Vitamin D Status, Cardiovascular Risk Profile, and miRNA-21 Levels in Hypertensive Patients: Results of the HYPODD Study
Abstract
1. Introduction
2. Materials and Methods
2.1. The HYPODD Study
2.2. miR-21 In Vivo Study
2.3. miR-21 In Vitro Study
2.4. Statistical Analysis
3. Results
3.1. The HYPODD Study
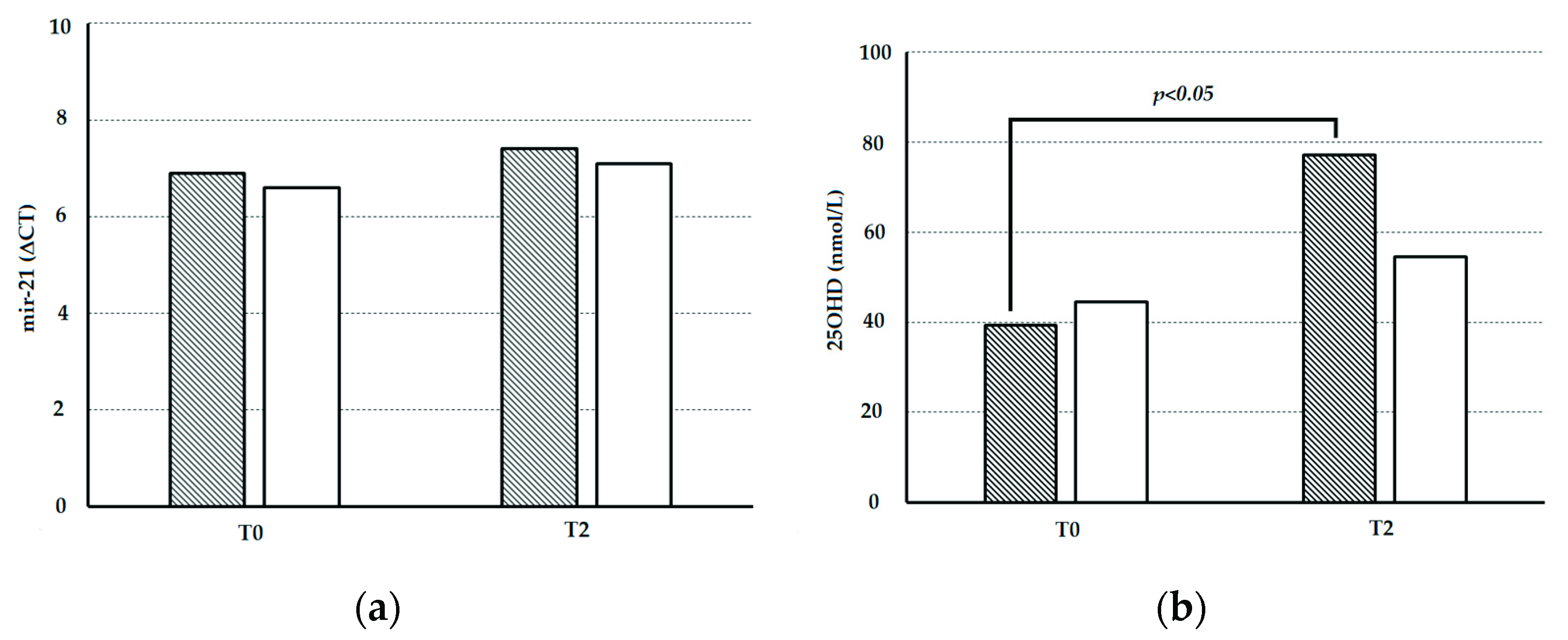
3.2. miR-21 In Vivo Study
3.3. miR-21 In Vitro Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Olsen, M.H.; Angell, S.Y.; Asma, S.; Boutouyrie, P.; Burger, D.; A Chirinos, J.; Damasceno, A.; Delles, C.; Gimenez-Roqueplo, A.-P.; Hering, D.; et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: The Lancet Commission on hypertension. Lancet 2016, 388, 2665–2712. [Google Scholar] [CrossRef]
- E Bauer, U.; A Briss, P.; A Goodman, R.; A Bowman, B. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014, 384, 45–52. [Google Scholar] [CrossRef]
- Bromfield, S.; Muntner, P. High Blood Pressure: The Leading Global Burden of Disease Risk Factor and the Need for Worldwide Prevention Programs. Curr. Hypertens. Rep. 2013, 15, 134–136. [Google Scholar] [CrossRef]
- Kienreich, K.; Dekker, J.M.; Pilz, S.; Zittermann, A.; Meinitzer, A.; März, W.; Lerchbaum, E.; Tomaschitz, A. Vitamin D and cardiovascular disease: Update and outlook. Scand. J. Clin. Lab. Investig. Suppl. 2012, 243, 83–91. [Google Scholar] [CrossRef]
- Rendina, D.; De Filippo, G.; Muscariello, R.; De Palma, D.; Fiengo, A.; De Pascale, F.; Strazzullo, P. Vitamin D and Cardiometabolic Disorders. High Blood Press. Cardiovasc. Prev. 2014, 21, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Bouillon, R. Vitamin D and cardiovascular disorders. Osteoporos. Int. 2019, 30, 2167–2181. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Chen, N.-C.; Hsu, C.-Y.; Mao, P.C.-M.; Dreyer, G.; Wu, F.-Z.; Chen, C.-L. The effects of correction of vitamin D deficiency on arterial stiffness: A systematic review and updated meta-analysis of randomized controlled trials. J. Steroid Biochem. Mol. Biol. 2019, 198, 105561. [Google Scholar] [CrossRef]
- Campbell, M.J. Vitamin D and the RNA transcriptome: More than mRNA regulation. Front. Physiol. 2014, 5, 181. [Google Scholar] [CrossRef]
- Lisse, T.S.; Adams, J.S.; Hewison, M. Vitamin D and microRNAs in bone. Crit. Rev. Eukaryot. Gene Expr. 2013, 23, 195–214. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Trump, D.L.; Johnson, C.S. Vitamin D and miRNAs in cancer. Curr. Gene Ther. 2014, 14, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Li, J.; Cairns, M.J. Identifying miRNAs, targets and functions. Brief. Bioinform. 2014, 15, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Wojciechowska, A.; Braniewska, A.; Kozar-Kamińska, K. MicroRNA in cardiovascular biology and disease. Adv. Clin. Exp. Med. 2017, 26, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Jusic, A.; Devaux, Y. EU-CardioRNA COST Action (CA17129) Noncoding RNAs in Hypertension. Hypertension 2019, 74, 477–492. [Google Scholar] [CrossRef]
- Kontaraki, J.E.; Marketou, M.E.; Parthenakis, F.I.; Maragkoudakis, S.; Zacharis, E.A.; Petousis, S.; Kochiadakis, G.E.; Vardas, P.E. Hypertrophic and antihypertrophic microRNA levels in peripheral blood mononuclear cells and their relationship to left ventricular hypertrophy in patients with essential hypertension. J. Am. Soc. Hypertens. 2015, 9, 802–810. [Google Scholar] [CrossRef]
- Li, X.; Wei, Y.; Wang, Z. microRNA-21 and hypertension. Hypertens. Res. 2018, 41, 649–661. [Google Scholar] [CrossRef]
- Cengiz, M.; Yavuzer, S.; Avcı, B.K.; Yürüyen, M.; Yavuzer, H.; Dikici, S.A.; Karataş, F.; Özen, M.; Uzun, H.; Öngen, Z. Circulating miR-21 and eNOS in subclinical atherosclerosis in patients with hypertension. Clin. Exp. Hypertens. 2015, 37, 643–649. [Google Scholar] [CrossRef]
- Ben-Nun, D.; Buja, L.M.; Fuentes, F. Prevention of heart failure with preserved ejection fraction (HFpEF): Reexamining microRNA-21 inhibition in the era of oligonucleotide-based therapeutics. Cardiovasc. Pathol. 2020, 49, 107243. [Google Scholar] [CrossRef]
- Watanabe, K.; Narumi, T.; Watanabe, T.; Otaki, Y.; Takahashi, T.; Aono, T.; Goto, J.; Toshima, T.; Sugai, T.; Wanezaki, M.; et al. The association between microRNA-21 and hypertension-induced cardiac remodeling. PLoS ONE 2020, 15, e0226053. [Google Scholar] [CrossRef]
- Sheane, B.; Smyth, P.; Scott, K.; Aziz, R.; Buckley, M.; Lodge, E.; Kiely, N.; Kingston, M.; McGovern, E.; Healy, M.; et al. An Association between MicroRNA-21 Expression and Vitamin D Deficiency in Coronary Artery Disease. MicroRNA 2015, 4, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Kocic, H.; Damiani, G.; Stamenkovic, B.; Tirant, M.; Jovic, A.; Tiodorovic, D.; Peris, K. Dietary compounds as potential modulators of microRNA expression in psoriasis. Ther. Adv. Chronic. Dis. 2019, 10, 2040622319864805. [Google Scholar] [CrossRef] [PubMed]
- Golmohammadi, M.G.; Banaei, S.; Nejati, K.; Chinifroush-Asl, M.M. Vitamin D3 and erythropoietin protect against renal ischemia-reperfusion injury via heat shock protein 70 and microRNA-21 expression. Sci. Rep. 2020, 10, 20906. [Google Scholar] [CrossRef]
- Loboda, A.; Sobczak, M.; Jozkowicz, A.; Dulak, J. TGF-β1/Smads and miR-21 in Renal Fibrosis and Inflammation. Mediat. Inflamm. 2016, 2016, 8319283. [Google Scholar] [CrossRef]
- Erkus, E.; Aktas, G.; Atak, B.M.; Kocak, M.Z.; Duman, T.T.; Savli, H. Haemogram Parameters in Vitamin D Deficiency. J. Coll. Physicians Surg. Pak. 2018, 28, 779–782. [Google Scholar] [PubMed]
- Aktas, G.; Khalid, A.; Kurtkulagi, O.; Duman, T.T.; Bilgin, S.; Kahveci, G.; Tel, B.M.A.; Sincer, I.; Gunes, Y. Poorly controlled hypertension is associated with elevated serum uric acid to HDL-cholesterol ratio: A cross-sectional cohort study. Postgrad. Med. 2022, 134, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Rendina, D.; Ippolito, R.; D’Elia, L.; Giacchetti, G.; Lonati, C.; Gianfrancesco, F.; Fallo, F.; Rebellato, A.; Ruggiero, C.; Rubattu, S.D.; et al. Hypovitaminosis D and Organ Damage In Patients With Arterial Hypertension: A Multicenter Double Blind Randomised Controlled Trial of Cholecalciferol Supplementation (HYPODD). High Blood Press. Cardiovasc. Prev. 2015, 22, 135–142. [Google Scholar] [CrossRef][Green Version]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; Yuan, J.; Wu, J.; Deng, X.; Peng, J.; Wang, S.; Yang, C.; Ge, J.; Zou, Y. Evaluation of the performance of serum miRNAs as normalizers in microRNA studies focused on cardiovascular disease. J. Thorac. Dis. 2018, 10, 2599–2607. [Google Scholar] [CrossRef]
- Piras, S.; Furfaro, A.L.; Caggiano, R.; Brondolo, L.; Garibaldi, S.; Ivaldo, C.; Marinari, U.M.; Pronzato, M.A.; Faraonio, R.; Nitti, M. microRNA-494 Favors HO-1 Expression in Neuroblastoma Cells Exposed to Oxidative Stress in a Bach1-Independent Way. Front. Oncol. 2018, 8, 199. [Google Scholar] [CrossRef]
- Verone-Boyle, A.R.; Shoemaker, S.; Attwood, K.; Morrison, C.D.; Makowski, A.J.; Battaglia, S.; Hershberger, P.A. Diet-derived 25-hydroxyvitamin D3 activates vitamin D receptor target gene expression and suppresses EGFR mutant non-small cell lung cancer growth in vitro and in vivo. Oncotarget 2016, 7, 995–1013. [Google Scholar] [CrossRef] [PubMed]
- Barrios, V.; Escobar, C.; Cicero, A.F.G.; Burke, D.; Fasching, P.; Banach, M.; Bruckert, E. A nutraceutical approach (Armolipid Plus) to reduce total and LDL cholesterol in individuals with mild to moderate dyslipidemia: Review of the clinical evidence. Atheroscler. Suppl. 2017, 24, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Sacheck, J.M.; Huang, Q.; I Van Rompay, M.; Chomitz, V.R.; Economos, C.D.; Eliasziw, M.; Gordon, C.M.; Goodman, E. Vitamin D supplementation and cardiometabolic risk factors among diverse schoolchildren: A randomized clinical trial. Am. J. Clin. Nutr. 2021, 115, 73–82. [Google Scholar] [CrossRef]
- Swart, K.M.; Lips, P.; Brouwer, I.; Jorde, R.; Heymans, M.W.; Grimnes, G.; Grübler, M.R.; Gaksch, M.; Tomaschitz, A.; Pilz, S.; et al. Effects of vitamin D supplementation on markers for cardiovascular disease and type 2 diabetes: An individual participant data meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2018, 107, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Tong, C.H.; Rowland, C.M.; Radcliff, J.; Bare, L.A.; McPhaul, M.J.; Devlin, J.J. Association of changes in lipid levels with changes in vitamin D levels in a real-world setting. Sci. Rep. 2021, 11, 21536. [Google Scholar] [CrossRef]
- Liu, W.; Wu, Z.; Zhu, D.; Chen, G.; Yan, G.; Zhang, S.; Chen, F.; Khan, B.A.; Hou, K. Vitamin D and Lipid Profiles in Postmenopausal Women: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. Front. Mol. Biosci. 2021, 8, 799934. [Google Scholar] [CrossRef]
- Zhang, W.; Yi, J.; Liu, D.; Wang, Y.; Jamilian, P.; Gaman, M.-A.; Prabahar, K.; Fan, J. The effect of vitamin D on the lipid profile as a risk factor for coronary heart disease in postmenopausal women: A meta-analysis and systematic review of randomized controlled trials. Exp. Gerontol. 2022, 161, 111709. [Google Scholar] [CrossRef]
- Tournis, S.; Makris, K.; Cavalier, E.; Trovas, G. Cardiovascular Risk in Patients with Primary Hyperparathyroidism. Curr. Pharm. Des. 2020, 26, 5628–5636. [Google Scholar] [CrossRef]
- Altay, H.; Zorlu, A.; Binici, S.; Bilgi, M.; Yilmaz, M.B.; Colkesen, Y.; Erol, T.; Muderrisoglu, H. Relation of Serum Parathyroid Hormone Level to Severity of Heart Failure. Am. J. Cardiol. 2012, 109, 252–256. [Google Scholar] [CrossRef]
- Deo, R.; Katz, R.; Shlipak, M.G.; Sotoodehnia, N.; Psaty, B.M.; Sarnak, M.J.; Fried, L.F.; Chonchol, M.; de Boer, I.H.; Enquobahrie, D.; et al. Vitamin D, parathyroid hormone, and sudden cardiac death: Results from the Cardiovascular Health Study. Hypertension 2011, 58, 1021–1028. [Google Scholar] [CrossRef]
- Yıldırım, E.; Kalkan, K.; Ipek, E.; Aksu, U.; Demirelli, S.; Ermiş, E.; Oztürk, M.; Hamur, H. OP-049 A Novel Marker for Asymptomatic Organ Damage in the Patients with Hypertension: MIR-21. Am. J. Cardiol. 2016, 117, S19. [Google Scholar] [CrossRef]
- Zhang, B.-H.; Shen, C.-A.; Zhu, B.-W.; An, H.-Y.; Zheng, B.; Xu, S.-B.; Sun, J.-C.; Sun, P.-C.; Zhang, W.; Wang, J.; et al. Insight into miRNAs related with glucometabolic disorder. Biomed. Pharmacother. 2019, 111, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Cappello, T.; Wang, L. Emerging role of microRNAs in lipid metabolism. Acta Pharm. Sin. B 2015, 5, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Su, L.; Duan, X.; Chen, X.; Hays, A.; Upadhyayula, S.; Shivde, J.; Wang, H.; Li, Y.; Huang, D.; et al. MicroRNA-21 down-regulates inflammation and inhibits periodontitis. Mol. Immunol. 2018, 101, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Erkus, E.; Aktas, G.; Kocak, M.Z.; Duman, T.T.; Atak, B.M.; Savli, H. Diabetic regulation of subjects with type 2 diabetes mellitus is associated with serum vitamin D levels. Rev. Assoc. Med. Bras. 2019, 65, 51–55. [Google Scholar] [CrossRef]
- Rendina, D.; De Filippo, G.; Strazzullo, P. Should vitamin D status be assessed in patients with congestive heart failure? Nutr. Metab. Cardiovasc. Dis. 2010, 20, 627–632. [Google Scholar] [CrossRef]
- Verdoia, M.; Gioscia, R.; Nardin, M.; Rognoni, A.; De Luca, G. Low levels of vitamin D and coronary artery disease: Is it time for therapy? Kardiologia Polska 2022, 80, 409–416. [Google Scholar] [CrossRef]
- Fillingim, R.B.; Price, D.D. What Is Controlled for in Placebo-Controlled Trials? Mayo Clin. Proc. 2005, 80, 1119–1121. [Google Scholar] [CrossRef]

| C-Cohort | P-Cohort | p | |
|---|---|---|---|
| NumberN | 15 | 20 | |
| M:F | 11 (73.3):4 (26.7) | 13 (65.0):7 (35.0) | 0.72 |
| Age (years) | 59.3 ± 8.3 | 60.8 ± 6.4 | 0.55 |
| BMI (kg/m2) | 27.3 ± 3.3 | 27.4 ± 3.4 | 0.94 |
| Waist Circumference (cm) | 98.0 ± 6.3 | 95.3 ± 9.1 | 0.27 |
| Diuretics (no:yes) | 8 (53.3):7 (46.7) | 8 (42.1):11 (57.9) | 0.73 |
| Calcium antagonists (no:yes) | 9 (60.0):6 (40.0) | 16 (84.2):3 (15.8) | 0.14 |
| RAAS Inhibitors (no:yes) | 3 (20.0):12 (80.0) | 3 (15.8):16 (84.2) | 0.98 |
| Beta-blockers (no:yes) | 12 (80.0):3 (20.0) | 13 (68.4):6 (31.6) | 0.69 |
| Alfa-blockers (no:yes) | 13 (86.7):2 (13.3) | 18 (94.7):1 (5.3) | 0.57 |
| Number of hypertensive drugs used (n) | 2.0 ± 1.1 | 1.94 ± 1.1 | 0.88 |
| C-Cohort | P-Cohort | |||||||
|---|---|---|---|---|---|---|---|---|
| T0 | T2 | T6 | T12 | T0 | T2 | T6 | T12 | |
| 25OHD (nmol/L) | 42.6 ± 10.4 | 78.1 ± 17.8 A | 79.9 ± 14.3 A | 82.9 ± 11.1 A | 43.1 ± 10.1 | 54.5 ± 11.2 B | 50.3 ± 10.3 B | 50.2 ± 9.9 B |
| PTH (pmol/L) | 4.75 ± 2.07 | 4.39 ± 1.84 A | 4.21 ± 1.79 A | 4.20 ± 1.68 A | 4.68 ± 1.97 | 4.58 ± 1.76 | 4.61 ± 1.59 | 4.60 ± 1.87 |
| Glu (mmol/L) | 4.97 ± 0.51 | 4.81 ± 0.48 | 4.73 ± 0.49 | 4.68 ± 0.48 | 5.09 ± 0.52 | 5.12 ± 0.51 | 5.14 ± 0.51 | 5.14 ± 0.52 |
| Ins (pmol/L) | 41.0 ± 25.0 | 39.6 ± 22.2 | 36.8 ± 19.5 | 35.4 ± 19.5 | 49.3 ± 22.9 | 50.1 ± 21.5 | 49.4 ± 21.5 | 49.3 ± 18.8 |
| HOMA-IR | 1.21 ± 0.22 | 1.21 ± 0.24 | 1.28 ± 0.21 | 1.32 ± 0.23 | 1.03 ± 0.24 | 1.02 ± 0.21 | 1.04 ± 0.23 | 1.04 ± 0.25 |
| T-Chol (mmol/L) | 4.67 ± 0.77 | 4.23 ± 0.47 A | 4.36 ± 0.44 A | 4.37 ± 0.44 A | 5.03 ± 0.53 | 4.92 ± 0.46 | 4.82 ± 0.47 | 4.88 ± 0.44 |
| HDL-Chol (mmol/L) | 1.43 ± 0.39 | 1.40 ± 0.37 | 1.39 ± 0.36 | 1.38 ± 0.35 | 1.52 ± 0.50 | 1.52 ± 0.40 | 1.48 ± 0.42 | 1.50 ± 0.43 |
| LDL-Chol (mmol/L) | 2.72 ± 0.90 | 2.52 ± 0.75 A | 2.48 ± 0.78 A | 2.47 ± 0.74 A | 2.93 ± 0.55 | 2.75 ± 0.55 | 2.80 ± 0.68 | 2.79 ± 0.64 |
| Tri (mmol/L) | 1.35 ± 0.80 | 1.16 ± 0.58 A | 1.15 ± 0.51 A | 1.15 ± 0.55 A | 1.34 ± 0.70 | 1.31 ± 0.61 | 1.34 ± 0.57 | 1.31 ± 0.56 |
| Crea (µmol/L) | 78.7 ± 15.9 | 78.7 ± 15.9 | 76.0 ± 15.0 | 76.9 ± 11.5 | 71.6 ± 15.0 | 71.6 ± 15.0 | 75.1 ± 11.5 | 76.9 ± 15.9 |
| Ca (mmol/L) | 2.41 ± 0.13 | 2.41 ± 0.13 | 2.40 ± 0.12 | 2.41 ± 0.13 | 2.44 ± 0.14 | 2.44 ± 0.14 | 2.43 ± 0.12 | 2.43 ± 0.13 |
| Alb (g/L) | 47 ± 3 | 47 ± 4 | 45 ± 6 | 46 ± 4 | 47 ± 4 | 46 ± 5 | 46 ± 5 | 46 ± 5 |
| Mg (mmol/L) | 0.75 ± 0.23 | 0.76 ± 0.28 | 0.77 ± 0.26 | 0.79 ± 0.25 | 0.67 ± 0.25 | 0.75 ± 0.23 | 0.76 ± 0.25 | 0.76 ± 0.21 |
| P (mmol/L) | 1.07 ± 0.13 | 1.07 ± 0.13 | 1.13 ± 0.16 | 1.16 ± 0.16 | 1.16 ± 0.20 | 1.16 ± 0.20 | 1.10 ± 0.16 | 1.07 ± 0.17 |
| Na (mmol/L) | 141.4 ± 1.5 | 141.6 ± 1.6 | 141.2 ± 1.5 | 141.9 ± 1.8 | 141.8 ± 1.9 | 142.1 ± 1.9 | 141.8 ± 1.8 | 141.8 ± 1.8 |
| K (mmol/L) | 4.28 ± 0.46 | 4.27 ± 0.51 | 4.30 ± 0.51 | 4.28 ± 0.41 | 4.21 ± 0.49 | 4.26 ± 0.47 | 4.27 ± 0.48 | 4.28 ± 0.39 |
| TSH (mUI/L) | 2.37 ± 0.91 | 2.19 ± 0.88 | 1.87 ± 0.76 | 1.71 ± 0.67 | 1.90 ± 0.81 | 2.08 ± 0.89 | 2.16 ± 0.71 | 2.18 ± 0.61 |
| SBP (mmHg) | 133.8 ± 6.1 | 128.7 ± 5.9 | 127.4 ± 5.8 | 124.8 ± 6.1 | 132.0 ± 6.3 | 128.0 ± 6.0 | 129.5 ± 6.1 | 131.3 ± 5.8 |
| DBP (mmHg) | 80.7 ± 6.1 | 80.1 ± 5.6 | 79.8 ± 5.6 | 79.7 ± 6.0 | 79.3 ± 7.5 | 80.4 ± 7.1 | 82.1 ± 6.9 | 83.4 ± 7.0 |
| C-Cohort | P-Cohort | |||||
|---|---|---|---|---|---|---|
| ΔT2 | ΔT6 | ΔT12 | ΔT2 | ΔT6 | ΔT12 | |
| 25OHD (nmol/L) | +35.5 ± 8.1 A | +37.3 ± 8.3 A | +40.3 ± 91.1 A | +11.4 ± 3.2 | +7.2 ± 4.1 | +7.1 ± 3.9 |
| PTH (pmol/L) | −0.36 ± 0.09 A | −0.54 ± 0.09 A | −0.55 ± 0.10 A | −0.10 ± 0.03 | −0.07 ± 0.02 | −0.08 ± 0.03 |
| Glu (mmol/L) | −0.16 ± 0.04 | −0.24 ± 0.06 | −0.29 ± 0.07 | +0.03 ± 0.01 | +0.05 ± 0.01 | +0.05 ± 0.01 |
| Ins (pmol/L) | −1.4 ± 0.7 | −4.2 ± 1.3 | −5.6 ± 1.5 | +0.8 ± 0.3 | +0.1 ± 0.1 | +0.0 ± 0.1 |
| HOMA-IR | 0.0 ± 0.15 | +0.07 ± 0.12 | +0.09 ± 0.12 | −0.01 ± 0.11 | 0.01 ± 0.09 | 0.01 ± 0.09 |
| T-Chol (mmol/L) | −0.44 ± 0.09 A | −0.31 ± 0.08 A | −0.30 ± 0.09 A | −0.11 ± 0.05 | −0.21 ± 0.07 | −0.15 ± 0.06 |
| HDL-Chol (mmol/L) | −0.03 ± 0.01 | −0.04 ± 0.02 | −0.05 ± 0.02 | +0.00 ± 0.01 | −0.04 ± 0.02 | −0.02 ± 0.02 |
| LDL-Chol (mmol/L) | −0.20 ± 0.05 | −0.24 ± 0.05 A | −0.25 ± 0.04 A | −0.18 ± 0.09 | −0.13 ± 0.07 | −0.14 ± 0.08 |
| Tri (mmol/L) | −0.19 ± 0.07 A | −0.20 ± 0.07 A | −0.20 ± 0.06 A | −0.03 ± 0.02 | 0.00 ± 0.02 | −0.03 ± 0.02 |
| rea (µmol/L) | 0.0 ± 0.9 | −2.7 ± 1.0 | −1.8 ± 1.1 | +0.0 ± 0.9 | +3.5 ± 1.4 | +5.3 ± 1.9 |
| Ca (mmol/L) | 0.00 ± 0.01 | −0.01 ± 0.01 | 0.00 ± 0.01 | +0.00 ± 0.01 | −0.01 ± 0.01 | −0.01 ± 0.01 |
| Alb (g/L) | 0 ± 2 | −2 ± 1 | −1 ± 1 | −1 ± 1 | −1 ± 1 | −1 ± 1 |
| Mg(mmol/L) | +0.01 ± 0.01 | +0.02 ± 0.01 | +0.04 ± 0.01 | +0.08 ± 0.05 | +0.09 ± 0.05 | +0.09 ± 0.04 |
| P (mmol/L) | +0.00 ± 0.03 | +0.06 ± 0.04 | +0.09 ± 0.06 | 0.00 ± 0.02 | −0.06 ± 0.03 | −0.09 ± 0.04 |
| Na (mmol/L) | +0.2 ± 0.6 | −0.2 ± 0.5 | +0.5 ± 0.4 | +0.3 ± 0.4 | +0.0 ± 0.8 | +0.0 ± 0.8 |
| K (mmol/L) | −0.01 ± 0.01 | +0.02 ± 0.01 | +0.00 ± 0.03 | +0.05 ± 0.04 | +0.06 ± 0.04 | +0.07 ± 0.04 |
| TSH (mUI/L) | −0.18 ± 0.10 | −0.50 ± 0.11 | −0.66 ± 0.12 | +0.18 ± 0.09 | +0.26 ± 0.11 | +0.28 ± 0.12 |
| SBP (mmHg) | −5.1 ± 3.9 | −6.4 ± 3.8 | −9.0 ± 4.1 A | −4.0 ± 3.1 | −2.5 ± 3.1 | −0.7 ± 2.8 |
| DBP (mmHg) | −0.6 ± 2.6 | −0.9 ± 2.1 | −1.0 ± 1.9 | +1.1 ± 2.1 | +2.8 ± 1.9 | +4.1 ± 2.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rendina, D.; D′Elia, L.; Abate, V.; Rebellato, A.; Buondonno, I.; Succoio, M.; Martinelli, F.; Muscariello, R.; De Filippo, G.; D′Amelio, P.; et al. Vitamin D Status, Cardiovascular Risk Profile, and miRNA-21 Levels in Hypertensive Patients: Results of the HYPODD Study. Nutrients 2022, 14, 2683. https://doi.org/10.3390/nu14132683
Rendina D, D′Elia L, Abate V, Rebellato A, Buondonno I, Succoio M, Martinelli F, Muscariello R, De Filippo G, D′Amelio P, et al. Vitamin D Status, Cardiovascular Risk Profile, and miRNA-21 Levels in Hypertensive Patients: Results of the HYPODD Study. Nutrients. 2022; 14(13):2683. https://doi.org/10.3390/nu14132683
Chicago/Turabian StyleRendina, Domenico, Lanfranco D′Elia, Veronica Abate, Andrea Rebellato, Ilaria Buondonno, Mariangela Succoio, Fabio Martinelli, Riccardo Muscariello, Gianpaolo De Filippo, Patrizia D′Amelio, and et al. 2022. "Vitamin D Status, Cardiovascular Risk Profile, and miRNA-21 Levels in Hypertensive Patients: Results of the HYPODD Study" Nutrients 14, no. 13: 2683. https://doi.org/10.3390/nu14132683
APA StyleRendina, D., D′Elia, L., Abate, V., Rebellato, A., Buondonno, I., Succoio, M., Martinelli, F., Muscariello, R., De Filippo, G., D′Amelio, P., Fallo, F., Strazzullo, P., & Faraonio, R. (2022). Vitamin D Status, Cardiovascular Risk Profile, and miRNA-21 Levels in Hypertensive Patients: Results of the HYPODD Study. Nutrients, 14(13), 2683. https://doi.org/10.3390/nu14132683









