We appreciate Dr. Shabih Manzar’s interest [1] in our recently published work, “Nutrient Intake with Early Progressive Enteral Feeding and Growth of Very Low-Birth-Weight Newborns” [2] and his comments on several issues in our study.
- Rate of necrotizing enterocolitis
We included 120 infants in the initial cohort and did not exclude, but censored, their data on the day of death or bowel resection, which is stated in the flowchart (Figure 1) [2]. The aim of the study was to assess nutrient intake and its relationship with early growth; thus, we assumed that infants with partial bowel resection would have some degree of malabsorption, and their growth should not be compared to those with an intact bowel. We excluded these infants’ data from the nutritional and growth analyses, but we used the demographic data of the initial cohort in Table 1 [2]. Thus, we reassure the reader that the total number of infants with necrotizing enterocolitis and spontaneous intestinal perforation was eight in the whole cohort, six of whom were in the <1000 g birth-weight group.
- Fluid intake and patent ductus arteriosus (PDA)
Daily fluid intake in Figure 3e [2] is separated to parenteral and enteral intake, and it does not exactly represent total daily intake. Our aim was to describe the trends of enteral and parenteral fluid intakes in the real picture of such an early transition phase. In our article we discussed the challenge of balancing between fluid overload and nutrient intake, though with a greater focus on potential nutrient deficit. More detailed data on total daily fluid intake in different birth-weight groups is presented in Table 1 [2], which indicates higher intake in the smallest infants during the first week, but lower intake afterwards.
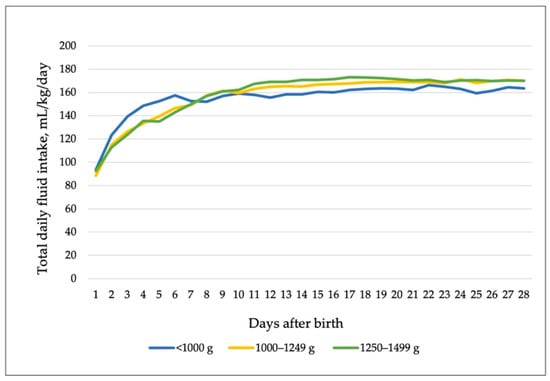
Figure 1.
Total daily fluid (parenteral and enteral) intake in different birth-weight groups. Data are medians.
There is no clear definition regarding the exact volume of parenteral or enteral fluid that may contribute to a higher risk of PDA, but we agree with the comment that it is important to be aware of the total daily fluid given during the transition from parenteral to enteral nutrition, especially in early life. The incidence of hemodynamically significant PDA in our cohort was 65.2% in the <1000 g group, similar to the rates reported in [3]; 23.2% in 1000–1249 g group; and 8.8% in 1250–1499 g group.
- Growth
Adding the calculations with the author’s suggested triple method, the median weight-gain velocity from birth to discharge, calculated using the 2-point method, was 13.9, 13.7, and 12.9 g/kg/day in birth-weight groups G1 (<1000 g), G2 (1000–1249 g), and G3 (1250–1499 g), respectively. Weight-gain velocity calculated using the exponential method was 15.6, 14.6, and 13.2 g/kg/day in G1, G2, and G3, respectively. The weight-gain ratio (WGR) was 0.93 in G1, 0.87 in G2, and 0.78 in G3, indicating that the weight-gain ratio of the smallest newborns was closer to the suggested values, as was the change in weight z-scores that we provided in our article. However, this triple method includes only the weight gain. We strongly support the approach that linear growth, i.e., length and head circumference, should be assessed concurrently [4]. Body length reflects lean body-mass accretion, and head-circumference growth reflects the brain growth, both contributing to optimal body composition and neurodevelopmental outcomes [5,6,7].
Author Contributions
Conceptualization, K.A.-W., R.V. and R.B.; methodology, K.A.-W., R.V. and R.B.; formal analysis, K.Š.; investigation, R.B. and A.V.; data curation, R.B. and K Š.; writing—original draft preparation, R.B.; writing—review and editing, K.A.-W., R.V. and R.T.; visualization, K.Š. and R.B. All authors have read and agreed to the published version of the manuscript.
Funding
The supplies for this study’s human milk analysis were donated by Rotary Club of Chicagoland Lithuanians.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Manzar, S. Comment on Brinkis et al. Nutrient Intake with Early Progressive Enteral Feeding and Growth of Very Low-Birth-Weight Newborns. Nutrients 2022, 14, 1181. Nutrients 2022, 14, 2651. [Google Scholar] [CrossRef]
- Brinkis, R.; Albertsson-Wikland, K.; Tamelienė, R.; Vinskaitė, A.; Šmigelskas, K.; Verkauskienė, R. Nutrient Intake with Early Progressive Enteral Feeding and Growth of Very Low-Birth-Weight Newborns. Nutrients 2022, 14, 1181. [Google Scholar] [CrossRef] [PubMed]
- Koch, J.; Hensley, G.; Roy, L.; Brown, S.; Ramaciotti, C.; Rosenfeld, C.R. Prevalence of Spontaneous Closure of the Ductus Arteriosus in Neonates at a Birth Weight of 1000 Grams or Less. Pediatrics 2006, 117, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Pereira-da-Silva, L.; Virella, D.; Fusch, C. Nutritional Assessment in Preterm Infants: A Practical Approach in the NICU. Nutrients 2019, 11, 1999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyers, J.M.; Tan, S.; Bell, E.F.; Duncan, A.F.; Guillet, R.; Stoll, B.J.; D’Angio, C.T.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental outcomes among extremely premature infants with linear growth restriction. J. Perinatol. 2019, 39, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Simon, L.; Théveniaut, C.; Flamant, C.; Frondas-Chauty, A.; Darmaun, D.; Rozé, J.-C. In Preterm Infants, Length Growth below Expected Growth during Hospital Stay Predicts Poor Neurodevelopment at 2 Years. Neonatology 2018, 114, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Raghuram, K.; Yang, J.; Church, P.T.; Cieslak, Z.; Synnes, A.; Mukerji, A.; Shah, P.S.; Canadian Neonatal Network; Canadian Neonatal Follow-Up Network Investigators. Head Growth Trajectory and Neurodevelopmental Outcomes in Preterm Neonates. Pediatrics 2017, 140, e20170216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).