The Ultra-Processed Food Content of School Meals and Packed Lunches in the United Kingdom
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Participants
2.3. Exposure: School Lunch Meal Type
2.4. Outcome: Ultra-Processed Food
2.5. Covariates
2.6. Statistical Analysis
3. Results
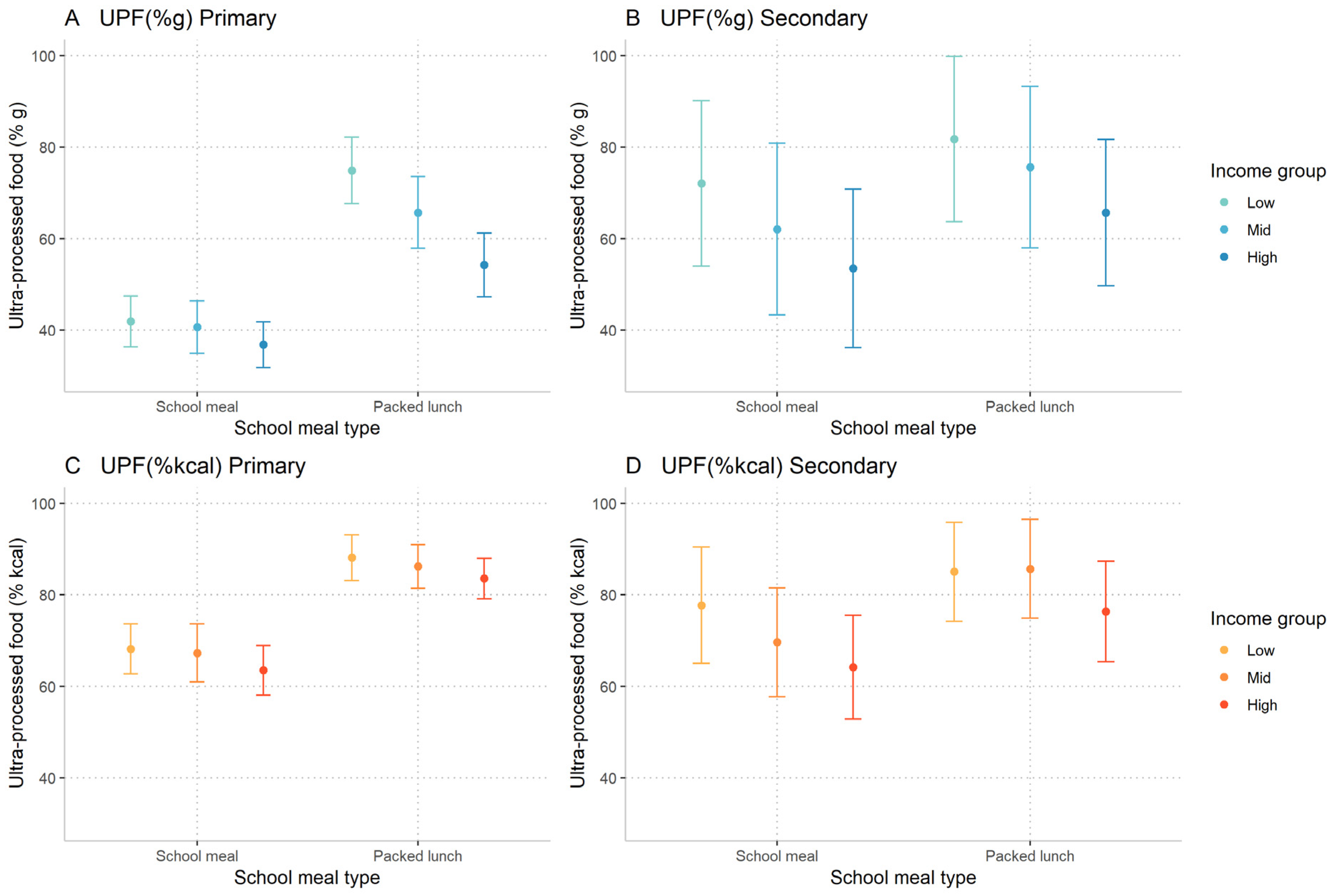
3.1. Ultra-Processed Food Intake by Population Subgroups
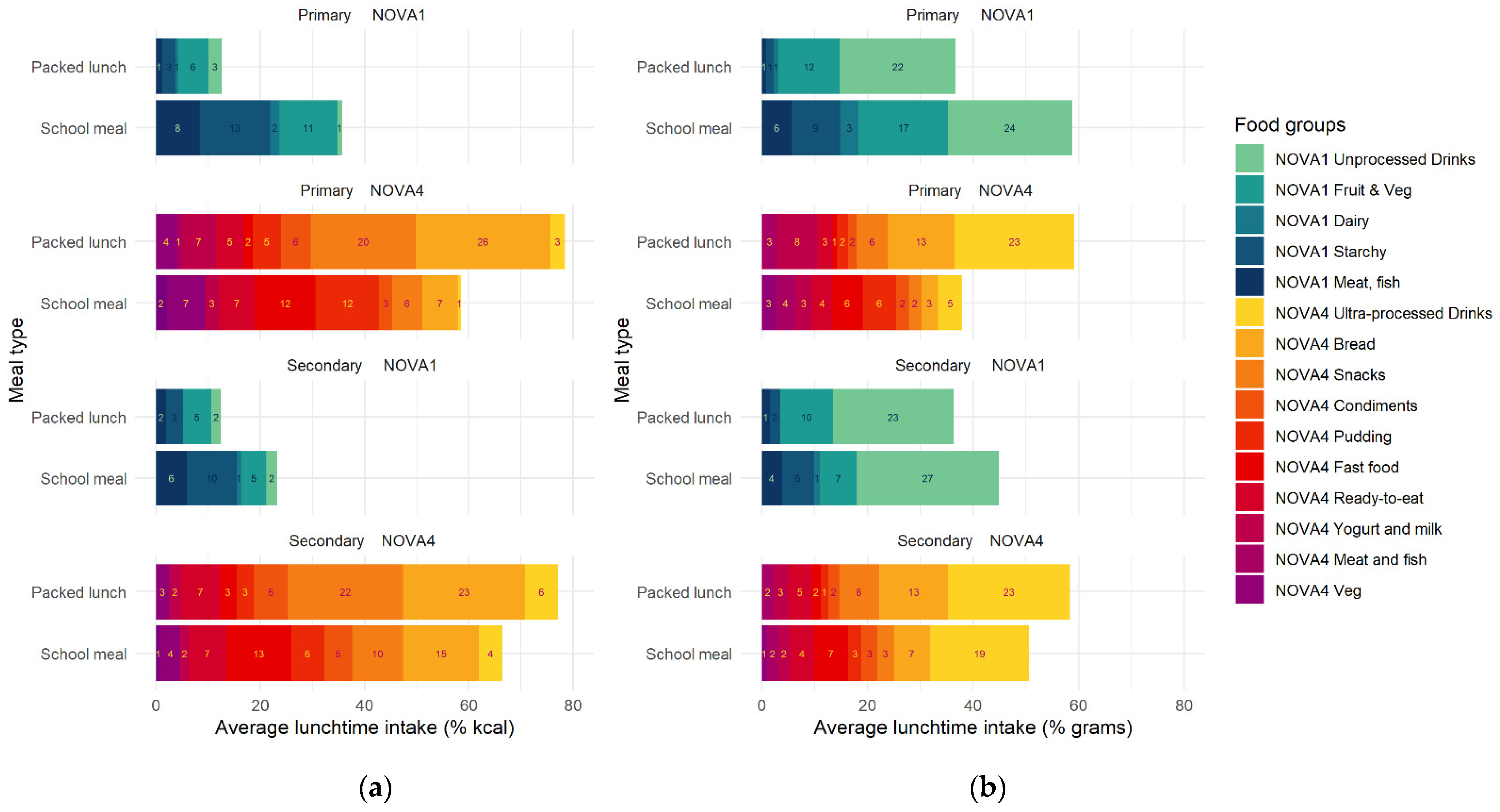
3.2. Composition of School Meals and Packed Lunches
3.3. Quantile Regression of Meal Type on Ultra-Processed Food Content
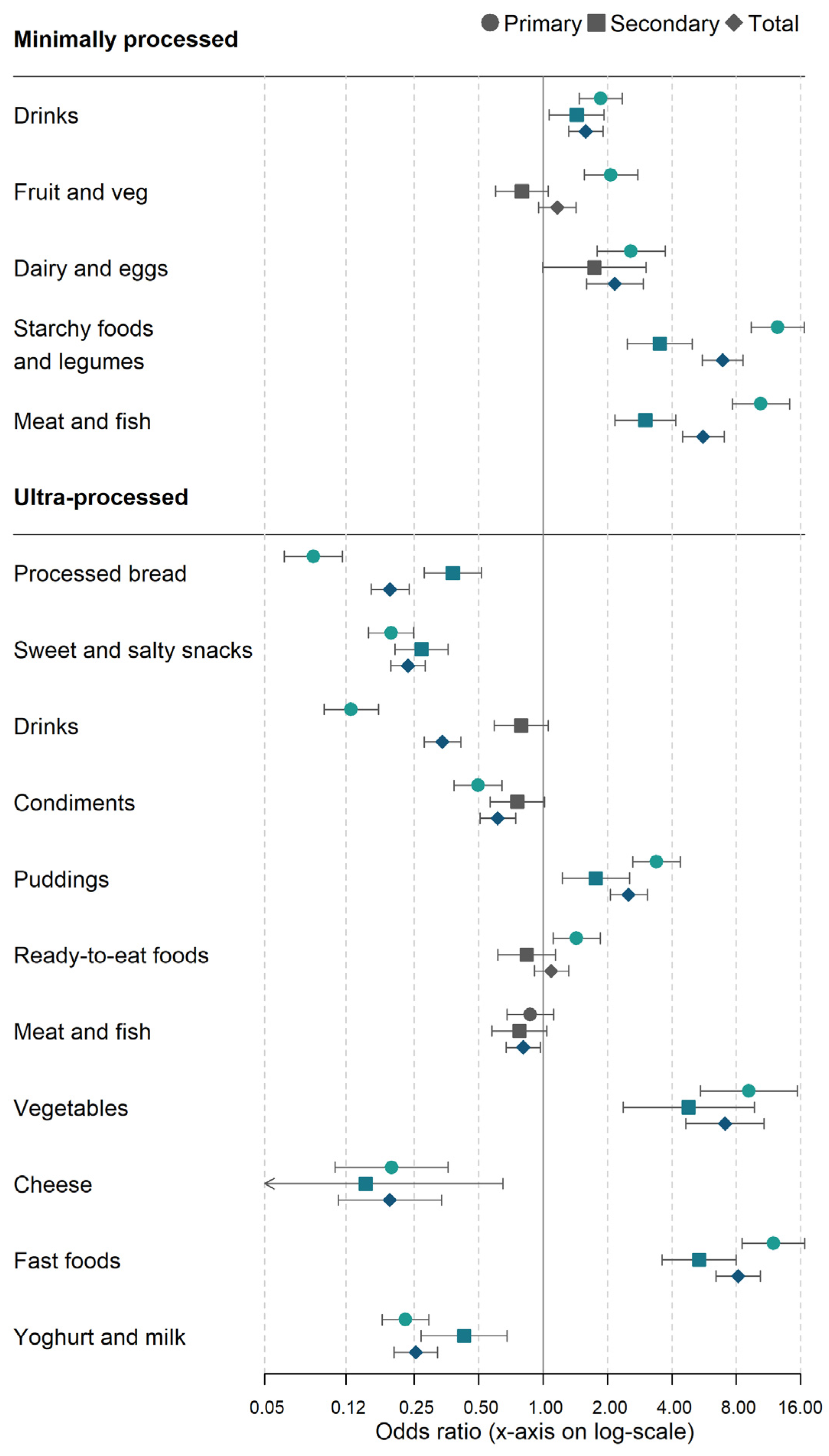
3.4. Logistic Regression of Meal Type on Minimally- and Ultra-Processed Food Groups
3.5. Sensitivity Analyses
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Onita, B.M.; Azeredo, C.M.; Jaime, P.C.; Levy, R.B.; Rauber, F. Eating context and its association with ultra-processed food consumption by British children. Appetite 2021, 157, 105007. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.-C.; Levy, R.B.; Canella, D.S.; da Louzada, M.L.C.; Cannon, G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2018, 21, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Fardet, A. Minimally processed foods are more satiating and less hyperglycemic than ultra-processed foods: A preliminary study with 98 ready-to-eat foods. Food Funct. 2016, 7, 2338–2346. [Google Scholar] [CrossRef]
- Fardet, A.; Richonnet, C. Nutrient density and bioaccessibility, and the antioxidant, satiety, glycemic, and alkalinizing potentials of fruit-based foods according to the degree of processing: A narrative review. Crit. Rev. Food Sci. Nutr. 2020, 60, 3233–3258. [Google Scholar] [CrossRef]
- Fardet, A.; Rock, E. Exclusive reductionism, chronic diseases and nutritional confusion: The degree of processing as a lever for improving public health. Crit. Rev. Food Sci. Nutr. 2020, 62, 1–16. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; da Costa Louzada, M.L.; Pereira Machado, P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; FAO: Rome, Italy, 2019. [Google Scholar]
- Lauria, F.; Dello Russo, M.; Formisano, A.; De Henauw, S.; Hebestreit, A.; Hunsberger, M.; Krogh, V.; Intemann, T.; Lissner, L.; Molnar, D.; et al. Ultra-processed foods consumption and diet quality of European children, adolescents and adults: Results from the I.Family study. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3031–3043. [Google Scholar] [CrossRef]
- Dicken, S.J.; Batterham, R.L. The Role of Diet Quality in Mediating the Association between Ultra-Processed Food Intake, Obesity and Health-Related Outcomes: A Review of Prospective Cohort Studies. Nutrients 2022, 14, 23. [Google Scholar] [CrossRef]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019, 30, 67–77.e3. [Google Scholar] [CrossRef]
- Rauber, F.; Chang, K.; Vamos, E.P.; da Costa Louzada, M.L.; Monteiro, C.A.; Millett, C.; Levy, R.B. Ultra-processed food consumption and risk of obesity: A prospective cohort study of UK Biobank. Eur. J. Nutr. 2021, 60, 2169–2180. [Google Scholar] [CrossRef]
- Costa de Miranda, R.; Rauber, F.; Levy, R.B. Impact of ultra-processed food consumption on metabolic health. Curr. Opin. Lipidol. 2021, 32, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Levy, R.B.; Rauber, F.; Chang, K.; da Louzada, M.L.C.; Monteiro, C.A.; Millett, C.; Vamos, E.P. Ultra-processed food consumption and type 2 diabetes incidence: A prospective cohort study. Clin. Nutr. 2021, 40, 3608–3614. [Google Scholar] [CrossRef]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Santé prospective cohort. BMJ 2018, 360, k322. [Google Scholar] [CrossRef]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Santé). BMJ 2019, 365, l1451. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Rojo, R.; Sandoval-Insausti, H.; López-Garcia, E.; Graciani, A.; Ordovás, J.M.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Consumption of Ultra-Processed Foods and Mortality: A National Prospective Cohort in Spain. Mayo Clin. Proc. 2019, 94, 2178–2188. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Angell, S.Y.; Lang, T.; Rivera, J.A. Role of government policy in nutrition—Barriers to and opportunities for healthier eating. BMJ 2018, 361, k2426. [Google Scholar] [CrossRef]
- McIntyre, R.L.; Adamson, A.J.; Nelson, M.; Woodside, J.; Beattie, S.; Spence, S. Changes and differences in school food standards (2010–2021) and free school meal provision during COVID-19 across the UK: Potential implications for children’s diets. Nutr. Bull. 2022, 47, 230–245. [Google Scholar] [CrossRef]
- Prynne, C.J.; Handford, C.; Dunn, V.; Bamber, D.; Goodyer, I.M.; Stephen, A.M. The quality of midday meals eaten at school by adolescents; school lunches compared with packed lunches and their contribution to total energy and nutrient intakes. Public Health Nutr. 2013, 16, 1118–1125. [Google Scholar] [CrossRef]
- Harrison, F.; Jennings, A.; Jones, A.; Welch, A.; van Sluijs, E.; Griffin, S.; Cassidy, A. Food and drink consumption at school lunchtime: The impact of lunch type and contribution to overall intake in British 9–10-year-old children. Public Health Nutr. 2013, 16, 1132–1139. [Google Scholar] [CrossRef]
- Stevens, L.; Nelson, M. The contribution of school meals and packed lunch to food consumption and nutrient intakes in UK primary school children from a low income population. J. Hum. Nutr. Diet. 2011, 24, 223–232. [Google Scholar] [CrossRef]
- Stevens, L.; Nicholas, J.; Wood, L.; Nelson, M. School lunches v. packed lunches: A comparison of secondary schools in England following the introduction of compulsory school food standards. Public Health Nutr. 2013, 16, 1037–1042. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Parnham, J.C.; Chang, K.; Millett, C.; Laverty, A.A.; von Hinke, S.; Pearson-Stuttard, J.; de Vocht, F.; White, M.; Vamos, E.P. The Impact of the Universal Infant Free School Meal Policy on Dietary Quality in English and Scottish Primary School Children: Evaluation of a Natural Experiment. Nutrients 2022, 14, 1602. [Google Scholar] [CrossRef] [PubMed]
- Haney, E.; Parnham, J.C.; Chang, K.; Laverty, A.A.; von Hinke, S.; Pearson-Stuttard, J.; White, M.; Millett, C.; Vamos, E.P. Dietary quality of school meals and packed lunches: A national study of primary and secondary school children in the UK. In Public Health Nutrition; Cambridge University Press: Cambridge, UK, 2022; pp. 1–30. [Google Scholar] [CrossRef]
- NatCen Social Research. MRC Elsie Widdowson Laboratory National Diet and Nutrition Survey Years 1–9, 2008/09-2016/17 2019; Public Health England: London, UK, 2012.
- Public Health England. Appendix B Methodology for Years 10 and 11 of the NDNS RP. In National Diet and Nutrition Survey. Years 9 to 11 of the Rolling Programme (2016/2017–2018/2019); Public Health England: London, UK, 2020. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.-C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Rauber, F.; da Louzada, M.L.C.; Martinez Steele, E.; de Rezende, L.F.M.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-processed foods and excessive free sugar intake in the UK: A nationally representative cross-sectional study. BMJ Open 2019, 9, e027546. [Google Scholar] [CrossRef]
- van Buuren, S. Classification and regression trees. In Flexible Imputation of Missing Data; Chapman and Hall/CRC: London, UK, 2018. [Google Scholar]
- Black, A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. 2000, 24, 1119–1130. [Google Scholar] [CrossRef]
- Börnhorst, C.; Huybrechts, I.; Hebestreit, A.; Vanaelst, B.; Molnár, D.; Bel-Serrat, S.; Mouratidou, T.; Moreno, L.A.; Pala, V.; Eha, M.; et al. Diet–obesity associations in children: Approaches to counteract attenuation caused by misreporting. Public Health Nutr. 2013, 16, 256–266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bates, B.; Collins, D.; Cox, L.; Nicholson, S.; Page, P.; Roberts, C.; Steer, T.; Swan, G. National Diet and Nutrition Survey Years 1 to 9 of the Rolling Programme (2008/2009–2016/17): Time Trend and Income Analyses 2019; Public Health England: London, UK, 2019.
- Rauber, F.; Martins, C.A.; Azeredo, C.M.; Leffa, P.S.; Louzada, M.L.C.; Levy, R.B. Eating context and ultraprocessed food consumption among UK adolescents. Br. J. Nutr. 2021, 127, 1–11. [Google Scholar] [CrossRef]
- Chang, K.; Khandpur, N.; Neri, D.; Touvier, M.; Huybrechts, I.; Millett, C.; Vamos, E.P. Association Between Childhood Consumption of Ultraprocessed Food and Adiposity Trajectories in the Avon Longitudinal Study of Parents and Children Birth Cohort. JAMA Pediatr. 2021, 175, e211573. [Google Scholar] [CrossRef]
- Rauber, F.; Campagnolo, P.D.B.; Hoffman, D.J.; Vitolo, M.R. Consumption of ultra-processed food products and its effects on children’s lipid profiles: A longitudinal study. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 116–122. [Google Scholar] [CrossRef]
- Leffa, P.S.; Hoffman, D.J.; Rauber, F.; Sangalli, C.N.; Valmórbida, J.L.; Vitolo, M.R. Longitudinal associations between ultra-processed foods and blood lipids in childhood. Br. J. Nutr. 2020, 124, 341–348. [Google Scholar] [CrossRef]
- Hayter, A.K.M.; Draper, A.K.; Ohly, H.R.; Rees, G.A.; Pettinger, C.; McGlone, P.; Watt, R.G. A qualitative study exploring parental accounts of feeding pre-school children in two low-income populations in the UK. Matern. Child Nutr. 2015, 11, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Rylatt, L.; Cartwright, T. Parental feeding behaviour and motivations regarding pre-school age children: A thematic synthesis of qualitative studies. Appetite 2016, 99, 285–297. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.L.; Melia, K.E.; Rippin, H.L.; Hancock, N.; Cade, J. A repeated cross-sectional survey assessing changes in diet and nutrient quality of English primary school children’s packed lunches between 2006 and 2016. BMJ Open 2020, 10, e029688. [Google Scholar] [CrossRef] [PubMed]
- Ensaff, H.; Russell, J.; Barker, M.E. Meeting school food standards—Students’ food choice and free school meals. Public Health Nutr. 2013, 16, 2162–2168. [Google Scholar] [CrossRef]
- Dimbleby, H.; Vincent, J. The School Food Plan. Available online: https://www.schoolfoodmatters.org/campaigns/school-food-plan (accessed on 24 March 2021).
- Olsen, J.R.; Patterson, C.; Caryl, F.M.; Robertson, T.; Mooney, S.J.; Rundle, A.G.; Mitchell, R.; Hilton, S. Exposure to unhealthy product advertising: Spatial proximity analysis to schools and socio-economic inequalities in daily exposure measured using Scottish Children’s individual-level GPS data. Health Place 2021, 68, 102535. [Google Scholar] [CrossRef]
- Baghlaf, K.; Muirhead, V.; Pine, C. Relationships between children’s sugar consumption at home and their food choices and consumption at school lunch. Public Health Nutr. 2020, 23, 2941–2949. [Google Scholar] [CrossRef]
- World Health Organisation Action Framework for Developing and Implementing Public Food Procurement and Service Policies for a Healthy Diet. Available online: https://apps.who.int/iris/handle/10665/338525 (accessed on 10 May 2021).
- Popkin, B.M.; Barquera, S.; Corvalan, C.; Hofman, K.J.; Monteiro, C.; Ng, S.W.; Swart, E.C.; Taillie, L.S. Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. lancet. Diabetes Endocrinol. 2021, 9, 462–470. [Google Scholar] [CrossRef]
- Noll, P.R.E.S.; Noll, M.; de Abreu, L.C.; Baracat, E.C.; Silveira, E.A.; Sorpreso, I.C.E. Ultra-processed food consumption by Brazilian adolescents in cafeterias and school meals. Sci. Rep. 2019, 9, 7162. [Google Scholar] [CrossRef]
- Boklis-Berer, M.; Rauber, F.; Azeredo, C.M.; Levy, R.B.; da Costa Louzada, M.L. School meals consumption is associated with a better diet quality of Brazilian adolescents: Results from the PeNSE 2015 survey. Public Health Nutr. 2021, 24, 6512–6520. [Google Scholar] [CrossRef]
- Boklis-Berer, M.; Rauber, F.; Azeredo, C.M.; Levy, R.B.; da Costa Louzada, M.L. The adherence to school meals is associated with a lower occurrence of obesity among Brazilian adolescents. Prev. Med. 2021, 150, 106709. [Google Scholar] [CrossRef]
- Long, R. School Meals and Nutritional Standards; House of Commons: London, UK, 2021. [Google Scholar]
- Environment Food and Rural Affairs Committee. Public Sector Procurement of Food; House of Commons: London, UK, 2021; Volume I. [Google Scholar]
- Dimbleby, H. National Food Strategy: The Plan. Available online: https://www.nationalfoodstrategy.org/ (accessed on 24 March 2021).
| Main Group | Description |
|---|---|
| NOVA 1 Unprocessed and minimally processed food (MPF) | Whole foods that have undergone no or minimal processing; e.g., fresh fruit and vegetables and their juices, cooked rice, plain milk or grilled fish. |
| NOVA 2 Processed culinary ingredients | MPF substances that are obtained directly from Group 1 foods (e.g., butter) or from nature (e.g., salt) and are used in food preparation |
| NOVA 3 Processed food | Foods that have undergone higher levels of processing and are manufactured with culinary ingredients; e.g., cheese, jam, or bread made from flour, water, and salt. |
| NOVA 4 Ultra-processed food (UPF) | Foods that are industrial formulations of substances derived from foods, and that contain cosmetic additives and little, if any, whole foods (e.g., carbonated beverages, French fries, or manufactured bread). |
| Subsidary Group | Definition |
|---|---|
| NOVA 1—minimally processed food (MPF) | |
| Drinks | Water, coffee and tea, fresh fruit juices and smoothies |
| Fruit and vegetables | Fruit, vegetables, fungi, nuts and seeds |
| Dairy and eggs | Milk, plain yoghurt, eggs |
| Starchy foods and legumes | Grains, legumes, pasta, homemade pies and pastries |
| Meat and fish | Fish, poultry, red meat, pies and pastries with meat or fish, seafood |
| NOVA 4—Ultra-processed (UPF) | |
| Processed bread | Industrially manufactured bread |
| Sweet and salty snacks | Industrially manufactured cakes, pies, biscuits, sweet snacks, salty snacks (crisps) |
| Drinks | Soft drinks (high and low calorie) and fruit drinks |
| Condiments | Sauces, dressings, gravy, spread, margarine |
| Puddings and desserts | Ice cream, ice pops, desserts, sweet spreads and icing, artificial sugars and sweeteners |
| Ready-to-eat foods | Pasta and rice dishes (ready-to-eat/heat), egg and cheese dishes (ready-to-eat/heat), bacon/sausages dishes (ready-to-eat/heat), meat dishes (ready-to-eat/heat) Chicken/turkey dishes (ready-to-eat/heat), fish dishes (ready-to-eat/heat), vegetables dishes (ready-to-eat/heat), meat alternatives Potato dishes (ready-to-eat/heat), instant and canned soups, industrially manufactured meat pies and pastries |
| Meat and fish | Processed meat and fish (bacon, ham) |
| Vegetables | Processed vegetables (baked beans, processed peas) |
| Cheese | Processed cheese and cheese products |
| Fast foods | Pizza, French fries and other potato products, sandwiches and hamburgers |
| Yoghurt and milk | Industrially manufactured yoghurts and milk drinks |
| Primary School Children (n = 1895, 57%) | Secondary School Children (n = 1408, 43%) | Total (n = 3303) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | School Meals | Packed Lunches | p 1 | School Meals | Packed Lunches | p 2 | School Meals | Packed Lunches | p 3 |
| n (%) | 928 (49.1) | 967 (50.9) | 654 (44.7) | 754 (55.3) | 1582 (47.1) | 1721 (52.9) | |||
| Age, M (SD) | 7.2 (2.0) | 7.7 (2.1) | <0.001 b | 13.7 (1.9) | 14.2 (1.9) | 0.001 b | 9.9 (3.8) | 10.8 (3.8) | <0.001 b |
| Sex, n (%) 4 | 0.03 a | 0.17 a | 0.55 a | ||||||
| Male | 480 (49.4) | 525 (55.6) | 327 (52.9) | 340 (48.3) | 807 (50.9) | 865 (52.2) | |||
| Female | 448 (50.6) | 442 (44.4) | 327 (47.1) | 414 (51.7) | 775 (49.1) | 856 (47.8) | |||
| Ethnicity, n (%) | 0.009 a | 0.02 a | <0.001 a | ||||||
| White | 791 (79.6) | 861 (85.6) | 573 (78.9) | 673 (85.5) | 1364 (79.3) | 1534 (85.5) | |||
| Ethnic minorities | 137 (20.4) | 106 (14.4) | 81 (21.1) | 81 (14.5) | 218 (20.7) | 187 (14.5) | |||
| Household income, n (%) | 0.002 b | 0.10 b | |||||||
| Low | 336 (37.5) | 268 (31.0) | 250 (43.1) | 247 (36.4) | 586 (39.9) | 515 (33.5) | |||
| Mid | 271 (27.0) | 370 (36.6) | 199 (28.1) | 261 (33.9) | 470 (27.4) | 631 (35.3) | |||
| High | 321 (35.5) | 329 (32.4) | 205 (28.9) | 246 (29.6) | 526 (32.7) | 575 (31.1) | |||
| IMD, n (%) | 0.10 a | 0.12 a | 0.01 a | ||||||
| 1 (Least deprived) | 188 (20.8) | 229 (22.5) | 143 (21.4) | 178 (23.7) | 331 (21.1) | 407 (23.1) | |||
| 2 | 162 (15.5) | 166 (19.1) | 126 (20.9) | 158 (21.8) | 288 (17.8) | 324 (20.4) | |||
| 3 | 199 (19.7) | 207 (17.7) | 127 (14.7) | 156 (18.9) | 326 (17.6) | 363 (18.3) | |||
| 4 | 170 (19.8) | 197 (21.9) | 123 (22.1) | 148 (20.8) | 293 (20.8) | 345 (21.4) | |||
| 5 (Most deprived) | 209 (24.1) | 168 (18.7) | 135 (20.9) | 114 (14.8) | 344 (22.8) | 282 (16.9) | |||
| Country, n (%) | 0.64 a | 0.29 a | 0.30 a | ||||||
| England | 555 (82.9) | 543 (83.0) | 366 (84.1) | 460 (87.2) | 921 (83.4) | 1003 (85.0) | |||
| Scotland | 135 (8.8) | 166 (9.2) | 87 (6.3) | 96 (5.5) | 222 (7.7) | 262 (7.5) | |||
| Wales | 120 (5.2) | 118 (4.3) | 88 (5.9) | 89 (4.3) | 208 (5.5) | 207 (4.3) | |||
| N. Ireland | 118 (3.1) | 140 (3.5) | 113 (3.7) | 109 (3.0) | 231 (3.4) | 249 (3.2) | |||
| UPF % kcal, med (Q25,Q75) | 61.0 (44, 75) | 81.2 (71, 91) | <0.001 c | 70.1 (48, 89) | 83.5 (65, 99) | 0.001 c | 64.0 (45, 80) | 82.1 (68, 94) | <0.001 c |
| UPF (% kcal), M (SD) | 58.7 (22.5) | 78.4 (17.4) | <0.001 b | 66.0 (28.3) | 76.2 (25.7) | 0.001 b | 61.8 (25.4) | 77.4 (21.7) | <0.001 b |
| UPF % g, med (Q25,Q75) | 35.4 (23, 49) | 59.9 (36, 82) | <0.001 c | 45.8 (22, 80) | 58.6 (29, 91) | 0.01 c | 37.7 (23, 60) | 59.7 (23, 60) | <0.001 c |
| UPF (% g), M (SD) | 38.2 (20.9) | 59.8 (27.0) | <0.001 b | 50.3 (32.0) | 57.8 (32.7) | 0.001 b | 43.3 (26.8) | 58.9 (29.8) | <0.001 b |
| Primary Schoolchildren | Secondary Schoolchildren | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 1 | Model 2 2 | Model 1 1 | Model 2 2 | |||||
| Variable | Coef. (95% CI) | p | Coef. (95% CI) | p | Coef. (95% CI) | p | Coef. (95% CI) | p |
| UPF (% g) | ||||||||
| Packed lunches | (ref) | (ref) | (ref) | (ref) | ||||
| School meals | −24.41 (−29.43, −21.45) | <0.001 | −24.78 (−28.12, −22.3) | <0.001 | −15.26 (−22.49, −7.21) | <0.001 | −11.64 (−21.03, −6.51) | <0.001 |
| UPF (% kcal) | ||||||||
| Packed lunches | (ref) | (ref) | (ref) | (ref) | ||||
| School meals | −20.42 (−22.72, −17.68) | <0.001 | −19.64 (−22.26, −17.48) | <0.001 | −13.07 (−16.49, −9.63) | <0.001 | −11.05 (−15.99, −6.96) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parnham, J.C.; Chang, K.; Rauber, F.; Levy, R.B.; Millett, C.; Laverty, A.A.; von Hinke, S.; Vamos, E.P. The Ultra-Processed Food Content of School Meals and Packed Lunches in the United Kingdom. Nutrients 2022, 14, 2961. https://doi.org/10.3390/nu14142961
Parnham JC, Chang K, Rauber F, Levy RB, Millett C, Laverty AA, von Hinke S, Vamos EP. The Ultra-Processed Food Content of School Meals and Packed Lunches in the United Kingdom. Nutrients. 2022; 14(14):2961. https://doi.org/10.3390/nu14142961
Chicago/Turabian StyleParnham, Jennie C., Kiara Chang, Fernanda Rauber, Renata B. Levy, Christopher Millett, Anthony A. Laverty, Stephanie von Hinke, and Eszter P. Vamos. 2022. "The Ultra-Processed Food Content of School Meals and Packed Lunches in the United Kingdom" Nutrients 14, no. 14: 2961. https://doi.org/10.3390/nu14142961
APA StyleParnham, J. C., Chang, K., Rauber, F., Levy, R. B., Millett, C., Laverty, A. A., von Hinke, S., & Vamos, E. P. (2022). The Ultra-Processed Food Content of School Meals and Packed Lunches in the United Kingdom. Nutrients, 14(14), 2961. https://doi.org/10.3390/nu14142961






