Adequate Dietary Intake and Vitamin D Supplementation: A Study of Their Relative Importance in Determining Serum Vitamin D and Ferritin Concentrations during Pregnancy
Abstract
:1. Introduction
2. Method
2.1. Participants
2.2. Design and Procedure
2.3. Measures
2.3.1. Dietary Patterns
2.3.2. Serum 25(OH)D and Ferritin Concentrations
2.3.3. Weekly Vitamin D Supplementation Frequency
2.3.4. Demographics
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Model Selection and Latent Subgroups
3.3. Associations of Vitamin D supplementation Frequency and Dietary Patterns with Serum 25(OH)D and Ferritin Concentrations among Pregnant Women
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mulligan, M.L.; Felton, S.K.; Riek, A.E.; Bernal-Mizrachi, C. Implications of vitamin D deficiency in pregnancy and lactation. Am. J. Obstet. Gynecol. 2010, 202, e421–e429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benedik, E. Sources of vitamin D for humans. Int. J. Vitam. Nutr. Res. 2021, 92, a000733. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hollis, B.W.; Johnson, D.; Hulsey, T.C.; Ebeling, M.; Wagner, C.L. Vitamin D supplementation during pregnancy: Double-blind, randomized clinical trial of safety and effectiveness. J. Bone Miner. Res. 2011, 26, 2341–2357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Callaghan, K.; Tariq, U.; Gernand, A.; Tinajero, M.; Onoyovwi, A.; Zlotkin, S.; Mahmud, A.A.; Ahmed, T.; Keya, F.; Roth, D. Effect of Maternal Vitamin D Supplementation on Iron Status During Pregnancy. Curr. Dev. Nutr. 2020, 4, 1054. [Google Scholar] [CrossRef]
- Braithwaite, V.S.; Crozier, S.R.; D’Angelo, S.; Prentice, A.; Cooper, C.; Harvey, N.C.; Jones, K.S.; Group, M.T. The effect of vitamin D supplementation on hepcidin, iron status, and inflammation in pregnant women in the United Kingdom. Nutrients 2019, 11, 190. [Google Scholar] [CrossRef] [Green Version]
- Smith, E.M.; Alvarez, J.A.; Kearns, M.D.; Hao, L.; Sloan, J.H.; Konrad, R.J.; Ziegler, T.R.; Zughaier, S.M.; Tangpricha, V. High-dose vitamin D3 reduces circulating hepcidin concentrations: A pilot, randomized, double-blind, placebo-controlled trial in healthy adults. Clin. Nutr. 2017, 36, 980–985. [Google Scholar] [CrossRef]
- Thomas, C.E.; Guillet, R.; Queenan, R.A.; Cooper, E.M.; Kent, T.R.; Pressman, E.K.; Vermeylen, F.M.; Roberson, M.S.; O’Brien, K.O. Vitamin D status is inversely associated with anemia and serum erythropoietin during pregnancy. Am. J. Clin. Nutr. 2015, 102, 1088–1095. [Google Scholar] [CrossRef] [Green Version]
- Department of Health HKSAR. Healthy Eating During Pregnancy and Breastfeeding. Available online: https://www.fhs.gov.hk/english/health_info/woman/20036.html (accessed on 15 March 2022).
- Yip, K.M.; Fung, M.K.K.; Cheung, C.K.M.; Lee, A.; So, H.K.; Wong, W.H.S.; Chan, R.S.M.; Ip, P. Validity and Reliability of Semi-Quantitative eFFQ for Hong Kong Chinese Pregnant Women. Austin J. Nutr. Metab. 2020, 7, 1093. [Google Scholar]
- Woo, J.; Leung, S.S.F.; Ho, S.C.; Lam, T.H.; Janus, E.D. A food frequency questionnaire for use in the Chinese population in Hong Kong: Description and examination of validity. Nutr. Res. 1997, 17, 1633–1641. [Google Scholar] [CrossRef]
- Woo, J.; Lau, W.; Xu, L.; Lam, C.W.K.; Zhao, X.; Yu, W.; Xing, X.; Lau, E.; Kuhn-Sherlock, B.; Pocock, N.; et al. Milk Supplementation and Bone Health in Young Adult Chinese Women. J. Women’s Health 2007, 16, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Carter, G.D.; Berry, J.; Durazo-Arvizu, R.; Gunter, E.; Jones, G.; Jones, J.; Makin, H.L.J.; Pattni, P.; Phinney, K.W.; Sempos, C.T.; et al. Quality assessment of vitamin D metabolite assays used by clinical and research laboratories. J. Steroid Biochem. Mol. Biol. 2017, 173, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Linzer, D.A.; Lewis, J.B. poLCA: An R package for polytomous variable latent class analysis. J. Stat. Softw. 2011, 42, 1–29. [Google Scholar] [CrossRef] [Green Version]
- Vrieze, S.I. Model selection and psychological theory: A discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol. Methods 2012, 17, 228–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, A.F.; Matthes, J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav. Res. Methods 2009, 41, 924–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGowan, C.A.; McAuliffe, F.M. Maternal dietary patterns and associated nutrient intakes during each trimester of pregnancy. Public Health Nutr. 2013, 16, 97–107. [Google Scholar] [CrossRef] [Green Version]
- Slater, K.; Rollo, M.E.; Szewczyk, Z.; Ashton, L.; Schumacher, T.; Collins, C. Do the Dietary Intakes of Pregnant Women Attending Public Hospital Antenatal Clinics Align with Australian Guide to Healthy Eating Recommendations? Nutrients 2020, 12, 2438. [Google Scholar] [CrossRef]
- Zareei, S.; Homayounfar, R.; Naghizadeh, M.M.; Ehrampoush, E.; Rahimi, M. Dietary pattern in pregnancy and risk of gestational diabetes mellitus (GDM). Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 12, 399–404. [Google Scholar] [CrossRef]
- Mikeš, O.; Brantsæter, A.L.; Knutsen, H.K.; Torheim, L.E.; Bienertová Vašků, J.; Pruša, T.; Čupr, P.; Janák, K.; Dušek, L.; Klánová, J. Dietary patterns and birth outcomes in the ELSPAC pregnancy cohort. J. Epidemiol. Community Health 2021, 76, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Hillier, S.E.; Olander, E.K. Women’s dietary changes before and during pregnancy: A systematic review. Midwifery 2017, 49, 19–31. [Google Scholar] [CrossRef] [Green Version]
- Popa, A.D.; Niţă, O.; Graur, L.I.; Popescu, R.M.; Botnariu, G.E.; Mihalache, L.; Graur, M. Nutritional knowledge as a determinant of vitamin and mineral supplementation during pregnancy. BMC Public Health 2013, 13, 1105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, L.; Lee, A.H.; Yau, K.K.; Hui, Y.V.; Binns, C.W. Consumption of dietary supplements by Chinese women during pregnancy and postpartum: A prospective cohort study. Matern. Child Nutr. 2017, 13, e12435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hooda, J.; Shah, A.; Zhang, L. Heme, an essential nutrient from dietary proteins, critically impacts diverse physiological and pathological processes. Nutrients 2014, 6, 1080–1102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beck, K.L.; Conlon, C.A.; Kruger, R.; Coad, J. Dietary determinants of and possible solutions to iron deficiency for young women living in industrialized countries: A review. Nutrients 2014, 6, 3747–3776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynch, S.R.; Cook, J.D. Interaction of vitamin C and iron. Ann. NY Acad. Sci. 1980, 355, 32–44. [Google Scholar] [CrossRef] [Green Version]
- Conrad, M.E.; Schade, S.G. Ascorbic acid chelates in iron absorption: A role for hydrochloric acid and bile. Gastroenterology 1968, 55, 35–45. [Google Scholar] [CrossRef]
- Canto-Costa, M.H.d.S.; Kunii, I.; Hauache, O.M. Body fat and cholecalciferol supplementation in elderly homebound individuals. Braz. J. Med. Biol. Res. 2006, 39, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Trang, H.M.; Cole, D.; Rubin, L.A.; Pierratos, A.; Siu, S.; Vieth, R. Evidence that vitamin D3 increases serum 25-hydroxyvitamin D more efficiently than does vitamin D2. Am. J. Clin. Nutr. 1998, 68, 854–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeLappe, E.; McGreevy, C.; Ni Chadhain, N.; Grimes, H.; O’Brien, T.; Mulkerrin, E. Vitamin D insufficiency in older female community-dwelling acute hospital admissions and the response to supplementation. Eur. J. Clin. Nutr. 2006, 60, 1009–1015. [Google Scholar] [CrossRef]
- Harris, S.S.; Dawson-Hughes, B. Plasma vitamin D and 25OHD responses of young and old men to supplementation with vitamin D3. J. Am. Coll. Nutr. 2002, 21, 357–362. [Google Scholar] [CrossRef]
- Veugelers, P.J.; Pham, T.M.; Ekwaru, J.P. Optimal vitamin D supplementation doses that minimize the risk for both low and high serum 25-hydroxyvitamin D concentrations in the general population. Nutrients 2015, 7, 10189–10208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, M.L.; Blum, J.M.; Hollis, B.W.; Rosen, C.; Sullivan, S.S. Supplements of 20 μg/d Cholecalciferol Optimized Serum 25-Hydroxyvitamin D Concentrations in 80% of Premenopausal Women in Winter. J. Nutr. 2009, 139, 540–546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Overall (n = 572) | Inadequate Dietary Intake (n = 276) | Adequate Dietary Intake (n = 296) | p-Value | |
|---|---|---|---|---|
| Chronological age (years), mean (SD) | 34.09 (3.98) | 34.05 (3.96) | 34.12 (4.01) | 0.84 |
| Gestational age (weeks), mean (SD) | 26.03 (4.81) | 26.26 (4.18) | 25.82 (5.33) | 0.27 |
| Gravidity, mean (SD) | 1.80 (1.04) | 1.79 (1.02) | 1.81 (1.07) | 0.83 |
| Parity, mean (SD) | 0.62 (0.79) | 0.60 (0.77) | 0.65 (0.81) | 0.44 |
| Marital status, n (%) a | ||||
| Married | 536 (94.4) | 258 (94.2) | 278 (94.6) | 0.84 |
| Single/divorced/widowed | 32 (5.6) | 16 (5.8) | 16 (5.4) | |
| Highest education level, n (%) a | 0.24 | |||
| Lower secondary education or below | 27 (4.8) | 17 (6.2) | 10 (3.4) | |
| Upper secondary education/higher certificate/diploma | 215 (37.9) | 106 (38.7) | 109 (37.2) | |
| Bachelor’s degree or above | 325 (57.3) | 151 (55.1) | 174 (59.4) | |
| Occupation, n (%) a | 0.54 | |||
| Housewife | 93 (19.2) | 42 (17.3) | 51 (21.1) | |
| Full-/part-time employment | 367 (75.7) | 189 (77.8) | 178 (73.6) | |
| Unemployment | 25 (5.2) | 12 (4.9) | 13 (5.4) | |
| Monthly family income (HKD ’000), mean (SD) | 51.3 (33.6) | 49.6 (30.9) | 52.8 (36.0) | 0.27 |
| History of chronic diseases, n (%) a | 0.98 | |||
| Yes | 50 (9.1) | 24 (9.1) | 26 (9.1) | |
| No | 500 (90.9) | 241 (90.9) | 259 (90.9) | |
| Weekly vitamin D supplementation frequency, n (%) a | 0.01 | |||
| At least 1 time per week | 427 (77.2) | 190 (72.5) | 237 (81.4) | |
| Less than 1 time per week | 126 (22.8) | 72 (27.5) | 54 (18.6) | |
| Vitamin D level (nmol/L), mean (SD) | 89.00 (26.30) | 87.83 (27.08) | 90.03 (25.56) | 0.32 |
| Log10 ferritin (pmol/L), mean (SD) | 1.79 (0.30) | 1.76 (0.29) | 1.81 (0.30) | 0.08 |
| Number of Classes | BIC | AIC | aBIC | cAIC |
|---|---|---|---|---|
| 1 | 2365.926 | 2352.878 | 2356.402 | 2368.926 |
| 2 | 2279.744 | 2249.301 | 2257.523 | 2286.744 |
| 3 | 2305.141 | 2257.301 | 2270.221 | 2316.141 |
| Food Group | Class 1 | Class 2 |
|---|---|---|
| Inadequate Dietary Intake | Adequate Dietary Intake | |
| (n = 276, 48.2%) | (n = 296, 51.8%) | |
| Vegetables (insufficient servings/day) | 0.85 | 0.25 |
| Fruits (insufficient servings/day) | 0.70 | 0.19 |
| Meat, fish, eggs, or alternatives (insufficient servings/day) | 0.62 | 0.17 |
| Ferritin | 25(OH)D | |||
|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Model 1 | ||||
| Inadequate dietary intake | −0.06 (−0.01, −0.11) | 0.03 | −2.57 (−6.99, 1.84) | 0.25 |
| Model 2 | ||||
| Inadequate dietary intake | −0.05 (−0.004, −0.10) | 0.04 | −1.97 (−6.38, 2.45) | 0.38 |
| Infrequent vitamin D supplementation | −0.03 (0.03, −0.09) | 0.39 | −6.89 (−12.15, −1.63) | 0.01 |
| Model 3 | ||||
| Inadequate dietary intake | −0.04 (−0.09, 0.02) | 0.22 | 1.03 (−3.97, 6.03) | 0.69 |
| Infrequent vitamin D supplementation | 0.02 (−0.07, 0.11) | 0.70 | 0.32 (−7.45, 8.08) | 0.94 |
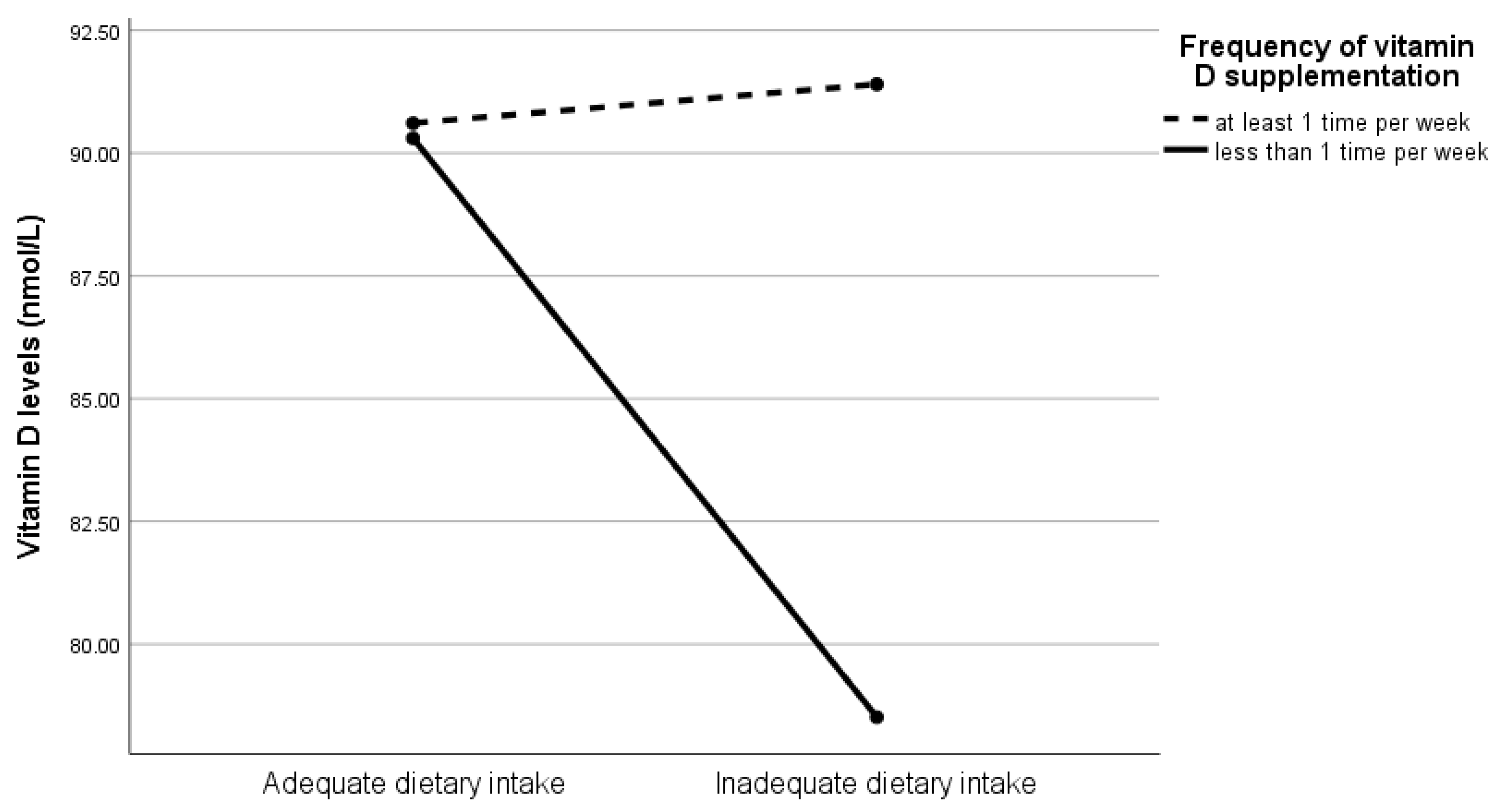
| Vitamin D × Diet | −0.08 (−0.20, 0.04) | 0.19 | −13.22 (−23.73, −2.71) | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, R.S.; Tung, K.T.S.; Chan, Y.W.K.; Chan, B.N.K.; Leung, W.-C.; Yam, J.C.; Ip, P. Adequate Dietary Intake and Vitamin D Supplementation: A Study of Their Relative Importance in Determining Serum Vitamin D and Ferritin Concentrations during Pregnancy. Nutrients 2022, 14, 3083. https://doi.org/10.3390/nu14153083
Wong RS, Tung KTS, Chan YWK, Chan BNK, Leung W-C, Yam JC, Ip P. Adequate Dietary Intake and Vitamin D Supplementation: A Study of Their Relative Importance in Determining Serum Vitamin D and Ferritin Concentrations during Pregnancy. Nutrients. 2022; 14(15):3083. https://doi.org/10.3390/nu14153083
Chicago/Turabian StyleWong, Rosa S., Keith T. S. Tung, Yannis W. K. Chan, Bianca N. K. Chan, Wing-Cheong Leung, Jason C. Yam, and Patrick Ip. 2022. "Adequate Dietary Intake and Vitamin D Supplementation: A Study of Their Relative Importance in Determining Serum Vitamin D and Ferritin Concentrations during Pregnancy" Nutrients 14, no. 15: 3083. https://doi.org/10.3390/nu14153083
APA StyleWong, R. S., Tung, K. T. S., Chan, Y. W. K., Chan, B. N. K., Leung, W.-C., Yam, J. C., & Ip, P. (2022). Adequate Dietary Intake and Vitamin D Supplementation: A Study of Their Relative Importance in Determining Serum Vitamin D and Ferritin Concentrations during Pregnancy. Nutrients, 14(15), 3083. https://doi.org/10.3390/nu14153083









