google Scholar]
- Chan, Y.C.; Suzuki, M.; Yamamoto, S. Dietary, anthropometric, hematological and biochemical assessment of the nutritional status of centenarians and elderly people in Okinawa, Japan. J. Am. Coll. Nutr. 1997, 16, 229–235. [Google Scholar] [CrossRef]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench 2013, 6, 14–17. [Google Scholar]
- Aliberti, S.M.; Schiavo, L.; Boccia, G.; Santoro, E.; Franci, G.; Ruggiero, A.; De Caro, F.; Capunzo, M. Gender and AB0 blood type difference in a unicentric group of university Professor in southern Italy who received the Vaxzevria COVID 19 vaccine: A cross sectional survey of vaccine side effects, attitudes and hesitation. Vaccines 2022, 10, 373. [Google Scholar] [CrossRef]
- Bolarinwa, O.A. Principles and Methods of Validity and Reliability Testing of Questionnaires used in Socila and Health Science Researches. Niger. Postgrad. Med. J. 2015, 22, 195–201. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Background Document to WHO Strategy Paper for Europe; Arbetsrapport No. 14; Institute for Futures Studies: Stockholm, Sweden, 2007. [Google Scholar]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; Wiley: New York, NY, USA, 2000. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 16.1; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- Evert, J.; Lawler, E.; Bogan, H.; Perls, T. Morbidity Profiles of Centenarians: Survivors, Delayers, and Escapers. J. Gerontol. Med. Sci. 2003, 58, 232–237. [Google Scholar] [CrossRef]
- von Berenberg, P.; Dräger, D.; Zahn, T.; Neuwirth, J.; Kuhlmey, A.; Gellert, P. Chronic conditions and use of health care service among German centenarians. Age Ageing 2017, 46, 939–945. [Google Scholar] [CrossRef]
- Abete, P.; Testa, G.; Della Morte, D.; Mazzella, F.; Galizia, G.; D’ambrosio, D.; Visconti, C.; Gargiulo, G.; Cacciatore, F.; Rengo, F. La comorbilità nell’anziano: Epidemiologia e caratteristiche cliniche. G Gerontol. 2004, 52, 267–272. [Google Scholar]
- Aliberti, S.M. Produzioni locali e tradizioni gastronomiche: Recupero e valorizzazione. In Tra Vulnerabilità e Resilienza. Immagini di Transizione Socio-Ecologica in Un’area Della Campania; Ammaturo, N., Ed.; Loffredo Editore: Napoli, Italy, 2012. [Google Scholar]
- Trichopoulou, A.; Martínez-González, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef]
- Buckland, G.; Gonzalez, C.A. The role of olive oil in disease prevention: A focus on the recent epidemiological evidence from cohort studies and dietary intervention trials. Br. J. Nutr. 2015, 113 (Suppl. S2), S94–S101. [Google Scholar] [CrossRef]
- De Santis, S.; Cariello, M.; Piccinin, E.; Sabbà, C.; Moschetta, A. Extra Virgin Olive Oil: Lesson from Nutrigenomics. Nutrients 2019, 11, 2085. [Google Scholar] [CrossRef]
- Yubero-Serrano, E.M.; Lopez-Moreno, J.; Gomez-Delgado, F.; Lopez-Miranda, J. Extra virgin olive oil: More than a healthy fat. Eur. J. Clin. Nutr. 2019, 72, 8–17. [Google Scholar] [CrossRef]
- Siervo, M.; Shannon, O.M.; Llewellyn, D.J.; Stephan, B.C.; Fontana, L. Mediterranean diet and cognitive function: From methodology to mechanisms of action. Free Radic. Biol. Med. 2021, 176, 105–117. [Google Scholar] [CrossRef]
- Dumic, A.; Miskulin, M.; Pavlovic, N.; Orkic, Z.; Bilic-Kirin, V.; Miskulin, I. The Nutrition Knowledge of Croatian General Practitioners. J. Clin. Med. 2018, 7, 178. [Google Scholar] [CrossRef]
- Longo, V. Dieta e Decalogo per una Vita Sana e Lunga longevità. Longevità ai Tempi del COVID; Vita Editore: Milano, Italy, 2020. [Google Scholar]
- Hem, J.D. Study and Interpretation of the Chemical Characteristics of Natural Water; University Press of the Pacific: Honolulu, HI, USA, 1959. [Google Scholar]
- Keller, W.D. Drinking water: A geochemical factor in human health. Geol. Soc. Am. Bull. 1978, 89, 334–336. [Google Scholar] [CrossRef]
- Lv, J.; Wang, W.; Li, Y. Effects of environmental factors on the longevous people in China. Arch. Gerontol. Geriatr. 2011, 53, 200–205. [Google Scholar] [CrossRef]
- Mitchell, P.B.; Harvey, S.B. Depression and the older medical patient—When and how to intervene. Maturitas 2014, 79, 153–159. [Google Scholar] [CrossRef]
- Aliberti, S.M. Le badanti e la cura domiciliare: Come tassello dei servizi integrati del welfare locale. In Narrazioni di salute nella Web Society; Corposanto, C., Ed.; Rubbettino Editore: Soveria Mannelli, Italy, 2017. [Google Scholar]
- Karagiannis, T.; Maio, V.; Del Canale, M.; Fabi, M.; Brambilla, A.; Del Canale, S. The Transformation of Primary Care: Are General Practitioners Ready? Am. J. Med. Qual. 2014, 29, 93–94. [Google Scholar] [CrossRef]
- Morselli, B.; Cilona, C.; Misale, F. Medicina Narrative. Temi, Esperienza e Riflessioni; Tre-Press: Roma, Italy, 2017. [Google Scholar]
- Hojat, M.; Louis, D.Z.; Maio, V.; Gonnella, J. Empathy and Health Care Quality. Am. J. Med. Qual. 2013, 28, 6–7. [Google Scholar] [CrossRef]
 protective factors that are statistically significant;
protective factors that are statistically significant;  risk factors that are statistically significant;
risk factors that are statistically significant;  factors that are not statistically significant;
factors that are not statistically significant;  positively correlated factors;
positively correlated factors;  negatively correlated factors. VFF—variety and freshness of foods; EM—consumption of ready-to-eat meals; BW—bottled water; TW—tap water; MC—meat consumption; FC—fish consumption; SD—specific diets; OW—overweight; D—use of drugs; T—tobacco; A—alcohol; AA—alcohol addiction; SA—smoking addiction; P—psychosomatic problems; D—depression; GLL—centenarians grateful for a long life; BnD—centenarians suffered the burden of not dying. For more information look at Table 2.
negatively correlated factors. VFF—variety and freshness of foods; EM—consumption of ready-to-eat meals; BW—bottled water; TW—tap water; MC—meat consumption; FC—fish consumption; SD—specific diets; OW—overweight; D—use of drugs; T—tobacco; A—alcohol; AA—alcohol addiction; SA—smoking addiction; P—psychosomatic problems; D—depression; GLL—centenarians grateful for a long life; BnD—centenarians suffered the burden of not dying. For more information look at Table 2.
 protective factors that are statistically significant;
protective factors that are statistically significant;  risk factors that are statistically significant;
risk factors that are statistically significant;  factors that are not statistically significant;
factors that are not statistically significant;  positively correlated factors;
positively correlated factors;  negatively correlated factors. VFF—variety and freshness of foods; EM—consumption of ready-to-eat meals; BW—bottled water; TW—tap water; MC—meat consumption; FC—fish consumption; SD—specific diets; OW—overweight; D—use of drugs; T—tobacco; A—alcohol; AA—alcohol addiction; SA—smoking addiction; P—psychosomatic problems; D—depression; GLL—centenarians grateful for a long life; BnD—centenarians suffered the burden of not dying. For more information look at Table 2.
negatively correlated factors. VFF—variety and freshness of foods; EM—consumption of ready-to-eat meals; BW—bottled water; TW—tap water; MC—meat consumption; FC—fish consumption; SD—specific diets; OW—overweight; D—use of drugs; T—tobacco; A—alcohol; AA—alcohol addiction; SA—smoking addiction; P—psychosomatic problems; D—depression; GLL—centenarians grateful for a long life; BnD—centenarians suffered the burden of not dying. For more information look at Table 2.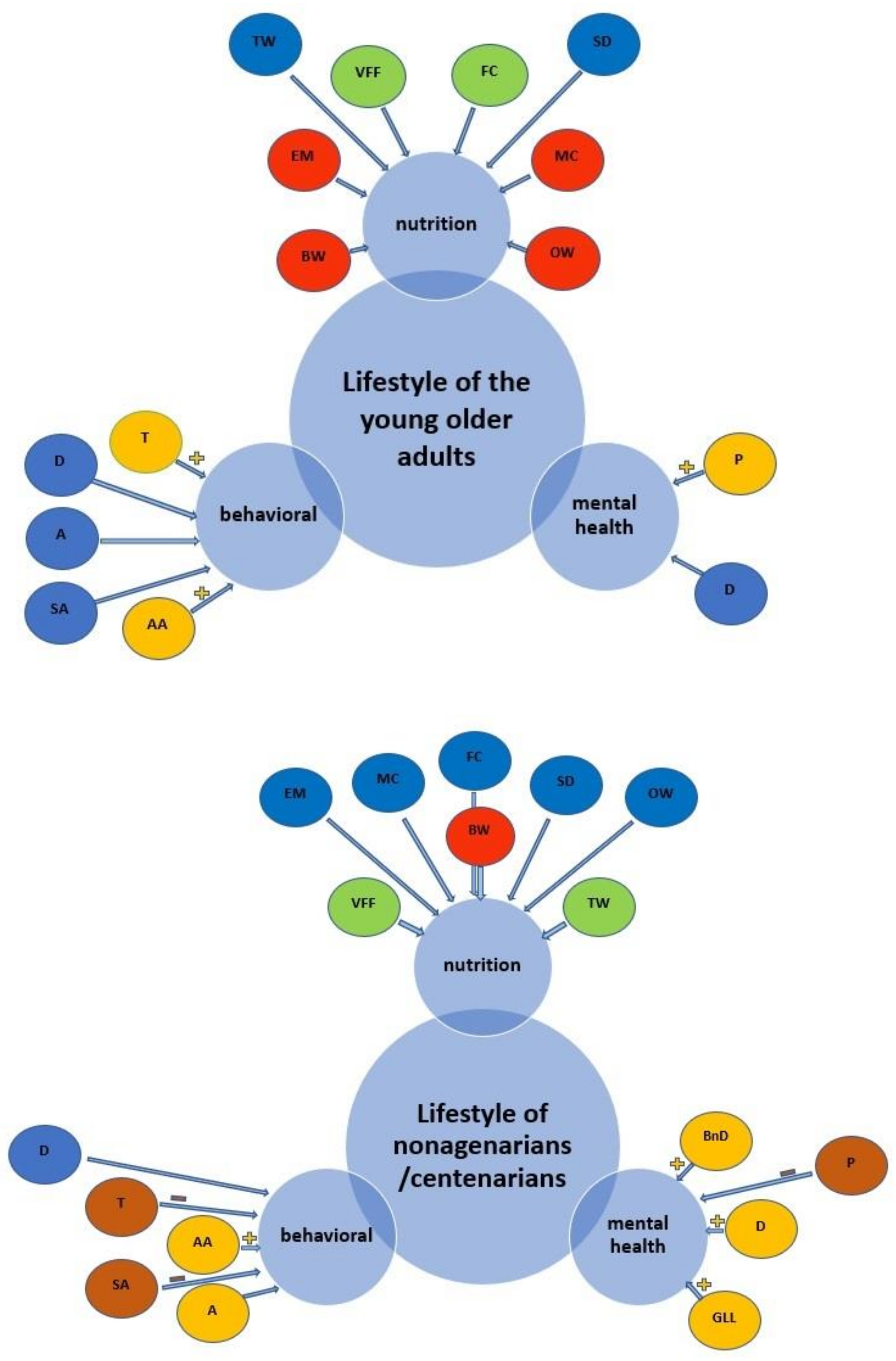
| Model 1 | Younger Older Adults (Outcome) Log Likelihood= −8822.6, x2 = 2873.08 (15 df), p < 0.001 | Nonagenarians/Centenarians (Outcome) Log Likelihood= −7728.0, x2 = 3632.16 (16 df), p < 0.001 | ||||
| Clinical Status Variables * | IRR | 95% CI | p | IRR | 95% CI | p |
| Completely healthy | 1.28 | 1.24–1.31 | <0.001 | 0.90 | 0.84–0.97 | 0.009 |
| Little limited ability | 0.98 | 0.96–0.99 | 0.024 | 1.31 | 1.25–1.37 | <0.001 |
| Clearly marked by diseases | 0.96 | 0.94–0.98 | <0.001 | 1.22 | 1.17–1.27 | <0.001 |
| Suffer a lot | 1.11 | 1.08–1.14 | <0.001 | 1.42 | 1.36–1.48 | <0.001 |
| Cardiovascular diseases | 1.04 | 1.02–1.06 | <0.001 | 0.82 | 0.77–0.86 | <0.001 |
| Respiratory diseases | 1.11 | 1.09–1.13 | <0.001 | 1.24 | 1.19–1.29 | <0.001 |
| Blood diseases | 0.99 | 0.97–1.01 | 0.634 | 1.40 | 1.34–1.45 | <0.001 |
| Rheumatic diseases | 1.06 | 1.05 - 1.08 | <0.001 | 1.20 | 1.15–1.25 | <0.001 |
| Metabolic diseases | 0.93 | 0.91–0.95 | <0.001 | 1.15 | 1.10–1.19 | <0.001 |
| Gastrointestinal diseases | 1.14 | 1.12–1.16 | <0.001 | 1.23 | 1.18–1.29 | <0.001 |
| Neurological diseases | 1.11 | 1.09–1.13 | <0.001 | 1.87 | 1.77–1.98 | <0.001 |
| Biliary diseases | 0.89 | 0.87 - 0.92 | <0.001 | 0.44 | 0.41–0.48 | <0.001 |
| Oncological diseases | 1.01 | 0.99–1.02 | 0.136 | 1.09 | 1.03–1.14 | 0.001 |
| Other diseases | 1.20 | 1.17–1.23 | <0.001 | 1.76 | 1.67–1.86 | <0.001 |
| Comorbidities | 1.00 | 1.00–1.00 | <0.001 | 1.00 | 1.00–1.00 | <0.001 |
| Model 2 | Log Likelihood = −3212.6, x2 = 611.68 (5 df), p < 0.001 | Log Likelihood = −2212.1, x2 = 396.84 (6 df), p < 0.001 | ||||
| Asymptomatic | 1.00 | 1.00–1.00 | <0.001 | 0.99 | 0.99–1.00 | 0.286 |
| Paucisymptomatic | 0.99 | 0.99–0.99 | <0.001 | 1.00 | 1.00–1.00 | <0.001 |
| Symptomatic | 1.00 | 1.00–1.00 | 0.015 | 0.99 | 0.99–0.99 | <0.001 |
| Symptomatic with severe disease | 0.99 | 0.99–0.99 | <0.001 | 1.01 | 1.01–1.02 | <0.001 |
| Deaths | 1.01 | 1.01–1.01 | <0.001 | 0.99 | 0.98–0.99 | 0.009 |
| Model 3 | Younger Older Adults (Outcome) Log Likelihood= −10343.7, x2 = 590.11 (7 df), p < 0.001 | Nonagenarians/Centenarians (Outcome) Log Likelihood= −7480.3, x2 = 2687.25 (11 df), p < 0.001 | ||||
| Behavioral and Mental Health Variables * | IRR | 95% CI | p | IRR | 95% CI | p |
| Use of drugs | 1.00 | 0.99–1.00 | 0.070 | 1.00 | 0.99–1.00 | 0.127 |
| Tobacco | 1.00 | 1.00–1.00 | <0.001 | 0.99 | 0.99–1.00 | <0.001 |
| Alcohol | 0.99 | 0.99–1.00 | 0.212 | 1.00 | 1.00–1.00 | 0.001 |
| Alcohol addition | 1.00 | 1.00–1.00 | <0.001 | 1.06 | 1.05–1.07 | <0.001 |
| Smoking addition | 1.00 | 1.00–1.00 | 0.780 | 0.99 | 0.99–0.99 | <0.001 |
| Psychosomatic problems | 1.00 | 1.00–1.00 | <0.001 | 0.99 | 0.99–0.99 | <0.001 |
| Depression | 0.99 | 0.99–1.00 | 0.458 | 1.01 | 1.01–1.01 | <0.001 |
| Nonagenarians/centenarians grateful for a long life | ||||||
| - Undecided | 1 a | 1 a | 1 a | |||
| - No | 1.66 | 1.58–1.75 | <0.001 | |||
| - Yes | 0.97 | 0.91–1.04 | 0.468 | |||
| Nonagenarians/centenarians suffered the burden of not dying | ||||||
| - Undecided | - | - | - | 1 a | 1 a | 1 a |
| - No | 1.06 | 1.01–1.11 | 0.006 | |||
| - Yes | 0.57 | 0.53–0.61 | <0.001 | |||
| Model 4 | Importance of Nutrition in YOA (Outcome) Log Likelihood= −8822.6, x2 =2873.08 (15 df), p < 0.001 | Importance of Nutrition in N/C (Outcome) Log Likelihood= −7728.0, x2 =3632.16 (16 df), p < 0.001 | ||||
| Nutritional Variables * | OR | 95% CI | p | OR | 95% CI | p |
| Variety and freshness of foods | 0.08 | 0.06–0.12 | <0.001 | 0.37 | 0.27–0.50 | <0.001 |
| Consumptions of ready to eat meals | 3.06 | 2.18–4.28 | <0.001 | 0.94 | 0.70–1.28 | 0.72 |
| Bottled water | 1.67 | 1.15–2.41 | 0.006 | 6.63 | 4.27–10.30 | <0.001 |
| Tap water | 1.42 | 0.97–2.07 | 0.06 | 0.40 | 0.27–0.62 | <0.001 |
| Meat consumption | 1.79 | 1.19 -2.68 | 0.004 | 0.94 | 0.63–1.38 | 0.75 |
| Fish consumption | 0.09 | 0.04–0.17 | <0.001 | 1.44 | 0.90–2.31 | 0.12 |
| Specific diets | 0.62 | 0.31–1.21 | 0.16 | 1.00 | 1.00–1.01 | 0.03 |
| Overweight | 1.01 | 1.01–1.02 | <0.001 | 1.01 | 1.00–1.02 | 0.008 |
| Model 5 | Young Older Adults (Outcome) Log Likelihood= −6680.1, x2 =1059.75 (12 df), p < 0.001 | Nonagenarians/Centenarians (Outcome) Log Likelihood= −6778.0, x2 =756.26 (11 df), p < 0.001 | ||||
|---|---|---|---|---|---|---|
| Social and Community Gradient Variables * | IRR | 95% CI | p | IRR | 95% CI | p |
| Living with family member | 1.00 | 0.99–1.00 | 0.610 | 0.99 | 0.99–0.99 | <0.001 |
| Living alone with family support | 0.99 | 0.99–0.99 | <0.001 | 1.00 | 0.99–1.00 | 0.160 |
| Living alone with third-party support (neighbors, caregivers) | 1.00 | 1.00–1.00 | <0.001 | 0.99 | 0.99–0.99 | <0.001 |
| Living in nursing homes or shared apartments | 1.00 | 0.99–1.00 | 0.971 | 1.00 | 1.00–1.00 | <0.001 |
| Continuing in professional positions | 0.93 | 0.87–0.99 | 0.042 | 0.59 | 0.51–0.68 | <0.001 |
| Honorary achievement | 0.93 | 0.91–0.95 | <0.001 | 0.75 | 0.71–0.79 | <0.001 |
| Physical activities (gardening, yoga, sports, etc.) | 1.48 | 1.42–1.54 | <0.001 | 0.69 | 0.60–0.78 | <0.001 |
| Cultural activities | 0.66 | 0.59–0.72 | <0.001 | 0.59 | 0.53–0.66 | <0.001 |
| Social life | 1.21 | 1.11–1.31 | <0.001 | 0.32 | 0.27–0.40 | <0.001 |
| Parish activities | 0.82 | 0.79–0.84 | <0.001 | 1.28 | 1.20–1.36 | <0.001 |
| Bar meetings | 1.04 | 1.02–1.07 | <0.001 | 1.40 | 1.32–1.50 | <0.001 |
| Association activities | 0.92 | 0.87–0.96 | 0.001 | 1.14 | 1.03–1.27 | 0.009 |
| Model 6 | Male and Female Physicians (Outcome) | ||
|---|---|---|---|
| Structural Variables of Health * | OR | 95% CI | p |
| Hospital equipment | |||
| good | 1 a | ||
| so-so | 1.63 | 1.09–2.43 | 0.015 |
| poor | 2.49 | 1.50–4.14 | <0.001 |
| Cooperations between institutions | |||
| good | 1 a | ||
| so-so | 0.25 | 0.13–0.47 | <0.001 |
| poor | 0.05 | 0.02—0.11 | <0.001 |
| Public health information | |||
| good | 1 a | ||
| so-so | 1.09 | 0.69–1.71 | 0.701 |
| poor | 1.04 | 0.60–1.79 | 0.888 |
| Cooperation between clinics and primary care physicians | |||
| good | 1 a | ||
| so-so | 5.45 | 2.93–10.16 | <0.001 |
| poor | 25.76 | 12.32–53.84 | <0.001 |
| Cooperations between clinics and rehabilitation facilities | |||
| good | 1 a | ||
| so-so | 0.58 | 0.34–0.97 | 0.041 |
| poor | 0.37 | 0.19–0.72 | 0.004 |
| Cooperations between hospitals and specialty clinics | |||
| good | 1 a | ||
| so-so | 0.44 | 0.25–0.77 | 0.004 |
| poor | 0.58 | 0.29–1.15 | 0.124 |
| Self-help group | |||
| good | 1 a | ||
| so-so | 1.21 | 0.64–2.26 | 0.544 |
| poor | 0.90 | 0.46–1.76 | 0.773 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aliberti, S.M.; Funk, R.H.W.; Schiavo, L.; Giudice, A.; Ciaglia, E.; Puca, A.A.; Gonnella, J.; Capunzo, M. Clinical Status, Nutritional Behavior, and Lifestyle, and Determinants of Community Well-Being of Patients from the Perspective of Physicians: A Cross-Sectional Study of Young Older Adults, Nonagenarians, and Centenarians in Salerno and Province, Italy. Nutrients 2022, 14, 3665. https://doi.org/10.3390/nu14173665
Aliberti SM, Funk RHW, Schiavo L, Giudice A, Ciaglia E, Puca AA, Gonnella J, Capunzo M. Clinical Status, Nutritional Behavior, and Lifestyle, and Determinants of Community Well-Being of Patients from the Perspective of Physicians: A Cross-Sectional Study of Young Older Adults, Nonagenarians, and Centenarians in Salerno and Province, Italy. Nutrients. 2022; 14(17):3665. https://doi.org/10.3390/nu14173665
Chicago/Turabian StyleAliberti, Silvana Mirella, Richard H. W. Funk, Luigi Schiavo, Aldo Giudice, Elena Ciaglia, Annibale Alessandro Puca, Joseph Gonnella, and Mario Capunzo. 2022. "Clinical Status, Nutritional Behavior, and Lifestyle, and Determinants of Community Well-Being of Patients from the Perspective of Physicians: A Cross-Sectional Study of Young Older Adults, Nonagenarians, and Centenarians in Salerno and Province, Italy" Nutrients 14, no. 17: 3665. https://doi.org/10.3390/nu14173665
APA StyleAliberti, S. M., Funk, R. H. W., Schiavo, L., Giudice, A., Ciaglia, E., Puca, A. A., Gonnella, J., & Capunzo, M. (2022). Clinical Status, Nutritional Behavior, and Lifestyle, and Determinants of Community Well-Being of Patients from the Perspective of Physicians: A Cross-Sectional Study of Young Older Adults, Nonagenarians, and Centenarians in Salerno and Province, Italy. Nutrients, 14(17), 3665. https://doi.org/10.3390/nu14173665