The Effect of Exogenous Melatonin on Eating Habits of Female Night Workers with Excessive Weight
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Sampling
2.2. Study Protocol
2.3. Study Variables
2.3.1. Outcomes
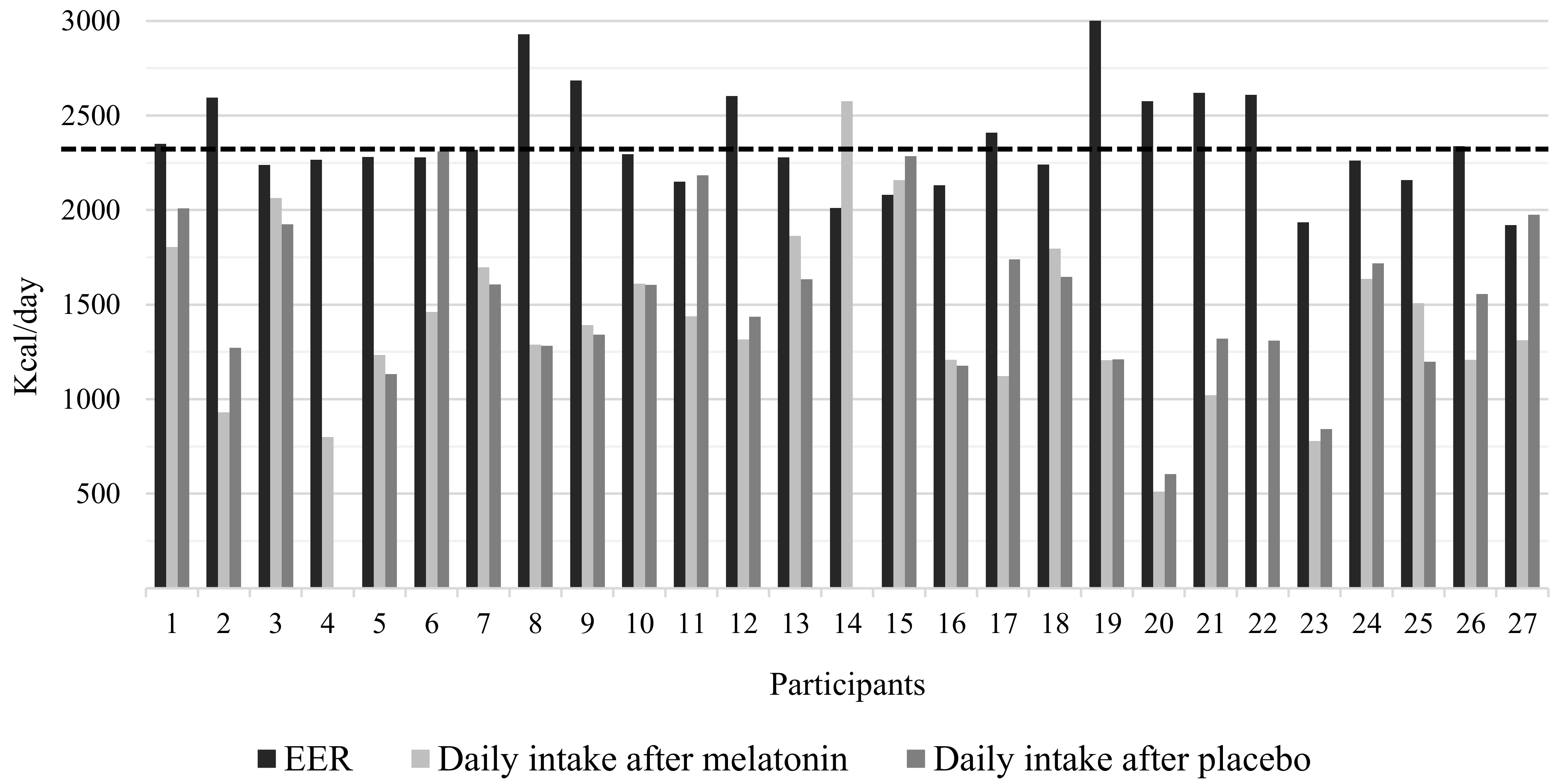
- Quantitative aspect of the diet: Total energy intake and macronutrient distribution
- Qualitative aspect of the diet: Food classification according to processing
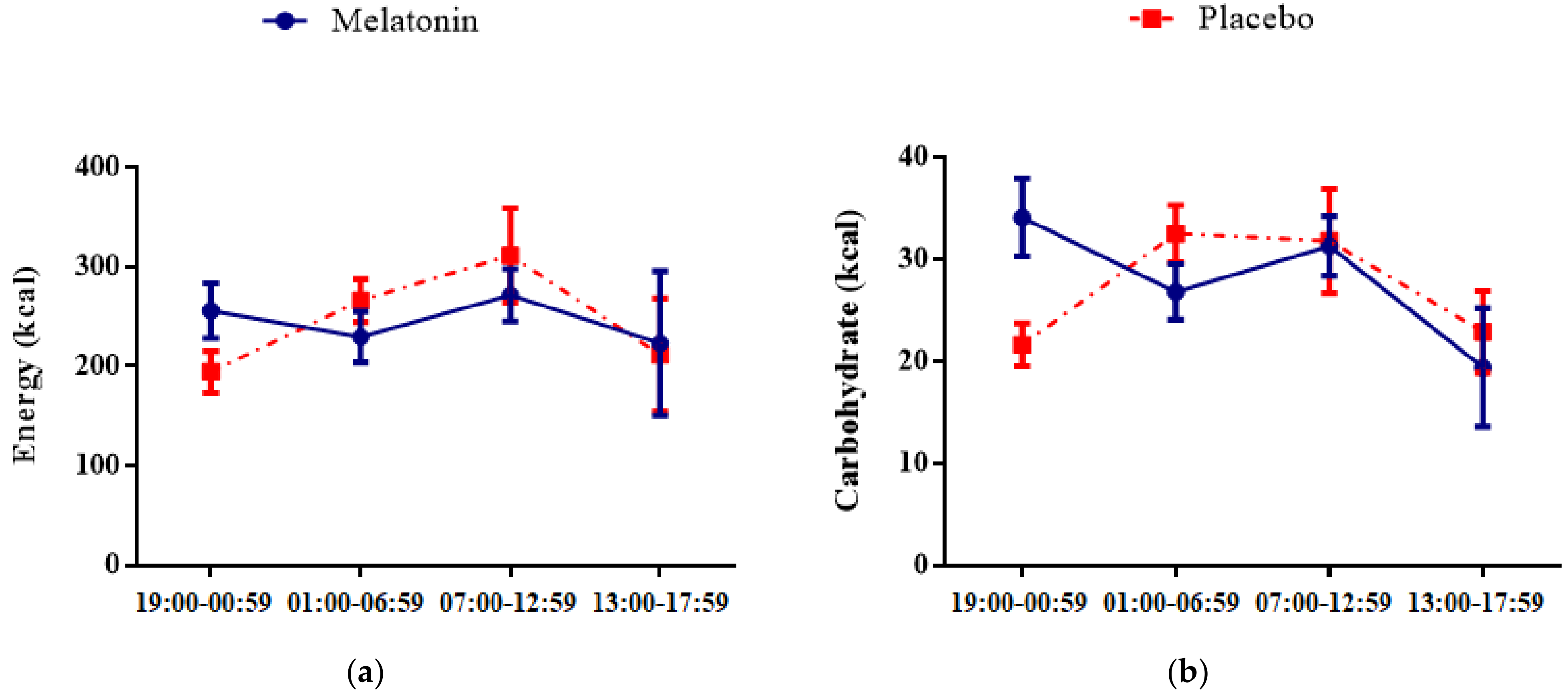
- Temporal distribution of food intake
2.3.2. Independent Variables
- Composite Phase Deviations
- Chronotype
2.3.3. Descriptive Variables
2.4. Statistical Analysis
2.5. Ethical Aspects
3. Results
4. Discussion
4.1. No Effects of Melatonin on Energy, Quali/Quantitative Intake and Meal Timing
4.2. No Effects of Melatonin Supplementation on Food Intake in Association with Circadian Misalignment or Chronotype
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buijs, R.M.; Kalsbeek, A. Hypothalamic integration of central and peripheral clocks. Nat. Rev. Neurosci. 2001, 2, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, U. Timing to Perfection: The Biology of Central and Peripheral Circadian Clocks. Neuron 2012, 74, 246–260. [Google Scholar] [CrossRef] [PubMed]
- Bodur, M.; Baspinar, B.; Özçelik, A.Ö. A cross-sectional evaluation of the relationship between social jetlag and diet quality. Chronobiol. Int. 2021, 38, 1557–1568. [Google Scholar] [CrossRef]
- Rusu, A.; Ciobanu, D.; Vonica, C.L.; Bala, C.; Mocan, A.; Sima, D. Chronic disruption of circadian rhythm with mistimed sleep and appetite-an exploratory research. Chronobiol. Int. 2021, 38, 807–816. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Merino, J.; Lane, J.M.; Song, Y.; Smith, C.E.; Tanaka, T.; McKeown, N.M.; Tucker, C.; Sun, D.; Bartz, T.M.; et al. Genome-wide association study of breakfast skipping links clock regulation with food timing. Am. J. Clin. Nutr. 2019, 110, 473–484. [Google Scholar] [CrossRef]
- Richter, J.; Herzog, N.; Janka, S.; Baumann, T.; Kistenmacher, A.; Oltmanns, K.M. Twice as High Diet-Induced Thermogenesis after Breakfast vs Dinner on High-Calorie as Well as Low-Calorie Meals. Int. J. Clin. Endocrinol. Metab. 2020, 105, e211–e221. [Google Scholar] [CrossRef]
- Atkinson, G.; Fullick, S.; Grindey, C.; Maclarem, D. Exercise, energy balance and the shift worker. Sports Med. 2008, 38, 671–685. [Google Scholar] [CrossRef]
- Akerstedt, T.; Wright, K.P., Jr. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med. Clin. 2009, 4, 257–271. [Google Scholar] [CrossRef]
- Alterman, T.; Luckhaupt, S.E.; Dahlhamer, J.M.; Ward, B.W.; Calvert, G.M. Prevalence rates of work organization characteristics among workers in the U.S.: Data from the 2010 National Health Interview Survey. Am. J. Ind. Med. 2013, 56, 647–659. [Google Scholar] [CrossRef]
- Fischer, F.M.; Moreno, C.R.C.; Rotenberg, L. Trabalho em Turnos e Noturno na Sociedade 24 Horas; Atheneu: São Paulo, Brazil, 2004. [Google Scholar]
- Statistics Canada. Work-life balance of shift workers. Perspectives 2008, 9, 5–16. [Google Scholar]
- Zerón-Rugerio, M.; Hernáez, Á.; Porras-Loaiza, A.P.; Cambras, T.; Izquierdo-Pulido, M. Eating Jet Lag: A Marker of the Variability in Meal Timing and Its Association with Body Mass Index. Nutrients 2019, 11, 2980. [Google Scholar] [CrossRef] [PubMed]
- McHill, A.W.; Melanson, E.L.; Higgins, J.; Connick, E.; Moehlman, T.M.; Stothard, E.R.; Wright, K.P., Jr. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc. Natl. Acad. Sci. USA 2014, 111, 17302–17307. [Google Scholar] [CrossRef]
- Baron, K.G.; Reid, K.J.; Kern, A.S.; Zee, P.C. Role of sleep timing in caloric intake and BMI. Obesity 2011, 19, 1374–1381. [Google Scholar] [CrossRef] [PubMed]
- Maukonen, M.; Kanerva, N.; Partonen, T.; Kronholm, E.; Tapanainen, H.; Kontto, J.; Männistö, S. Chronotype differences in timing of energy and macronutrient intakes: A population-based study in adults. Obesity 2017, 25, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Mazri, F.H.; Manaf, Z.A.; Shahar, S.; Ludin, A.F.M. The Association between Chronotype and Dietary Pattern among Adults: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 17, 68. [Google Scholar] [CrossRef]
- Hulsegge, G.; Picavet, H.S.J.; van der Beek, A.J.; Verschuren, W.M.M.; Twisk, J.W.; Proper, K.I. Shift work, chronotype and the risk of cardiometabolic risk factors. Eur. J. Public Health 2019, 29, 128–134. [Google Scholar] [CrossRef]
- Vetter, C. Circadian disruption: What do we actually mean? Eur. J. Neurosci. 2020, 51, 531–550. [Google Scholar] [CrossRef]
- Phoi, Y.Y.; Rogers, M.; Bonham, M.P.; Dorrian, J.; Coates, A.M. A scoping review of chronotype and temporal patterns of eating of adults: Tools used, findings, and future directions. Nutr. Res. Rev. 2021, 35, 112–135. [Google Scholar] [CrossRef]
- Amaral, F.G.; Cipolla-Neto, J. A brief review about melatonin, a pineal hormone. Arch. Endocrinol. Metab. 2018, 62, 472–479. [Google Scholar] [CrossRef]
- Garaulet, M.; Qian, J.; Florez, J.C.; Arendt, J.; Saxena, R.; Scheer, F.A.J.L. Melatonin Effects on Glucose Metabolism: Time to Unlock the Controversy. Trends Endocrinol. Metab. 2020, 31, 192–204. [Google Scholar] [CrossRef]
- Sack, R.L.; Lewy, A.J. Melatonin as a chronobiotic: Treatment of circadian desynchrony in night workers and the blind. J. Biol. Rhythm. 1997, 12, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Folkard, S.; Arendt, J.; Clark, M. Can melatonin improve shift workers’ tolerance of the night shift? Some preliminary findings. Chronobiol. Int. 1993, 10, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Marqueze, E.C.; Nogueira, L.F.R.; Vetter, C.; Skene, D.J.; Cipolla-Neto, J.; Moreno, C.R.C. Exogenous melatonin decreases circadian misalignment and body weight among early types. J. Pineal Res. 2021, 71, e12750. [Google Scholar] [CrossRef] [PubMed]
- Isherwood, C.M.; van der Veen, D.R.; Johnston, J.D.; Skene, D.J. Twenty-four-hour rhythmicity of circulating metabolites: Effect of body mass and type 2 diabetes. FASEB 2017, 31, 5557–5567. [Google Scholar] [CrossRef]
- Wehrens, S.M.T.; Christou, S.; Isherwood, C.; Middleton, B.; Gibbs, M.A.; Archer, S.N.; Skene, D.J.; Johnston, J.D. Meal Timing Regulates the Human Circadian System. Curr. Biol. 2017, 27, 1768–1775.e3. [Google Scholar] [CrossRef]
- Silva, L.E.S.; Oliveira, M.M.; Stopa, S.R.; Gouvea, E.C.D.P.; Ferreira, K.R.D.; Santos, R.O.; Valença Neto, P.F.; Macário, E.M.; Sardinha, L.M.V. Temporal trend of overweight and obesity prevalence among Brazilian adults, according to sociodemographic characteristics, 2006–2019. Epidemiol. Serv. Saude 2021, 30, e2020294. [Google Scholar] [CrossRef]
- ASchwiter, K.; Nentwich, J.; Keller, M. Male privilege revisited: How men in female-dominated occupations notice and actively reframe privilege. Gender Work Organ. 2021, 28, 2199–2215. [Google Scholar] [CrossRef]
- Emens, J.S.; Burgess, H.J. Effect of Light and Melatonin and Other Melatonin Receptor Agonists on Human Circadian Physiology. Sleep Med. Clin. 2015, 10, 435–453. [Google Scholar] [CrossRef]
- Ma, X.; Idle, J.R.; Krausz, K.W.; Gonzalez, F.J. Metabolism of melatonin by human cytochromes p450. Drug Metab. Dispos. 2005, 33, 489–494. [Google Scholar] [CrossRef]
- Pinheiro, A.B.V.; Lacerda, E.M.A.; Benzecry, E.H.; Gomes, M.C.S.; Costa, V.M. Tabela Para Avaliação de Consumo Alimentar em Medidas Caseiras, 4th ed.; Atheneu: São Paulo, Brazil, 2000. [Google Scholar]
- NEPA-UNICAMP. Tabela Brasileira de Composição de Alimentos-TACO, 4th ed.; NEPA-UNICAMP: Campinas, Brazil, 2011. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; Louzada, M.L.C.; Machado, P.P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; FAO: Rome, Italy, 2019. [Google Scholar]
- Fischer, D.; Vetter, C.; Roenneberg, T. A novel method to visualize and quantify circadian misalignment. Sci. Rep. 2016, 6, 38601. [Google Scholar] [CrossRef]
- Juda, M.; Vetter, C.; Roenneberg, T. The Munich ChronoType Questionnaire for shift-workers (MCTQshift). J. Biol. Rhythm. 2013, 28, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Books: Champaign, IL, USA, 1988. [Google Scholar]
- Trumbo, P.; Schlicker, S.; Yates, A.A.; Poos, M.; Food and Nutrition Board of the Institute of Medicine; The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J. Am. Diet. Assoc. 2002, 102, 1621–1630. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; for the CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. PLoS Med. 2010, 7, e1000251. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, L.F.R.; Marqueze, E.C. Effects of melatonin supplementation on eating habits and appetite-regulating hormones: A systematic review of randomized controlled clinical and preclinical trials. Chronobiol. Int. 2021, 38, 1089–1102. [Google Scholar] [CrossRef]
- Bahrami, M.; Cheraghpour, M.; Jafarirad, S.; Avalinejad, P.; Cheraghian, B. The role of melatonin supplement in metabolic syndrome: A randomized double blind clinical trial. Food Sci. Nutr. 2019, 49, 965–977. [Google Scholar] [CrossRef]
- Frank, S.; Christopher, J.M.; Steven, A.S. The internal circadian clock increases hunger and appetite in the evening independent of food intake and other behaviors. Obesity 2013, 21, 421–423. [Google Scholar]
- Della Torre, S.B.; Wild, P.; Dorribo, V.; Danuser, B.; Amati, F. Energy, nutrient and food intakes of male shift workers vary according to the schedule type but not the number of nights worked. Nutrients 2020, 12, 919. [Google Scholar] [CrossRef]
- Silva, F.M.; Giatti, L.; Figueiredo, R.C.; Molina, M.C.B.; Cardoso, L.O.; Duncan, B.B.; Barreto, S.M. Consumption of ultra-processed food and obesity: Cross sectional results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort (2008–2010). Public Health Nutr. 2018, 21, 2271–2279. [Google Scholar] [CrossRef]
- Shechter, A.; O’Keeffe, M.; Roberts, A.L.; Zammit, G.K.; Choudhury, A.R.; St-Onge, M.P. Alterations in sleep architecture in response to experimental sleep curtailment are associated with signs of positive energy balance. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2012, 303, R883–R889. [Google Scholar] [CrossRef]
- Gupta, C.C.; Coates, A.M.; Dorrian, J.; Banks, S. The factors influencing the eating behaviour of shiftworkers: What, when, where and why. Ind. Health 2019, 57, 419–453. [Google Scholar] [CrossRef]
- World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation; WHO Technical Report Series, n. 916; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Webber, J. Energy balance in obesity. Proc. Nutr. Soc. 2003, 62, 539–543. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.A. Measurement of energy expenditure. Public Health Nutr. 2005, 8, 1123–1132. [Google Scholar] [CrossRef] [PubMed]
- Markwald, R.R.; Melanson, E.L.; Smith, M.R.; Higgins, J.; Perreault, L.; Eckel, R.H.; Wright, K.P., Jr. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc. Natl. Acad. Sci. USA 2013, 110, 5695–5700. [Google Scholar] [CrossRef]
- Cipolla-Neto, J.; Amaral, F.G.; Afeche, S.C.; Tan, D.X.; Reiter, R.J. Melatonin, energy metabolism, and obesity: A review. J. Pineal Res. 2014, 56, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, A.; Lowson, E.; Arber, S.; Griffin, B.A.; Skene, D.J. Dietary patterns of nurses on rotational shifts are marked by redistribution of energy into the nightshift. Nutrients 2020, 12, 1053. [Google Scholar] [CrossRef]
- Amaral, F.G.D.; Andrade-Silva, J.; Kuwabara, W.M.T.; Cipolla-Neto, J. New insights into the function of melatonin and its role in metabolic disturbances. Expert Rev. Endocrinol. Metab. 2019, 14, 293–300. [Google Scholar] [CrossRef]
- Phillips, A.J.K.; Vidafar, P.; Burns, A.C.; Mcglashan, E.M.; Anderson, C.; Rajaratnam, S.M.W.; Lockley, S.W.; Cain, S.W. High sensitivity and interindividual variability in the response of the human circadian system to evening light. Proc. Natl. Acad. Sci. USA 2019, 116, 12019–12024. [Google Scholar] [CrossRef]
- Cipolla-Neto, J.; Amaral, F.G. Melatonin as a hormone: New physiological and clinical insights. Endocr. Rev. 2018, 39, 990–1028. [Google Scholar] [CrossRef]
- Lowden, A.; Moreno, C.; Holmbäck, U.; Lennernäs, M.; Tucker, P. Eating and shift work-effects on habits, metabolism and performance. Scand. J. Work Environ. Health 2010, 36, 150–162. [Google Scholar] [CrossRef]
- Wong, H.; Wong, M.C.; Wong, S.Y.; Lee, A. The association between shift duty and abnormal eating behavior among nurses working in a major hospital: A cross-sectional study. Int. J. Nurs. Stud. 2010, 47, 1021–1027. [Google Scholar] [CrossRef]

| Variables | n (%) or Mean ± SE |
|---|---|
| Age (years) | 37.1 ± 0.6 |
| Marital status (married) | 17.0 (63.0) |
| Current position (nursing technician) | 14.0 (51.9) |
| Education level (complete or incomplete graduation) | 16.0 (59.2) |
| Lifetime exposure to night work (years) | 9.1 ± 0.7 |
| The main reason to work at night (reconcile work with home and/or children’s care) | 11.0 (40.7) |
| Second job (yes) | 2.0 (7.4) |
| Smoking (no) | 27.0 (100.0) |
| Alcohol intake (only on special occasions) | 17.0 (63.0) |
| Physical activity (none) | 17.0 (63.0) |
| BMI (kg/m2) | 29.8 ± 0.4 |
| CPD (hours) | 2.9 ± 0.2 |
| Chronotype (hours) | 3.3 ± 0.2 |
| Variables | Mean ± SE | Effects (p) | Goodness of Fit *** | |
|---|---|---|---|---|
| % TEI * | Melatonin | Placebo | Intervention ** | |
| Qualitative aspect | ||||
| Unprocessed or minimally processed foods | 49.2 ± 3.2 | 52.6 ± 3.5 | 0.17 | 12.1 |
| Processed foods | 15.3 ± 1.9 | 13.1 ± 1.8 | 0.43 | 23.5 |
| Ultra-processed foods | 34.7 ± 2.4 | 34.8 ± 3.2 | 0.98 | 15.2 |
| Quantitative aspect | ||||
| Carbohydrate | 46 ± 9.7 | 44.6 ± 9.0 | 0.89 | 10.4 |
| Protein | 20.7 ± 10.2 | 21.3 ± 10.0 | 0.67 | 13.9 |
| Fat | 32.1 ± 7.9 | 33.1 ± 8.0 | 0.80 | 13.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nogueira, L.F.R.; Crispim, C.A.; Cipolla-Neto, J.; de Castro Moreno, C.R.; Marqueze, E.C. The Effect of Exogenous Melatonin on Eating Habits of Female Night Workers with Excessive Weight. Nutrients 2022, 14, 3420. https://doi.org/10.3390/nu14163420
Nogueira LFR, Crispim CA, Cipolla-Neto J, de Castro Moreno CR, Marqueze EC. The Effect of Exogenous Melatonin on Eating Habits of Female Night Workers with Excessive Weight. Nutrients. 2022; 14(16):3420. https://doi.org/10.3390/nu14163420
Chicago/Turabian StyleNogueira, Luciana Fidalgo Ramos, Cibele Aparecida Crispim, José Cipolla-Neto, Claudia Roberta de Castro Moreno, and Elaine Cristina Marqueze. 2022. "The Effect of Exogenous Melatonin on Eating Habits of Female Night Workers with Excessive Weight" Nutrients 14, no. 16: 3420. https://doi.org/10.3390/nu14163420
APA StyleNogueira, L. F. R., Crispim, C. A., Cipolla-Neto, J., de Castro Moreno, C. R., & Marqueze, E. C. (2022). The Effect of Exogenous Melatonin on Eating Habits of Female Night Workers with Excessive Weight. Nutrients, 14(16), 3420. https://doi.org/10.3390/nu14163420







