Abstract
We evaluated the relationship of daily coffee intake with endothelial function assessed by flow-mediated vasodilation and vascular smooth muscle function assessed by nitroglycerine-induced vasodilation in patients with hypertension. A total of 462 patients with hypertension were enrolled in this cross-sectional study. First, we divided the subjects into two groups based on information on daily coffee intake: no coffee group and coffee group. The median coffee intake was two cups per day in the coffee group. There were significant differences in both flow-mediated vasodilation (2.6 ± 2.8% in the no coffee group vs. 3.3 ± 2.9% in the coffee group, p = 0.04) and nitroglycerine-induced vasodilation (9.6 ± 5.5% in the no coffee group vs. 11.3 ± 5.4% in the coffee group, p = 0.02) between the two groups. After adjustment for confounding factors, the odds ratio for endothelial dysfunction (OR: 0.55, 95% CI: 0.32–0.95) and the odds ratio for vascular smooth muscle dysfunction (OR: 0.50, 95% CI: 0.28–0.89) were significantly lower in the coffee group than in the no coffee group. Next, we assessed the relationship of the amount of daily coffee intake with vascular function. Cubic spline curves revealed that patients with hypertension who drank half a cup to 2.5 cups of coffee per day had lower odds ratios for endothelial dysfunction assessed by flow-mediated vasodilation and vascular smooth muscle dysfunction assessed by nitroglycerine-induced vasodilation. Appropriate daily coffee intake might have beneficial effects on endothelial function and vascular smooth muscle function in patients with hypertension.
1. Introduction
Coffee is one of the most popular beverages worldwide. Alcohol and tobacco are considered to be harmful for health [,], whereas coffee is considered to be beneficial for health []. The World Health Organization (WHO) issued a warning that alcohol consumption causes about three million deaths and that tobacco causes more than eight million deaths worldwide every year [,]. On the other hand, several lines of evidence have shown that individuals who drink coffee have a lower risk for all-cause mortality []. Previously, coffee had been considered to be carcinogenic []. However, in 2016, the International Agency for Research for Cancer and WHO reported that there is no evidence that coffee increases the risk of cancer []. On the other hand, the relationship between the hazard ratio for cardiovascular disease (CVD) and daily coffee intake is still controversial. Some studies have shown that coffee intake or even excessive intake can be associated with decreased CVD events [,,,]. It is also still not clear whether coffee intake has beneficial effects or not in patients with hypertension. A meta-analysis revealed that light to moderate coffee intake (1 to 3 cups/day) increased the risk of hypertension []. On the other hand, another meta-analysis showed that regular coffee intake has no effects on blood pressure level and risk of hypertension []. A previous study showed that high coffee intake (≥4 cups/day) increases the risk of stroke []. However, other studies have shown that even high coffee intake has no effects or beneficial effects on CVD events [,]. It is also still not clear whether daily coffee intake increases the risk for CVD events in patients with hypertension.
Endothelium cells maintain endothelial function by secreting several vasodilators such as nitric oxide (NO) and endothelium-derived hyperpolarizing factor [,]. Endothelial function is impaired by cardiovascular risk factors in the initial step of atherosclerosis [,,,], and vascular smooth muscle function is impaired in the progressed state of atherosclerosis []. Measurement of flow-mediated vasodilation (FMD) in the brachial artery is the most popular tool for assessing endothelial function and measurement of nitroglycerine-induced vasodilation (NID) is the most popular tool for assessing vascular smooth muscle function [,]. Both FMD and NID are associated with cardiovascular risk factors, are targets for the treatment of cardiovascular disease, and are predictors for cardiovascular events. Although previous studies have shown that FMD and NID are correlated with daily lifestyle habits including smoking, tooth brushing, and daily physical activity [,], the effects of coffee intake on vascular function are still controversial. Several interventional studies have shown acute beneficial effects of coffee intake on vascular function [,], while some studies showed no effect [,] or harmful effects on vascular function [,].
Furthermore, there is little information on the relationship between daily coffee intake and endothelial function, and there is no information on the relationship between daily coffee intake and vascular smooth muscle function. There is also no information on the relationships between amounts of daily coffee intake and vascular function. Therefore, in the present study, we assessed the relationship of daily coffee intake with vascular function using FMD and NID.
2. Materials and Methods
2.1. Study Subjects
Between April 2016 and August 2021, a total of 462 patients with hypertension who underwent a health checkup at Hiroshima University were enrolled in this cross-sectional study. We excluded the following subjects: subjects being treated with nitrate, subjects with severe chronic heart failure (New York Heart Association level of III or higher), and subjects without information on coffee intake (cups/day). Hypertension was defined as the use of antihypertensive drugs or systolic blood pressure of more than 140 mm Hg or diastolic blood pressure of more than 90 mm Hg measured in a sitting position on at least three occasions. Dyslipidemia was defined according to the third report of the National Cholesterol Education Program []. Diabetes mellitus was defined according to the American Diabetes Association recommendation []. Smokers were defined as current smokers or former smokers. CVD was defined as coronary heart disease and cerebrovascular disease. Coronary heart disease included angina pectoris, prior myocardial infarction, and unstable angina. Cerebrovascular disease included ischemic stroke, hemorrhagic stroke, and transient ischemic attack. The Ethics Committee of Hiroshima University approved the study protocol. Written informed consent for participation in this study was obtained from all participants.
2.2. Study Protocol
This study was a cross-sectional study. We assessed vascular function in all subjects by using measurements of FMD and NID. The patients fasted overnight and abstained from alcohol, caffeine including coffee, antioxidant vitamins, and smoking for at least 12 h before the study. We divided the subjects into two groups based on information on daily coffee intake: no coffee group and coffee group. We assessed endothelial function and vascular smooth muscle function in each group. Multivariate regression analysis was performed to identify independent variables associated with vascular function. As a post hoc analysis, we fitted a cubic spline curve relationship between the daily amount of coffee intake and vascular function assessed by using FMD and NID. The participants were kept in the supine position in a quiet, dark, air-conditioned room (constant temperature of 22 °C to 25 °C) throughout the study. A 23-gauge polyethylene catheter was inserted into the deep antecubital vein to obtain blood samples. After maintaining the supine position for 30 min, FMD and NID were measured. The observers were blind to the form of examination.
2.3. Measurements of FMD and NID
A high-resolution linear artery transducer was coupled to computer-assisted analysis software (UNEXEF18G, UNEX Co., Nagoya, Japan) that used an automated edge detection system for measurement of the brachial artery diameter []. Additional details are available in the supplementary materials.
2.4. Evaluation of Daily Coffee Intake
Information on daily coffee intake was obtained by using a self-reported questionnaire. The questionnaire consisted of a question on daily coffee intake (yes or no) and the question “How many cups of coffee do you drink each day?”. We defined one cup of coffee as about 200 mL and assessed the amount of coffee intake in the unit of 0.5-cup increments.
2.5. Statistical Analysis
Results are presented as means ± SD or medians (interquartile range). Normal distribution was assessed by the Shapiro–Wilk test. All reported probability values were two-sided, and a probability value of <0.05 was considered statistically significant. Categorical values were compared by means of the chi-square test. Leven’s test was used to compare the coffee group and the no-coffee group. Continuous variables were compared by using an unpaired Student’s t-test or Wilcoxson rank-sum test. We categorized subjects into three tertiles based on FMD and NID. The lowest tertile of FMD was 1.6% and the lowest tertile of NID was 8.4%. Therefore, we defined endothelial dysfunction as FMD of <1.6% and vascular smooth muscle dysfunction as NID of <8.4%. Multivariate logistic regression analysis was performed to identify independent variables associated with endothelial dysfunction and vascular smooth muscle dysfunction. Age, sex, body mass index, smokers, presence of dyslipidemia, presence of diabetes mellitus, presence of cardiovascular disease, and systolic blood pressure level were entered into the multivariate logistic regression analysis. The effect of the amount of coffee intake on endothelial function was assessed as a continuous variable by cubic spline curves with the no coffee group as the reference. All data were processed using JMP Pro. Ver 14.0 software (SAS Institute, Cary, NC, USA) and R software version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
3. Results
3.1. Baseline Characteristics of the Subjects
The baseline clinical characteristics of the 462 patients with hypertension are summarized in Table 1. The 462 subjects included 274 men (59.7%). Among the subjects, 301 (65.2%) had dyslipidemia, 135 (29.2%) had diabetes mellitus, 94 (20.6%) had previous cardiovascular disease and 252 (54.7%) were smokers. The median amount of coffee intake was 1.5 cups/day. The mean FMD value was 3.2 ± 2.9% and the mean NID value was 11.0 ± 5.4%.

Table 1.
Clinical Characteristics of Subjects in Groups According to Daily Coffee Intake.
3.2. Vascular Function in the No Coffee Group and Coffee Group
The baseline clinical characteristics of the patients with hypertension who did not drink coffee (no coffee group) and patients with hypertension who drank coffee (coffee group) are also summarized in Table 1. There were significant differences in sex, low-density lipoprotein cholesterol, creatinine, prevalence of diabetes mellitus, and prevalence of cardiovascular disease between the two groups. The median coffee intake was two cups per day in the coffee group. The FMD value was significantly lower in the no coffee group than in the coffee group (2.6 ± 2.8% vs. 3.3 ± 2.9%, p = 0.04) (Figure 1A). The NID value was significantly lower in the no coffee group than in the coffee group (9.6 ± 5.5% vs. 11.3 ± 5.4%, p = 0.02) (Figure 1B).
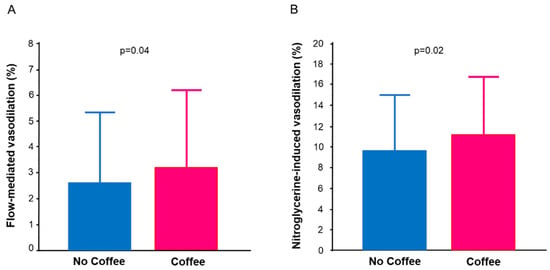
Figure 1.
Bar graphs show flow-mediated vasodilation (A) and nitroglycerine-induced vasodilation (B) in patients with hypertension who did not drink coffee and patients with hypertension who drank coffee.
Next, we performed multiple logistic analysis to determine whether daily coffee intake was independently associated with endothelial function and vascular smooth muscle function. After adjustments for age, sex, body mass index, systolic blood pressure, presence of dyslipidemia, presence of diabetes mellitus, prevalence of cardiovascular disease, smokers, and systolic blood pressure, the odds ratio for endothelial dysfunction was significantly lower in the coffee group than in the no coffee group (OR: 0.55, 95% CI: 0.32–0.95) (Table 2). After adjustments for age, sex, body mass index, presence of dyslipidemia, presence of diabetes mellitus, presence of cardiovascular disease, and smokers, the odds ratio for vascular smooth muscle dysfunction was significantly lower in the coffee group than in the no coffee group (OR: 0.50, 95% CI: 0.28–0.89) (Table 3).

Table 2.
Multivariate Analysis of Endothelial Dysfunction in No Coffee and Coffee Groups.

Table 3.
Multivariate Analysis of Vascular Smooth Muscle Dysfunction in No Coffee and Coffee Groups.
Finally, we assessed the effects of the amount of coffee intake on endothelial function by cubic spline curves. The cubic spline curves revealed that a daily intake of 0.5 cups to 2.5 cups of coffee had lower odds ratios for endothelial dysfunction and vascular smooth muscle dysfunction (Figure 2A,B).
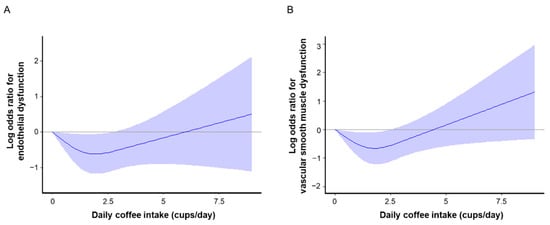
Figure 2.
Cubic splines of the relationships of amount of daily coffee intake with log odds ratios for endothelial dysfunction (A) and vascular smooth muscle function (B). Endothelial dysfunction was defined as flow-mediated vasodilation of less than 1.6% and vascular smooth muscle dysfunction was defined as nitroglycerine-induced vasodilation of less than 8.4%. Vertical lines show 95% confidence intervals.
4. Discussion
In the present study, we demonstrated that both endothelial function and vascular smooth muscle function were more impaired in patients with hypertension who did not drink coffee than in patients with hypertension who drank coffee. An appropriate amount of coffee intake (e.g., less than 2.5 cups/day) might have beneficial effects on endothelial function and vascular smooth muscle function in patients with hypertension.
First, the subjects were divided into two groups of subjects who drank coffee and those who did not drink coffee and vascular function was assessed in each group. Both FMD and NID were significantly smaller in patients with hypertension who did not drink coffee than in patients with hypertension who drank coffee. Next, we assessed the relationship between the amount of daily coffee intake and vascular function in patients with hypertension. Cubic spline curves revealed that the median amount of coffee intake (2 cups per day) decreased the odds ratios for endothelial dysfunction and vascular smooth muscle dysfunction and that excessive coffee intake was harmful to endothelial function and vascular smooth muscle function. Previous studies showed that an excessive amount of caffeine intake elevated blood pressure through the activation of renin activity and activation of the sympathetic nervous system [,]. In addition, about 300 mg of caffeine intake per day has been shown to affect blood pressure levels []. Furthermore, excessive caffeine intake causes unpleasant symptoms such as depression, headaches, insomnia, and palpitations []. In the present study, coffee intake of two cups per day had beneficial effects on endothelial function and vascular smooth muscle function in patients with hypertension. It is likely that coffee intake is a double-edged sword for endothelial function and vascular smooth muscle function depending on its amount.
The mechanisms by which daily coffee intake has beneficial effects on vascular function might be an increase in NO bioavailability caused by compounds in coffee. Coffee contains several compounds including caffeine and chlorogenic acid (CGA), which has an antioxidant property. CGA is one of the polyphenols and is contained in coffee beans. CGA has a protective effect against oxidative stress by scavenging reactive oxygen species and activating adenosine monophosphate-activated protein kinase [,]. Our previous study showed that intake of coffee containing a large amount of CGA and a small amount of hydroxy hydroquinone (HHQ), which has a pro-oxidative property, decreased oxidative stress, and improved endothelial function in patients with borderline and stage 1 hypertension. On the other hand, intake of coffee containing a large amount of CGA and a large amount of HHQ had no effect, as did a placebo, on endothelial function in those patients []. Caffeine is one of the most popular substances in coffee and also in tea, chocolate, and supplements. Caffeine has several effects on vascular function through various actions including acting as an antagonist of adenosine receptors, increasing intracellular calcium concentration, and inhibiting phosphodiesterase (PDE). Caffeine increases NO production in endothelial cells by binding to the adenosine A1 receptor as an antagonist. In addition, caffeine increases eNOS activity by binding to G-protein-coupled receptors and activating the calcium/calmodulin-dependent protein kinase. It has been shown that caffeine activates cyclic adenosine monophosphate and cyclic guanosine monophosphate through the inhibition of PDE5 []. On the other hand, caffeine decreases NO production in endothelial cells by binding to the adenosine A2A receptor as an antagonist. Caffeine per se is also a double-edged sword for vascular function.
This study has potential limitations. First, this study showed the association of daily coffee intake with vascular function. However, this was a single-center, cross-sectional study. Therefore, we cannot define causal relationships between coffee intake with vascular function. Second, only patients with hypertension were recruited in the present study. Assessment of the relationship between vascular function and daily coffee intake in a general population including healthy subjects would enable more specific conclusions to be drawn. Third, the amount of daily coffee intake by Japanese is relatively small. A previous study showed that only about 3% of Japanese adults drank more than five cups of coffee per day []. In the present study, the median daily coffee intake was two cups. Therefore, we could not determine the association of a large amount of coffee intake with vascular function. Furthermore, the sample size in the present study was relatively small. Therefore, we cannot clearly indicate that an excessive amount of coffee intake might have negative effects on endothelial function and vascular smooth muscle function in patients with hypertension. Further studies are needed to establish the association of a large amount of coffee intake with vascular function using a large sample size. Fourth, information on daily coffee intake was obtained by using a self-reported questionnaire. However, in previous studies that focused on the relationships of daily coffee intake with variables, information on daily coffee intake was also obtained by using a self-reported questionnaire [,,].
5. Conclusions
In conclusion, patients with hypertension who drank two cups of coffee per day had larger FMD and NID than those patients with hypertension who did not drink coffee. Appropriate coffee intake might have beneficial effects on endothelial function and vascular smooth muscle function in patients with hypertension.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14132719/s1. Supplemental Methods.
Author Contributions
T.Y. and Y.H. (Yukihito Higashi) drafting the article and conception of the study; T.Y., T.H., Y.H (Yu Hashimoto)., M.K., C.G., A.M., S.T., F.M.Y., S.K., T.M. and A.N. acquiring subjects and/or data; Y.N. and K.Y. revising the article critically for important intellectual content. Y.H. (Yukihito Higashi) is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis. All authors contributed to the interpretation of data and review of the manuscript and approved this manuscript for submission. All authors have read and agreed to the published version of the manuscript.
Funding
Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898 to Y.Higashi).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Review Board of Hiroshima University.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to institutional policies requiring a data-sharing agreement.
Acknowledgments
The authors would like to thank all of the patients who participated in this study. In addition, we thank Ki-ichiro Kawano, Megumi Wakisaka, Miki Kumiji, and Satoko Michiyama for their excellent secretarial assistance.
Conflicts of Interest
The authors declared that they do not have anything to disclose regarding conflict of interest with respect to this manuscript.
References
- Minzer, S.; Losno, R.A.; Casas, R. The Effect of Alcohol on Cardiovascular Risk Factors: Is There New Information? Nutrients 2020, 12, 912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poole, R.; Kennedy, O.J.; Roderick, P.; Fallowfield, J.A.; Hayes, P.C.; Parkes, J. Coffee consumption and health: Umbrella review of meta-analyses of multiple health outcomes. BMJ 2017, 359, j5024. [Google Scholar] [CrossRef] [Green Version]
- Fouad, H.; Commar, A.; Hamadeh, R.; El-Awa, F.; Shen, Z.; Fraser, C. Estimated and projected prevalence of tobacco smoking in males, Eastern Mediterranean Region, 2000–2025. East. Mediterr. Health J. 2021, 27, 76–82. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Alcohol. Available online: https://www.who.int/news-room/fact-sheets/detail/alcohol (accessed on 21 September 2018).
- Freedman, N.D.; Park, Y.; Abnet, C.C.; Hollenbeck, A.R.; Sinha, R. Association of coffee drinking with total and cause-specific mortality. N. Engl. J. Med. 2012, 366, 1891–1904. [Google Scholar] [CrossRef] [PubMed]
- Coffee, tea, mate, methylxanthines and methylglyoxal. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 27 February to 6 March 1990. IARC Monogr. Eval. Carcinog. Risks Hum. 1991, 51, 1–513.
- Loomis, D.; Guyton, K.Z.; Grosse, Y.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Mattock, H.; Straif, K. Carcinogenicity of drinking coffee, mate, and very hot beverages. Lancet Oncol. 2016, 17, 877–878. [Google Scholar] [CrossRef]
- LaCroix, A.Z.; Mead, L.A.; Liang, K.Y.; Thomas, C.B.; Pearson, T.A. Coffee consumption and the incidence of coronary heart disease. N. Engl. J. Med. 1986, 315, 977–982. [Google Scholar] [CrossRef] [Green Version]
- Happonen, P.; Voutilainen, S.; Salonen, J.T. Coffee drinking is dose-dependently related to the risk of acute coronary events in middle-aged men. J. Nutr. 2004, 134, 2381–2386. [Google Scholar] [CrossRef]
- Wu, J.N.; Ho, S.C.; Zhou, C.; Ling, W.H.; Chen, W.Q.; Wang, C.L.; Chen, Y.M. Coffee consumption and risk of coronary heart diseases: A meta-analysis of 21 prospective cohort studies. Int. J. Cardiol. 2009, 137, 216–225. [Google Scholar] [CrossRef]
- Lopez-Garcia, E.; Rodriguez-Artalejo, F.; Rexrode, K.M.; Logroscino, G.; Hu, F.B.; van Dam, R.M. Coffee consumption and risk of stroke in women. Circulation 2009, 119, 1116–1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Z.; Hu, G.; Caballero, B.; Appel, L.; Chen, L. Habitual coffee consumption and risk of hypertension: A systematic review and meta-analysis of prospective observational studies. Am. J. Clin. Nutr. 2011, 93, 1212–1219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Keefe, J.H.; Bhatti, S.K.; Patil, H.R.; DiNicolantonio, J.J.; Lucan, S.C.; Lavie, C.J. Effects of habitual coffee consumption on cardiometabolic disease, cardiovascular health, and all-cause mortality. J. Am. Coll. Cardiol. 2013, 62, 1043–1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hakim, A.A.; Ross, G.W.; Curb, J.D.; Rodriguez, B.L.; Burchfiel, C.M.; Sharp, D.S.; Yano, K.; Abbott, R.D. Coffee consumption in hypertensive men in older middle-age and the risk of stroke: The Honolulu Heart Program. J. Clin. Epidemiol. 1998, 51, 487–494. [Google Scholar] [CrossRef]
- Larsson, S.C.; Virtamo, J.; Wolk, A. Coffee consumption and risk of stroke in women. Stroke 2011, 42, 908–912. [Google Scholar] [CrossRef] [Green Version]
- Vane, J.R.; Anggård, E.E.; Botting, R.M. Regulatory functions of the vascular endothelium. N. Engl. J. Med. 1990, 323, 27–36. [Google Scholar] [CrossRef]
- Higashi, Y.; Noma, K.; Yoshizumi, M.; Kihara, Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ. J. Off. J. Jpn. Circ. Soc. 2009, 73, 411–418. [Google Scholar] [CrossRef] [Green Version]
- Matsui, S.; Kajikawa, M.; Hida, E.; Maruhashi, T.; Iwamoto, Y.; Iwamoto, A.; Oda, N.; Kishimoto, S.; Hidaka, T.; Kihara, Y.; et al. Optimal Target Level of Low-density Lipoprotein Cholesterol for Vascular Function in Statin Naïve Individuals. Sci. Rep. 2017, 7, 8422. [Google Scholar] [CrossRef] [Green Version]
- Yamaji, T.; Harada, T.; Hashimoto, Y.; Takaeko, Y.; Kajikawa, M.; Kihara, Y.; Hida, E.; Chayama, K.; Goto, C.; Han, Y.; et al. Pre-impaired fasting glucose state is a risk factor for endothelial dysfunction: Flow-mediated Dilation Japan (FMD-J) study. BMJ Open Diabetes Res. Care 2020, 8, e001610. [Google Scholar] [CrossRef]
- Maruhashi, T.; Soga, J.; Fujimura, N.; Idei, N.; Mikami, S.; Iwamoto, Y.; Kajikawa, M.; Matsumoto, T.; Hidaka, T.; Kihara, Y.; et al. Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart 2013, 99, 1837–1842. [Google Scholar] [CrossRef]
- Hashimoto, H.; Maruhashi, T.; Yamaji, T.; Harada, T.; Han, Y.; Takaeko, Y.; Kihara, Y.; Chayama, K.; Goto, C.; Aibara, Y.; et al. Smoking status and endothelial function in Japanese men. Sci. Rep. 2021, 11, 95. [Google Scholar] [CrossRef] [PubMed]
- Maruhashi, T.; Soga, J.; Fujimura, N.; Idei, N.; Mikami, S.; Iwamoto, Y.; Kajikawa, M.; Matsumoto, T.; Hidaka, T.; Kihara, Y.; et al. Nitroglycerine-induced vasodilation for assessment of vascular function: A comparison with flow-mediated vasodilation. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 1401–1408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsui, S.; Kajikawa, M.; Maruhashi, T.; Iwamoto, Y.; Iwamoto, A.; Oda, N.; Kishimoto, S.; Hidaka, T.; Kihara, Y.; Chayama, K.; et al. Decreased frequency and duration of tooth brushing is a risk factor for endothelial dysfunction. Int. J. Cardiol. 2017, 241, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, T.; Harada, T.; Hashimoto, Y.; Nakano, Y.; Kajikawa, M.; Yoshimura, K.; Chayama, K.; Goto, C.; Han, Y.; Mizobuchi, A.; et al. Stair climbing activity and vascular function in patients with hypertension. Hypertens. Res. 2021, 44, 1274–1282. [Google Scholar] [CrossRef]
- Lopez-Garcia, E.; Rodriguez-Artalejo, F.; Li, T.Y.; Mukamal, K.J.; Hu, F.B.; van Dam, R.M. Coffee consumption and mortality in women with cardiovascular disease. Am. J. Clin. Nutr. 2011, 94, 218–224. [Google Scholar] [CrossRef]
- Kajikawa, M.; Maruhashi, T.; Hidaka, T.; Nakano, Y.; Kurisu, S.; Matsumoto, T.; Iwamoto, Y.; Kishimoto, S.; Matsui, S.; Aibara, Y.; et al. Coffee with a high content of chlorogenic acids and low content of hydroxyhydroquinone improves postprandial endothelial dysfunction in patients with borderline and stage 1 hypertension. Eur. J. Nutr. 2019, 58, 989–996. [Google Scholar] [CrossRef] [Green Version]
- Molnar, J.; Somberg, J.C. Evaluation of the Effects of Different Energy Drinks and Coffee on Endothelial Function. Am. J. Cardiol. 2015, 116, 1457–1460. [Google Scholar] [CrossRef]
- Agudelo-Ochoa, G.M.; Pulgarín-Zapata, I.C.; Velásquez-Rodriguez, C.M.; Duque-Ramírez, M.; Naranjo-Cano, M.; Quintero-Ortiz, M.M.; Lara-Guzmán, O.J.; Muñoz-Durango, K. Coffee Consumption Increases the Antioxidant Capacity of Plasma and Has No Effect on the Lipid Profile or Vascular Function in Healthy Adults in a Randomized Controlled Trial. J. Nutr. 2016, 146, 524–531. [Google Scholar] [CrossRef] [Green Version]
- Buscemi, S.; Verga, S.; Batsis, J.A.; Donatelli, M.; Tranchina, M.R.; Belmonte, S.; Mattina, A.; Re, A.; Cerasola, G. Acute effects of coffee on endothelial function in healthy subjects. Eur. J. Clin. Nutr. 2010, 64, 483–489. [Google Scholar] [CrossRef] [Green Version]
- Papamichael, C.M.; Aznaouridis, K.A.; Karatzis, E.N.; Karatzi, K.N.; Stamatelopoulos, K.S.; Vamvakou, G.; Lekakis, J.P.; Mavrikakis, M.E. Effect of coffee on endothelial function in healthy subjects: The role of caffeine. Clin. Sci. 2005, 109, 55–60. [Google Scholar] [CrossRef] [Green Version]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42, S13–S28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robertson, D.; Frölich, J.C.; Carr, R.K.; Watson, J.T.; Hollifield, J.W.; Shand, D.G.; Oates, J.A. Effects of caffeine on plasma renin activity, catecholamines and blood pressure. N. Engl. J. Med. 1978, 298, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Dobmeyer, D.J.; Stine, R.A.; Leier, C.V.; Greenberg, R.; Schaal, S.F. The arrhythmogenic effects of caffeine in human beings. N. Engl. J. Med. 1983, 308, 814–816. [Google Scholar] [CrossRef]
- Nawrot, P.; Jordan, S.; Eastwood, J.; Rotstein, J.; Hugenholtz, A.; Feeley, M. Effects of caffeine on human health. Food Addit. Contam. 2003, 20, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, S.; Majhi, S.; Saha, B.P.; Mukherjee, P.K. Chlorogenic acid-phospholipid complex improve protection against UVA induced oxidative stress. J. Photochem. Photobiol. B 2014, 130, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.C.; Liou, S.S.; Tzeng, T.F.; Lee, S.L.; Liu, I.M. Effect of topical application of chlorogenic acid on excision wound healing in rats. Planta Med. 2013, 79, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Higashi, Y. Coffee and Endothelial Function: A Coffee Paradox? Nutrients 2019, 11, 2104. [Google Scholar] [CrossRef] [Green Version]
- Saito, E.; Inoue, M.; Sawada, N.; Shimazu, T.; Yamaji, T.; Iwasaki, M.; Sasazuki, S.; Noda, M.; Iso, H.; Tsugane, S. Association of coffee intake with total and cause-specific mortality in a Japanese population: The Japan Public Health Center-based Prospective Study. Am. J. Clin. Nutr. 2015, 101, 1029–1037. [Google Scholar] [CrossRef] [Green Version]
- Zhou, A.; Hyppönen, E. Long-term coffee consumption, caffeine metabolism genetics, and risk of cardiovascular disease: A prospective analysis of up to 347,077 individuals and 8368 cases. Am. J. Clin. Nutr. 2019, 109, 509–516. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).